Abstract
Background
Charles Bonnet Syndrome (CBS) is widely considered a transient condition without adverse consequence, questioning the need for treatment. Yet, while this view may be true of the majority of people with CBS, it is recognised that some have negative experiences and outcomes. Here, we attempt to better understand negative outcome CBS and the factors that influence it.
Methods
4000 members of the Macular Society were sent a structured questionnaire covering the phenomenology of CBS, its prognosis and impact, symptom reporting, patient knowledge and sources of information.
Results
492 people with CBS were identified. Kaplan–Meier analysis suggested 75% had CBS for 5 years or more. Thirty-two per cent had negative outcome. Factors associated with negative outcome were: (1) frequent, fear-inducing, longer-lasting hallucination episodes, (2) one or more daily activities affected, (3) attribution of hallucinations to serious mental illness, (4) not knowing about CBS at the onset of symptoms. Duration of CBS or the type of content hallucinated were not associated with negative outcome.
Conclusions
CBS is of longer duration than previously suspected with clinically relevant consequences in a third of those affected. Interventions that reduce the frequency, duration or fear of individual hallucination episodes and education prior to hallucination onset may help reduce negative outcome.
Keywords: Visual perception, Macula, Epidemiology
Introduction
Charles Bonnet's description of his grandfather's visual hallucinations1 2 lies at the boundary of what might be considered a ‘clinical’ condition. Bonnet focussed on positive aspects of the experience, such as the pleasure and intellectual curiosity hallucinations gave, and the fact they were not associated with psychological or cognitive problems. His grandfather had significant visual impairment, plausibly related to age-related macular disease (AMD),3 but there was no suggestion the hallucinations themselves were an illness or that treatment would have been necessary or appropriate. Furthermore, the hallucinations resolved within a few months, so that any problems would have been short-lived. Reawakened interest in Charles Bonnet Syndrome (CBS) has done little to dispel this view with consistent reports that the majority of patients with CBS do not find it troublesome.4–8 Yet, a sizable minority report a range of negative experiences and outcomes. Compared to patients with the same degree of visual loss without hallucinations, patients with CBS have decreased measures of quality of life and functional ability,9 and some fear being labelled as having serious mental illness.7 Around a third find the hallucinations themselves an unpleasant or disturbing experience.5–8 CBS thus covers a spectrum of outcomes, one end celebrated by Bonnet in his description of hallucinations as ‘playthings of the brain’, the other a predominantly negative outcome characterised by distress, stigma and reduced quality of life. Given that this latter group is potentially large (between 16 000 and 100 000 people in the UK based on a ∼500 000 population with late AMD10 and CBS prevalence of 10–60%11) it is becoming increasingly important to better understand what factors lead to negative outcome and how people with negative experiences of CBS differ from those that do not find CBS distressing. Furthermore, there is emerging evidence that CBS may not be as transient as traditionally held. One study has reported hallucinations continuing for 4 years or more in 45% of people with CBS,8 while another found 41% of people with CBS had an estimated minimal average duration of 8 years (minimal as hallucinations were ongoing at the end of the study).6 It is difficult to dismiss CBS as a clinical irrelevance if it results in troubling symptoms that persist for many years for a large group of people. Here, we set out to re-evaluate the prognosis of CBS, and characterise factors associated with its negative outcome in a large-scale survey of members of the Macular Society, a UK charity for people affected by central vision loss that provides practical and emotional support, campaigns for improvements in services and funds research.
Methods
Four thousand members of the Macular Society were selected at random from the membership database (database n=10 847 after excluding members surveyed the previous year) using campaign management software (NFP CARE, Advance computer software group). Those selected were sent a structured questionnaire in October 2012 covering CBS: demographics, risk factors, phenomenology, duration/prognosis, (using items derived from the Institute of Psychiatry Visual Hallucinations Interview8) impact on daily living and wellbeing, reporting of symptoms and sources of information (see online supplementary material for questionnaire content). Questionnaires were returned by post. Members unable to read the questionnaire were offered support in completing it by telephone. The study was approved by the King's College London, Psychiatry, Nursing and Midwifery Research Ethics subcommittee (PMN/11/12-64). All participants gave informed consent. Categorical variables were compared using χ2 tests with Bonferroni correction where appropriate. Continuous variables were examined using analysis of variance (ANOVA) models. Duration of CBS was calculated from the month/year of CBS onset and month/year of last hallucination, with a resolution of 3 months, and analysed using the Kaplan-Meier method,12 with cessation of hallucinations as the outcome event of interest. To avoid inflating the estimate of duration through rounding error, if no month was specified for month/year of onset, the end of the year was used.
Results
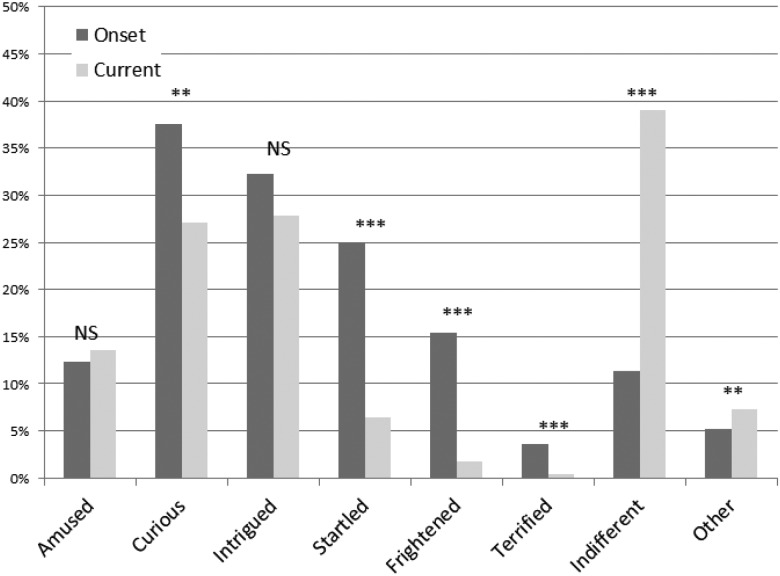
A total of 1254 surveys were returned by members who reported a diagnosis of macular disease (31% of questionnaires sent). Of these, 39% (n=492) had experienced hallucinations of patterns (63%), faces (39%), objects (39%), figures (36%) and animals (22%) and had been told they had, or judged themselves to have had, CBS. Typical hallucinations were of short duration, lasting either minutes (44%) or seconds (34%). When judged at their worst, hallucinations could occur weekly (30%), monthly (21%), daily (22%) or constantly (13%). Figure 1 shows different categories of emotional response (more than one could be selected) at the onset of CBS (dark grey bars) and at the time of the questionnaire (light grey bars). At CBS onset, 38% reported one or more of responses: startling, terrifying and frightening (pooled as ‘fear-inducing’), reducing to 8% at the time of the questionnaire. Forty-six per cent reported that CBS had an effect on daily activities, selecting responses: television watching (24%), moving about (14%), cooking (8%) and sleeping (14%) with free-text answers of: reading, driving and relaxing. Only 7% had not told anyone about CBS. Forty-seven per cent had discussed it with a medical professional with around a third of these selecting responses indicating the professional was unsure or did not know about the diagnosis. Sixty-seven per cent had not heard of CBS at symptom onset and attributed the hallucinations to one or more of responses: sight loss (50%), mental illness (11%), Alzheimer's disease (5%) or unknown (40%) with free text answers: side-effects of medication, physical illness and real events. Sixty-three per cent were relieved and/or reassured by receiving information on CBS.
Figure 1.
Emotional responses to Charles Bonnet Syndrome hallucinations. Bars indicate % of hallucinators reporting each emotion. Dark grey indicates emotions at the onset of symptoms, light grey at the time of the questionnaire. χ2 corrected for multiple comparisons ***pcorr<0.001; **pcorr<0.01; NS pcorr>0.05.
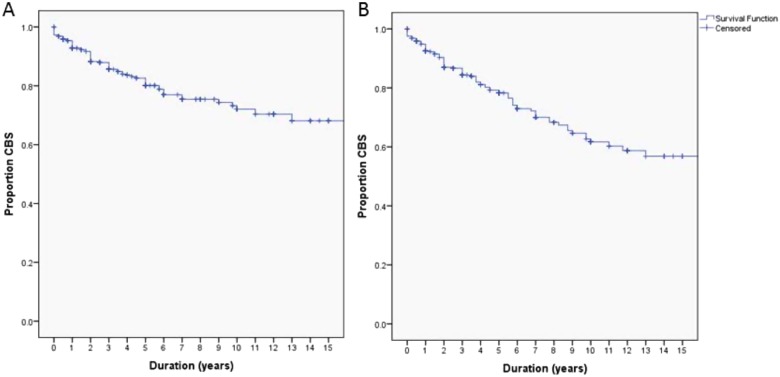
Prognosis of CBS
Figure 2 shows the Kaplan–Meier plot of CBS duration. The method takes into account the fact that many of the participants were still having hallucinations at the time of the survey, so that the duration of their CBS is unknown (censored data). However, the large sample size meant that ∼100 CBS resolution events were available from which to estimate the duration (survival) function. Two measures of symptom resolution were used. One was derived from the questionnaire item asking whether CBS had stopped or was on-going at the time of the questionnaire (figure 2A). Using this measure, 88% of the sample (95% CI 85% to 92%) had CBS for 2 years or more, resolving in only 25% at 9 years. We recognised that it might be difficult to judge whether CBS has resolved if hallucinations only occur infrequently (eg, every 6 months). We therefore repeated the analysis applying an arbitrary definition of resolution as having no hallucinations in the 3 months prior to the questionnaire (figure 2B). The prognosis at 2 years was the same using this definition (87% with ongoing CBS; 95% CI 83% to 90%) but the time for 25% to resolve reduced to 5.75 years.
Figure 2.
Kaplan–Meier plots of Charles Bonnet Syndrome (CBS) duration. (A) The proportion of the sample with CBS each year after onset based on self-report of CBS resolution. The vertical dashes indicate censored observations. (B) The proportion of the sample with CBS each year after onset with CBS resolution defined as an absence of hallucinations in the 3 months prior to the questionnaire.
Negative outcome CBS
While the majority of people with CBS felt it had no real effect on their life (60%), a subset judged it to have a fairly negative (25%) or very negative (8%) effect, and 6% reported a fairly pleasant or very pleasant effect (1%). We collapsed these responses into three outcome valencies: negative (fairly and very negative, n=156), positive (fairly and very pleasant, n=36) and neutral (n=289). Negative outcome was not associated with gender or diagnosis (wet, dry, wet and dry AMD; p>0.05). It was associated with longer-duration hallucination episodes (χ2=38.9, p<0.00 001) and more frequent hallucination episodes (χ2=31.7, p=0.0001). There was no difference in mean overall duration of CBS (CBS onset to cessation) for subgroups with negative outcome (mean duration 2.7±2.0 years), positive outcome (1.9±1.3 years) and neutral outcome (3.3±3.9 years) (F2,75=0.452; p=0.638—censored data excluded). Negative outcome was not associated with a particular type of hallucination content (pcorr>0.05 for patterns, faces, people, animals and objects). Fear-inducing hallucinations at CBS onset were associated with negative outcome (45% of the subgroup with fear-inducing hallucinations at onset had negative outcome vs 25% of the subgroup without fear-inducing hallucinations; χ2=23.2, pcorr=0.00001). CBS affecting one or more daily activities was associated with negative outcome (52% of the subgroup with an activity affected had negative outcome vs 16% of the subgroup with no activities affected, χ2=75.3, p<0.000001). Attributing CBS to mental illness or, at trend significance, Alzheimer's disease was associated with negative outcome (58% of the subgroup attributing CBS to mental illness had negative outcome vs 30% of the subgroup not attributing CBS to mental illness, χ2=12.0, pcorr=0.01). Attributing CBS to sight loss was not associated with negative outcome (χ2=0.087, pcorr>0.05). Lack of prior knowledge about CBS at symptom onset was associated with negative outcome (25% of the subgroup familiar with CBS at onset had negative outcome vs 35% of the subgroup unfamiliar with CBS at onset; χ2=6.4, p=0.04). There was also a trend association between the quality of information given by medical professional and negative outcome (47% of the subgroup not given a clear account, had negative outcome vs 36% of the subgroup given a clear account; χ2=4.5, p=0.10).
Discussion
This is the largest phenomenological survey of CBS reported to date, with 492 people identified, compared to an average of 42 people (range 4–150) in previous surveys.4–9 13–21 The scaling in sample size allows us to explore issues less amenable to investigation in smaller studies due to their limitations of statistical power. Although our sample is derived from members of a voluntary society, the phenomenology of the hallucinations reported (ie, relative frequency of each content category, distribution of emotional responses, temporal characteristics etc) match those of previous surveys in clinical settings giving us confidence the findings are representative of CBS as a whole.
How long does CBS continue?
CBS continued for 5 years or more in 75% of the sample. This seems inconsistent with previous longitudinal studies suggesting 28% recovery at 1 year 22 or an average duration of 18 months.23 However, the former study relates to resolution over the course of a year without specifying prior duration of CBS, while the latter study does not take into account participants with on-going CBS (censored observations). Our study indicates the typical duration of CBS is far longer than these estimates, and questions the traditional view that CBS is a transient condition. It is possible our estimate is biased by people with shorter-duration CBS choosing not to participate in the survey. However, this seems unlikely, as the estimate of CBS prevalence based on the total number of questionnaires sent (12%) is similar to previous prevalence estimates for ophthalmic populations (∼10%)3 suggesting we were not missing a large proportion of respondents.
Factors influencing negative outcome CBS
The 32% prevalence of negative outcome in our sample is similar to that described in previous studies.4 5 21 Since our definition of negative outcome CBS is derived from self-report, without formal measures of psychopathology, well-being, or quality of life, its true clinical significance remains to be determined. However, a higher proportion of the negative outcome CBS subgroup sought medical advice suggesting it has clinical implications (61% of the negative outcome subgroup sought medical advice vs 45% of the neutral or 44% of the positive subgroup, χ2=10.3 p=0.006). Some of the factors associated with negative outcome were linked to the hallucinations themselves (eg, how long a typical hallucination lasts and whether it induced fear) while others related to knowledge of CBS and quality of information. We explored the relative importance of each hallucination-related and education-related factor as a target for theoretical intervention by calculating the expected reduction in negative outcome for each intervention (table 1). There was a clear advantage for interventions targeting hallucination-related factors over education-related factors. This may reflect the fact that Macular Society members were well informed at baseline, with only 13% unfamiliar with CBS prior to the questionnaire. In comparison, 71% of the clinical sample reported by Abbott et al20 had no knowledge of CBS prior to their study. It is thus likely that information about CBS prior to symptom onset will have a greater impact on negative outcome in the wider clinical population than found here. Replicating findings of a previous study,24 less than half of those with CBS sought medical advice. This low rate of advice-seeking sets a limit on the ability to reduce negative outcome by targeted training of medical professionals.
Table 1.
Reduction in proportion of negative outcome CBS from base rate (32%) using hypothetical interventions indicated
| Treatment category | Theoretical treatment target | % Reduction in negative outcome |
|---|---|---|
| Hallucination-related | Reduction of duration of hallucination episodes to seconds | 44 |
| Reduction of hallucination frequency to monthly | 47 | |
| Resolution of fearful emotional responses | 24 | |
| No limitation of activities | 52 | |
| Education-related | CBS awareness at symptom onset | 20 |
| No attribution of CBS to mental illness | 6 | |
| Improved clarity of explanation | 2 |
CBS, Charles Bonnet Syndrome.
An unexpected finding was the lack of association between overall duration of CBS and negative outcome. This may reflect a habituation to CBS over time, as supported by the reduction in fear-inducing hallucinations from symptom onset to the time of the questionnaire. Consistent with previous reports,4 23 some participants suggested the frequency and duration of individual hallucination episodes reduced with time so that they no longer considered them a problem. For other participants, hallucinations ceased for a period but returned with subsequent progression of their macular disease. Such observations highlight the difficulty in defining when CBS resolves and question the relevance of CBS cessation as an endpoint for clinical trials.
Conclusions
What are the clinical implications of the findings? It is clear that CBS can no longer be considered a homogeneous, transient condition. For most people with CBS, symptoms continue for many years with negative consequences in around a third. This changes CBS from a symptom that can be largely ignored by clinical services to one that needs further characterisation to identify those with negative outcome and offer appropriate interventions. The low priority given to CBS research to date means there is currently an absence of evidence as to what treatments might be effective. Our study suggests an alternative treatment goal to cessation of hallucinations might be to target negative outcome, reducing the duration, frequency, fear association and interference with activities of ongoing hallucinations to result in a more benign form of CBS. The findings also suggest negative outcome might be preventable, and the need for trials to examine the effectiveness of information/psychoeducation prior to the onset of hallucinations. The era of CBS as an incidental curiosity has ended; for those with negative outcome, CBS now lies unequivocally within the clinical domain.
Supplementary Material
Acknowledgments
We thank Cathy Yelf, Head of External Relations at the Macular Society, who helped design the survey and oversaw its production and dissemination, Becca Yelf for data entry and Daniel Harbison for assistance with data quality assurance. We also thank members of the Macular Society for participating in the survey.
Footnotes
Contributors: DHF designed and supervised the study, its analysis and preparation of the manuscript. TMC analysed the data and drafted the manuscript.
Competing interests: DHF is supported by NIHR programme grant RP-PG-0610-10100: Towards an evidence-based clinical management of visual hallucinations.
Ethics approval: King's College London, Psychiatry, Nursing and Midwifery Research Ethics subcommittee (PMN/11/12-64).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Bonnet C. L’ Essai analytique sur les facultés de l’ âme. Copenhagen, C & A Philibert: 1760 [Google Scholar]
- 2.Hedges TR., Jr Charles Bonnet, his life, and his syndrome. Surv Ophthalmol 2007;52:111–14 [DOI] [PubMed] [Google Scholar]
- 3.ffytche DH. Visual hallucinations and the Charles Bonnet Syndrome. Curr Psychiatr Rep 2005;7:168–79 [DOI] [PubMed] [Google Scholar]
- 4.Vukicevic M, Fitzmaurice K. Butterflies and black lacy patterns: the prevalence and characteristics of Charles Bonnet hallucinations in an Australian population. Clin Exp Ophth 2008;36:659–65 [DOI] [PubMed] [Google Scholar]
- 5.Teunisse RJ, Cruysberg JR, Hoefnagels WH, et al. Visual hallucinations in psychologically normal people: Charles Bonnet's syndrome. Lancet 1996;347:794–7 [DOI] [PubMed] [Google Scholar]
- 6.Khan JC, Shahid H, Thurlby DA, et al. Charles Bonnet syndrome in age-related macular degeneration: the nature and frequency of images in subjects with end-stage disease. Ophthalmic Epidemiol 2008;15:202–8 [DOI] [PubMed] [Google Scholar]
- 7.Menon GJ. Complex visual hallucinations in the visually impaired: a structured history-taking approach. Arch Ophthalmol 2005;123:349–55 [DOI] [PubMed] [Google Scholar]
- 8.Santhouse AM, Howard RJ, ffytche DH. Visual hallucinatory syndromes and the anatomy of the visual brain. Brain 2000;123:2055–64 [DOI] [PubMed] [Google Scholar]
- 9.Scott IU, Schein OD, Feuer WJ, et al. Visual hallucinations in patients with retinal disease. Am J Ophthalmol 2001;131:590–8 [DOI] [PubMed] [Google Scholar]
- 10.Owen CG, Jarrar Z, Wormald R, et al. The estimated prevalence and incidence of late stage age related macular degeneration in the UK. Br J Ophthalmol 2012;96:752–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.ffytche DH. Visual hallucinations in eye disease. Curr Opin Neurol 2009;22:28–35 [DOI] [PubMed] [Google Scholar]
- 12.Kaplan E, Meier P. Nonparametric estimation from incomplete observations. Am Stat Assoc J 1958;53:457–81 [Google Scholar]
- 13.Holroyd S, Rabins PV, Finkelstein D, et al. Visual hallucinations in patients with macular degeneration. Am J Psych 1992;149:1701–6 [DOI] [PubMed] [Google Scholar]
- 14.Brown GC, Murphy RP. Visual symptoms associated with choroidal neovascularization. Photopsias and the Charles Bonnet syndrome. Arch Ophthalmol 1992;110:1251–6 [DOI] [PubMed] [Google Scholar]
- 15.Holroyd S, Rabins PV, Finkelstein D, et al. Visual hallucinations in patients from an ophthalmology clinic and medical population. J Nerv Ment Dis 1994;182:273–6 [DOI] [PubMed] [Google Scholar]
- 16.Teunisse RJ, Zitman FG, Raes DC. Clinical evaluation of 14 patients with the Charles Bonnet syndrome (isolated visual hallucinations). Compr Psychiatry 1994;35:70–5 [DOI] [PubMed] [Google Scholar]
- 17.Crane WG, Fletcher DC, Schuchard RA. Prevalence of photopsias and Charles Bonnet Syndrome in a low vision population. Ophthalmol Clin North Am 1994;7:143–9 [Google Scholar]
- 18.Schultz G, Needham W, Taylor R, et al. Properties of complex hallucinations associated with deficits in vision. Perception 1996;25:715–26 [DOI] [PubMed] [Google Scholar]
- 19.Tan CS, Lim VS, Ho DY, et al. Charles Bonnet syndrome in Asian patients in a tertiary ophthalmic centre. Br J Ophthalmol 2004;88:1325–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abbott EJ, Connor GB, Artes PH, et al. Visual loss and visual hallucinations in patients with age-related macular degeneration (Charles Bonnet syndrome). Invest Ophthalmol Vis Sci 2007;48:1416–23 [DOI] [PubMed] [Google Scholar]
- 21.Gilmour G, Schreiber C, Ewing C. An examination of the relationship between low vision and Charles Bonnet syndrome. Can J Ophthalmol 2009;44:49–52 [DOI] [PubMed] [Google Scholar]
- 22.Jackson ML, Bassett KL. The natural history of the Charles Bonnet Syndrome. Do the hallucinations go away? Eye 2010;24:1303–4 [DOI] [PubMed] [Google Scholar]
- 23.Holroyd S, Rabins PV. A three year follow-up study of visual hallucinations in patients with macular degeneration. J Nerv Ment Dis 1996;184:188–9 [DOI] [PubMed] [Google Scholar]
- 24.Mitchell J, Bradley P, Anderson SJ, et al. Perceived quality of health care in macular disease: a survey of members of the Macular Disease Society. Br J Ophthalmol 2002;86:777–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.