Abstract
CD8+ T cell responses are critical for the control of virus infections. Following infection, epitope-specific responses establish an unpredictable but reproducible pattern of dominance that is dictated by a large number of both positive and negative factors. Immunodomination, or diminution of subdominant epitope-specific responses by dominant epitopes, can play a substantial role in the establishment of epitope hierarchy. To determine the role of a dominant (KdM282–90) and a subdominant (DbM187–195) epitope of respiratory syncytial virus in viral control and immunodomination, MHC-binding anchor residues in the two epitopes were mutated individually in recombinant infectious viruses, greatly reducing or deleting the epitope-specific CD8+ T cell responses. Neither mutation negatively affected viral clearance in mice, and compensation by the unmutated epitope was seen in both cases, whereas compensation by five other subdominant epitopes was minimal. Mutation of the dominant KdM282–90 response resulted in effective viral clearance by the subdominant epitope with less illness, whereas mutation of the subdominant DbM187–195 response resulted in overcompensation of the already dominant KdM282–90 epitope, and increased severity of illness. Increased illness was associated with poor functionality of the abundant population of CD8+ T cells specific to the dominant KdM282–90 epitope, as measured by the percentage and magnitude of IFN-γ production. These data demonstrate efficient viral clearance, and a protective effect of subdominant CD8+ T cell responses.
Cytotoxic T lymphocytes are the primary immune mechanism to control infection by viruses and other intracellular pathogens. Viral peptides are processed and presented in the context of MHC class I molecules for recognition by CD8+ T cells (1). The requirements for presentation by MHC class I limit the number of viral epitopes that can be recognized by CD8+ T cells, and responses are often limited to a surprisingly small number of epitopes. Within responding CD8+ T cells, reproducible epitope dominance patterns are often established, creating an immunodominance hierarchy. Many factors can contribute to epitope hierarchy, including those related to epitope processing and presentation, those inherent to CD8+ T cell frequency and function, and regulation imposed by other elements of the immune response or local environment (2–5). The primary factors responsible for the establishment of epitope dominance may vary depending on the system and infection studied, and additional factors may come into play and alter immunodominance during chronic infection or following reinfection (2–9).
Respiratory syncytial virus (RSV) is a virus that can cause severe disease in infants, the institutionalized elderly, and hosts with compromised cellular immunity. It is the major cause of bronchiolitis, pneumonia, mechanical ventilation, respiratory failure, and hospitalization in infants in the United States (10). The role of CD8+ T cells in RSV infection is still somewhat controversial. Although some studies show an extensive presence of Ag and a near absence of CD8+ T cells in infants that experience severe infection or died of severe RSV (11, 12), we demonstrated that, although not the predominant cell type, CD8+ T cells are found in the peribronchiolar and interstitial infiltrates and significantly outnumbered CD4+ T cells in the lungs of an RSV-infected infant (13). Robust, systemic virus-specific CD8+ T cell responses have been found in infants with severe disease and do not correlate with disease severity (14, 15). In fact, the RSV-specific T cell responses peak during convalescence, and are unlikely to contribute to disease (14). In addition to their role in viral clearance, CD8+ T cells have been found to protect against vaccine-enhanced illness after vaccination with formalin-inactived RSV in the mouse model (16).
Immune responses to RSV are often studied in the mouse model, where CD8+ T cell responses are strong and sufficient to eliminate the virus, but are also the source of immunopathology and illness (17). We use the CB6F1 mouse model, where both d- and b-allele responses can be measured simultaneously, and the majority of the response is to two viral epitopes, K M282–90 and D M187–195, which respond in a predictable hierarchy (18). To determine the contribution of individual epitope-specific responses, we mutated peptide anchor residues to eliminate or alter the response to the K M282–90 and D M187–195 epitopes. Either dramatically reducing an epitope-specific response, or eliminating the response all together resulted in compensation by the other epitope, with little compensation observed by five other subdominant epitopes. This indicates a reciprocity between the KdM282–90 and the DbM187–195 epitope, and showed that both epitopes immunodominate the other five epitopes during primary RSV infection. Surprisingly, having a quantitatively smaller response to the normally immunodominant KdM282–90 epitope resulted in reduced illness without reducing the efficiency of viral clearance. Conversly, abrogating the response to the already subdominant DbM187–195 epitope, resulting in overcompensation by the dominant KdM282–90 epitope, exacerbated illness with no benefit with regard to viral clearance.
Materials and Methods
Generation of live RSV with single amino acid changes in epitope anchor residues
Recombinant epitope-mutated RSV was generated using reverse genetics (19). Point mutations were generated by site-directed mutagenesis of sub-cloned portions of the whole RSV genome using a Quickchange site-directed mutagenesis kit (Stratagene, La Jolla, CA) and primers with mutations at the nucleotides of interest. Following confirmation of single amino acid changes, whole genome cDNA constructs with the mutations were generated. All mutations were made in antigenome cDNA 46/6120, with a deletion in the downstream noncoding region of the SH gene and silent modifications in the last few codons of the SH open reading frame previously shown to improve stability of the cDNA without effecting the efficiency of viral replication in vitro or in mice (20). Following antigenome construction, live viruses were rescued as previously described (19, 21). Briefly, BSR T7/5 cells were cotransfected with 5 mg antigenome DNA and plasmids expressing N (2 mg), P (2 μg), M2-1 (1 μg), and L (1 μg) using Lipofectamine 2000. Cells were incubated overnight at 32°C prior to scraping into media and adding to subconfluent monolayers of HEp-2 cells. Cultures were incubated at 32°C, and viruses were harvested 14 d posttransfection. RSVwt, RSV-M2I90T, and RSV-MN191S viral stocks for infection were purified by four rounds of plaque purification and derived by sonication of infected HEp-2 monolayers as previously described (22). This method ensures that viral stocks originate from a single viral clone. All epitope mutations were confirmed by RT-PCR of the M and M2 proteins from infected HEp-2 cells following generation of the final stock. HEp-2 cells were maintained in Eagle's MEM containing 10% FBS (10% EMEM), and were supplemented with 2 mM glutamine, 10 U penicillin G per ml, and 10 mg streptomycin sulfate per ml. Cells were determined to be free of mycoplasma contamination by PCR analysis (American Type Culture Collection, Manassas, VA).
Mice and RSV infections
Adult (6- to 10-wk-old) female CB6F1/J mice (The Jackson Laboratory, Bar Harbor, ME) were used for all experiments. All mice were housed in our animal care facility at National Institute of Allergy and Infectious Disease under specific, pathogen-free conditions, and maintained on standard rodent chow and water supplied ad libitum. All studies were reviewed and approved by the National Institutes of Health Animal Care and Use Committee. Mice were anesthetized i.m. with ketamine (40 μg/g body weight) and xylazine (6 μg/g body weight) prior to intranasal inoculation with 3 × 106 PFU live RSV in 100 μl 10% EMEM. Mice were weighed daily postinfection, and percent weight lost was used to assess the severity of illness.
Plaque assays
Mice were sacrificed and lung tissue was removed and quick frozen in 10% EMEM. Thawed tissues were kept chilled while individually ground with mortar and pestle as previously described. Dilutions of clarified supernatant were inoculated on 80% confluent HEp-2 cell monolayers in triplicate and overlaid with 0.75% methyl cellulose in 10% EMEM. After incubation for 4 d at 37°C, the monolayers were fixed with 10% buffered formalin and stained with H&E. Plaques were counted and expressed as log10 PFU/g of tissue. The limit of detection is 1.8 log10 PFU/g of tissue.
Synthetic peptides
RSV M282–90 wild-type (wt) and mutant I90T (SYIGSINNI and SYIGSINNT) and RSV M187–195 wt and mutant N191S (NAITNAKII and NAITSAKII) peptides were derived from the RSV M2 and M proteins. Peptides for subdominant epitopes M2127–135 (VYNTVISYI), F85–93 (KYKNAVTEL), F250–258 (YLTNSELL), F433–442 (KTFSNGCDYV), N57–64 (ANHKFTGL), and N360–368 (NGVINYSVL) were similarly generated from the sequence of RSV-A2. The H2-Kd–binding influenza virus A/Puerto Rico/8/34 NP147–155 (TYQRTRALV) peptide, and H2-Db–binding influenza A/Puerto Rico/8/34 NP366–374 (ASNENMETM) peptide were used as negative controls. All peptides were synthesized by Anaspec (San Jose, CA), and confirmed to be >95% pure by analytical HPLC at the National Institute of Allergy and Infectious Disease peptide core facility (Bethesda, MD).
Tetramer and intracellular cytokine staining
Mice were sacrificed and lung and spleen tissues were harvested at various times between days 4–14 postinfection. Spleens were also harvested 60– 100 d postinfection to analyze memory responses. Tissues were disrupted manually between the frosted ends of two sterile glass microscope slides in RPMI 1640 containing 10% FBS (RPMI-10), or by tissue dissociation using a gentleMACS machine (Miltenyi, Germany). Lymphocytes were purified using Ficol LITE at room temperature, washed, then resuspended in RPMI-10. For intracellular cytokine staining (ICS), lymphocytes were incubated at 37°C for 5 h with 1 μM of the appropriate peptide, 1 μg/ml of the costimulatory Abs against CD28 and CD49d, and 1 μg/ml monensin. After the incubation, cells were surface stained with fluorochrome-conjugated Abs against CD3 (145-2C11), CD4 (GK1.5), and CD8 (2.43) then fixed and permeabilized using an ICS kit according to the manufacturer's instructions (BD Pharmingen, San Diego, CA). Intracellular stains were done with labeled Abs to IFN-γ (XMG1.2), IL-2 (JES6-5H4), and TNF-α (MP6-XT22) for 20 min at 4°C. For tetramer analysis, cells were stained with KdM282–90, KdM2127–135, or DbM187–195 tetramer (Beckman Coulter, San Diego, CA) during a surface stain also containing Abs for CD3, CD4, and CD8. After staining, cells were washed and analyzed by flow cytometry. Cells were analyzed on an LSR-II (Becton Dickinson, San Jose, CA), and data were analyzed using FlowJo version 8.8.5 (Tree Star, San Carlos, CA). For ICS analysis, Boolean gating was performed after single gating for each cytokine, and background from influenza peptide stimulated control samples was subtracted in Pestle (software provided by Mario Roederer, Bethesda, MD) prior to graphing.
In vivo CTL assays
Lymphocytes were harvested from spleens of naive CB6F1 mice and prepared as targets. After isolation, cells were divided into four samples. One sample of cells was incubated with M282–90 peptide, one was incubated with M187–195 peptide, and the remaining two samples were incubated without peptide as controls, all at 37°C for 1 h in RPMI-10. Cells were washed in PBS, and resuspended in 1 mL PBS per sample. The M282–90-pulsed cells were incubated with a high concentration of CFSE (CFDA-SE, 2 mM, Molecular Probes, Eugene, OR), whereas one control sample was stained with a low concentration of CFSE (0.1 μM). M187–195-pulsed cells were incubated with high concentrations of chloromethylbenzoylaminotetramethylrhodamine (CMTMR, 25 μM, Molecular Probes), and the final control sample was stained with a low concentration of CMTMR (2.5 μM). All samples were stained for 10 min in a 37°C water bath, then 0.5 ml heat-inactivated FBS was added, followed by a 5-min incubation at room temperature. Finally, the samples were washed three times with RPMI-10, resuspended in PBS, and combined. Mice that had been infected 7 d prior were injected i.v. in the tail vein with 100 ml of the mixture containing 5 × 106 cells of each of the four labeled populations. Fifteen hours later, lung and spleen lymphocytes were harvested, and the frequency of each of the populations labeled with CFSE or CMTMR was determined by flow cytometry. Cells were injected into naive recipients as controls, and percent specific lysis was determined by comparing the recovered frequency of peptide-pulsed cells to the frequency of cells not pulsed with peptide in infected mice compared with naive controls.
Statistical analysis
Data were analyzed in GraphPad Prism using a one-way or two-way ANOVA, followed by Bonferroni's posttests for multiple comparisons for significance between all groups.
Results
Live RSV tolerates single amino acid changes in anchor residues of the KdM282–90 and DbM187–195 CD8+ T cell epitopes
To date, several CD8+ T cell epitopes have been mapped in H-2d (BALB/c) and H-2b (C57BL/6) strains (23–29). Our laboratory has made use of the H-2d/b CB6F1 hybrid mouse to simultaneously investigate responses to a larger number of epitopes (Table I). The KdM282–90 is a strongly dominant response in the RSV-infected BALB/c (H-2d) parental strain with only a small fraction of CD8+ T cells specific for other described epitopes (23–27). In primary infected C57BL/6 mice (H-2b), the DbM187–195 epitope is similarly dominant, with significantly lower responses to other described epitopes (28, 29). Following infection of the CB6F1 mouse, the KdM282–90 epitope dominates the CD8+ T cell response and the DbM187–195 epitope becomes subdominant and accounts for 3- to 5-fold fewer tetramer-positive CD8+ T cells than the dominant response. Overall, the combined response to the KdM282–90 and the DbM187–195 epitopes can account for up to 75% of all CD8+ T cells found in the lungs of infected CB6F1 (18), with other described epitopes (Table I) playing a minor role in the overall CD8+ T cell response.
Table I. CD8+ T cell epitopes described in BALB/c and C57BL/6 mouse strains.
| Epitopes | Reference | RSV Protein | MHC Restriction | Peptide Sequencea |
|---|---|---|---|---|
| Epitopes described in BALB/c mice (H-2d) | (26) | M282–90 | Kd | SYIGSINNI |
| (23) | F85–93 | Kd | KYKNAVTEL | |
| (27) | M2127–135 | Kd | VYNTVISYI | |
| (24) | F92–106 | Kd | ELQLLMQSTPPTNNR | |
| (25) | F249–258 | Kd | TYMLTNSELL | |
| Epitopes described in C57BL/6 (H-2b) | (29) | M187–195 | Db | NAITNAKII |
| (28) | F250-258 | Db | YMLTNSELL | |
| (28) | F433–442 | Db | KTFSNGCDYV | |
| (28) | N57–64 | Kb | ANHKFTGL | |
| (28) | N360–368 | Db | NGVINYSVL |
Anchor residues are shown in bold.
First, we asked how the response hierarchy would change if a major component of the response was removed. We sought to eliminate the CD8+ T cell response to either the KdM282–90 or the DbM187–195 epitope of RSV and evaluate subsequent CD8+ T cell responses in infected CB6F1. To abrogate peptide binding to the MHC molecule, the anchor residues of each peptide were targeted for mutation. Site-directed mutagenesis of the RSVA2 antigenome plasmid was performed, and attempts to rescue epitope mutant viruses were performed by transfecting BHK-T7 cells with the antigenome plasmid in conjunction with helper plasmids expressing N, P, M2-1, and L as summarized in the Materials and Methods and previously described (19). Successful mutations of the anchor amino acid residues were confirmed by RT-PCR and sequencing of the targeted gene following infection of HEp-2 cells.
Initial attempts were made to change the tyrosine at residue 2 of the M282–90 peptide (SYIGSINNI) to an arginine (Y83R), a mutation previously shown to completely abolish the response to the KdM282–90 epitope (26). As described by others, live RSV of this genotype could not be rescued despite numerous attempts, indicating that the mutation most likely negatively affects the function of the M2 protein (30). Likewise, attempts to rescue viruses with threonine (Y83T) or serine (Y83S) at the position 2 anchor were also unsuccessful. Although live RSV could be rescued with a more conservative substitution of another hydrophobic aromatic amino acid at the position 2 MHC binding residue (Y83F), we found that this mutation resulted in a virus that also induced a strongly dominant KdM282–90 response, indicating that phenylalanine in position 83 may also serve as an MHC-binding anchor residue (data not shown). Finally, live RSV with a mutation of the anchor residue at position 9 from an isoleucine to a threonine (RSV-M2I90T) was successfully rescued (Fig. 1A). This mutation is known to result in a 10-fold lower binding affinity of the M282–90 peptide for H2-Kd (31).
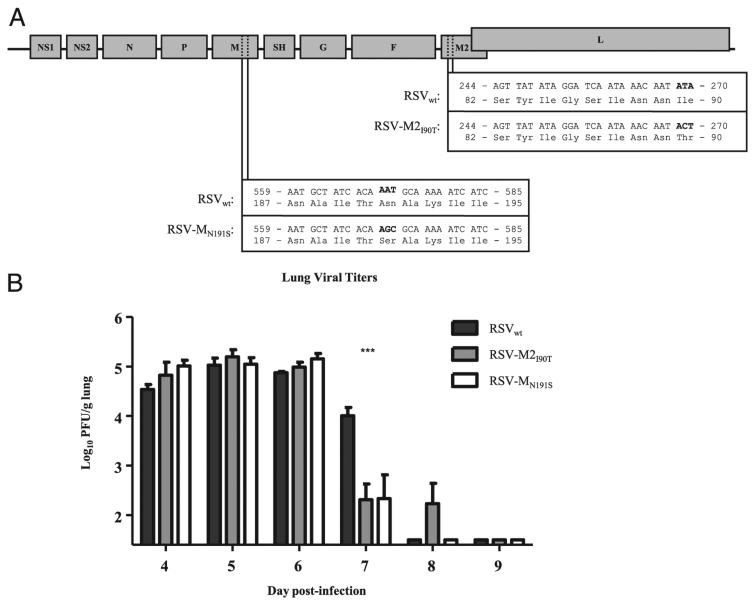
Figure 1.
Live RSV with anchor residue mutations in the KdM282–90 and DbM187–195 epitopes can be rescued and grow with wt phenotype. A, Single amino acid changes of the RSV genome were made by point mutation in smaller subcloning plasmids prior to introduction into a plasmid containing the entire RSV genome and rescue by reverse genetics (as described in Materials and Methods). B, RSV viral titers in the lungs following infection with 3 × 106 PFU of RSVwt, RSV-M2I90T, or RSV-MN191S between days 4 and 9 postinfection. ***p < 0.001. Data are representative of two experiments with four to five mice/group and error bars represent the SEM.
The M187–195 subdominant response peptide contains MHC-binding anchor residues at amino acid positions 5 and 9. In this case, substitution of the asparagine at position 5 for a serine resulted in a virus that was readily and reproducibly rescued (RSV-MN191S, Fig. 1A). Both RSV-M2190T and RSV-MN191S grew well in cultured HEp-2 cells.
Epitope-mutant RSV replicate like wt in CB6F1 mice and are cleared with similar kinetics
Four rounds of plaque purification were done for each RSVwt, RSV-M2I90T, and RSV-MN191S, and high-titer stocks derived from single isolated plaques were generated as previously described (22). Viral titer typically peaks at day 4 or 5 following intranasal infection of CB6F1 mice with RSVwt, and clearance is achieved by 7–8 d postinfection. CB6F1 mice infected with 3 × 106 PFU of wt RSVwt, RSV-M2I90T, and RSV-MN191S had similar lung viral titer kinetics when measured daily between days 4–9 following infection (Fig. 1B). At day 7, epitope-mutated viruses were cleared better than RSVwt (p < 0.001), but each virus was completely cleared by 9 d postinfection.
RSV epitope-specific responses have different abilities to compensate for lost or altered epitopes
RSV epitope-specific CD8+ T cell responses for KdM282–90, DbM187–191, as well as the minor KdM2127–135 epitope, were measured in the lungs between 4 and 14 d postprimary infection in mice infected with RSVwt, RSV-M2I90T, and RSV-MN191S. As previously reported (18), RSVwt infection resulted in a strongly KdM282–90 dominated response, a 4-fold lower response to the DbM187–195 epitope, and near-baseline response to the KdM2127– 135 epitope (Fig. 2A). Mice infected with RSV with the dominant epitope mutated, RSV-M2I90T, demonstrated a 10-fold reduction in the response to the KdM282–90 epitope. Of the epitopes tested in this experiment, the DbM187–195 epitope dominated the CD8+ T cell response in RSV-M2I90T mice, with a significantly (p < 0.05) higher response to this epitope than in mice infected with RSVwt. There was no detectable increase in the KdM2127–135-specific CD8+ T cell in response to the change in KdM282–90 (Fig. 2A). Finally, mice infected with RSV-MN191S completely lacked a response to the DbM187–195 epitope. Although the minor KdM2127–135 response did not compensate for the loss of the DbM187–195 epitope, the KdM282–90 response compensated significantly (p < 0.05).
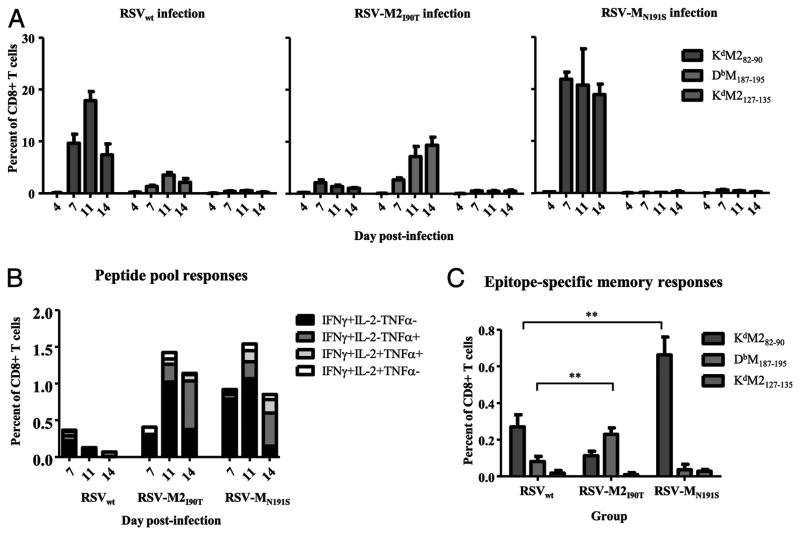
Figure 2.
RSV epitope-specific CD8+ T cell responses and memory in mice infected with RSVwt, RSV-M2I90T, or RSV-MN191S. A, Tetramer-positive cells specific for KdM282–90, DbM187–195, and KdM2127–135 following infection with RSVwt, RSV-M2I90T, and RSV-MN191S. Lymphocytes were isolated from the lungs of infected CB6F1, and stained with tetramers and surface phenotype Abs. Percentages of CD3+CD8+ T cells staining with tetramer are shown. B, Intracellular cytokine responses to a pool of minor epitope peptides (F85–93, F250–258, F433–442, N57–64, and N360–368) in the lungs following infection with RSVwt, RSV-M2I90T, and RSV-MN191S. C, Epitope-specific memory responses in the spleen of mice infected 100 d earlier with RSVwt, RSV-M2I90T, and RSV-MN191S as determined by staining with tetramer and surface phenotype Abs. **p < 0.01. Data are representative of two to three experiments done with four to five mice per group and error bars represent the SEM.
To evaluate the extent of compensation by several nearly background CD8+ T cell responses during primary RSV infection, peptides corresponding to five additional epitopes (F85–93, F250–258, F433–442, N57–64, and N360–368) were pooled and used to stimulate lung CD8+ T cells from infected mice. As measured by cytokine (IFN-γ, TNF-α, and IL-2) production following stimulation, these five epitopes together account for <0.5% of the CD8+ T cell response in the lungs of RSVwt infected CB6F1 mice (Fig. 2B). Following infection with RSV-M2I90T or RSV-MN191S, the response to this combination of epitopes peaked at 1.5% of lung-resident CD8+ T cells 11 d postinfection, indicating only slight compensation by one or more peptides within the pool.
Epitope dominance patterns established during primary infection with RSVwt, RSV-M2I90T, and RSV-MN191S persisted into the memory phase (Fig. 2C). Mice infected with RSV-M2I90T had lower CD8+ T cell memory responses to KdM282–90, and significantly higher (p < 0.01) responses to DbM187–195 in the spleen than mice infected with RSVwt. Conversely, CB6F1 infected with RSV-MN191S had a significantly higher (p < 0.01) response to KdM282–90 and no detectable memory response to DbM187–195. Responses to KdM2127–135 were not significantly different between groups of mice infected with the three different viruses.
Quantitative changes in CD8+ T cell responses following mutant virus infection occur with or without qualitative changes
We compared the CD8+ T cell quantity (as measured by tetramer) to the quality of KdM282–90 and DbM187–195 specific responses (capacity to produce cytokines upon stimulation) in the lungs of infected mice. In vitro peptide stimulation can result in down-regulation of the TCR, so parallel samples from the same mouse lungs were stained separately for tetramer or cytokine production after stimulation. As we and others have previously reported (18, 32), the dominant KdM282–90 response has a large disparity between quantity and quality: less than half of the CD8+ T cells recovered from the lungs of mice following RSVwt infection that are specific for this epitope produced cytokine upon stimulation in vitro with the M282–90 peptide (Fig. 3A). Although CD8+ T cells from the lungs of mice infected with RSV-M2I90T contain 10-fold fewer cells specific for the KdM282–90 epitope, these cells were highly functional, and all produced cytokine after stimulation with the M282–90 peptide (Fig. 3A). A side-by-side comparison of Kd M282–90 responses following infection with RSVwt or RSV-M2I90T is presented in Supplemental Fig. 1. The Vβ profile of epitope-specific cells is similar between mice infected with either virus, suggesting that cells responding to the mutant epitope are a subset of those that respond to the wt epitope. Stimulation with either the native M282–90 peptide, or the M2I90T peptide (SYIGSINNT) following infection with either RSVwt or RSV-M2I90T results in expression of IFN-γ by cells with an identical Vβ distribution, indicating that both peptides stimulate the same population of cells (Supplemental Fig. 1). These data are consistent with an alteration in the anchor residue with no changes in the TCR contact residues, and the reported 10-fold lower binding affinity to H2-Kd associated with this mutation (31). Finally, infection with RSV-MN191S resulted in an increased KdM282–90 response, yet as in infection with RSVwt, only half of the cells produced cytokine upon stimulation (Fig. 3A), indicating that the compensation was only in magnitude and not quality of the response. Dividing the T cell quality by the quantity for the KdM282–90 epitope at all timepoints combined quantifies the proportion of epitope-specific cells capable of producing cytokines. Using this method, it is clear that similar proportions of KdM282–90 cells produce cytokine in the RSVwt and RSV-MN191S–infected groups, and those in RSV-M2I90T–infected mice are more highly functional (Fig. 3B). Cells in this final group were also found to produce more cytokine per cell, as reflected by measuring the median fluorescence intensity (MFI) for IFNγ in producing cells (p < 0.0001, Fig. 3C). The basis for the improved quality of the response is under investigation.
Figure 3.
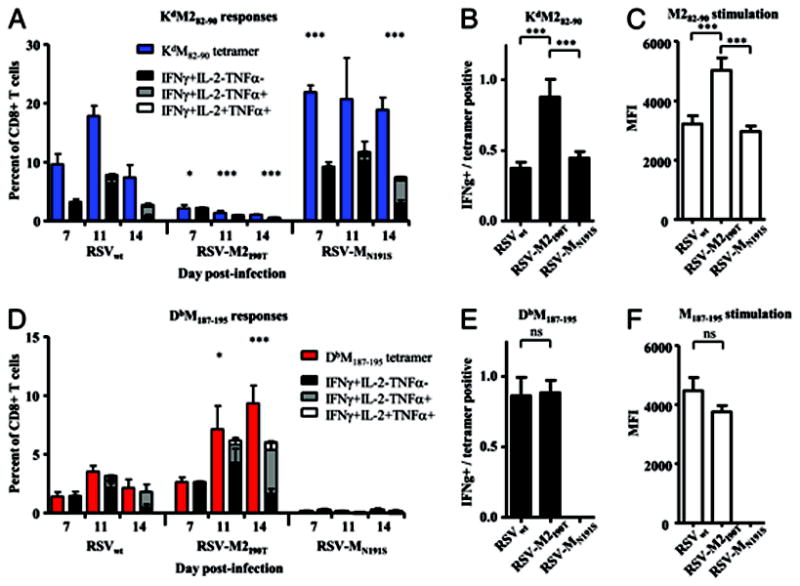
Quantity versus quality of RSVepitope-specific CD8+ T cell responses in mice infected with RSVwt, RSV-M2I90T, or RSV-MN191S. A, Frequency and cytokine production by KdM282–90-specific CD8+ T cells in the lung following infection with RSVwt, RSV-M2I90T, or RSV-MN191S. Parallel samples were stained with tetramer and incubated with M282–90 peptide for 5 h in the presence of the transport inhibitor monensin. B, Fraction of KdM282–90-specific cells capable of producing cytokine following M282–90 peptide stimulation. C, MFI of IFN-γ–positive cells following peptide stimulation with M282–90 following group gating on cells producing IFN-γ. D, Frequency and cytokine production by DbM187–195 epitope-specific CD8+ T cells following infection. E, Fraction of DbM187–195-specific cells capable of producing cytokine following M187–195 peptide stimulation. F, MFI of IFN-γ–positive cells following peptide stimulation with M187–195. *p < 0.05 compared with RSVwt; ***p < 0.001 compared with RSVwt. Data are representative of two experiments with four to five mice/group and error bars represent the SEM. ns, no significance.
DbM187–195-specific responses were similarly analyzed in mice infected with RSVwt and RSV-M2I90T. Cells specific for this epi-tope were undetectable in mice infected with RSV-MN191S, and the mutant peptide (NAITSAKII) did not stimulate any production of IFN-γ following in vitro stimulation of RSV-MN191S–infected mice. The altered peptide was, however, able to stimulate the DbM187–195 specific cells following RSVwt infection (data not shown). There were more CD8+ T cells specific for DbM187–195 in mice infected with RSV-M2I90T compared with RSVwt, and most of these cells produced cytokine following stimulation, as observed following infection with RSVwt (Fig. 3D). Although the proportion of IFN-γ–producing cells was slightly reduced at later time points, the proportion of DbM187–195-specific cells from RSV-M2I90T–infected mice that expressed cytokine was similar to that of RSVwt, (Fig. 3E). Between the two groups, there was no significant difference in MFI (Fig. 3F). Overall, more DbM187–195-specific cells were double positive for production of both IFN-γ and TNF-α, than were KdM282–90 cells, which tend to produce IFN-γ only (Fig. 3D versus 3A).
We measured the ability of KdM282–90 and DbM187–195-specific cells to kill peptide-pulsed autologous primary lymphocytes as targets with an in vivo CTL assay. Peptide pulsed cells were labeled with high concentrations of CFSE (M282–90) and CMTMR (M187–195) prior to i.v. injection into mice that had been infected 7 d earlier. Fifteen hours later, cells were harvested from the lungs and spleen and the proportion of cells that were killed was quantified by comparison with coinjected cells labeled with low concentrations of CFSE and CMTMR that were not pulsed with peptide. In both the lung and the spleen of RSVwt-infected mice, more M282–90-pulsed cells were killed than M187–195-pulsed, with virtually all of the M282–90-pulsed cells killed by 15 h post-injection (Fig. 4A). This suggests that an excess of KdM282–90-specific cells can sufficiently kill all the transferred targets, or that the discordance in tetramer binding and cytokine production may not be associated with a defect in cytolytic activity. Interestingly, in mice infected with RSV-M2I90T, more M282–90-pulsed targets were killed than M187–195 pulsed in the lungs (p < 0.001); however, nearly equal proportions of both targets were killed in the spleen. These data confirm high functionality of the remaining KdM282–90-specific cells in the lungs of mice infected with RSV-M2I90T. Finally, nearly all M282–90-pulsed cells were killed in both the lungs and spleen of RSV-MN191S–infected mice, whereas all cells pulsed with M187–195 remained (Fig. 4A), consistent with the near-absence of DbM187–195-specific CD8+ T cells (Fig. 2A).
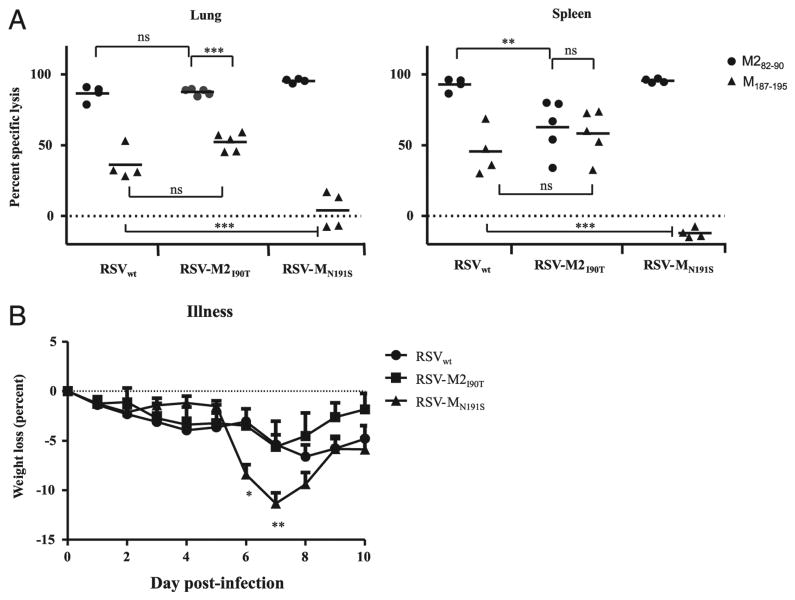
Figure 4.
In vivo cytotoxicity and illness in mice infected with RSVwt, RSV-M2I90T, or RSV-MN191S. A, Specific lysis of peptide-pulsed target cells fifteen hours after i.v. transfer into mice infected with RSVwt, RSV-M2I90T, and RSV-MN191S. Percent specific lysis of cells pulsed with M282–90 (circle) or M187–195 (triangle) were calculated by comparison with labeled cells not pulsed with peptide. Cells recovered from naive mice injected with all four cell populations were used to calculate input. **p < 0.01; ***p < 0.001. ns, no significance. B, Illness in mice infected with RSVwt, RSV-M2I90T, and RSV-MN191S was evaluated by weighing mice daily and comparing to their weight at the time of infection (day 0). *p < 0.05; **p < 0.01.
Increased illness/immunopathology results from overcompensation by a dominant RSV epitope
Immunopathology in the mouse model of primary RSV infection can be measured by weight loss. Illness caused by the CD8+ T cell response peaks at 7–8 d postinfection. Mice infected with RSVwt experienced a loss of 6.6% of their body weight by day 8, after which they recovered (Fig. 4B). Mice infected with RSV-MN191S experienced more dramatic weight loss earlier than those infected with RSVwt, losing almost double (11.3%) the weight lost by mice infected with RSVwt by 7 d postinfection (p < 0.05). Although not statistically significant, RSV-M2I90T infected mice tended to lose less weight than mice infected with RSVwt, and began their recovery 1 d sooner. This suggests that the subdominant T cell responses make a significant contribution to viral clearance without exacerbating illness.
Discussion
Various studies reporting mutations in epitope-specific CD8+ T cell responses within a virus have reported either little to no compensation by other CD8+ responses (30, 33–35), or more significant compensation by one or multiple epitopes (36, 37). Some report little compensation during primary infection, but a greater amount during secondary infection (33, 34). The ability of epitopes to compensate for the loss of others has been shown to have an effect on the ability to control viral pathogens (30, 37). We demonstrate in this study that changes of even a single amino acid can abolish specific CD8+ T cell responses to RSV during primary infection of CB6F1 mice, alter immunodominance hierarchy and illness, and change the functional properties of the responding T cell population.
In these studies, we saw compensation by other epitopes following mutation of either the dominant KdM282–90 or the sub-dominant DbM187–195 response. In the case of mutation of the KdM282–90 (RSV-M2I90T), which resulted in one log10 reduction in this response, the next dominant DbM187–195 epitope provided the most compensation, with only modest compensation by a pool of subdominant responses. Following mutation of the subdominant DbM187–195 response (RSV-MN191S), which essentially ablated that response, we again found modest compensation by the sub-dominant pool, and “overcompensation” by the already dominant KdM282–90 response. These data clearly show that the subdominant DbM187–195 response exerts some level of control over the dominant KdM282–90 response, which is of benefit to the host. This may account for the observation that CB6F1 hybrid mice, which recognize a greater number of subdominant viral determinants, experience more mild disease following infection than the BALB/c parent strain, which has an almost exclusively KdM282–90-specific CD8 T cell response (18).
In contrast to work by Vallbracht et al. (30), we saw no compensation by the subdominant KdM2127–135 epitope postinfection with either RSV-M2I90T or RSV-MN191S. They mutated the KdM282–90 epitope at position 8 (SYIGSINNI → SYIGSINAI), a mutation in the TCR binding region predicted to affect TCR recognition rather than MHC binding, and saw a complete abolition of the response. Following infection with this virus, they found that the KdF85–93 epitope did not compensate at all, but saw a small increase in the response to the KdM2127–135 epitope and no measurable responses to previously undetected epitopes. Similarly, Mok et al. (31) saw compensation by the KdM2127–135 epi-tope in the context of multiple rounds of DNA immunization with a plasmid expressing the M2 protein with a mutation in both anchor residues of the KdM282–90 epitope that abolished the response entirely prior to infection with RSV. Both of these studies were done in BALB/c mice, where the CD8+ response was limited to responses restricted to d-allele MHC proteins. This demonstrates that the factors defining the ability of a particular epitope to respond and compensate may differ by mouse strain, and the presence or absence of other MHC molecules. It is possible in our study, that the combined responses to the DbM187–195 and mutated KdM282–90 following RSV-M2I90T infection, and the overly dominant responses to the KdM282–90 during RSV-MN191S infection sufficiently immunodominate the KdM2127–135 epitope during infection with either of these viruses and that the response to this epitope is dispensable.
Although one postulated mechanism for immunodomination is the negative effect of production of IFN-γ by dominant epitopes on the subdominant (38), several studies have proven that the outcome of infection after epitope mutation is not easy to predict, and compensation does not always occur by the “next best” epitope (33–35). Responses to some epitopes appear to be more inherently self-limited than others and can only be expanded to a certain extent, whereas minor epitopes previously below the level of detection, or “weak” subdominant responses may arise in some cases (39, 40). Although efforts that extended beyond measuring already defined epitopes within RSV were not taken, we believe that there is a low likelihood for the emergence of a new strong response to an undescribed epitope based on both the lack of illness in the RSV-M2I90T–infected group of mice and the strong reciprocal compensation of the two major CD8+ T cell responses.
The mechanism for the enhanced function of the remaining KdM282–90 response in mice infected with RSV-M2I90T is unknown. Despite a 10-fold reduction in numbers, these cells are functionally superior to KdM282–90-specific cells in an infection with RSVwt in both their frequency of cytokine production and the amount of cytokine they produce (Fig. 3B, 3C). We can correlate this increase in function with a strong ability to kill cells that present the M282–90 peptide in vivo in these studies, as M282–90-pulsed cells were as readily, or more readily killed in the spleen and lungs of RSV-M2I90T–infected mice than cells pulsed with the M187–195 peptide (Fig. 4A). Clonotyping and other analysis of this response is a subject of ongoing investigation.
Several studies suggest that responses to subdominant epitopes are as effective, or more effective, than responses targeting immunodominant epitopes. As one example, dominant responses against the hepatitis B surface Ag severely limit the diversity of the antiviral response. Upon elimination of immunodominant epitopes, subdominant responses were found to have striking antiviral potential (39). In the influenza mouse model system, immunodominant epitopes like the DbPA224–233 have been found to have poor protective efficacy due in part to aspects of Ag presentation following infection (41). Strong responses to this epitope can actually delay viral clearance. Other epitopes of influenza have demonstrated a similar inability to clear virus following epitope-specific immunization (42). It has also been shown that sub-dominant epitopes are responsible for durable control of SIV-mac239 replication in a rhesus macaque model of HIV-1 (43). Responses can be generated against subdominant epitopes even in the context of ongoing infection and are potentially beneficial in controlling disease (39, 44).
The development of narrowly focused, strongly immunodominant responses, which inhibit the response to subdominant epitopes, may diminish effective control of the pathogen depending on the epitope. Certainly, they are of limited use if the virus adapts to abrogate responses to one or two immunodominant epitopes, as would be likely to occur in more persistent viral infections. We demonstrate in this study that an overall lower CD8+ T cell response, with more codominance between the normally subdominant DbM187–195 and the mutant KdM282–90 epitope shows benefit to the host by clearing virus with minimal illness. Following viral infection in vivo, multiple subdominant epitopes working together toward viral clearance that exert pressure on a sufficient number of viral determinants may be most favorable for the host. This strategy to avoid immunodomination would increase immunological flexibility, reduce the risk of escape, and potentially diminish immunopathology.
Designing vaccines that elicit codominant CD8+ T cell responses is a strategy that should be considered for some viral pathogens. Achieving optimal vaccination will require a greater understanding of what constitutes a protective epitope, the role of immunodominance and immunodomination on final outcome, and the basis for CD8 T cell-mediated immunopathology. We have shown in this study that mutation of an immunodominant epitope, which dampens the magnitude of response, diminishes immunodomination, and increases its functionality in vivo, may result in a more efficient CTL response that can clear virus with less immunopathology. Alternatively, eliminating a subdominant epitope may increase dominance of an already dominant epitope, resulting in enhanced CD8+ mediated immunopathology. Defining the properties of epi-topes that produce unfavorable, immunodominating responses that have poor killing efficiency and their counterpart responses that can efficiently clear virus may be necessary to fully exploit T cell-based vaccine approaches. In addition, this study cautions that simple enumeration of vaccine-induced T cell responses may not be a reliable surrogate for vaccine efficacy.
In summary, compensation for mutated CD8+ T cell epitopes is a complex phenomenon. Defining factors that determine the capacity for individual epitopes to compensate, as well as those that confer increases in functionality, will be valuable for the design of immunogens that promote effective responses without the potential for deleterious effects.
Acknowledgments
This work was supported by the National Institute of Allergy and Infectious Disease Intramural Research Program.
Abbreviations
- CMTMR
chloromethylbenzoylaminotetramethylrhodamine
- EMEM
Eagle's MEM
- ICS
intracellular cytokine staining
- MFI
median fluorescence intensity
- RSV
respiratory syncytial virus
- wt
wild-type
Footnotes
The online version of this article contains supplemental material.
Disclosures: The authors have no financial conflicts of interest.
References
- 1.Zinkernagel RM, Doherty PC. Restriction of in vitro T cell-mediated cytotoxicity in lymphocytic choriomeningitis within a syngeneic or semiallogeneic system. Nature. 1974;248:701–702. doi: 10.1038/248701a0. [DOI] [PubMed] [Google Scholar]
- 2.Chen W, Antón LC, Bennink JR, Yewdell JW. Dissecting the multifactorial causes of immunodominance in class I-restricted T cell responses to viruses. Immunity. 2000;12:83–93. doi: 10.1016/s1074-7613(00)80161-2. [DOI] [PubMed] [Google Scholar]
- 3.Kedl RM, Kappler JW, Marrack P. Epitope dominance, competition and T cell affinity maturation. Curr Opin Immunol. 2003;15:120–127. doi: 10.1016/s0952-7915(02)00009-2. [DOI] [PubMed] [Google Scholar]
- 4.Yewdell JW, Bennink JR. Immunodominance in major histocompatibility complex class I-restricted T lymphocyte responses. Annu Rev Immunol. 1999;17:51–88. doi: 10.1146/annurev.immunol.17.1.51. [DOI] [PubMed] [Google Scholar]
- 5.Yewdell JW, Del Val M. Immunodominance in TCD8+ responses to viruses: cell biology, cellular immunology, and mathematical models. Immunity. 2004;21:149–153. doi: 10.1016/j.immuni.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 6.Chen W, Pang K, Masterman KA, Kennedy G, Basta S, Dimopoulos N, Hornung F, Smyth M, Bennink JR, Yewdell JW. Reversal in the immunodominance hierarchy in secondary CD8+ T cell responses to influenza A virus: roles for cross-presentation and lysis-independent immunodomination. J Immunol. 2004;173:5021–5027. doi: 10.4049/jimmunol.173.8.5021. [DOI] [PubMed] [Google Scholar]
- 7.Crowe SR, Turner SJ, Miller SC, Roberts AD, Rappolo RA, Doherty PC, Ely KH, Woodland DL. Differential antigen presentation regulates the changing patterns of CD8+ T cell immunodominance in primary and secondary influenza virus infections. J Exp Med. 2003;198:399–410. doi: 10.1084/jem.20022151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flesch IE, Woo WP, Wang Y, Panchanathan V, Wong YC, La Gruta NL, Cukalac T, Tscharke DC. Altered CD8(+) T cell immunodominance after vaccinia virus infection and the naive repertoire in inbred and F(1) mice. J Immunol. 2010;184:45–55. doi: 10.4049/jimmunol.0900999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.La Gruta NL, Kedzierska K, Pang K, Webby R, Davenport M, Chen W, Turner SJ, Doherty PC. A virus-specific CD8+ T cell immunodominance hierarchy determined by antigen dose and precursor frequencies. Proc Natl Acad Sci USA. 2006;103:994–999. doi: 10.1073/pnas.0510429103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heymann PW, Carper HT, Murphy DD, Platts-Mills TA, Patrie J, McLaughlin AP, Erwin EA, Shaker MS, Hellems M, Peerzada J, et al. Viral infections in relation to age, atopy, and season of admission among children hospitalized for wheezing. J Allergy Clin Immunol. 2004;114:239–247. doi: 10.1016/j.jaci.2004.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Welliver TP, Garofalo RP, Hosakote Y, Hintz KH, Avendano L, Sanchez K, Velozo L, Jafri H, Chavez-Bueno S, Ogra PL, et al. Severe human lower respiratory tract illness caused by respiratory syncytial virus and influenza virus is characterized by the absence of pulmonary cytotoxic lymphocyte responses. J Infect Dis. 2007;195:1126–1136. doi: 10.1086/512615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Welliver TP, Reed JL, Welliver RC., Sr Respiratory syncytial virus and influenza virus infections: observations from tissues of fatal infant cases. Pediatr Infect Dis J. 2008;27(10, Suppl):S92–S96. doi: 10.1097/INF.0b013e318168b706. [DOI] [PubMed] [Google Scholar]
- 13.Johnson JE, Gonzales RA, Olson SJ, Wright PF, Graham BS. The histopathology of fatal untreated human respiratory syncytial virus infection. Mod Pathol. 2007;20:108–119. doi: 10.1038/modpathol.3800725. [DOI] [PubMed] [Google Scholar]
- 14.Heidema J, Lukens MV, van Maren WW, van Dijk ME, Otten HG, van Vught AJ, van der Werff DB, van Gestel SJ, Semple MG, Smyth RL, et al. CD8+ T cell responses in bronchoalveolar lavage fluid and peripheral blood mononuclear cells of infants with severe primary respiratory syncytial virus infections. J Immunol. 2007;179:8410–8417. doi: 10.4049/jimmunol.179.12.8410. [DOI] [PubMed] [Google Scholar]
- 15.Lukens MV, van de Pol AC, Coenjaerts FE, Jansen NJ, Kamp VM, Kimpen JL, Rossen JW, Ulfman LH, Tacke CE, Viveen MC, et al. A systemic neutrophil response precedes robust CD8(+) T-cell activation during natural respiratory syncytial virus infection in infants. J Virol. 2010;84:2374–2383. doi: 10.1128/JVI.01807-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Olson MR, Hartwig SM, Varga SM. The number of respiratory syncytial virus (RSV)-specific memory CD8 T cells in the lung is critical for their ability to inhibit RSV vaccine-enhanced pulmonary eosinophilia. J Immunol. 2008;181:7958–7968. doi: 10.4049/jimmunol.181.11.7958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Graham BS, Bunton LA, Wright PF, Karzon DT. Role of T lymphocyte subsets in the pathogenesis of primary infection and rechallenge with respiratory syncytial virus in mice. J Clin Invest. 1991;88:1026–1033. doi: 10.1172/JCI115362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rutigliano JA, Ruckwardt TJ, Martin JE, Graham BS. Relative dominance of epitope-specific CD8+ T cell responses in an F1 hybrid mouse model of respiratory syncytial virus infection. Virology. 2007;362:314–319. doi: 10.1016/j.virol.2006.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Collins PL, Hill MG, Camargo E, Grosfeld H, Chanock RM, Murphy BR. Production of infectious human respiratory syncytial virus from cloned cDNA confirms an essential role for the transcription elongation factor from the 59 proximal open reading frame of the M2 mRNA in gene expression and provides a capability for vaccine development. Proc Natl Acad Sci USA. 1995;92:11563–11567. doi: 10.1073/pnas.92.25.11563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bukreyev A, Belyakov IM, Berzofsky JA, Murphy BR, Collins PL. Granulocyte-macrophage colony-stimulating factor expressed by recombinant respiratory syncytial virus attenuates viral replication and increases the level of pulmonary antigen-presenting cells. J Virol. 2001;75:12128–12140. doi: 10.1128/JVI.75.24.12128-12140.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luongo C, Yang L, Winter CC, Spann KM, Murphy BR, Collins PL, Buchholz UJ. Codon stabilization analysis of the “248” temperature sensitive mutation for increased phenotypic stability of respiratory syncytial virus vaccine candidates. Vaccine. 2009;27:5667–5676. doi: 10.1016/j.vaccine.2009.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Graham BS, Perkins MD, Wright PF, Karzon DT. Primary respiratory syncytial virus infection in mice. J Med Virol. 1988;26:153–162. doi: 10.1002/jmv.1890260207. [DOI] [PubMed] [Google Scholar]
- 23.Chang J, Srikiatkhachorn A, Braciale TJ. Visualization and characterization of respiratory syncytial virus F-specific CD8(+) T cells during experimental virus infection. J Immunol. 2001;167:4254–4260. doi: 10.4049/jimmunol.167.8.4254. [DOI] [PubMed] [Google Scholar]
- 24.Jiang S, Borthwick NJ, Morrison P, Gao GF, Steward MW. Virus-specific CTL responses induced by an H-2K(d)-restricted, motif-negative 15-mer peptide from the fusion protein of respiratory syncytial virus. J Gen Virol. 2002;83:429–438. doi: 10.1099/0022-1317-83-2-429. [DOI] [PubMed] [Google Scholar]
- 25.Johnstone C, de León P, Medina F, Melero JA, García-Barreno B, Del Val M. Shifting immunodominance pattern of two cytotoxic T-lymphocyte epitopes in the F glycoprotein of the Long strain of respiratory syncytial virus. J Gen Virol. 2004;85:3229–3238. doi: 10.1099/vir.0.80219-0. [DOI] [PubMed] [Google Scholar]
- 26.Kulkarni AB, Collins PL, Bacik I, Yewdell JW, Bennink JR, Crowe JE, Jr, Murphy BR. Cytotoxic T cells specific for a single peptide on the M2 protein of respiratory syncytial virus are the sole mediators of resistance induced by immunization with M2 encoded by a recombinant vaccinia virus. J Virol. 1995;69:1261–1264. doi: 10.1128/jvi.69.2.1261-1264.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee S, Miller SA, Wright DW, Rock MT, Crowe JE., Jr Tissue-specific regulation of CD8+ T-lymphocyte immunodominance in respiratory syncytial virus infection. J Virol. 2007;81:2349–2358. doi: 10.1128/JVI.01910-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lukens MV, Claassen EA, de Graaff PM, van Dijk ME, Hoogerhout P, Toebes M, Schumacher TN, van der Most RG, Kimpen JL, van Bleek GM. Characterization of the CD8+ T cell responses directed against respiratory syncytial virus during primary and secondary infection in C57BL/6 mice. Virology. 2006;352:157–168. doi: 10.1016/j.virol.2006.04.023. [DOI] [PubMed] [Google Scholar]
- 29.Rutigliano JA, Rock MT, Johnson AK, Crowe JE, Jr, Graham BS. Identification of an H-2D(b)-restricted CD8+ cytotoxic T lymphocyte epitope in the matrix protein of respiratory syncytial virus. Virology. 2005;337:335–343. doi: 10.1016/j.virol.2005.04.032. [DOI] [PubMed] [Google Scholar]
- 30.Vallbracht S, Jessen B, Mrusek S, Enders A, Collins PL, Ehl S, Krempl CD. Influence of a single viral epitope on T cell response and disease after infection of mice with respiratory syncytial virus. J Immunol. 2007;179:8264–8273. doi: 10.4049/jimmunol.179.12.8264. [DOI] [PubMed] [Google Scholar]
- 31.Mok H, Lee S, Wright DW, Crowe JE., Jr Enhancement of the CD8+ T cell response to a subdominant epitope of respiratory syncytial virus by deletion of an immunodominant epitope. Vaccine. 2008;26:4775–4782. doi: 10.1016/j.vaccine.2008.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chang J, Braciale TJ. Respiratory syncytial virus infection suppresses lung CD8+ T-cell effector activity and peripheral CD8+ T-cell memory in the respiratory tract. Nat Med. 2002;8:54–60. doi: 10.1038/nm0102-54. [DOI] [PubMed] [Google Scholar]
- 33.Andreansky SS, Stambas J, Thomas PG, Xie W, Webby RJ, Doherty PC. Consequences of immunodominant epitope deletion for minor influenza virus-specific CD8+-T-cell responses. J Virol. 2005;79:4329–4339. doi: 10.1128/JVI.79.7.4329-4339.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thomas PG, Brown SA, Keating R, Yue W, Morris MY, So J, Webby RJ, Doherty PC. Hidden epitopes emerge in secondary influenza virus-specific CD8+ T cell responses. J Immunol. 2007;178:3091–3098. doi: 10.4049/jimmunol.178.5.3091. [DOI] [PubMed] [Google Scholar]
- 35.Webby RJ, Andreansky S, Stambas J, Rehg JE, Webster RG, Doherty PC, Turner SJ. Protection and compensation in the influenza virus-specific CD8+ T cell response. Proc Natl Acad Sci USA. 2003;100:7235–7240. doi: 10.1073/pnas.1232449100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gallimore A, Hombach J, Dumrese T, Rammensee HG, Zinkernagel RM, Hengartner H. A protective cytotoxic T cell response to a sub-dominant epitope is influenced by the stability of the MHC class I/peptide complex and the overall spectrum of viral peptides generated within infected cells. Eur J Immunol. 1998;28:3301–3311. doi: 10.1002/(SICI)1521-4141(199810)28:10<3301::AID-IMMU3301>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 37.Weidt G, Utermöhlen O, Heukeshoven J, Lehmann-Grube F, Deppert W. Relationship among immunodominance of single CD8+ T cell epitopes, virus load, and kinetics of primary antiviral CTL response. J Immunol. 1998;160:2923–2931. [PubMed] [Google Scholar]
- 38.Rodriguez F, Harkins S, Slifka MK, Whitton JL. Immunodominance in virus-induced CD8(+) T-cell responses is dramatically modified by DNA immunization and is regulated by gamma interferon. J Virol. 2002;76:4251–4259. doi: 10.1128/JVI.76.9.4251-4259.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Riedl P, Wieland A, Lamberth K, Buus S, Lemonnier F, Reifenberg K, Reimann J, Schirmbeck R. Elimination of immunodominant epitopes from multispecific DNA-based vaccines allows induction of CD8 T cells that have a striking antiviral potential. J Immunol. 2009;183:370–380. doi: 10.4049/jimmunol.0900505. [DOI] [PubMed] [Google Scholar]
- 40.Wieland A, Riedl P, Reimann J, Schirmbeck R. Silencing an immunodominant epitope of hepatitis B surface antigen reveals an alternative repertoire of CD8 T cell epitopes of this viral antigen. Vaccine. 2009;28:114–119. doi: 10.1016/j.vaccine.2009.09.096. [DOI] [PubMed] [Google Scholar]
- 41.Crowe SR, Miller SC, Shenyo RM, Woodland DL. Vaccination with an acidic polymerase epitope of influenza virus elicits a potent antiviral T cell response but delayed clearance of an influenza virus challenge. J Immunol. 2005;174:696–701. doi: 10.4049/jimmunol.174.2.696. [DOI] [PubMed] [Google Scholar]
- 42.Crowe SR, Miller SC, Woodland DL. Identification of protective and non-protective T cell epitopes in influenza. Vaccine. 2006;24:452–456. doi: 10.1016/j.vaccine.2005.07.090. [DOI] [PubMed] [Google Scholar]
- 43.Friedrich TC, Valentine LE, Yant LJ, Rakasz EG, Piaskowski SM, Furlott JR, Weisgrau KL, Burwitz B, May GE, León EJ, et al. Subdominant CD8+ T-cell responses are involved in durable control of AIDS virus replication. J Virol. 2007;81:3465–3476. doi: 10.1128/JVI.02392-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kloverpris H, Karlsson I, Bonde J, Thorn M, Vinner L, Pedersen AE, Hentze JL, Andresen BS, Svane IM, Gerstoft J, et al. Induction of novel CD8+ T-cell responses during chronic untreated HIV-1 infection by immunization with subdominant cytotoxic T-lymphocyte epitopes. AIDS. 2009;23:1329–1340. doi: 10.1097/QAD.0b013e32832d9b00. [DOI] [PubMed] [Google Scholar]