Abstract
Background
The aim of this study was to investigate the degree of impact of obstructive sleep apnea hypopnea syndrome (OSAHS) severity on pediatric psychological and behavioral abnormalities.
Material/Methods
Fifty-one children aged 5–12 years with a confirmed diagnosis of OSAHS were divided into 3 groups according to the severity of OSAHS. They underwent bilateral tonsillectomy plus adenoidectomy or adenoidectomy alone. Repeated polysomnography and integrated visual and auditory continuous performance testing (IVA-CPT) was performed to assess full-scale response control quotient (FRCQ), full-scale attention quotient (FAQ), and hyperactivity (HYP) before surgery and 3 and 6 months after surgery.
Results
Mean FRCQ, FAQ, and HYP significantly improved over time in the 3 groups (FRCQ, F=292.05; FAQ, F=258.27; HYP, F=295.10, all P<0.001). FRCQ and HYP were not significantly different among the groups at the 3 time points. FAQ was significantly different among the groups (F=3.89, P<0.05). For FRCQ, FAQ, and HYP, there was no interaction between time and disease severity. Within groups, the effect of time on the apnea-hypopnea index (AHI) and lowest oxygen saturation (LaSO2) were significant for each group and they were significantly different among the 3 groups at each time point (all P<0.001).
Conclusions
These results suggest that OSAHS may have a significant impact on self-control, attention, and hyperactivity in children, which is gradually alleviated after surgery. Disease severity was not closely related to preoperative mental and psychological function or postoperative recovery. Thus, we find it difficult to determine the impact degree of OSAHS severity on mental and psychological function or predict postoperative recovery by using OSAHS severity alone in children.
MeSH Keywords: Behavioral Research, Child, Psychological Tests, Severity of Illness Index, Sleep Apnea, Obstructive
Background
Obstructive sleep apnea-hypopnea syndrome (OSAHS) is a relatively common condition that may impair physical and mental development in children. In addition to snoring, mouth breathing, night terrors, and apnea, children with OSAHS may experience a series of concurrent mental and psychological symptoms, including poor self-control, inattention, hyperactivity, memory loss, cognitive decline, and poor academic performance, as well as impaired growth and development [1–7]. Indeed, research suggests that approximately 20–30% of children with OSAHS experience inattention and hyperactivity [8]. Attention deficit hyperactivity disorder (ADHD)-like symptoms may even occur in severe cases [9].
Typically, one would assume that the mental and psychological abnormalities caused by OSAHS in children are related to the severity of OSAHS. However, in our clinical practice, we have found that some children with severe OSAHS, as indicated by polysomnography (PSG), do not have obvious mental and psychological abnormalities, whereas some children with mild OSAHS have marked mental and psychological abnormalities. We therefore decided to examine which OSAHS factors are related to concurrent mental and psychological abnormalities in children with OSAHS. This study aimed to explore the relationship between the severity of OSAHS and the degree of mental and psychological abnormalities caused by OSAHS.
Previously, the impact of OSAHS on psychological behavior in children has been assessed using a variety of scales, and the degree of impact determined by taking into account physicians’ observations. Unfortunately, due to limitations associated with many factors, (e.g., expression capability, education level, observation capability, and subjective consciousness), family members’ descriptions and physicians’ observations often do not accurately reflect the true disease status of children.
Integrated visual and auditory continuous performance testing (IVA-CPT) is commonly used for the diagnosis of ADHD in children and adults [10,11]. Subjects provide instant reactions to simple auditory and visual cues given by clicking a mouse, and data are analyzed by computer software to provide quantitative results. Therefore, IVA-CPT is relatively objective, quantifiable, and easy to perform. In this study, we used the IVA-CPT method to measure the full-scale response control quotient (FRCQ), full-scale attention quotient (FAQ), and hyperactivity (HYP) in children with PSG-confirmed OSAHS before and after surgery. In doing so, we aimed to explore the impact of OSAHS on psychological behavior, the extent of impact, postoperative recovery, and the relationship between the severity of OSAHS and the impact of OSAHS on psychological behavior, as well as postoperative recovery in these children.
Material and Methods
Patients
All patients included in this study were children with OSAHS who were treated at the Department of Otorhinolaryngology Head and Neck Surgery, Hangzhou First People’s Hospital Affiliated to Nanjing Medical University from February 2010 to October 2011. These pediatric OSAHS patients were consecutively sampled during this period. Each patient had an at least 2-year history of snoring, mouth-breathing, and/or multiple sleep apneas before admission to our hospital. According to eligibility criteria, 70 patients were enrolled in this study. The present study was approved by the Institutional Ethics Committee of Hangzhou First People’s Hospital Affiliated to Nanjing Medical University.
Eligibility criteria
Inclusion criteria
1) Children underwent PSG and met the diagnostic criteria for OSAHA as specified by the Otolaryngology Chapter of the Chinese Medical Association [12]. 2) Children had a normal history of birth, feeding, and growth. 3) Children were aged 5–12 years and experienced onset of OSAHS at 3 years of age. Children had not yet entered puberty and had not experienced any major changes in living environment. 4) Parents agreed to allow their children to participate in the study and provided written informed consent. 5) All children underwent physical examination, lateral nasopharynx x-ray, nasopharynx computed tomography, and/or nasopharyngoscopy to confirm that OSAHS was caused by adenoid hyperplasia with 2/3-complete obstruction of nasopharynx and/or tonsillar hypertrophy with a class II, III, or IV of Friedman classification.
Exclusion criteria
1) Congenital anatomical abnormalities of the mouth, nose, or pharynx and/or facial morphology. 2) Severe neonatal asphyxia or hypoxic-ischemic encephalopathy at birth. 3) History of chronic disease, including tuberculosis, viral hepatitis, nephrotic syndrome or severe trauma. 4) History of cerebral palsy or epileptic seizures. 5) Recurrent upper respiratory tract infections. 6) Family history of familial short stature, congenital mental retardation, mental illness, or other congenital genetic and metabolic diseases in 3 generations on the maternal or paternal side that can affect physical development. 7) Diseases with manifestations of obstructive sleep apnea-hypopnea not caused by adenoid and/or tonsillar hypertrophy. 8) Recent history of antipsychotic drug use.
Grouping and PSG
Children were divided into 2 groups according to the duration of disease: <5 years and ≥5 years. PSG was performed using an Embletta X100 type polysomnography system (Embla, Broomfield, CO). All children underwent continuous PSG for more than 7 h prior to surgery and at 3 and 6 months after surgery (termed the first, second, and third time point); the apnea-hypopnea index (AHI) and lowest oxygen saturation (LaSO2) measures were recorded. Patients were also divided into groups by the severity of OSAHS (mild: 5< AHI ≤10 Times/h, moderate: 10< AHI ≤20 Times/h, or severe: AHI >20 Times/h) before surgery according the criteria published by Otolaryngology Chapter of the Chinese Medical Association [12]. Body mass index (BMI) was measured at each assessment time point.
IVA-CPT
Psychologists, who were not allowed to obtain patients’ PSG results, administered the IVA-CPT to all children before surgery using version 1.1 of the IVA-CPT test system (BrainTrain, North Chesterfield, VA).
The basic principle of the IVA-CPT is to observe and record patients’ responses to 13 min of auditory and visual stimuli, including reaction time, omissions, endurance, and the number of repeats. An assessment conclusion is made by computer using an algorithm. The IVA-CPT report contains 6 comprehensive quotients based on a total of 22 original quotients. We selected 3 indicators closely related to our study for analysis: FRCQ, FAQ, and HYP. FRCQ<85, FAQ<85 or HYP<100 is considered abnormal. In accordance with the IVA-CPT-related diagnostic criteria for ADHD [13], children with abnormal FRCQ or FAQ plus abnormal HYP were considered to have mental abnormalities.
Surgical treatment and follow-up
All patients underwent bilateral tonsillectomy plus adenoidectomy or adenoidectomy alone and were discharge without incident.
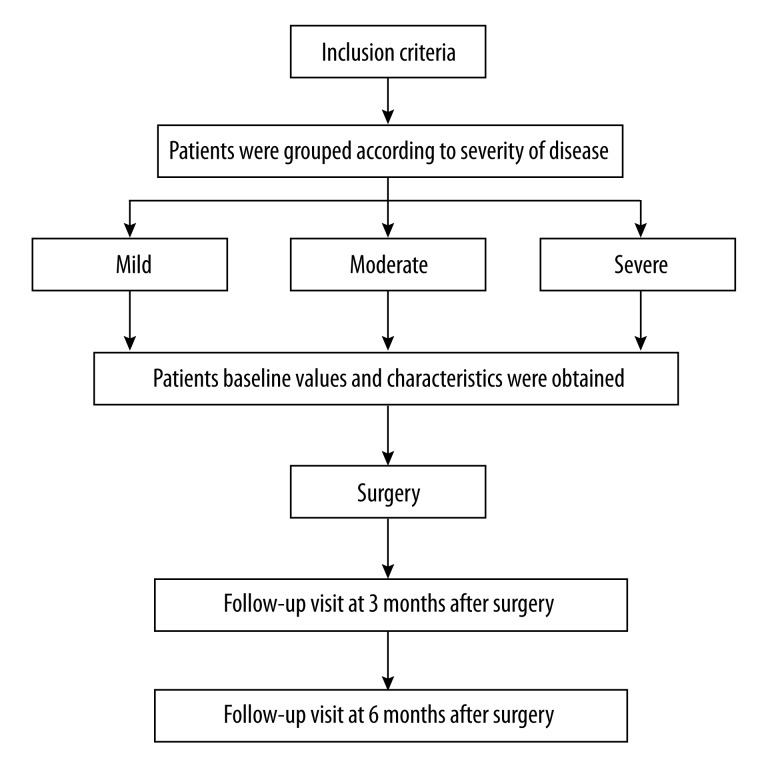
Follow-up PSG and IVA-CPT assessments were carried out 3 and 6 months after surgery. Figure 1 summarizes the study design/flow.
Figure 1.
Study flow diagram.
Statistical analysis
Normality of the data was tested using the K-S test. Data are presented as mean ± standard deviation. Group means were compared using Student’s t-test or chi-square test. Repeated measures analysis of variance was used to examine the effects of group and time. Statistical significance was indicated by P<0.05. All analyses were performed using SPSS19.0 statistical software (SPSS Inc., Chicago, IL).
Results
A total of 70 children were included in the study. Of these, 19 children were either lost to follow-up, had incomplete follow-up, or did not complete IVA-CPT assessment. Therefore, complete data were available for 51 children (35 males and 16 females). A total 26 children had a course of disease ≥5 years, whereas 25 children had a course of disease <5 years. There were 16, 16, and 19 children in the mild, moderate, and severe OSAHS groups, respectively. A total of 42 patients underwent bilateral tonsillectomy plus adenoidectomy and 9 patients underwent adenoidectomy alone.
There were no significant differences in preoperative age, sex, BMI, or course of disease among children with differing levels of OSAHS severity (Table 1).
Table 1.
Preoperative characteristics of children in groups with differing levels of OSAHS1 severity.
| Severity of OSAHS | n | Age (years) | Sex | Preoperative BMI2 | Course of disease (years) | ||
|---|---|---|---|---|---|---|---|
| Male | Female | <5 | ≥5 | ||||
| Mild | 17 | 7.76±1.92 | 11 | 6 | 17.67±4.01 | 8 | 9 |
| Moderate | 18 | 7.33±2.33 | 12 | 6 | 18.11±4.47 | 11 | 7 |
| Severe | 16 | 8.00±2.25 | 12 | 4 | 18.01±4.89 | 6 | 10 |
| F or χ2 | 0.415 | 0.455 | 0.047 | 1.929 | |||
| P | 0.663 | 0.796 | 0.954 | 0.381 | |||
Data are presented as mean ± standard deviation;
OSAHS – obstructive sleep apnea hypopnea syndrome;
BMI – body mass index.
The mean FRCQ, FAQ, and HYP results for the 3 time points are shown in Table 2. The mean values of the 3 indicators were normal or close to normal by 6 months after surgery. The effect of time was significant for FRCQ, FAQ, and HYP. The effect of group/disease severity was significant for FAQ, but not FRCQ or HYP. There was no significant group-by-time interaction for FRCQ, FAQ, or HYP (Table 3).
Table 2.
Comparison of integrated visual and auditory continuous performance testing parameters at different time points in patients of differing severity.
| Severity of OSAHS1 | n | FRCQ2 | FAQ3 | HYP4 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Before surgery | 3 months after surgery | 6 months after surgery | Before surgery | 3 months after surgery | 6 months after surgery | Before surgery | 3 months after surgery | 6 months after surgery | ||
| Mild | 17 | 78.71±8.35 | 86.41±9.50 | 99.18±13.05 | 80.29±6.12 | 86.18±5.63 | 96.94±10.58 | 82.76±7.35 | 89.88±9.47 | 103.06±12.71 |
| Moderate | 18 | 78.61±9.63 | 87.89±11.08 | 100.72±14.23 | 78.44±9.11 | 81.69±7.99 | 94.06±9.51 | 83.89±12.02 | 90.94±13.46 | 102.17±13.85 |
| Severe | 16 | 75.75±7.59 | 82.81±8.65 | 97.06±11.68 | 72.75±7.71 | 78.25±7.05 | 90.69±7.61 | 76.56±9.52 | 83.44±8.39 | 96.44±12.13 |
| Group effect | F=0.669 P=0.517 | F=3.89 P=0.027 | F=2.098 P=0.134 | |||||||
| Time effect | F=292.05 P<0.001* | F=258.27 P<0.001* | F=295.10 P<0.001* | |||||||
| Interaction | F=0.378 P=0.754* | F=0.763 P=0.491* | F=0.403 P=0.774* | |||||||
Data are presented as mean ± standard deviation;
OSAHS – obstructive sleep apnea hypopnea syndrome;
FRCQ – full scale response control quotient;
FAQ – full scale attention quotient;
HYP – hyperactivity;
After G-G correction.
Table 3.
Comparison of integrated visual and auditory continuous performance testing parameters at different time points.
| Parameter | Time | F value | P value |
|---|---|---|---|
| FRCQ1 | Before surgery vs. 3 months after surgery | 210.88 | <0.001 |
| 3 months after surgery vs. 6 months after surgery | 203.58 | <0.001 | |
| FAQ2 | Before surgery vs. 3 months after surgery | 250.43 | <0.001 |
| 3 months after surgery vs. 6 months after surgery | 176.31 | <0.001 | |
| HYP3 | Before surgery vs. 3 months after surgery | 130.89 | <0.001 |
| 3 months after surgery vs. 6 months after surgery | 189.44 | <0.001 |
FAQ – full scale attention quotient.
FRCQ – full scale response control quotient.
HYP – hyperactivity.
The mean AHI and LaSO2 results for the 3 time points are shown in Table 4. There were significant effects of time, group/disease severity, and the group-by-time interaction for both AHI and LaSO2 (Tables 4 and 5).
Table 4.
Comparison of polysomnography findings at different time points in patients of differing severity.
| Severity of OSAHS1 | n | AHI2 | LaSO23 | ||||
|---|---|---|---|---|---|---|---|
| Before surgery | 3 months after surgery | 6 months after surgery | Before surgery | 3 months after surgery | 6 months after surgery | ||
| Mild | 17 | 8.46±1.12 | 4.15±2.3 | 3.12±0.96 | 0.85±0.02 | 0.87±0.04 | 0.89±0.04 |
| Moderate | 18 | 16.21±2.63 | 4.61±0.90 | 4.02±0.99 | 0.77±0.05 | 0.85±0.04 | 0.88±0.04 |
| Severe | 16 | 28.53±10.39 | 6.01±2.72 | 5.05±1.66 | 0.69±0.08 | 0.83±0.06 | 0.85±0.04 |
| Group effect | F=37.96 P<0.001 | F=20.18 P<0.001 | |||||
| Effect of time | F=276.99 P<0.001* | F=95.22 P<0.001* | |||||
| Interaction | F=42.57 P<0.001* | F=9.59 P<0.001* | |||||
Data are presented as mean ± standard deviation;
OSAHS – obstructive sleep apnea hypopnea syndrome;
AHI – apnea-hypopnea index;
LaSO2 – lowest oxygen saturation;
After G-G correction.
Table 5.
Comparison of polysomnography results at different time points.
| Parameter | Time | F value | P value |
|---|---|---|---|
| AHI1 | Before surgery vs. 3 months after surgery | 289.95 | <0.001 |
| 3 months after surgery vs. 6 months after surgery | 16.52 | <0.001 | |
| LaSO22 | Before surgery vs. 3 months after surgery | 78.26 | <0.001 |
| 3 months after surgery vs. 6 months after surgery | 25.96 | <0.001 |
AHI – apnea-hypopnea index;
LaSO2 – lowest oxygen saturation.
Discussion
Generally, disease severity and course of disease are 2 factors that can determine the treatment efficacy and prognosis in most diseases; OSAHS is no exception. Because concurrent poor self-control, attention deficit, and hyperactivity in children with OSAHS may affect quality of life [14], OSAHS is an increasing area of interest and concern for clinicians. Therefore, it is necessary to understand the relationship between the severity of these complications and OSAHS severity, as well as the course of disease.
Previously, the impact of OSAHS on children’ psychological behavior was often assessed using a variety of scales, and the degree of impact was determined by considering physicians’ observations. Owens et al. [15] and Stewart et al. [16] used the Eyberg Child Behavior Scale and the Global Quality of Life Scale to assess 100 and 39 children with OSAHS, respectively, and found that the incidence of abnormal behaviors was significantly higher in children with OSAHS compared with children in the control group. Goldstein et al. [17,18] and Avior et al. [19] used the Achenbach Child Behavior Scale to assess preoperative and postoperative self-control, attention, and hyperactivity in children with OSAHS and found that abnormalities were significantly improved after surgery. Due to limitations in various factors, including expression capability, education level, observation capability, and subjective consciousness, family members’ descriptions and physicians’ observations often do not always objectively, accurately, and quantifiably reflect the true disease condition of children. Therefore, scales are only appropriate for qualitative assessment; performing more accurate quantitative analysis is difficult.
The IVA-CPT is a relatively objective and accurate test for diagnosing of ADHD that produces quantitative results. The test is easy to administer and has associated sensitivity and specificity of up to 92% and 90%, respectively [20]. However, the test must be performed under the guidance of professional examiners to ensure consistency and accuracy. In this study, the IVA-CPT was used to assess the effects of OSAHS on self-control, attention, and hyperactivity in children, and to determine how these factors change after intervention. We chose to use the IVA-CPT because this means of assessment is relatively objective, quantifiable, and simple to use.
The accuracy of IVA-CPT results may to a certain extent be affected by examiner and subject factors. Therefore, examiners must be professional psychologists. In our study, the same professional psychologist performed all IVA-CPT assessments. Children’s medical histories were reviewed before testing to exclude mental abnormalities possibly caused by drugs or non-OSAHS factors. The examiner repeated the instructions and demonstrations so that the children could fully understand and perform proficiently. As computer use is common in everyday life, all children were able to complete the test easily, which helped maximize the accuracy of the study results. The criteria for abnormalities referred to the IVA-CPT-related diagnostic criteria for ADHD – abnormalities were considered to be present if any of the 2 main indicators, FRCQ or FAQ, were abnormal and HYP was abnormal.
Our results showed that the mean psychological behavioral indicators were below the lower limit of normal in children with OSAHS of differing levels of severity. In all 3 groups, the effects time were significant for FRCQ, FAQ, and HYP, and pair-wise comparisons of the 3 indicators between each of the 2 time points also showed significant differences. The results indicate that children with OSAHS had significantly abnormal self-control, attention, and hyperactivity before surgery, and that these abnormalities improved with time after surgery. We also found that the group effects for FRCQ and HYP were not significant, but the group effect for FAQ was significant. The group-by-time interaction was not significant for any of the 3 indicators. These results suggest that the severity of OSAHS was related to the degree of attention deficit. However, the group effects for FRCQ and HYP were not significant, and there were no group-by-time interactions for FRCQ, FAQ, and HYP. Therefore, there is no definite association between OSAHS severity and degree of psychological abnormality and postoperative recovery of this abnormality. Differences in the 3 indicators between the second and third time points were greater than those between the first and second time points, indicating that postoperative recovery of psychological abnormalities in children was more rapid during the period 3–6 months after surgery than during the period 0–3 months after surgery.
AHI and LaSO2 are the main indicators used to assess OSAHS severity. We found that there were significant effects of group, time, and group-by-time interaction for both AHI and LaSO2. The changes in AHI and LaSO2 from time point 1 to 2 were greater than those from time point 2 to 3, indicating that postoperative recovery was more rapid during 0 to 3 months after surgery than during 3 to 6 months after surgery. This pattern of change is different from that observed in the recovery of psychological abnormalities in these children. This suggests that after surgery, patients quickly recover from respiratory obstruction, and after 3 months they will show a substantial decline in AHI. However, psychological abnormalities cause long-term damage; children begin to recover slowly, and then recovery accelerates. This is only our observation, and the mechanism requires further study.
The above results were quite useful to clarify the impact of pediatric OSAHS severity and surgery intervention on psychological and behavioral abnormalities and surgery outcomes, but we should also attach importance to a limitation that 19 subjects dropped-out, which is a high rate. Of these, 10 parents thought that there might be no need for their children to follow up due to good recovery after the operation. In addition, 4 families moved to other cities. Two children had chronic nephritis and 2 were injured in motor vehicle crashes. The remaining 3 patients could not be reached though their registered addresses and phone numbers. Therefore, only some of the 19 patients had follow-up PSG and IVA-CPT assessments after surgery. To allow more definitive conclusions, larger trials are needed to verify these results.
Conclusions
OSAHS might have a significant impact on self-control, attention, and hyperactivity in children. Psychological and behavioral abnormalities show a gradual recovery after surgical intervention. The severity of OSAHS is not closely related to the severity of psychological and behavioral abnormalities caused by OSAHS, or to the postoperative recovery of these abnormalities. Therefore, according to OSAHS severity alone, it may be extremely difficult to determine the severity of pediatric psychological and behavioral abnormalities caused by OSAHS or to predict postoperative recovery.
Footnotes
Source of support: This work was supported by grants from Science and Technology Development Project of Hangzhou (No: 20100633B03) and Science and Technology Plan Program of Zhejiang Province (No: 2012C33036)
Conflicts of interest statement
None declared.
References
- 1.Hiscock H, Canterford L, Ukoumunne OC, Wake M. Adverse associations of sleep problems in Australian preschoolers: National population study. Pediatrics. 2007;119:86–93. doi: 10.1542/peds.2006-1757. [DOI] [PubMed] [Google Scholar]
- 2.Ray RM, Bower CM. Pediatric obstructive sleep apnea: The year in review. Curr Opin Otolaryngol Head Neck Surg. 2005;13:360–65. doi: 10.1097/01.moo.0000186076.53986.71. [DOI] [PubMed] [Google Scholar]
- 3.Brunetti L, Rana S, Lospalluti ML, et al. Prevalence of obstructive sleep apnea syndrome in a cohort of 1,207 children of southern Italy. Chest. 2001;120:1930–35. doi: 10.1378/chest.120.6.1930. [DOI] [PubMed] [Google Scholar]
- 4.Kurnatowski P, Putynski L, Lapienis M, Kowalska B. Neurocognitive abilities in children with adenotonsillar hypertrophy. Int J Pediatr Otorhinolaryngol. 2006;70:419–24. doi: 10.1016/j.ijporl.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 5.Ali NJ, Pitson DJ, Stradling JR. Snoring, sleep disturbance, and behaviour in 4–5 year olds. Arch Dis Child. 1993;68:360–66. doi: 10.1136/adc.68.3.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gozal D. Sleep-disordered breathing and school performance in children. Pediatrics. 1998;102:616–20. doi: 10.1542/peds.102.3.616. [DOI] [PubMed] [Google Scholar]
- 7.Rosen CL, Palermo TM, Larkin EK, Redline S. Health-related quality of life and sleep-disordered breathing in children. Sleep. 2002;25:657–66. [PubMed] [Google Scholar]
- 8.Ali NJ, Pitson D, Stradling JR. Sleep disordered breathing: Effects of adenotonsillectomy on behaviour and psychological functioning. Eur J Pediatr. 1996;155:56–62. doi: 10.1007/BF02115629. [DOI] [PubMed] [Google Scholar]
- 9.Youssef NA, Ege M, Angly SS, et al. Is obstructive sleep apnea associated with ADHD. Ann Clin Psychiatry. 2011;23:213–24. [PubMed] [Google Scholar]
- 10.Tinius TP. The Integrated Visual and Auditory Continuous Performance Test as a neuropsychological measure. Arch Clin Neuropsychol. 2003;18:439–54. [PubMed] [Google Scholar]
- 11.Gruber R, Grizenko N, Schwartz G, et al. Performance on the continuous performance test in children with ADHD is associated with sleep efficiency. Sleep. 2007;30:1003–9. doi: 10.1093/sleep/30.8.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Editorial Board of Chinese Journal of Otorhinolaryngology and Head and Neck Surgery, Otolaryngology Branch of Chinese Medical Association. Draft guideline for the diagnosis and treatment of OSAHS in children (Urumqi) Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2007;42:83–84. [PubMed] [Google Scholar]
- 13.Edwards G. Determining the role of a new continuous performance test in the diagnostic evaluation for ADHD. ADHD Report. 1998;6:11–13. [Google Scholar]
- 14.Nelson R. Obstructive sleep apnoea in children might impair cognition and behaviour. Lancet. 2002;359:1754. doi: 10.1016/S0140-6736(02)08666-X. [DOI] [PubMed] [Google Scholar]
- 15.Owens J, Opipari L, Nobile C, Spirito A. Sleep and daytime behavior in children with obstructive sleep apnea and behavioral sleep disorders. Pediatrics. 1998;102:1178–84. doi: 10.1542/peds.102.5.1178. [DOI] [PubMed] [Google Scholar]
- 16.Stewart MG, Glaze DG, Friedman EM, et al. Quality of life and sleep study findings after adenotonsillectomy in children with obstructive sleep apnea. Arch Otolaryngol Head Neck Surg. 2005;131:308–14. doi: 10.1001/archotol.131.4.308. [DOI] [PubMed] [Google Scholar]
- 17.Goldstein NA, Post JC, Rosenfeld RM, Campbell TF. Impact of tonsillectomy and adenoidectomy on child behavior. Arch Otolaryngol Head Neck Surg. 2000;126:494–98. doi: 10.1001/archotol.126.4.494. [DOI] [PubMed] [Google Scholar]
- 18.Goldstein NA, Fatim AM, Campbell TF, Rosenfeld RM. Child behavior and quality of life before and after tonsillectomy and adenoidectomy. Arch Otolaryngol Head Neck Surg. 2002;128:770–75. doi: 10.1001/archotol.128.7.770. [DOI] [PubMed] [Google Scholar]
- 19.Avior G, Fishman G, Leor A, et al. The effect of tonsillectomy and adenoidectomy on inattention and impulsivity as measured by the Test of Variables of Attention (TOVA) in children with obstructive sleep apnea syndrome. Arch Otolaryngol Head Neck Surg. 2004;131:367–71. doi: 10.1016/j.otohns.2004.04.015. [DOI] [PubMed] [Google Scholar]
- 20.Quinn CA. Detection of malingering in assessment of adult ADHD. Arch Clin Neuropsychol. 2003;18:379–95. [PubMed] [Google Scholar]