Abstract
Generalized linear models were used to assess the relationship between religious attendance and lifetime smoking status among middle-aged adults (n = 666) sampled from waves three (1993 to 1996) and four (2004 to 2005) of the Baltimore Epidemiologic Catchment Area (ECA) study. Religious attendance once per week or greater as compared to never was inversely associated with smoking status. Future research should explore potential mediating factors of the association between religious attendance and smoking among middle-aged adults in order to gain a greater understanding of the mechanisms underlying this relationship. Funding: NIMH grant DA026652; NIDA grant T32DA007292.
Keywords: religious attendance, smoking, tobacco, baltimore ECA, middle-aged, urban
INTRODUCTION
Cigarette smoking is the leading cause of preventable death in the United States (Danaei et al., 2009; Mokdad, Marks, Stroup, & Gerberding 2004), leading to approximately 443,000 premature deaths per year. This translates to nearly 20% of deaths nationally (Centers for Disease Control and Prevention, 2008). By 2030, worldwide tobacco attributable deaths are projected to reach a high of 8.3 million, and by 2015 kill 50% more people than HIV/AIDS, and account for 10% of all deaths globally (Mathers & Loncar, 2006). Given the high mortality rates associated with tobacco use, it is critical that protective factors are identified in order to circumvent risk associated with smoking.
Religious attendance [a facet of religious orientation that contributes to a general frame of reference from which life can be understood (Pargament & Brant, 1998)] and other facets of religiousness have been associated with smoking cessation in several studies. According to a review by Koenig and colleagues (2012), at least 125 studies examining the association of religiousness and spirituality with tobacco use were published between 2000 and 2010. However, the majority of these studies focused on youth and young adults (Koenig, King, & Carson, 2012), and showed that religiousness and spirituality were protective against smoking (Koenig, 2011). For example, among high school students, religious attendance, and religious importance (e.g., the perceived importance of religion in one’s life) were significantly and inversely associated with tobacco use, such that higher frequencies of attendance and importance were associated with higher odds of abstaining from tobacco use (Wallace Jr, Brown, Bachman, & Laveist, 2003). Another study demonstrated that among 7th to 10th grade students, higher self-ratings of religious importance were inversely related to tobacco, alcohol, and marijuana use, and buffered the impact of life stress on substance use (Wills, Yaeger, & Sandy, 2003). Similar benefits have been demonstrated among young adults. In one study, religious affiliation, higher levels of participation in organized religious activities (e.g., religious attendance, and bible study), and higher levels of self-rated religiousness were associated with a lower likelihood of smoking initiation (Timberlake et al., 2006). Similarly, in another study focused on young adults, Whooley and colleagues (2002), found an inverse relationship between religious attendance, current smoking, and smoking initiation.
Relative to studies among youth and young adults, fewer studies have focused on the relationship between religiousness and smoking among urban, middle-aged adults in the United States. Exceptions include findings from Nollen and colleagues (2005), which suggest that religious practices, beliefs, and values were not associated with smoking cessation among African American smokers. However, in contrast, among a sample of predominately white, urban adult smokers, weekly religious attendance was significantly associated with quitting smoking over time (Strawbridge, Shema, Cohen, & Kaplan, 2001). However, these studies are potentially limited by having racially homogenous samples, therefore further research on middle-aged urban populations is warranted. Furthermore, it is not uncommon for middle-aged Americans to experience job instability (US Bureau of Labor Statistics, 2010) and job loss (Dupre, George, Liu, & Peterson, 2012) during this stage of life, which can be concerning when considering the linkages between stress, poverty, and smoking that have been documented (Perettti-Watel & Constance, 2009; Shuaib et al., 2011). Given the socioeconomic challenges faced by many middle-aged Americans, coupled with the potential for increased exposure to environmental cues to smoke such as high concentrations of tobacco outlets (Peterson et al., 2011; Rodriguez, Carlos, Adachi-Mejia, Berke, & Sargent, 2012; Yu, Peterson, Sheffer, Reidm, & Schnieder, 2010) and tobacco advertising (Johns, Sacks, Rane, & Kansagra, 2013) in urban settings, identifying factors that protect against tobacco use among urban middle-aged persons is warranted. The purpose of the current study is to examine the influence of religious attendance on smoking status over time among a diverse sample of middle-aged lifetime smokers who reside in an urban setting. Based on previous literature suggesting that facets of religiousness may be protective against tobacco use, we hypothesized that higher frequencies of religious attendance, as compared to no attendance, would be associated with smoking cessation in this population.
METHODS
Data Source
Participants were sampled from the Baltimore Epidemiologic Catchment Area (ECA) Study. The Baltimore ECA study is a longitudinal, community-based cohort study, conducted from 1981 to 2005. The Baltimore ECA study is part of the larger, multisite ECA program commissioned by the National Institute of Mental Health (NIMH) to estimate the incidence and prevalence of mental health disorders in a community sample according to the Diagnostic Interview Schedule (DIS), and the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, 3rd Edition criteria (Eaton, Regier, Locke, & Taube, 1981; Regier et al., 1984). The NIMH ECA program includes five sites across the United States—St. Louis, Missouri; Los Angeles, California; Hartford, Connecticut; Durham, North Carolina; and Baltimore, Maryland.
In 1981 (wave 1), a probability sample of 175, 211 household residents, who were at least 18 years old and lived in Eastern Baltimore were invited to participate in the Baltimore ECA study. Ultimately, 3,481 completed the baseline interview (Eaton, Kalaydjian, Scharfstein, Mezuk, & Ding, 2007). Follow-up interviews were administered in several subsequent waves: 1982 (wave two; N = 2,768), from 1993 through 1996 (wave three; N = 1,920), and from 2004 through the first half of 2005 (wave four; N = 1,071) (Eaton et al, 2007). The Johns Hopkins Bloomberg School of Public Health Institutional Review Board approved this research. Study design, sampling procedures, questionnaire development, and details of the larger study have been previously published (Eaton et al., 1981; Eaton et al., 2007; Regier et al., 1984).
Study Sample
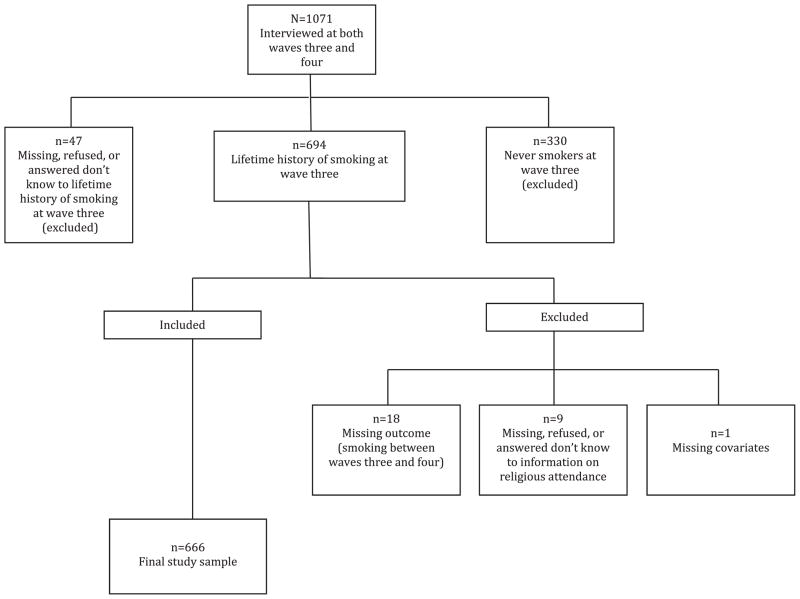
Inclusion in the study sample used in the current prospective analysis was restricted to waves three and four because these were the only waves that assessed religious attendance (the exposure of interest). Participants in the current study (n = 666) were eligible if they reported lifetime smoking at wave three (conducted between 1993 and 1996) and completed a follow-up interview at wave four (between 2004 and 2005). Individuals were excluded from the study (n = 405) if they answered no to having ever-smoked in their lifetime at wave three, were missing information on the exposure of interest (frequency of religious attendance), the outcome (smoking status at wave four), or potential confounders (age, race, sex, education, financial stability, marital status, social connectedness, lifetime episode of dysphoria, and general wellness) (Figure 1).
FIGURE 1.
Flowchart of the Baltimore ECA participants included in the study.
Measurement
All variables were assessed via self-report by trained lay interviewers (Eaton et al., 1981; Rasic, Robinson, Bolton, Bienvenu, & Sareen, 2011). Lifetime smoking status was assessed at wave three as part of the inclusion criteria, by asking participants the following question: “Have you ever smoked tobacco cigarettes?” Participants who responded by indicating that they used cigarettes, cigars but not cigarettes, pipes but not cigarettes, or both cigars and pipes but not cigarettes, were considered lifetime smokers. Smoking status at wave four was the outcome of interest, and measured by asking participants whether or not they smoked cigarettes or other tobacco products since wave three.
The primary exposure, religious attendance, and potential confounders were measured at wave three. Religious attendance was measured by asking participants: “How often do you usually attend religious services?” Participants provided one of the following five answer choices; “never, less than once per month, one to three times per month, about once per week, or more than once per week.” The “never attendance” category was the reference group in this analysis.
Potential confounders included race, age, sex, marital status, education, financial stability, social connectedness, and dysphoria and they were selected based on previous literature. All potential confounders were considered as binary variables, except for age, which was included as a continuous variable. Race was dichotomized as white or other. Education was dichotomized as high-school graduate or not. Financial stability was defined based on whether or not participants reported having at least enough money to meet their general financial needs. Participants were classified as either currently married or not. Participants were classified as socially connected if they talked on the phone or got together with friends a few times per week or more, as compared to less. Overall wellness was rated as either good to excellent health, or fair to poor health. Dysphoria, which is also associated with smoking status (Leventhal, Zvolensky, & Schmidt, 2011; Pomerleau et al., 2005) and characteristics of religiousness (Hettler & Cohen, 1998) was measured with the following question from the DIS—“in your lifetime, have you ever had two weeks or more when nearly everyday you felt sad, blue, or depressed?”
Statistical Analysis
Chi-squared tests and Student’s t-tests were used to assess group differences in smoking status by demographic characteristics at wave three. Generalized linear models using a log link, and Poisson family with robust error variances, also known as a modified Poisson regression, which is a validated method to estimate relative risk when data are binary (Zou, 2004), were used to estimate risk ratios of the association between religious attendance at wave three and smoking status at wave four. This method was chosen because the prevalence of smoking among this population was high (41.3%), thus calculation of the odds ratio would have overestimated the risk ratio. Data were analyzed using Stata/SE statistical software version 10.0 (StataCorp LP, College Station, TX).
RESULTS
The study sample (N = 666) was predominantly female (59.5%), white (62.5%), with at least a high school education (70.7%), and the majority reported smoking cigarettes in their lifetime (97.0%) at wave three. The sample was on average 47.1 years old (standard deviation 11.6 years), financially stable (69.5%), currently married (53.9%), frequently connected with friends (62.9%), in good to excellent health (79.1%), and never experienced daily dysphoria over two weeks or more (68.9%). Approximately 33% attended religious services about once per week or more; 51% attended up to three times per month, and about16% never attended (Table 1). A statistically significant inverse relationship between religious attendance and smoking between waves was demonstrated in both crude and adjusted analyses (Table 2). In the unadjusted model, attending religious services about once per week was associated with a 52% increase in smoking cessation between waves (RR 1.52; 95% CI 1.13, 2.03), whereas attending more than once per week was associated with a 53% increase in smoking cessation between waves (RR 1.53; 95% CI 1.10, 2.13). In the adjusted model, religious attendance about once per week was associated with a 32% increase in smoking cessation (ARR 1.32; 95% CI 1.00, 1.75), and attendance greater than once per week was associated with a 40% increase in smoking cessation between waves (ARR 1.40; 95% CI 1.01, 1.95) (Table 2).
TABLE 1.
Demographic characteristics at wave three of Baltimore ECA participants by smoking status between waves three (1993–1996) and four (2004–2005)
| Smoked between waves
|
||||
|---|---|---|---|---|
| No (n = 275) | Yes (n = 391) | χ 2 p-value | Total n (%) | |
| Demographics | ||||
| Race—No. (%) | p < .01 | |||
| White | 188 (68.4) | 228 (58.3) | 416 (62.5) | |
| Other | 87 (31.6) | 163 (41.7) | 250 (37.5) | |
| Age—years | p < .001* | |||
| Mean (SE) | 50 (.76) | 45 (.52) | 666 (100.0) | |
| Sex—No. (%) | p = .93 | |||
| Males | 112 (40.7) | 158 (40.4) | 270 (40.5) | |
| Females | 163 (59.3) | 233 (59.6) | 396 (59.5) | |
| Education—No. (%) | p = .07 | |||
| at least high school | 205 (74.5) | 266 (68.0) | 471 (70.7) | |
| less than high school | 70 (25.5) | 125 (32.0) | 195 (29.3) | |
| Financial Stability—No. (%) | p < .01 | |||
| Able to meet needs | 209 (76.0) | 254 (65.0) | 463 (69.5) | |
| Unable to meet needs | 66 (24.0) | 137 (35.0) | 203 (30.5) | |
| Currently Married—No. (%) | p < .001 | |||
| Yes | 172 (62.5) | 187 (47.8) | 359 (53.9) | |
| No | 103 (37.5) | 204 (52.2) | 307 (46.1) | |
| Social Connectedness—No. (%) | p = .25 | |||
| Frequent | 180 (65.5) | 239 (61.1) | 419 (62.9) | |
| Infrequent | 95 (34.5) | 152 (38.9) | 247 (37.1) | |
| Dysphoria—No. (%) | p = .05 | |||
| Yes | 74 (26.9) | 133 (34) | 207 (31.1) | |
| No | 201 (73.1) | 258 (66) | 459 (68.9) | |
| Wellness—No. (%) | p = .79 | |||
| Good to excellent health | 219 (79.6) | 308 (78.8) | 527 (79.1) | |
| Fair to poor health | 56 (20.4) | 83 (21.2) | 139 (20.9) | |
| Attend Religious Services—No. (%) | p < .001 | |||
| Greater than once per week | 38 (13.8) | 32 (8.2) | 70 (10.5) | |
| About once per week | 79 (28.7) | 68 (17.4) | 147 (22.1) | |
| 1 to 3 times per month | 41 (14.9) | 81 (20.7) | 122 (18.3) | |
| Less than once per month | 78 (28.4) | 139 (35.5) | 217 (32.6) | |
| Never | 39 (14.2) | 71 (18.2) | 110 (16.5) | |
Asterisk indicates that the p-value for age was obtained from a Student’s t-test, otherwise Chi-squared tests were used.
— Of the non-White group, 231 (92%) were African–American, and 19 (8%) were of other ethnicities.
— Abbreviation: SE = Standard Error.
TABLE 2.
Risk Ratios (RR) for smoking cessation between waves three and four among Baltimore ECA participants
| Crude
|
Adjusted
|
|||
|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | |
| Race | ||||
| White (ref) | 0.77 | (0.63–0.94)** | 0.87 | (0.70 – .1.08) |
| Age | 1.02 | (1.02–1.03)*** | 1.02 | (1.01–1.03)*** |
| Sex | ||||
| Females (ref) | 1.01 | (0.84–1.21) | 0.93 | (0.78–1.11) |
| Education | ||||
| Less than high school (ref) | 1.21 | (0.98–1.50) | 1.32 | (1.07–1.63)** |
| Financial stability | ||||
| Unable to meet needs (ref) | 1.39 | (1.11–1.73)** | 1.11 | (0.88–1.40) |
| Currently married | ||||
| No (ref) | 1.43 | (1.18–1.73)*** | 1.39 | (1.14–1.69)*** |
| Social connectedness | ||||
| Infrequent (ref) | 1.12 | (0.92–1.35) | 1.13 | (0.94–1.37) |
| Dysphoria | ||||
| No (ref) | 0.82 | (0.66–1.01) | 0.85 | (0.69–1.03) |
| Wellness | ||||
| Fair to poor health (ref) | 1.03 | (0.82–1.29) | 0.88 | (0.70–1.09) |
| Attend religious services | ||||
| Greater than once per week | 1.53 | (1.10–2.13)** | 1.40 | (1.01–1.95)* |
| About once per week | 1.52 | (1.13–2.03)** | 1.32 | (1.00–1.75)* |
| 1 to 3 times per month | 0.95 | (0.66–1.35) | 0.96 | (0.68–1.35) |
| Less than once per month | 1.01 | (0.74–1.38) | 1.05 | (0.78–1.41) |
| Never (ref) | – | – | – | – |
— The adjusted model exploring religious attendance and smoking includes age, gender, education, financial stability, marital status, social connectedness, dysphoria, and wellness.
— Abbreviation: Ref indicates reference category.
p-value ≤ .05.
p-value ≤ .01.
p-values ≤ .001.
DISCUSSION
This study found that attending religious services once per week or greater as compared to never was significantly associated with smoking cessation over time among middle-aged, urban adults in Baltimore, Maryland. These results are consistent with other studies that have reported an inverse association between facets of religiousness and tobacco use among older (Koenig et al., 1998), and young populations (Timberlake et al., 2006; Wallace Jr et al., 2003; Whooley et al., 2002; Wills et al., 2003). Smoking at any point across the life span has been associated with poor health outcomes including cancer (Lu et al., 2011), and high health care costs (Rasmussen, Prescott, Sorensen, & Sogaard, 2004). For example, among middle-aged and older populations, smoking has been associated with increased mortality, disability, hospitalization, difficulty performing activities of daily living, poor mobility, and poor self-rated health (Ostbye, Taylor, & Jung, 2002). Promoting quitting among lifetime smokers who are middle-aged may be associated with lifetime health cost savings and other health benefits. For example, one study reported that former smokers who quit smoking between the ages of 35 and 55 as compared to older ages, experienced substantial total lifetime health cost savings (Rasmussen, Prescott, Sorensen, & Sogaard, 2005). Religious attendance may be one activity that can be encouraged, which can promote smoking cessation among urban middle-aged lifetime smokers, and thus lead to potential health benefits.
The mechanisms driving the observed relationship between religious attendance and tobacco use were not assessed in this study. However, another study conducted using the Baltimore ECA cohort, demonstrated that religious attendance was inversely associated with distress, such that more frequent attendance was associated with lower levels of distress (Kidwai, Mancha, Brown, & Eaton, 2013). Stress theories posit that poverty is associated with increased stress levels and increased tobacco use as a potential means to cope with stress (Lambert, Brown, Phillips, & Ialongo, 2004; Perettti-Watel & Constance 2009; Shuaib et al., 2011). Considering that some participants in this cohort were sampled from neighborhoods in East Baltimore that are characterized by high poverty, crime, and violence (Baltimore Neighborhood Indicators Alliance—Jacob France Institute, 2013; U.S. Census Bureau, 2013), religious attendance may have served as a mechanism to relieve stress, and thus reduce the need to smoke as a means of managing stress.
Results from this study should be interpreted with consideration of its limitations. For example, participants may not have been regular smokers at wave three when lifetime smoking status was assessed, which limits an understanding of the duration of abstinence in this study. Nonetheless, the information presented is useful in providing preliminary information on the relationship between lifetime tobacco use and religious attendance among urban, middle-aged adults, an understudied population. Smoking status was obtained via self-report, thus there was the potential for recall bias between waves. Additionally, due to frequent missingness on marijuana use, we did not adjust for marijuana use, which has been associated with smoking status in this population between waves one and two (Ford, Vu, & Anthony, 2002).
The limitations of this study should not over shadow the strengths. For example, this study suggests that religious attendance may be beneficial in helping urban, middle-aged lifetime smokers abstain from smoking. Furthermore, this study elucidates several of the necessary criteria for causal inference (Hill, 1965). First, the prospective design eliminates temporal ambiguity. Additionally, the association between religious attendance and a reduced likelihood of smoking is consistent with other studies that have demonstrated potential benefits of religiousness on health (Kidwai et al, 2013; Koenig et al., 1998; Rasic et al., 2011; Timberlake et al., 2006; Wallace Jr et al., 2003; Whooley et al., 2002; Wills et al., 2003). Future research is needed, however, to corroborate these findings among middle-aged urban adults, and strengthen evidence of a causal relationship.
Considering the potential benefits of religious attendance on reducing smoking among urban middle-aged populations, public health practitioners should consider working with faith-based institutions to develop or strengthen community-based smoking cessation programs in urban communities that target this population. This is relevant because smoking remains prevalent among middle-aged adults in Maryland (Centers for Disease Control and Prevention, 2006), and nationally (Substance Abuse and Mental Health Services Administration, 2012). Furthermore, there is a willingness among this population to use spiritual and religious resources in an effort to quit smoking (Gonzales et al., 2007). Additionally, using faith-based institutions as potential venues for the implementation of smoking cessation programs may be acceptable to many middle-aged adults as they have been found to frequently attend religious services (Rasic et al., 2011; Kidwai et al 2013). Moreover, in the face of broader societal challenges (e.g., economic difficulty), churches can offer the stability, infrastructure, expertise, and resources needed to implement health promotion programs aimed at reducing smoking (Campbell et al., 2007; Reinert, Carver, & Range, 2005).
Acknowledgments
This research was supported by the National Institute of Mental Health grant DA026652 (P.I. William W. Eaton, PhD); and the National Institute on Drug Abuse grant T32DA007292 (P.I. Debra Furr-Holden, PhD).
GLOSSARY
- ECA study
Epidemiologic Catchment Area Study
- Prospective study
The process and analytical methods associated with observing a cohort of people, without the outcome of interest, over time for the development of the outcome
- Religious attendance
Participating in religious activities such as church services
- Smoking
To breathe in smoke from tobacco products
- Tobacco products
Tobacco containing goods such as cigarettes, cigars, or items used for smoking tobacco such as pipes
Biographies
Qiana Brown, MPH, MSW, is an epidemiologist, and licensed social worker. Her research focuses on the role of substance abuse on maternal and child health, and the influence of religiousness and spirituality on recovery. Qiana is also the founder and president of Jane’s House of Inspiration (www.jhofi.org), a nonprofit organization named in honor of her late mother, which helps women and their families recover from substance abuse. Currently, Qiana is a NIDA funded pre-doctoral fellow in the Drug Dependence Epidemiology Training Program at the Johns Hopkins Bloomberg School of public health.

Sabriya Linton, is a doctoral student in the Department of Epidemiology at the Johns Hopkins Bloomberg School of Public Health. She also holds a Masters in Public Health from the Rollins School of Public Health, and a Bachelors of Science from Florida A&M University. After obtaining her MPH, she worked in Rwanda and Zambia as a project coordinator for the Rwanda Zambia HIV Research Group, and later provided domestic technical support for international development projects as a Health Associate at Medical Care Development International. Her research interests are at the intersection of social epidemiology, substance abuse, and infectious diseases.
Paul T. Harrell, PhD, is currently a postdoctoral fellow at Moffitt Cancer Center. He is primarily a health psychology and epidemiology researcher with a focus on substance dependence. Substances of interest have varied from caffeine to tobacco to heroin, but with all substances he has emphasized cognitive and learning factors. His experimental models, focused thus far on caffeine and nicotine, allow for safe, convenient, and ethical testing of theoretical cognitive and learning processes in controlled laboratory settings. His epidemiological research complements this approach by extending these findings into ecologically valid settings, thereby enhancing translation into policy.
Brent E. Mancha, PhD, MHS, is an epidemiologist for the US Department of Defense and a consultant for the University of Florida. He has also worked with the Johns Hopkins Hubert H. Humphrey Fellowship Program and is a graduate of the NIDA Drug Dependence Epidemiology Training (DDET) Program at the Johns Hopkins Bloomberg School of Public Health. Dr. Mancha’s research focuses on the epidemiology of alcohol and drug dependence, behavioral, and mental health disorders, in adolescent, adult, and military populations.
Pierre Kébreau Alexandre, PhD, MS, MPH, is an Associate Professor of Health Economics at the Johns Hopkins Bloomberg School of Public Health in the Department of Mental Health. His work experience includes policy and program evaluation, substance abuse and mental health policy and economics, HIV/AIDS economics, cost and benefit analysis, cost-effectiveness analysis, and the economics of crime. He has been principal investigator and co-investigator on numerous research grants from U.S. National Institutes of Health and state agencies. He has conducted international research in Uganda, Ivory Coast, Mexico, and Haiti. He has several publications in health economics; particularly behavioral economics.
Dr. Kuan-Fu Chen, is an assistant professor and an emergency physician of “Emergency Medicine” and “Clinical Informatics and Medical Statistics” at the Chang Gung University, Taiwan. He received his MD from the Chung Shan Medical University in Taiwan and visited the Emergency Department of the Johns Hopkins University as a research fellow, where he also earned a PhD degree in clinical investigation. He is interested in developing clinical prediction rule to assist patient risk stratification and rapid identification in emergency medicine.
William W. Eaton, PhD, is a professor in the Department of Mental Health, Bloomberg School of Public Health. He received the Administrator’s Award from the Alcohol, Drug Abuse, and Mental Health Administration for “implementing the Epidemiologic Catchment Area Program” in 1980 and the Rema Lapouse Award for psychiatric epidemiology from the American Public Health Association in 2000. His research concerns risk factors and natural history of mental disorders. The third edition of his The Sociology of Mental Disorders appeared in 2001. In 2012, he edited, together with faculty, students, and fellows of the Department of Mental Health, Public Mental Health.
Footnotes
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
References
- Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: Evidence and lessons learned. Annual Review of Public Health. 2007;28:213–234. doi: 10.1146/annurev.publhealth.28.021406.144016. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Behavioral risk factor surveillance system: Prevalence and trends data: Maryland 2006 adults who are current smokers. 2006 Retrived from http://apps.nccd.cdc.gov/BRFSS/age.asp?cat=TU&yr=2006&qkey=4396&state=MD.
- Centers for Disease Control and Prevention. Smoking-attributable mortality, years of potential life lost, and productivity losses: United States, 2000–2004. Morbidity and Mortality Weekly Report. 2008;57(45):1226–1228. [PubMed] [Google Scholar]
- Baltimore Neighborhood Indicators Alliance – Jacob France Institute. Vital signs 11. 2013 Retrieved from http://bniajfi.org/vs11report.
- Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJL, Ezzati M. The preventable causes of death in the United States: Comparative risk assessment of dietary, lifestyle, and metabolic risk factors. Plos Medicine. 2009;6(4):1–23. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupre ME, George LK, Liu G, Peterson ED. The cummulative effect of unemployment on risks for acute myocardial infarction. Archives of Internal Medicine. 2012;172(22):1731–1737. doi: 10.1001/2013.jamainternmed.447. [DOI] [PubMed] [Google Scholar]
- Eaton WW, Kalaydjian A, Scharfstein DO, Mezuk B, Ding Y. Prevalence and incidence of depressive disorder: The Baltimore ECA follow-up, 1981–2004. Acta Psychiatrica Scandinavica. 2007;116(3):182–188. doi: 10.1111/j.1600-0447.2007.01017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton WW, Regier DA, Locke BZ, Taube CA. The Epidemiologic Catchment Area Program of the National Institute of Mental Health. Public Health Reports. 1981;96(4):319–325. [PMC free article] [PubMed] [Google Scholar]
- Ford DE, Vu HT, Anthony JC. Marijuana use and cessation of tobacco smoking in adults from a community sample. Drug and Alcohol Dependence. 2002;67(3):243–248. doi: 10.1016/s0376-8716(02)00066-2. [DOI] [PubMed] [Google Scholar]
- Gonzales D, Redtomahawk D, Pizacani B, Bjornson WG, Spradley J, Allen E, Lees P. Support for spiritiuality in smoking cessation: Results of a pilot study. Nicotine and Tobacco Research. 2007;9(2):299–303. doi: 10.1080/14622200601078582. [DOI] [PubMed] [Google Scholar]
- Hettler TR, Cohen LH. Intrinsic religiousness as a stress-moderator for adult Protestant churchgoers. Journal of Community Psychology. 1998;26(6):597–609. [Google Scholar]
- Hill AB. The environment and disease: Association or causation? Proceedings of the Royal Society of Medicine. 1965;58:295–300. doi: 10.1177/003591576505800503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns M, Sacks R, Rane M, Kansagra SM. Exposure to tobacco retail outlets and smoking initiation among New York City Adolescents. Journal of Urban Health. 2013;90(6):1091–1101. doi: 10.1007/s11524-013-9810-2. doi:10.1007/s11524-013–9810-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kidwai R, Mancha BE, Brown QL, Eaton WW. The effects of spirituality and religious attendance on the relationship between psychological distress and negative life events. Social Psychiatry and Psychiatric Epidemiology. 2013;49(3):487–497. doi: 10.1007/s00127-013-0723-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig HG. Spirituality and health research: Methods, measurement, statistics, and resources. West Conshohocken, PA: Templeton Press; 2011. [Google Scholar]
- Koenig HG, George LK, Cohen HJ, Hays JC, Larson DB, Blazer DG. The relationship between religious activities and cigarette smoking in older adults. The Journals of Gerontology: Series A, Biological Sciences and Medical Sciences. 1998;53(6):M426–M434. doi: 10.1093/gerona/53a.6.m426. [DOI] [PubMed] [Google Scholar]
- Koenig HG, King DE, Carson VB. Hanbook of religion and health. 2. Oxford, NY: Oxford University Press, Inc; 2012. [Google Scholar]
- Lambert SF, Brown TL, Phillips CM, Ialongo NS. The relationship between perceptions of neighborhood characteristics and substance use among urban African American adolescents. American Journal of Community Psychology. 2004;34(3–4):205–218. doi: 10.1007/s10464-004-7415-3. [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Zvolensky MJ, Schmidt NB. Smoking-related correlates of depressive symptom dimensions in treatment-seeking smokers. Nicotine and Tobacco Research. 2011;13(8):668–676. doi: 10.1093/ntr/ntr056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Y, Wang SS, Reynolds P, Chang ET, Ma H, Sullivan-Halley J, Bernstein L. Cigarette smoking, passive smoking, and non-hodgkin lymphoma risk: Evidence from the California Teachers Study. American Journal of Epidemiology. 2011;174(5):563–573. doi: 10.1093/aje/kwr127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLos Medicine. 2006;3(11):2011–2030. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Nollen LN, Catley D, Davies G, Hall M, Ahluwalia JS. Religiosity, social support, and smoking cessation among urban African American smokers. Addictive Behaviors. 2005;30(6):1225–1229. doi: 10.1016/j.addbeh.2004.10.004. [DOI] [PubMed] [Google Scholar]
- Ostbye T, Taylor DH, Jung SH. A longitudinal study of the effects of tobacco smoking and other modifiable risk factors on ill health in middle-aged and old Americans: Results from the Health and Retirement Study and Asset and Health Dynamics among the Oldest Old survey. Preventive Medicine. 2002;34(3):334–345. doi: 10.1006/pmed.2001.0991. [DOI] [PubMed] [Google Scholar]
- Pargament KI, Brant CR. Religion and coping. In: Koenig HG, editor. Handbook of Religion and Mental Health. San Diego, CA: Academic Press; 1998. pp. 111–128. [Google Scholar]
- Peretti-Watel P, Constance J. It’s all we got left: Why poor smokers are less sensitive to cigarette price increases. International Journal of Environmental Research and Public Health. 2009;6(2):608–621. doi: 10.3390/ijerph6020608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson NA, Yu D, Morton CM, Reid RJ, Sheffer MA, Schneider JE. Tobacco outlet density and demographics at the tract level of analysis in New Jersey: A statewide analysis. Drugs: Education, Prevention, and Policy. 2011;18(1):47–52. [Google Scholar]
- Pomerleau OF, Pomerleau CS, Mehringer AM, Snedecor SM, Ninowski R, Sen A. Nicotine dependence, depression, and gender: Characterizing phenotypes based on withdrawal discomfort, response to smoking, and ability to abstain. Nicotine and Tobacco Research. 2005;7(1):91–102. doi: 10.1080/14622200412331328466. [DOI] [PubMed] [Google Scholar]
- Rasic D, Robinson JA, Bolton J, Bienvenu OJ, Sareen J. Longitudinal relationships of religious worship attendance and spirituality with major depression, anxiety disorders, and suicidal ideation and attempts: Findings from the Baltimore Epidemiologic Catchment area study. Journal of Psychiatric Research. 2011;45(6):848–854. doi: 10.1016/j.jpsychires.2010.11.014. [DOI] [PubMed] [Google Scholar]
- Rasmussen SR, Prescott E, Sorensen TIA, Sogaard J. The total lifetime costs of smoking. European Journal of Public Health. 2004;14(1):95–100. doi: 10.1093/eurpub/14.1.95. [DOI] [PubMed] [Google Scholar]
- Rasmussen SR, Prescott E, Sorensen TIA, Sogaard J. The total lifetime health cost savings of smoking cessation to society. European Journal of Public Health. 2005;15(6):601–606. doi: 10.1093/eurpub/cki024. [DOI] [PubMed] [Google Scholar]
- Regier DA, Myers JK, Kramer M, Robins LN, Blazer DG, Hough RL, Locke BZ. The NIMH Epidemiologic Catchment Area program. Historical context, major objectives, and study population characteristics. Archives Of General Psychiatry. 1984;41(10):934–941. doi: 10.1001/archpsyc.1984.01790210016003. [DOI] [PubMed] [Google Scholar]
- Reinert B, Carver V, Range L. Church leaders’ opinions about tobacco prevention. Health Education. 2005;106(3):201–209. [Google Scholar]
- Rodriguez D, Carlos HA, Adachi-Mejia AM, Berke EM, Sargent JD. Predictors of tobacco outlet density nationwide: a geographic analysis. Tobacco Control. 2012;22(5):349–355. doi: 10.1136/tobaccocontrol-2011-050120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuaib F, Foushee HR, Ehiri J, Bagchi S, Baumann A, Kohler C. Smoking, sociodemographic determinants, and stress in the Alabama Black Belt. The Journal of Rural Health. 2011;27(1):50–59. doi: 10.1111/j.1748-0361.2010.00317.x. [DOI] [PubMed] [Google Scholar]
- Strawbridge WJ, Shema SJ, Cohen RD, Kaplan GA. Religious attendance increases survival by improving and maintaining good health behaviors, mental health, and social relationships. Annals of Behavioral Medicine. 2001;23(1):68–74. doi: 10.1207/s15324796abm2301_10. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. (NSDUH Series H-46, HHS Publication No. SMA 13–4795) 2013. [Google Scholar]
- Timberlake DS, Rhee SH, Haberstick BC, Hopfer C, Ehringer M, Lessem JM, Hewitt JK. The moderating effects of religiosity on the genetic and environmental determinants of smoking initiation. Nicotine & Tobacco Research. 2006;8(1):123–133. doi: 10.1080/14622200500432054. [DOI] [PubMed] [Google Scholar]
- U.S. Bureau of Labor Statistics. US Department of Labor, The Editor’s Desk, number of jobs held by baby boomers, 1978–2008. 2010 Retrieved from http://www.bls.gov/opub/ted/2010/ted20100924.htm.
- U.S. Census Bureau. State and County quickfacts. Baltimore City, Maryland: 2013. Retrieved from http://quickfacts.census.gov/qfd/states/24/24510.html. [Google Scholar]
- Wallace JM, Jr, Brown TN, Bachman JG, Laveist TA. The influence of race and religion on abstinence from alcohol, cigarettes and marijuana among adolescents. Journal of Studies on Alcohol. 2003;64(6):843–848. doi: 10.15288/jsa.2003.64.843. [DOI] [PubMed] [Google Scholar]
- Whooley MA, Boyd AL, Gardin JM, Williams DR. Religious involvement and cigarette smoking in young adults: The CARDIA study. Archives of Internal Medicine. 2002;162(14):1604–1610. doi: 10.1001/archinte.162.14.1604. [DOI] [PubMed] [Google Scholar]
- Wills TA, Yaeger AM, Sandy JM. Buffering effect of religiosity for adolescent substance use. Psychology of Addictive Behaviors. 2003;17(1):24–31. doi: 10.1037/0893-164x.17.1.24. [DOI] [PubMed] [Google Scholar]
- Yu D, Peterson NA, Sheffer MA, Reid RJ, Schnieder JE. Public Health. Tobacco outlet density and demographics: Analysing the relationships with a spatial regression approach. 2010;124(7):412–416. doi: 10.1016/j.puhe.2010.03.024. [DOI] [PubMed] [Google Scholar]
- Zou G. A modified poisson regression approach to prospective studies with binary data. American Journal of Epidemiology. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]