Abstract
Objectives
To evaluate safety and efficacy of weekly (qw) and every other week (q2w) dosing of sarilumab, a fully human anti-interleukin 6 receptor α (anti-IL-6Rα) monoclonal antibody, for moderate-to-severe rheumatoid arthritis (RA).
Methods
In this dose-ranging study, patients (n=306) with active RA, despite methotrexate, were randomly assigned to placebo or one of five subcutaneous doses/regimens of sarilumab: 100 mg q2w, 150 mg q2w, 100 mg qw, 200 mg q2w, 150 mg qw for 12 weeks, plus methotrexate. The primary end point was ACR20 at Week 12. Secondary endpoints included ACR50, ACR70, Disease Activity Score in 28 joints (C reactive protein). Safety, pharmacokinetics, pharmacodynamics and efficacy in population subgroups were assessed.
Results
The proportion of patients achieving an ACR20 response compared with placebo was significantly higher for sarilumab 150 mg qw (72.0% vs 46.2%, multiplicity adjusted p=0.0203). Higher ACR20 responses were also attained with 150 mg q2w (67%; unadjusted (nominal) p=0.0363) and 200 mg q2w (65%; unadjusted p=0.0426) versus placebo. Sarilumab ≥150 mg q2w reduced C reactive protein, which did not return to baseline between dosing intervals. Infections were the most common adverse event; none were serious. Changes in laboratory values (neutropenia, transaminases and lipids) were consistent with reports with other IL-6Rα inhibitors.
Conclusions
Sarilumab improved signs and symptoms of RA over 12 weeks in patients with moderate-to-severe RA with a safety profile similar to reports with other IL-6 inhibitors. Sarilumab 150 mg and sarilumab 200 mg q2w had the most favourable efficacy, safety and dosing convenience and are being further evaluated in Phase III.
Keywords: Rheumatoid Arthritis, Treatment, Cytokines, DMARDs (biologic)
Introduction
Therapies in rheumatoid arthritis (RA) have evolved from symptomatic treatments to non-biological disease modifying antirheumatic drugs (DMARDs) such as methotrexate (MTX).1 2 Over the past 15 years, biological immunomodulating therapies have been shown to slow the progression of joint damage and improve the clinical manifestations of RA superior to DMARDs. Nine agents, in five therapeutic classes, are approved for clinical use in Europe and USA.3–11 The risk of disease progression persists in patients with RA who do not respond completely to currently available treatment options.12 Therefore, unmet needs in the treatment of RA still exist, and additional therapies are needed. Interleukin 6 (IL-6) is a key driver of inflammation, and is elevated in the serum and synovial fluid of patients with RA.13 Tocilizumab, a humanised monoclonal antibody (mAb) directed against IL-6 receptor α (IL-6Rα) has been shown to be an effective treatment option, either as monotherapy or in combination with non-biological DMARDS, for many patients with an inadequate response to one or more DMARDs or antitumour necrosis factor agents, or in whom DMARDs are contraindicated.14–19
Sarilumab (SAR153191/REGN88) is a fully human anti-IL-6Rα mAb that binds membrane-bound and soluble human IL-6Rα with high affinity thereby blocking cis and trans IL-6-mediated inflammatory signalling cascade, and with no evidence of complement-dependent or antibody-dependent cell-mediated cytotoxicity.20 Sarilumab has been shown in preclinical studies to inhibit IL-6 signalling in a dose-dependent manner.21–23 In Phase I studies subcutaneous sarilumab was generally well tolerated and, in patients with RA,24 25 reduced acute phase reactants including C reactive protein (CRP).24 26
Results from the dose ranging study, Part A of the MOnoclonal antiBody to IL-6Rα In RA patients: A pivotal Trial with X-raY (MOBILITY) seamless-design Phase II/III study (NCT01061736), are reported here. The primary objective was to demonstrate that sarilumab dosed qw or q2w plus MTX is effective in reducing the signs and symptoms of RA at week 12 in patients with active RA who have inadequate response to MTX, and to select one or more dose regimens to be evaluated in the pivotal Phase III MOBILITY Part B study. Key secondary objectives were to assess the safety of sarilumab in combination with MTX, and to document its pharmacokinetic (PK) and pharmacodynamic (PD) profile. Exploratory objectives included an analysis of sarilumab efficacy in a wide range of population subgroups to test the robustness of the therapeutic activity of the drug.
Methods
Patients and study design
MOBILITY Part A was a Phase II, randomised, double-blind, placebo-controlled, multicentre, dose-ranging study conducted between March 2010 and May 2011; patients fulfilled the American College of Rheumatology (ACR) revised criteria for the diagnosis of RA.27 Patients were 18–75 years of age, had active RA (swollen joint count ≥6, tender joint count ≥8, and CRP ≥1 mg/dL) of at least 3 months duration despite MTX treatment for a minimum of 12 weeks, stable dose (10–25 mg/week) for at least 6 weeks prior to the screening visit. Details of patient inclusion and exclusion criteria, assessment measures and study treatment are provided in the online supplement.
The study duration was 22 weeks, comprised of 4 weeks screening, 12 weeks treatment and 6 weeks post-treatment follow-up. Patients were randomised to placebo or to one of five subcutaneous sarilumab doses (100 mg q2w (200 mg total monthly dose), 150 mg q2w (300 mg total monthly dose), 100 mg qw (400 mg total monthly dose), 200 mg q2w (400 mg total monthly dose) and 150 mg qw (600 mg total monthly dose)) (see online supplementary figure S1). Randomisation was performed centrally with allocation generated by interactive voice response system, stratified by region and prior biological use. All patients and investigators were blinded to the study treatments. The protocol was approved by ethics committees/institutional review boards within each country, and each patient gave informed consent. The study was conducted in compliance with Institutional Review Board regulations, International Conference on Harmonisation Good Clinical Practice guidelines and the Declaration of Helsinki. Patients who completed the 12-week treatment period, and if eligible, could enter an open-label, long-term extension study (SARIL-RA-EXTEND, NCT01146652).
Efficacy assessments
The efficacy population included all randomised patients who had received at least one dose of study drug and had at least one postbaseline assessment. The primary end point was the proportion of patients who achieved improvement of ≥20% according to the ACR criteria (ACR20 response rate) at Week 12.28 Secondary end points included ACR50 and ACR70 responses, change from baseline in individual disease activity measures (swollen joint count, tender joint count, physician and patient global assessment of disease activity, patient's pain score, CRP, Health Assessment Questionnaire score), as well as Disease Activity Score in 28 joints (DAS28(CRP)).29 Disease remission was defined as DAS28(CRP) score <2.6.
Safety assessments
The safety population consisted of all randomised patients who received at least one dose of study drug. Safety assessments included monitoring of vital signs, 12-lead ECGs and physical examinations, adverse events (AEs), clinical laboratory analyses of haematology, serum biochemistry, immunological parameters and urine. Treatment-emergent AEs were defined as AEs which developed, worsened or became serious on or after the first sarilumab dose, up to the end of the study.
Bioanalytical methods
Functional sarilumab assay
Functional sarilumab levels in human serum were measured using a validated ELISA. In this assay, the levels of sarilumab with either one or two available binding sites were measured. The assay does not detect sarilumab with both binding sites occupied (fully bound sarilumab). The functional assay employs human IL-6Rα as the capture reagent and a biotinylated goat polyclonal antibody specific for human κ light chain as the detection reagent. The lower limit of quantification of the assay is 294 ng/mL of functional sarilumab in neat human serum.
Bound sarilumab assay
Bound sarilumab levels in human serum were measured using a validated direct ELISA. This assay measures the levels of IL-6Rα:sarilumab complex. It does not detect sarilumab that is not in complex with IL-6Rα (free sarilumab). The bound assay employs a mouse mAb selective for IL-6Rα as the capture reagent and a horseradish peroxidase conjugated goat polyclonal antibody specific for the human κ light chain as the detection reagent. The lower limit of quantification of the assay is 662 ng/mL of bound sarilumab in neat human serum.
IL-6 assay
IL-6 was measured using the ELISA-based Quantikine Human IL-6 Immunoassay (R&D Systems, Minneapolis, Minnesota, USA).
Sample size calculation
Sample size calculations were performed assuming an ACR20 response rate of 75% in at least one sarilumab dose group versus a placebo response rate of 40%. With 50 patients per group, the study had approximately 80% power to detect a difference of 35% between sarilumab and placebo using a two-sided test with α=0.01. The difference of 35% between groups was based on available data from approved biological DMARDs (etanercept, infliximab, adalimumab and tocilizumab).3–5 11
Statistical analysis
Primary efficacy
The primary endpoint, the ACR20 response rate at Week 12, was assessed in the intent-to-treat population, which included all randomised patients, and was analysed according to the treatment group allocated by randomisation. ACR20 response rate was analysed using the two-sided Cochran-Mantel-Haenszel test stratified by prior biological use and geographical region. Pairwise comparisons for the response rates between each dose of sarilumab and placebo were derived by testing each active dose group versus placebo separately. The Mantel-Haenszel estimate of the OR and the corresponding 95% CI were derived by testing each active dose group versus placebo separately. Details of data handling for patients who discontinued study treatment, correction for the multiplicity that arose from testing multiple doses of sarilumab against placebo, and sensitivity analysis are provided in the online supplement.
Secondary efficacy
The secondary efficacy end points were also analysed as described above. An analysis of covariance (ANCOVA) model, including terms for baseline, treatment, prior biological use and region, was used to assess treatment differences in the change from baseline for each of the seven ACR components and for DAS28(CRP). Descriptive statistics and post hoc correction for multiplicity in the secondary efficacy end points of ACR50 and ACR70 are provided in the online supplement. Sarilumab efficacy was also analysed in a number of subgroups by testing treatment-by-subgroup interaction terms and statistically significant interaction indicated differential drug effect within the corresponding subgroups.
Safety analysis
All safety data were summarised descriptively based on the safety population. Summarisation of treatment emergent adverse events (TEAEs) was based on Medical Dictionary for Regulatory Activities coding of verbatim terms reported by investigators. The safety and PK analyses sets included patients who received at least one dose of sarilumab and who provided at least one qualified sample.
Results
Patients
Three hundred and six patients who met the inclusion criteria were randomly allocated among six treatment groups (figure 1). A total of 305 patients received study treatment. One patient from the placebo group who had received a single 150 mg q2w dose in error was considered to be in the placebo group for efficacy analyses but in the 150 mg q2w group for safety and PK analyses. One patient in the 200 mg q2w group who did not receive treatment was included in the 200 mg q2w group for efficacy analysis, but excluded from the safety analysis. Three patients in the placebo group and 32 in the sarilumab group discontinued treatment before Week 12 due to AEs or lack of efficacy. Baseline demographic and disease characteristics of the treatment groups were similar (table 1). The mean duration of RA was approximately 8 years and for those patients with a prior use of biological DMARDs, the majority had been previously treated with one, some with two, but none with three.
Figure 1.
Patient disposition. Not randomised=patients who did not meet inclusion criteria. SAR, sarilumab; q2w, every 2 weeks; qw, every week; MTX, methotrexate; all patients were required to receive and tolerate a minimum of 12 weeks of MTX treatment prior to the randomisation visit with a stable dose for 6 weeks prior to screening. All randomised patients received assigned treatment except one patient randomised to the placebo group who received in error a single 150 mg q2w dose (between days 57 and 78), and one patient randomised to the SAR 200 mg q2w group who did not receive study treatment.
Table 1.
Demographics and baseline characteristics
| Placebo (n=52) | SAR 100 mg q2w (n=51) | SAR 150 mg q2w (n=51) | SAR 100 mg qw (n=50) | SAR 200 mg q2w (n=52) | SAR 150 mg qw (n=50) | All (n=306) | |
|---|---|---|---|---|---|---|---|
| Population | |||||||
| Age, mean (SD) | 55.2 (12.5) | 53.5 (11.8) | 51.2 (12.9) | 53.9 (12.3) | 48.7 (12.4) | 50.9 (11.1) | 52.2 (12.3) |
| Female, N (%) | 38 (73.1) | 38 (74.5) | 42 (82.4) | 41 (82.0) | 42 (80.8) | 42 (84.0) | 243 (79.4) |
| Caucasian/White, N (%) | 49 (94.2) | 49 (96.1) | 49 (96.1) | 47 (94.0) | 47 (90.4) | 46 (92.0) | 287 (93.8) |
| Region, N (%) | |||||||
| Western countries | 16 (30.8) | 15 (29.4) | 16 (31.4) | 14 (28.0) | 16 (30.8) | 17 (34.0) | 94 (30.7) |
| South America | 13 (25.0) | 14 (27.5) | 13 (25.5) | 13 (26.0) | 14 (26.9) | 13 (26.0) | 80 (26.1) |
| Rest of the world | 23 (44.2) | 22 (43.1) | 22 (43.1) | 23 (46.0) | 22 (42.3) | 20 (40.0) | 132 (43.1) |
| Baseline Disease Characteristics | |||||||
| Duration of RA (years), mean (SD) | 8.07 (8.62) | 9.76 (9.08) | 7.74 (7.20) | 8.07 (8.68) | 5.95 (6.18) | 7.30 (8.28) | 7.81 (8.08) |
| Average MTX dose (mg/wk), mean (SD) | 16.9 (4.2) | 16.2 (4.1) | 17.1 (6.4) | 16.7 (3.5) | 16.6 (3.8) | 16.4 (4.9) | 16.6 (4.5) |
| Prior biological DMARD use, N (%) | 12 (23.1) | 13 (25.5) | 12 (23.5) | 12 (24.0) | 14 (26.9) | 12 (24.0) | 75 (24.5) |
| RF positive, N (%) | 35 (67.3) | 42 (82.4) | 44 (86.3) | 35 (70.0) | 44 (86.3) | 43 (86.0) | 243 (79.7) |
| Anti-CCP antibody positive, N (%) | 16 (72.7) | 16 (80.0) | 21 (95.5) | 14 (70.0) | 20 (87.0) | 18 (85.7) | 105 (82.0) |
| TJC (0–68), mean (SD) | 27.09 (16.12) | 30.31 (14.68) | 26.94 (16.79) | 29.12 (15.36) | 25.52 (14.21) | 25.36 (11.97) | 27.39 (14.93) |
| SJC (0–66), mean (SD) | 17.45 (11.68) | 19.53 (9.46) | 17.59 (10.60) | 16.76 (9.05) | 16.63 (8.94) | 16.29 (8.33) | 17.38 (9.73) |
| DAS28(CRP), mean (SD) | 6.08 (0.86) | 6.28 (0.92) | 6.11 (0.91) | 6.05 (0.79) | 6.06 (0.90) | 6.07 (0.65) | 6.11 (0.84) |
| CRP (mg/L), median | 21.8 | 19.8 | 17.6 | 17.0 | 19.0 | 17.1 | 19.2 |
All patients received methotrexate (MTX) 10–25 mg/week.
anti-CCP, anti-cyclic citrullinated peptide; CRP, C reactive protein; DAS28, disease activity score 28 joint count; DMARDs, disease-modifying antirheumatic drugs; q2w, every 2 weeks; qw, every week; RA, rheumatoid arthritis; RF, rheumatoid factor; SAR, sarilumab; SJC, swollen joint count; TJC, tender joint count.
Primary efficacy end point
The highest dose group, 150 mg qw, achieved an ACR20 response rate of 72% at Week 12 compared with 46.2% in the placebo group (unadjusted (nominal) p=0.0041; Hommel-adjusted (for multiplicity) p=0.0203) (figure 2A). An ACR20 response at Week 12 was also achieved by 67% of patients receiving 150 mg q2w (unadjusted p=0.0363) and 65% with 200 mg q2w (unadjusted p=0.0426). ACR20 results for other dose groups are shown in figure 2A, with the 100 mg q2w dose identified as a non-efficacious treatment group.
Figure 2.
ACR and DAS28(CRP) response, week 12. (A) ACR20, (B) ACR50, (C) ACR70 at week 12, (D) improvement from baseline, and (E) number of patients in remission defined as DAS28(CRP) <2.6. ACR20/50/70 indicates at least 20%, 50% or 70% improvement in tender and swollen joint counts as well as at least 20%, 50% or 70% improvement in three of the other five ACR components. Panel A shows unadjusted (nominal) p values; *adjusting for multiplicity resulted in significance for the highest dose group as discussed in the text. Unadjusted p values are shown in panels B, C, D and E; Bonferroni adjustment for multiplicity considers p value <0.01 statistically significant. ACR, American College of Rheumatology; DAS28, disease activity score 28 joint count; MTX, methotrexate; q2w, every 2 weeks; qw, every week; SAR, sarilumab.
Secondary efficacy end points
For ACR50 and ACR70 response rates, as well as DAS28(CRP) improvement from baseline, sarilumab doses of 150 mg q2w and higher resulted in numerical rates substantially better than placebo, most with unadjusted p values <0.05 (figures 2B–D); these doses also led to improvement in the clinical components of the ACR assessment (table 2). Evaluation of DAS28(CRP) suggested a dose response with highest incidence DAS28(CRP) <2.6 in the 150 mg qw group (figure 2E). Although not a prespecified end point, clinical disease activity index (CDAI) scores at baseline and 12 weeks are shown in online supplementary table S1.
Table 2.
Change from baseline in ACR components at Week 12
| Placebo (n=52) LS Mean (SE) |
SAR 100 mg q2w (n=51) LS Mean (SE) |
SAR 150 mg q2w (n=51) LS Mean (SE) |
SAR 100 mg qw (n=50) LS Mean (SE) |
SAR 200 mg q2w (n=52) LS Mean (SE) |
SAR 150 mg qw (n=50) LS Mean (SE) |
|
|---|---|---|---|---|---|---|
| TJC (0–68) p Value vs placebo |
−8.72 (1.69) | −11.87 (1.70) 0.1740 |
−15.64 (1.70) 0.0029 |
−14.43 (1.73) 0.0151 |
−14.57 (1.69) 0.0118 |
−12.84 (1.72) 0.0772 |
| SJC (0–68) p Value vs placebo |
−6.74 (1.13) | −5.97 (1.13) 0.6184 |
−9.36 (1.14) 0.0894 |
−9.93 (1.16) 0.0410 |
−10.16 (1.12) 0.0268 |
−8.87 (1.15) 0.1698 |
| Pain (VAS) p Value vs placebo |
−22.28 (3.46) | −21.02 (3.47) 0.7899 |
−29.05 (3.49) 0.1531 |
−29.19 (3.55) 0.1499 |
−32.46 (3.48) 0.0332 |
−25.26 (3.51) 0.5312 |
| Physician global (VAS) p Value vs placebo |
−26.79 (2.88) | −28.85 (2.89) 0.6021 |
−34.32 (2.90) 0.0559 |
−35.20 (2.95) 0.0347 |
−39.66 (2.89) 0.0012 |
−34.91 (2.92) 0.0410 |
| Patient global (VAS) p Value vs placebo |
−21.10 (3.39) | −20.12 (3.40) 0.8312 |
−27.57 (3.42) 0.1636 |
−30.22 (3.47) 0.0522 |
−31.66 (3.41) 0.0241 |
−27.80 (3.44) 0.1515 |
| HAQ-DI p Value vs placebo |
−0.26 (0.07) | −0.35 (0.07) 0.3527 |
−0.62 (0.07) 0.0003 |
−0.42 (0.07) 0.0997 |
−0.57 (0.07) 0.0019 |
−0.45 (0.07) 0.0545 |
| CRP p Value vs placebo |
−3.1 (2.8) | −10.2 (2.8) 0.0661 |
−21.9 (2.8) <0.0001 |
−25.0 (2.9) <0.0001 |
−21.9 (2.8) <0.0001 |
−20.7 (2.9) <0.0001 |
All patients received methotrexate 10–25 mg/week. To adjust for multiplicity p values <0.01 can be regarded as statistically significant.
CRP, C-reactive protein (mg/L); HAQ-DI, health assessment questionnaire disability index; LS, least-square; q2w, every 2 weeks; qw, every week; SAR, sarilumab; SJC, swollen joint count; TJC, tender joint count; VAS, visual analogue scale.
Compared with placebo, as expected with an antibody to IL-6, sarilumab doses higher than 150 mg q2w produced a prompt and sustained suppression of CRP (figure 3). By Week 4 the median percentage change in CRP from baseline was −85%, −95%, −95% and −97%, respectively in the 150 mg q2w, 100 mg qw, 200 mg q2w and 150 mg qw groups, compared with −11% in the placebo group. The maximum CRP suppression achieved in each of the treatment groups was maintained to Week 12. In each of the three q2w doses, CRP levels did not return to baseline values at the end of the dosing intervals. However, only the 150 mg and 200 mg q2w doses substantially reduced CRP values throughout the study.
Figure 3.
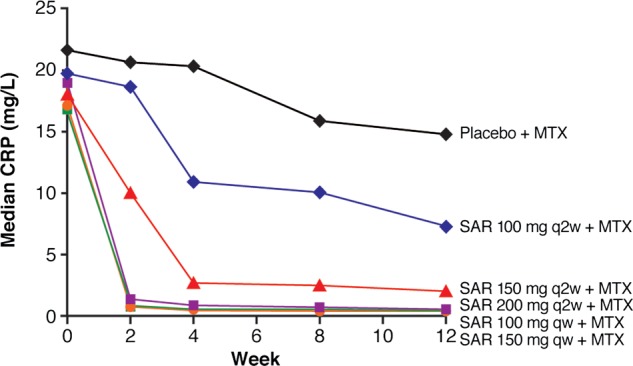
Change in CRP serum levels over time. CRP, C-reactive protein; MTX, methotrexate 10 to 25 mg/week; q2w, every 2 weeks; qw, every week; SAR, sarilumab.
Testing of treatment-by-subgroup interactions indicated that sarilumab efficacy was not influenced by gender, race, age, geographical region, weight, body mass index (BMI), prior biological use, rheumatoid factor or cyclic citrullinated peptide antibody positivity, baseline CRP, smoking history, duration of RA disease or number of prior DMARDs (see online supplementary tables S2 and S3). In online supplementary table S3, the incidence of ACR20 response comparing patients with and without prior biological use suggests there is no significant difference between these subgroups.
Safety
Table 3 summarises the key safety results. Incidence rates of any TEAE were 47% for placebo and between 43% and 72% across the sarilumab groups (table 3A). Twenty-four patients discontinued treatment due to a TEAE; 13 of these patients were in the 100 mg qw dose group with between 1 and 4 patients in each of the other groups. Infection and protocol-mandated discontinuation due to neutropenia were the primary reasons for treatment discontinuations; 2 patients discontinued treatment due to infection (1 patient in the 100 mg qw group, who experienced an Escherichia coli urinary tract infection, and 1 patient in the 150 mg q2w group, who experienced herpes zoster infection). There was no dose trend in the incidence of serious adverse events (table 3A,B). One death from stroke/acute respiratory distress syndrome occurred in the non-efficacious 100 mg q2w group. The investigator judged the acute respiratory distress syndrome to be potentially drug related, and the stroke to be unrelated.
Table 3.
Safety parameters
| Primary system organ class preferred term | Placebo (n=51) N (%) |
SAR 100 mg q2w (n=51) N (%) |
SAR 150 mg q2w (n=52) N (%) |
SAR 100 mg qw (n=50) N (%) |
SAR 200 mg q2w (n=51) N (%) |
SAR 150 mg qw (n=50) N (%) |
|---|---|---|---|---|---|---|
| (A) Safety overview | ||||||
| Any TEAE | 24 (47.1) | 22 (43.1) | 28 (53.8) | 36 (72.0) | 33 (64.7) | 27 (54.0) |
| Any treatment-emergent SAE | 2 (3.9) | 3 (5.9) | 0 | 3 (6.0) | 0 | 0 |
| Any TEAE leading to treatment discontinuation | 2 (3.9) | 4 (7.8) | 2 (3.8) | 13 (26.0) | 4 (7.8) | 3 (6.0) |
| Deaths | 0 | 1 | 0 | 0 | 0 | 0 |
| (B) Treatment-emergent serious adverse events | ||||||
| Basal cell carcinoma | 1 (2.0) | 0 | 0 | 0 | 0 | 0 |
| Plasmacytoma | 0 | 1 (2.0) | 0 | 0 | 0 | 0 |
| Squamous cell carcinoma | 1 (2.0) | 0 | 0 | 0 | 0 | 0 |
| Neutropenia | 0 | 0 | 0 | 1 (2.0) | 0 | 0 |
| Hypersensitivity | 0 | 0 | 0 | 1 (2.0) | 0 | 0 |
| Cerebrovascular accident | 0 | 1 (2.0) | 0 | 0 | 0 | 0 |
| Acute respiratory distress syndrome | 0 | 1 (2.0) | 0 | 0 | 0 | 0 |
| Alcoholic pancreatitis | 0 | 0 | 0 | 1 (2.0) | 0 | 0 |
| Arthralgia | 1 (2.0) | 0 | 0 | 0 | 0 | 0 |
| RA | 0 | 1 (2.0) | 0 | 0 | 0 | 0 |
| (C) TEAEs occurring in ≥5% of patients | ||||||
| Infections and infestations | 7 (13.7) | 6 (11.8) | 12 (23.1) | 13 (26.0) | 12 (23.5) | 10 (20.0) |
| Nasopharyngitis | 3 (5.9) | 2 (3.9) | 2 (3.8) | 2 (4.0) | 2 (3.9) | 1 (2.0) |
| Upper respiratory tract infection | 2 (3.9) | 0 | 2 (3.8) | 1 (2.0) | 3 (5.9) | 2 (4.0) |
| Urinary tract infection | 1 (2.0) | 1 (2.0) | 1 (1.9) | 3 (6.0) | 1 (2.0) | 0 |
| Blood and lymphatic system disorders | 0 | 1 (2.0) | 1 (1.9) | 9 (18.0) | 11 (21.6) | 6 (12.0) |
| Neutropenia | 0 | 0 | 1 (1.9) | 7 (14.0) | 10 (19.6) | 5 (10.0) |
| Musculoskeletal/connective tissue | 5 (9.8) | 5 (9.8) | 1 (1.9) | 1 (2.0) | 2 (3.9) | 5 (10.0) |
| RA | 1 (2.0) | 2 (3.9) | 0 | 0 | 0 | 3 (6.0) |
| Investigations | 3 (5.9) | 0 | 4 (7.7) | 3 (6.0) | 3 (5.9) | 2 (4.0) |
| ALT increased | 0 | 0 | 3 (5.8) | 2 (4.0) | 2 (3.9) | 2 (4.0) |
| Injury/poisoning/procedural complications | 6 (11.8) | 1 (2.0) | 5 (9.6) | 2 (4.0) | 6 (11.8) | 3 (6.0) |
| Accidental overdose* | 5 (9.8) | 1 (2.0) | 3 (5.8) | 2 (4.0) | 2 (3.9) | 3 (6.0) |
All patients received methotrexate 10–25 mg/week.
*Accidental overdose was defined as the administration of at least twice the treatment dose during an interval of less than 6 days (qw regimen) or less than 11 days (q2w regimen). There were no adverse events associated with these protocol-defined overdoses.
ALT, alanine aminotransferase; q2w, every 2 weeks; qw, every week; RA, rheumatoid arthritis; SAE, serious adverse event; SAR, sarilumab; TEAE, treatment-emergent adverse event.
Table 3C shows those TEAEs that occurred in >5% of patients in any treatment group. Fifteen patients (14 (5.5%) on sarilumab; 1 (2.0%) on placebo) experienced injection site reactions. All were mild to moderate in intensity with the exception of one patient who experienced a severe reaction, as assessed by the investigator, which led to permanent treatment discontinuation. Sixteen patients (11 on sarilumab; 5 on placebo) reported ‘accidental overdose’ (defined in the protocol as dosed outside the dosing administration window); no AEs were associated with these protocol-defined ‘overdoses’. Other AEs and safety data are reported in the online supplement.
Neutropenia (Grade 1, absolute neutrophil count (ANC)≥1500–<2000) was reported in one patient in the placebo group. There was a general dose-related reduction in neutrophil count during treatment with sarilumab (figure 4A). In the 100 mg qw, 200 mg q2w and 150 mg qw groups, ANC≥500–<1000 was reported in three, six and four patients, respectively. ANC<500 was reported in the 200 mg q2w (four patients) and 150 mg qw (one patient) groups. Of the 13 patients in the 100 mg qw group who discontinued treatment due to TEAE, 2 discontinuations were due to ANC≥500–<1000 and 4 due to ANC<500. The 150 mg q2w dose group yielded a relatively small average decrease from baseline in neutrophil count at Week 12 (figure 4A).
Figure 4.
Change in laboratory values over time. Total neutrophil count (A), alanine aminotransferase (ALT) (B), high density lipoprotein (HDL) (C) and low density lipoprotein (LDL) (D). MTX, methotrexate 10 to 25 mg/week; q2w, every 2 weeks; qw, every week; SAR, sarilumab.
‘Infections and infestations’ were the most common TEAEs, and the incidence was greater than placebo in patients treated with doses of 150 mg q2w and higher. The proportion of patients with infections was 14% in patients treated with placebo. There were no serious infections. One patient developed herpes zoster that was limited to one dermatome.
Infection rates in patients on sarilumab did not appear to be associated with neutropenia. For sarilumab-treated patients with ANC>2000 (normal), infection was reported in 24%. Among those with ANC≥1500 and <2000, ANC≥1000 and <1500, and ANC<1000, infection was reported in 13% (4/32), 13% (4/30), and 22% (4/18), respectively. Among sarilumab-treated patients within the effective q2w dose groups (pooled 150 mg and 200 mg q2w doses), the proportions of patients with infections was 29% in patients with ANC>2000 (normal), 15% in patients with ANC≥1500 and <2000, 8% in patients with ANC≥1000 and <1500, and 14% in patients with ANC <1000.
Sarilumab doses of 150 mg q2w and higher produced an increase in alanine aminotransferase (ALT) level during the dosing period (figure 4B). Elevation in ALT >3–≤5× upper limit of normal (ULN), was reported in seven sarilumab-treated patients (150 mg q2w (four patients), 100 mg qw (two patients) and 150 mg qw (one patient)). Elevation in ALT >5–≤10×ULN was reported in four sarilumab-treated patients (100 mg qw (one patient), 200 mg q2w (one patient) and 150 mg qw (two patients)). In general, these abnormalities resolved on treatment or at the end of the study. No patients in the placebo group experienced ALT >3×ULN during the dosing period. The incidence of categorical changes in aspartate transaminase (AST) was similar to changes in ALT (data not shown). One patient had a bilirubin of 1.58× ULN.
Overall, lipid changes occurred early and the mean change in high density lipoprotein (HDL) and low density lipoprotein (LDL) cholesterol from baseline at Week 12 was similar in all active treatment groups (figure 4C,D). At Week 12 mean total cholesterol was higher in the four highest dose groups; the increase from baseline was 9.4%, 10%, 16.4% and 21.1%, respectively in the 150 mg q2w, 100 mg qw, 200 mg q2w and 150 mg qw groups, compared with 4.9% in the placebo group.
Pharmacokinetic and pharmacodynamic assessments
Prior Phase I studies have demonstrated that the clearance of sarilumab is biphasic, consistent with target mediated clearance that is revealed at low drug concentrations.30 In this study, trough levels of functional sarilumab in serum increased in a dose-related manner. At Week 12, the geometric mean and median concentrations were above zero at the end of the dosing interval for all doses except for 100 mg q2w. Geometric mean and median concentrations for q2w dosing were 0.78 and 2995 ng/mL for 150 mg and 995.12 and 12 960 ng/mL for 200 mg. Geometric mean and median concentrations for qw dosing were 5794.19 and 15 100 ng/mL for 100 mg and 3205.14 and 36 900 ng/mL for 150 mg. Functional and bound sarilumab trough levels are shown in online supplementary figure S2.
Sarilumab doses of 100 mg qw, 200 mg q2w and 150 mg qw were associated with rapid suppression of CRP (figure 3). Sarilumab 150 mg q2w also suppressed CRP but more slowly than higher doses. The effect of 100 mg q2w was modest. Sarilumab doses of 150 mg q2w or higher continued to suppress CRP throughout the dosing interval regardless of whether the drug was administered weekly or every other week (figure 3).
Concentrations of IL-6 increased as has been reported for other IL-6 blockers (see online supplementary figure 2C).
Discussion
This study investigated the efficacy and safety of subcutaneous sarilumab, a fully human anti-IL-6Rα mAb, for the treatment of moderate-to-severe RA. Of the five sarilumab doses and regimens investigated, the lowest cumulative monthly dose (100 mg q2w) was ineffective; all primary and secondary efficacy endpoints in this group, as well as safety and PK and PD assessments were similar to placebo. Among the four remaining sarilumab doses and regimens, ACR20 responses ranged from 62% to 72%. Of note, the overall efficacy of 150 mg and 200 mg q2w dosing was similar to that observed with 100 mg and 150 mg qw dosing. For example, all four of these groups had statistically significant improvements in DAS28(CRP) reduction. In addition, secondary endpoints showed that responses achieved with 200 mg q2w were numerically similar to and, in some cases, greater than the highest sarilumab dose (150 mg qw).31 Furthermore, the exploratory results for CDAI support the efficacy of sarilumab at Week 12. Because this Phase II dose ranging study (MOBILITY part A) was limited in its scope, duration and sample size, results of secondary or exploratory efficacy endpoints (eg, ACR50, ACR70 and CDAI) and subgroup analyses will require confirmation in the larger Phase III portion of the operationally seamless MOBILITY study (part B).
Acute phase reactants as well as IL-6 levels are typically elevated in patients with RA.13 As expected, based on its inhibition of IL-6 signalling, the effective sarilumab doses reduced the CRP concentration by more than 90% relative to baseline throughout the dosing interval with qw and q2w dosing.
In the current study, the four effective doses (those above 100 mg q2w) had trough levels of functional sarilumab above zero throughout the tested time points. Although these levels were higher in the qw dosing regimens compared with the q2w regimens, the q2w regimens had similar effects on suppressing acute phase reactants such as CRP throughout the dosing interval and on clinical endpoints such as ACR20, 50, 70 and DAS28(CRP) reduction.
The transient increase in circulating IL-6 concentrations early in the treatment period was smaller in the q2w doses compared with the qw doses. A similar relationship between drug exposure levels and elevation in serum IL-6 has been reported for tocilizumab, and may be due to receptor blockade.32 The relationship among sarilumab dose regimens, sarilumab trough levels, and changes in CRP in MOBILITY Part A is consistent with data reported in a Phase I study in patients with RA.30 Those results show that sarilumab PK is characterised as non-linear, consistent with an initial absorption phase, followed by a saturating β phase and a subsequent terminal target-mediated elimination phase. Patients in the higher dose groups had higher functional sarilumab concentrations. In addition, preclinical studies comparing sarilumab with tocilizumab demonstrated that sarilumab had a higher relative binding affinity for IL-6Rα, and blocked IL-6Rα activation, and inhibited IL-6-induced cellular responses such as cell proliferation at lower concentrations than tocilizumab.23 Overall, sarilumab PK characteristics and its high binding affinity support q2w dosing as confirmed by the efficacy observed in the present Phase II study with the 150 mg and 200 mg q2w regimens.
Of note is the high ACR20 placebo response rate of 46%, which is consistent with the placebo response rate reported in a tocilizumab dose ranging study.33 The underlying cause of the high placebo response rate is unclear. In this study, patients were required to have received MTX for a minimum of 3 months and stable for at least 6 weeks prior to the screening visit, and then continued MTX according to the study dosing schedule for the duration of the study. As suggested by the investigators in the Chugai Humanized Anti-Human Recombinant Interleukin-6 Monoclonal Antibody (CHARISMA) study, extending the time period during which patients received stable MTX prior to trial entry may reduce the high placebo rate.33 Confirmation of the efficacy of sarilumab relative to placebo will be sought in larger studies of longer duration currently being conducted in sarilumab’s global Phase III program.
In this study, sarilumab exhibited a safety profile consistent with that observed previously with other anti-IL-6 therapies.14–18 34 Laboratory changes were primarily neutropenia and increases in liver function tests and serum lipids. As observed with other biologicals, non-serious infections were the most commonly reported AEs. There were no serious infections observed in this 12 week study. Also, consistent with results for other IL-6 inhibitors,35 in patients treated with sarilumab, there was no clear association between rates of infection and decreases in neutrophil counts. This suggests that the observed effect on peripheral neutrophil counts may not have overt clinical or functional consequences. Further studies are required to determine the mechanism of this change in peripheral neutrophil counts associated with blockade of IL-6 signalling. An increase in transaminases (ALT and AST) was associated with sarilumab treatment. In this study, no cases of Hy's law (elevation of ALT/AST ≥3× ULN plus total bilirubin >2× ULN) were observed. Similar effects on transaminases were also observed in the studies with tocilizumab.14 15 18 The aetiology of these changes is not understood. LDL and HDL cholesterol increases were observed with sarilumab doses higher than 100 mg q2w. As had been previously described, inflammation in RA has been associated with decreases in cholesterol,36 and control of inflammation results in subsequent increases in cholesterol levels.37 Systemic inflammation and elevation of cholesterol have also been linked to increased risk of cardiovascular events and death in the general population and patients with RA.38 The lipid findings in the current study may not be surprising based on the known mechanism of actions of anti-IL-6Rα therapies,14–18 but the exact clinical consequences remain to be fully elucidated.
Although 150 mg and 200 mg q2w were reasonably similar in efficacy, suppression of neutrophil counts and some safety parameters were less marked in the 150 mg q2w group. These data, taken together with the more convenient dosing interval, support q2w dosing as optimal for sarilumab when dosed at 150 mg and 200 mg.
Conclusion
The MOBILITY Part A study demonstrated that four subcutaneous sarilumab doses (150 mg q2w, 100 mg qw, 200 mg q2w, 150 mg qw) administered in combination with MTX over 12 weeks were effective in reducing the signs and symptoms of moderate-to-severe RA in patients with an inadequate response to MTX. Among these doses, the efficacy findings, as well as the PK and PD parameters, showed that the every other week dosing regimens (150 mg and 200 mg q2w) were as effective as the weekly dosing regimens (100 mg and 150 mg qw). Sarilumab was generally well tolerated, with changes in neutrophil counts and trends for other safety lab parameters favouring q2w dosing. In light of the above and the convenience of every other week dosing, the 150 mg and 200 mg q2w doses are being assessed in multiple Phase III studies in patients with RA.
Supplementary Material
Acknowledgments
The authors would like to thank the study participants, staff and co-investigators at participating centres. The contributions of Ellen Matzkin (clinical leader), Patricia Rohane (senior director, medical operations), Hubert van Hoogstraten (clinical leader), Marius Ardeleanu (clinical study director), Vanessa Marks (clinical trial manager), Fan Chunpeng (biostatistician), Alex Boddy (biostatistician), Albert Torri (bioanalytical scientist), Thomas DiCioccio (pharmacokinetic scientist), Yongtao Li (pharmacokineticist) are greatly appreciated. Medical writing support was provided by Helen Fosam PhD of Prime Medica during the preparation of this paper, supported by Sanofi and Regeneron. Responsibility for opinions, conclusions and interpretation of data lies with the authors. The MOBILITY Part A study was supported by Sanofi and Regeneron.
Footnotes
Funding: Sanofi and Regeneron Pharmacueticals.
Competing interests: TWJH has received lecture fees/consultancy fees from Merck, UCB, Bristol Myers Squibb, Biotest AG, Pfizer, Novartis, Roche, Sanofi, Abbott, Crescendo Bioscience, Nycomed, Boeringher, Takeda and Eli Lilly. RMF has received consultancy fees and study grants from Sanofi and Regeneron Pharmaceuticals. MCG has received consultancy fees and study grants from Sanofi and Regeneron Pharmaceuticals. MJ and SF are employees and shareholders of Sanofi. Xiaohong Huang was an employee of Sanofi during the conduct of the study. ARR, JvA, GDY, and NS are employees and shareholders of Regeneron Pharmaceuticals.
Ethics approval: Participating sites’ IRBs and/or participating countries’ ECs.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Several abstracts have been presented at EULAR and ACR, however, this is the first manuscript.
References
- 1.Upchurch KS, Kay J. Evolution of treatment for rheumatoid arthritis. Rheumatology (Oxford) 2012;51(Suppl 6):vi28–36 [DOI] [PubMed] [Google Scholar]
- 2.Katchamart W, Trudeau J, Phumethum V, et al. Methotrexate monotherapy versus methotrexate combination therapy with non-biologic disease modifying anti-rheumatic drugs for rheumatoid arthritis. Cochrane Database Syst Rev 2010;(4):CD008495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Enbrel (etanercept) prescribing information. http://pi.amgen.com/united_states/enbrel/derm/enbrel_pi.pdf. (accessed 23 Jul 2013)
- 4.REMICADE (infliximab) prescribing information. http://www.remicade.com/remicade/assets/hcp_ppi.pdf (accessed 23 Jul 2013) [Google Scholar]
- 5.HUMIRA (adalimumab) prescribing information. http://www.rxabbott.com/pdf/humira.pdf (accessed 23 Jul 2013)
- 6.SIMPONI (golimumab) prescribing information. http://www.simponi.com/sites/default/files/pdf/prescribing-information.pdf (accessed 23 July 2013)
- 7.CIMZIA (certolizumab pegol) prescribing information. http://cimzia.com/pdf/Prescribing_Information.pdf (accessed 23 Jul 2013)
- 8.Kineret (anakinra) prescribing information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2003/anakamg062703LB.pdf (accessed 23 July 2013)
- 9.ORENCIA (abatacept) prescribing information. http://packageinserts.bms.com/pi/pi_orencia.pdf (accessed 23 Jul 2013)
- 10.RITUXAN (rituximab) prescribing information. http://www.gene.com/gene/products/information/pdf/rituxan-prescribing.pdf (accessed 23 Jul 2013)
- 11.Actemra (tocilizumab) Prescribing Information 2010. http://www.gene.com/gene/products/information/actemra/pdf/pi.pdf (accessed 23 Jul 2013)
- 12.Smolen JS, Landewé R, Breedveld FC, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs. Ann Rheum Dis 2010;69:964–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Srirangan S, Choy EH. The role of interleukin 6 in the pathophysiology of rheumatoid arthritis. Ther Adv Musculoskelet Dis 2010;2:247–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones G, Sebba A, Gu J, et al. Comparison of tocilizumab monotherapy versus methotrexate monotherapy in patients with moderate to severe rheumatoid arthritis: the AMBITION study. Ann Rheum Dis 2010;69:88–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smolen JS, Beaulieu A, Rubbert-Roth A, et al. Effect of interleukin-6 receptor inhibition with tocilizumab in patients with rheumatoid arthritis (OPTION study): a double-blind, placebo-controlled, randomised trial. Lancet 2008;371:987–97 [DOI] [PubMed] [Google Scholar]
- 16.Emery P, Keystone E, Tony HP, et al. IL-6 receptor inhibition with tocilizumab improves treatment outcomes in patients with rheumatoid arthritis refractory to anti-tumour necrosis factor biologicals: results from a 24-week multicentre randomised placebo-controlled trial. Ann Rheum Dis 2008;67:1516–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smolen JS, Avila JC, Aletaha D. Tocilizumab inhibits progression of joint damage in rheumatoid arthritis irrespective of its anti-inflammatory effects: disassociation of the link between inflammation and destruction. Ann Rheum Dis 2012;71:687–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Genovese MC, McKay JD, Nasonov EL, et al. Interleukin-6 receptor inhibition with tocilizumab reduces disease activity in rheumatoid arthritis with inadequate response to disease-modifying antirheumatic drugs: the tocilizumab in combination with traditional disease-modifying antirheumatic drug therapy study. Arthritis Rheum 2008;58:2968–80 [DOI] [PubMed] [Google Scholar]
- 19.Kremer JM, Blanco R, Brzosko M, et al. Tocilizumab inhibits structural joint damage in rheumatoid arthritis patients with inadequate responses to methotrexate: results from the double-blind treatment phase of a randomized placebo-controlled trial of tocilizumab safety and prevention of structural joint damage at one year. Arthritis Rheum 2011;63:609–21 [DOI] [PubMed] [Google Scholar]
- 20.Genovese MC, Fleischmann RM, Fiore S, et al. Sarilumab, a subcutaneously-administered, fully-human monoclonal antibody inhibitor of the IL-6 receptor: Relationship between EULAR responses and change from baseline of selected clinical parameters. Ann Rheum Dis 2013;72(Suppl 3):620 [Google Scholar]
- 21.Zhang L, Luan B, Adler A, et al. Sarilumab (REGN88), a fully-human anti-IL6R antibody, inhibits tumor growth in preclinical models, as a single agent and in combination with the VEGF blocker aflibercept. Cancer Res 2012;72(8 Suppl 1):2723. doi:10.1158/1538-7445.AM2012-2723. [Google Scholar]
- 22.Wang L-H, Xue Y, Liu X, et al. Preclinical development of sarilumab, the first fully human monoclonal antibody (mAb) against IL-6R alpha: utilization and value of double humanized animal model. Ann Rheum Dis 2013;72(Suppl 3):375 [Google Scholar]
- 23.Rafique A, Martin J, Blome M, et al. Evaluation of the binding kinetics and functional bioassay activity of sarilumab and tocilizumab to the human IL-6 receptor (IL-6R) alpha. Ann Rheum Dis 2013;72(Suppl 3):79723291386 [Google Scholar]
- 24.Radin AR, Mellis SJ, Jasson M, et al. REGN88/SAR153191, a fully-human interleukin-6 receptor monoclonal antibody, reduces acute phase reactants in patients with rheumatoid arthritis: preliminary observations from Phase 1 studies. Arthritis Rheum 2010;62(Suppl 10):S470 [Google Scholar]
- 25.Radin A, Mellis S, Jasson M, et al. Safety and effects on markers of inflammation of subcutaneously administered REGN88/SAR153191, an interleukin-6 receptor inhibitor, in patients with rheumatoid arthritis: findings from Phase 1 studies. Ann Rheum Dis 2010;69(Suppl 3):99 [Google Scholar]
- 26.Huizinga TW, Kivitz AJ, Rell-Bakalarska M, et al. Sarilumab for the treatment of moderate-to-severe rheumatoid arthritis: results of a phase 2, randomized, double-blind, Placebo-Controlled, International Study. Ann Rheum Dis. 2012;71(Suppl 3):60 [Google Scholar]
- 27.Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988;31:315–24 [DOI] [PubMed] [Google Scholar]
- 28.Felson DT, Anderson JJ, Boers M,et al. American College of Rheumatology preliminary definition of improvement in rheumatoid arthritis. Arthritis Rheum. 1995;38:727–35 [DOI] [PubMed] [Google Scholar]
- 29.Fransen J, Stucki G, van Riel PLCM. Rheumatoid arthritis measures: disease activity score (DAS), disease activity score-28 (DAS28), rapid assessment of disease activity in rheumatology (RADAR), and rheumatoid arthritis disease activity index (RADAI). Arthritis Care Res 2003;49(S5):S214–24 [Google Scholar]
- 30.Belomestnov P, Hamilton J, DiCioccio AT, et al. Sarilumab, a subcutaneously-administered, fully-human monoclonal antibody inhibitor of the IL-6 receptor: pharmacokinetic profile and its relationship to changes in pharmacodynamic markers in patients with rheumatoid arthritis. Arthritis Rheum 2012;64:S576 [Google Scholar]
- 31.Fleischmann R, Fiore S, Fan C, et al. Sarilumab, a fully human mAb against IL-6R alpha, subcutaneously-administered shows significant improvement in RA patients as early as 2 weeks: a time to event analysis for ACR50 and EULAR good response. Ann Rheum Dis 2013;72(Suppl 3):62723204515 [Google Scholar]
- 32.Nishimoto N, Terao K, Mima T, et al. Mechanisms and pathologic significances in increase in serum interleukin-6 (IL-6) and soluble IL-6 receptor after administration of an anti–IL-6 receptor antibody, tocilizumab, in patients with rheumatoid arthritis and Castleman disease. Blood 2008;112:3959–64 [DOI] [PubMed] [Google Scholar]
- 33.Maini RN, Taylor PC, Szechinski J, et al. Double-blind randomized controlled clinical trial of the interleukin-6 receptor antagonist, tocilizumab, in European patients with rheumatoid arthritis who had an incomplete response to methotrexate. Arthritis Rheum 2006;54:2817–29 [DOI] [PubMed] [Google Scholar]
- 34.Shakib S, Francis B, Smith J, et al. Safety, pharmacokinetics and pharmacodynamics of ALD518 (BMS-945429), a high-affinity monoclonal antibody directed against interleukin-6 (IL-6) administered by subcutaneous injection: a phase I trial. [abstract]. Arthritis Rheum 2010;62(Suppl 10):1124 [Google Scholar]
- 35.Schiff MH, Kremer JM, Jahreis A, et al. Integrated safety in tocilizumab clinical trials. Arthritis Res Ther 2011;13:R141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choy E, Sattas N. Interpreting lipid levels in the context of high-grade inflammatory states with a focus on rheumatoid arthritis: a challenge to conventional cardiovascular risk actions. Ann Rheum Dis 2009;68:460–9 [DOI] [PubMed] [Google Scholar]
- 37.Navarro-Millán I, Charles-Schoeman C, Yang S, et al. Changes in lipoproteins associated with methotrexate or combination therapy in early rheumatoid arthritis: results from the treatment of early rheumatoid arthritis trial. Arthritis Rheum 2013;65:1430–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ridker PM, Hennekens CH, Buring JE, et al. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med 2000;342:836–43 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.





