Abstract
Patient: Male, 66
Final Diagnosis: Hepatocellular carcinoma
Symptoms: Abdominal distension • painful right facial swelling • weight loss
Medication: —
Clinical Procedure: —
Specialty: —
Objective:
Rare disease
Background:
Hepatocellular carcinoma is a common cancer, but it rarely metastasizes to the salivary glands. A review of the literature revealed only 5 reported cases of hepatocellular carcinoma metastatic to parotid glands. We here report an additional case of this rare association.
Case Report:
A 66-year-old male with a background of type 2 diabetes mellitus and post-alcoholic decompensated liver cirrhosis presented with a progressively enlarging painful right facial swelling for 2 months that was eventually found to be due to hepatocellular carcinoma metastatic to the right parotid gland. Fine needle aspiration from the right parotid showed sheets and single malignant cells that were interpreted as carcinoma not otherwise specific. However, biopsy showed metastatic hepatocellular carcinoma into the right parotid gland.
Conclusions:
We report an additional case of the rare metastasis of hepatocellular carcinoma to the parotid glands. It should therefore be considered in a patient with decompensated liver cirrhosis presenting with a parotid swelling. Furthermore, the present case demonstrates the importance of the tissue biopsy for obtaining an accurate final diagnosis.
MeSH Keywords: Carcinoma, Hepatocellular; Gastrointestinal Neoplasms; Neoplasm Metastasis; Neoplasm Metastasis; Parotid Gland
Background
Hepatocellular carcinoma is one of the most prevalent cancers worldwide. It commonly metastasizes to the lungs, lymph nodes, peritoneum, adrenal glands, and bone, although there are uncommon reports of metastases to the ovaries, skin, heart, pharynx, orbit, and external auditory canal [1–6]. Metastasis to parotid glands is rare and to the best of our knowledge only 5 cases of hepatocellular carcinoma metastatic to parotid glands have been reported [7–11]. We report the case of a 66-year-old male who presented with a 2-month history of a progressively enlarging right facial swelling that was eventually found to be hepatocellular carcinoma with metastases to the right parotid gland.
Case Report
A 66-year-old male Sudanese patient with a background of type 2 diabetes mellitus and post-alcoholic liver cirrhosis presented with a progressively enlarging painful right facial swelling for 2 months (Figure 1). He also reported a history of significant weight loss and progressive abdominal distention and discomfort. His past medical history was significant for 1 episode of variceal bleeding that was treated with sclerotherapy and a history of heavy alcohol intake. Physical examination revealed right-sided swelling in the face of about 7×7 cm on the upper part of the right mandible extending to the right ear that was firm and mildly tender to palpation, as well as hepatosplenomegaly. Shifting dullness was positive by percussion and hepatic bruit was present on auscultation.
Figure 1.

The right facial swelling.
Initial laboratory investigations revealed WBC 2.2×103 /uL, RBC 3.6×106/uL, hemoglobin 11.9 g/dL, platelets 71×103/uL, and MCH 31.4 pg. Urea 8.9 mmol/L, serum creatinine 87 umol/L, albumin 23 g/L, total protein 70 g/L, sodium 132 mmol/L, potassium 4.9 mmol/L, total bilirubin 21 umol/L, bicarbonate 25 mmol/L, ALT 100 u/L, and AST 73 u/L. Alpha-fetoprotein was 3525 IU/ml, PT 11.3 seconds, INR 1, and PTT 26.5 seconds.
Abdominal ultrasound showed cirrhotic liver with a heterogeneous mass in the right upper lobe, signs of portal hypertension, splenomegaly, and ascites. A tri-phasic CT scan of the abdomen showed a cirrhotic liver, portal hypertension, and multicenter hepatocellular carcinoma of the right lobe of the liver; the largest mass was 7×10 cm and another smaller mass was 3 cm in diameter. The lesion showed hypo-attenuation in the venous phase and delayed phase with iso-dense arterial phase (Figure 2A, 2B). There was no evidence of lung metastasis. The result of ascetic fluid examination for cytology was negative for malignant cells. CT scan of the neck showed right mandibular angle osteolytic destructive lesion with buckle side soft tissue mass infiltrating the masseter muscle and ventrally indenting the right parotid salivary gland (Figure 3A, 3B), findings indicating a malignant tumor lesion, most likely metastatic (considering the patient history and CT-scan abdomen findings). A bone scan showed increased uptake in the right mandible, representing reactive hyperemia to the soft-tissue tumor or bone involvement. There was no evidence of metastatic lesion.
Figure 2.
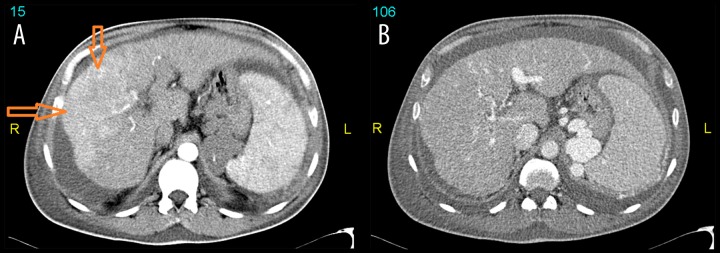
CT scan of the upper abdomen in arterial (A) and venous (B) phases revealed a small cirrhotic liver with wide spread infiltrative type of hepatocellular carcinoma involving almost the whole right lobe and segment IV of the left lobe which showed patchy areas of arterial enhancement (arrows) with washout in venous phase. Splenomegaly and portal hypertension associated with spleno-renal shunt and extensive varicose veins formation is seen as well as bilateral pleural effusion and ascites.
Figure 3.
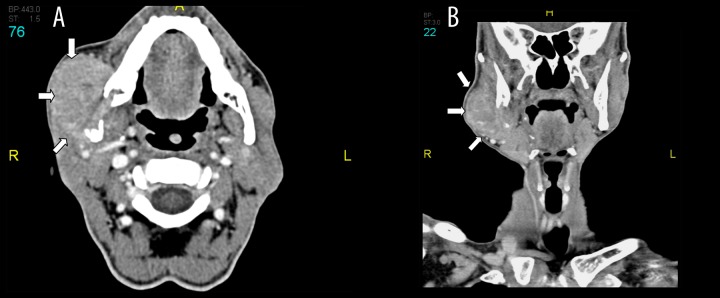
Post contrast CT scan axial (A) and coronal (B) shows right mandibular angle osteolytic destructive lesion with buckle side soft tissue mass infiltrating the masseter muscle and ventrally indenting the right parotid salivary gland (block arrows).
Fine-needle aspiration from the right parotid showed sheets and single malignant cells that were interpreted as carcinoma not otherwise specific. Tru-cut biopsy from the right parotid gland was then performed and histopathology examination showed metastatic hepatocellular carcinoma into parotid gland tissue (Figure 4A, 4B). The metastatic deposits are formed of cords and acinar structures with moderate nuclear atypia and immunohistochemical profile indicating hepatocellular origin: positive CK18, HepPar 1, and canalicular pattern staining for pCEA.
Figure 4.
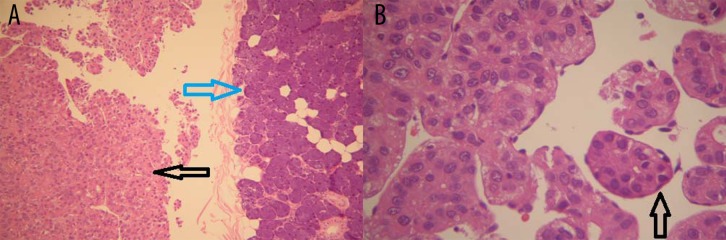
(A) Microscopic appearance of the tumor to the left side (black arrow) adjacent to the salivary gland tissue in the right half of the picture (blue arrow) (H&E ×100). (B) Details of the tumor cells which are arranged in trabeculae and nests (arrow) with sinusoidal cells covering the tumor cells (H&E ×400).
Based on these findings, the final diagnosis was multicentric hepatocellular carcinoma with right parotid gland metastases in a patient with Childs C liver cirrhosis. Palliative care was the final plan of treatment for the patient. The patient’s hospital course was complicated by an episode of hepatic encephalopathy, spontaneous bacterial peritonitis, hypoglycemia, and peritoneal bleeding. Computed tomography angiography of the abdomen revealed a focal defect in the liver capsule. After supportive treatment, the patient was discharged in stable condition and planned for out-patient follow-up. He died 2 months later due to massive upper GI bleeding.
Discussion
In the present report we described the case of a male Sudanese patient with decompensated liver cirrhosis complicated with end-stage multicentric hepatocellular carcinoma (stage D according to Barcelona Clinic of Liver Cancer, BCLC, staging classification) [12,13] with right parotid gland metastasis and without lung metastasis. Based on our review of the English literature, we were able to locate only 5 cases of metastatic hepatocellular carcinoma to parotid glands since 1966 [7–11], suggesting that this association is rare. Table 1 summarizes all 5 previous case reports of metastatic hepatocellular carcinoma to the parotid glands and compares it with the present case report. The right parotid gland was involved in 4 of the 5 previously reported cases [7–10], as well as in the present case. However, the left parotid was only involved in 1 case [11] and additionally involved in another [7]. Moreover, as in the present case, the primary lesion was in the right lobe of the liver in the 2 case reports [8,10] in which details about the imaging studies of the liver were provided.
Table 1.
Summary of previous reported cases of hepatocellular carcinoma (HCC) patients metastasis to parotid glands.
| Author/year (reference) | Age/gender | Patient’s origin | Risk factor for cirrhosis | Liver lobe site of HCC | Size of HCC (cm) | Other metastasis than parotid gland | Parotid lobe involved | AFP level at diagnosis (IU/ml) | Treatment/outcome | FNA | Histopathology |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Current case | 66/male | Sudanese | Alcoholism | Right | 10×7 | No | Right | 3525 | Died after 2 months | Not diagnostic | Diagnostic |
| Dargent JL, et al., 1998 [7] | 62/male | Zairian | HCV, alcoholism | – | 3.5×2.8 | Bone | Right and left | 3520 | Not reported | Typical for HCC | Diagnostic |
| Romanns M, et al., 2004 [8] | 47/male | Not reported | HCV, alcoholism | Right | 7×7 | No | Right | Normal | Died after 4 months | Typical for HCC | Diagnostic |
| Vitale AR et al., 2009 [9] | 82/male | Caucasian | Not reported | Not reported | 3.8 (on US) | No | Right | Not reported | Died after 6 months | Not diagnostic | Diagnostic |
| Moore F, et al., 2010 [10] | 75/male | Not reported | Alcoholism | Right | Not reported | Bone | Right | Not reported | Stable at 2 years on chemotherapy | Not Diagnostic | Diagnostic |
| Yu YD, et al., 2013 [11] | 36/male | Korean | HBV | Right | Multiple largest 9.3×7.5 | No | Left | Normal | Stable at 1 year | Not diagnostic | Diagnostic |
HBV – hepatitis B virus; HCV – hepatitis C virus; HCC – hepatocellular carcinoma; US – ultrasound of the liver.
In the present patient, FNA of the right parotid lesion showed malignant cells but did not suggest the presence of metastatic hepatocellular carcinoma cells, similar to 2 previous reported cases [9,11]. In the other reported cases [7,8,10], FNA was suggestive of metastatic hepatocellular carcinoma. In all cases, including our case, biopsy of the right parotid confirmed the diagnosis.
In 2 of the case reports the outcome was death within a few months [8,9], 2 cases reported apparently stable patients during follow-up [10,11] and another case was lost to follow-up [7]. The present case died 2 months later due to massive upper GI bleeding.
Conclusions
In conclusion, metastasis of hepatocellular carcinoma to the parotid glands is rare, but it should be considered in a patient with a history of hepatocellular carcinoma presenting with parotid swelling. Biopsy of the affected parotid gland is needed for definite histological diagnosis of metastasized hepatocellular carcinoma and it is superior to fine-needle aspiration.
Footnotes
Conflict of interest
No conflict of interest to declare.
References:
- 1.Kim TH, Cheung DY, Chung WB, et al. A case of metastatic hepatocellular carcinoma of the ovary. Korean J Gastroenterol. 2004;43(3):215–18. [PubMed] [Google Scholar]
- 2.Masci G, Magagnoli M, Grimaldi A, et al. Metastasis of hepatocellular carcinoma to the heart: a case report and review of the literature. Tumori. 2004;90(3):345–47. doi: 10.1177/030089160409000317. [DOI] [PubMed] [Google Scholar]
- 3.Yamanishi K, Kishimoto S, Hosokawa Y, et al. Cutaneous metastasis from hepatocellular carcinoma resembling granuloma teleangiectaticum. J Dermatol. 1989;16(6):500–4. doi: 10.1111/j.1346-8138.1989.tb01593.x. [DOI] [PubMed] [Google Scholar]
- 4.Oida Y, Ishii M, Dowaki S, et al. Hepatocellular carcinoma with metastasis to the pharynx: report of a case. Tokai J Experimental Clin Medicine. 2005;30(1):31–34. [PubMed] [Google Scholar]
- 5.Font RL, Maturi RK, Small RG, Garcia-Rojas M. Hepatocellular carcinoma metastatic to the orbit. Arch Ophthalmol. 1998;116(7):942–45. doi: 10.1001/archopht.116.7.942. [DOI] [PubMed] [Google Scholar]
- 6.Yasumatsu R, Okura K, Sakiyama Y, et al. Metastatic hepatocellular carcinoma of the external auditory canal. World J Gastroenterol. 2007;13(47):6436–38. doi: 10.3748/wjg.v13.i47.6436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dargent JL, Deplace J, Schneider E, et al. Hepatocellular carcinoma metastatic to the parotid gland: initial diagnosis by fine needle aspiration biopsy. Acta Cytol. 1998;42(3):824–26. [PubMed] [Google Scholar]
- 8.Romanas MM, Cherian R, McGregor DH, et al. Hepatocellular carcinoma diagnosed by fine-needle aspiration of the parotid gland. Diagn Cytopathol. 2004;30(6):401–5. doi: 10.1002/dc.20040. [DOI] [PubMed] [Google Scholar]
- 9.Vitale AR, Compilato D, Coletti G, et al. Metastatic hepatocellular carcinoma of the parotid region without lung metastasis: a case report. Int J Oral Maxillofa Surg. 2009;38(6):696–98. doi: 10.1016/j.ijom.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 10.Moore FR, Bergman S, Geisinger KR. Metastatic hepatocellular carcinoma mimicking acinic cell carcinoma of the parotid gland: a case report. Acta Cytol. 2010;54(5 Suppl.):889–92. [PubMed] [Google Scholar]
- 11.Yu YD, Kima DS, Jung SW, et al. Metastatic hepatocellular carcinoma to the parotid gland: Case report and review of the literature. Intern J Surg Case Report. 2013;4(1):76–80. doi: 10.1016/j.ijscr.2012.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liovet JM, Bru C, Bruix J. Prognosis of Hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis. 1999;19(3):329–38. doi: 10.1055/s-2007-1007122. [DOI] [PubMed] [Google Scholar]
- 13.Forner A, Reig ME, de Lope CR, Bruix J. Current Strategy for Staging and Treatment: the BCLC update and future prospects. Semin Liver Dis. 2010;30(1):61–74. doi: 10.1055/s-0030-1247133. [DOI] [PubMed] [Google Scholar]


