Abstract
Background:
Preterm infants constitute a large proportion of the newborn population in the neonatal intensive care units (NICUs). Parents, as the main members of the care team, are not adequately supported as the focus is chiefly on infant care. The present study aimed to evaluate the effect of a family support intervention on the stress levels among the parents of preterm infants in NICU.
Materials and Methods:
In this quasi-experimental study, convenience sampling method was used to select 50 parents of preterm infants. The subjects were allocated to two groups of intervention and control (n = 25 pairs in each). While the control group received routine care, the intervention group benefitted from a two-stage family support program (including informational and observational phases in the first stage and emotional supportive intervention in the second). The Parental Stressor Scale-NICU (PSS-NICU) was completed by both fathers and mothers of the two groups (before and after intervention). Descriptive and inferential statistics were employed to analyze data in SPSS version 18.
Results:
Before the intervention, the mean total scores of PSS-NICU and also the mean scores of its three subscales were not significantly different between the two groups. However, after the intervention, significant differences were observed between the two groups. The scores of the intervention group showed significant reduction following the intervention, but such a difference was not detected in the control group.
Conclusions:
Apparently, early educational and emotional support for parents of preterm infants decreased their stress. Similar interventions may thus be effective in empowering parents for caring of their infant and playing their parental role.
Keywords: Intensive care unit, nursing, parents, preterm birth, stress
INTRODUCTION
Preterm birth, a major concern during the perinatal period,[1] has a global annual incidence of around 13 million.[2] A cross-sectional study in Yasuj, Iran estimated the prevalence of prematurity and low birth weight at 8.4% and 6.7%, respectively.[3] Although more than half of preterm infants need admission to a neonatal intensive care unit (NICU),[4] in many countries, care in the NICU is limited to infants and neglects the role of parents, especially the father. Despite the presence of mothers in the NICU, they have little information about their infant's conditions and how to take care of him/her. Research has shown that parents of preterm infants in the NICU experience high levels of psychological distress including acute anxiety disorder, post-traumatic stress disorder,[5,6,7,8] and depression.[9,10,11,12] Factors such as physical environment of the NICU and equipments and invasive procedures (e.g. injections, catheterization, intravenous lines, and blood sampling) used in the unit can cause stress and anxiety for the parents. Similarly, rules of the NICU, the infants’ appearance and behavior, separation of the infants from the family due to their critical conditions, changes in the expected parental role, and inability to protect the infant will all contribute to the parents’ feelings of grief, loss, fear, anger, guilt, and helplessness.[1,13,14,15] Such stress and mental suffering will often lead to persistent problems such as depression, anxiety disorders, and impaired parenting, even after the baby is discharged from the hospital.[16,17] Consequently, parents having to deal with a preterm infant and his/her admission to the NICU will undoubtedly require support.
Budin was the first to highlight the importance of parent–infant relationship in 1907. Not more than 1 year later, supporting parents was introduced as a key nursing role.[18] However, neonatal nursing is still challenged with supporting parents in not only adaptation to the birth of a preterm infant, but also properly playing their parental role through various care practices.[19]
Previous studies have shown the efficacy of supportive nursing interventions in reducing parental stress and enabling the parents to cope with problems during their infant's hospitalization.[20,21,22,23,24,25] While some of these studies only supported mothers and reported decreased stress among this group,[23,24] others targeted both parents and found the interventions to reduce stress more effectively in mothers than in fathers.[20,21,22] In contrast, Ahn and Kim (2007) suggested that a supportive educational intervention could significantly lower stress scores among the fathers of infants in the NICU, but did not significantly change the mothers’ stress scores.[25]
Although the effects of such supportive educational interventions on the parents’ stress, anxiety, depression, involvement in caring for the baby, beliefs, physiological variables, and satisfaction, and also, the infant's weight gain and length of NICU stay have been evaluated in previous studies, none of the studies have provided emotional support.[20,21,22,23,24,25] Apparently, to minimize the short- and long-term consequences of an infant's admission to the NICU (including parental stress), the nurses are required to provide emotional support for both parents.[13] In fact, a combination of educational and emotional support might be most effective in reducing the psychological distress experienced by parents during their infant's hospitalization. Therefore, this study evaluated the effects of a family support program on the stress levels of parents of preterm infants in the NICU. We tried to prove the following two hypotheses:
Total stress scores are lower in the parents of the intervention group than in the control group
The mean scores of all three subscales of stress are lower in the experimental group than in the control group.
MATERIALS AND METHODS
This quasi-experimental study used a pre-test–post-test design with both an intervention group and a control group. It was conducted in the NICU of Behashti Hospital (Isfahan, Iran) from September 2012 to March 2013.
In each group, parents of 25 preterm infants were selected by convenience sampling. The parents who were older than 18 years and able to read and write, at least met their baby once, were not health care professionals, had not experienced major stressors such as divorce, separation, and loss of employment during last year, and with their infants having the required characteristics participated in the study after obtaining written informed consent. Infants’ required characteristics were: Being single infant with gestational age of less than 35 weeks, having the fifth second Apgar score of greater than 5, and not having severe disabling problems such as intraventricular hemorrhage of grade 3 or 4, or major congenital defects.
The participants were allocated to two groups of control and intervention (25 couples in each group). During the 2-4 days after the infant's admission, the parents in the intervention group were allowed to meet the infant in the NICU. Demographic data were collected in the same period.
The control group participants received routine care. The intervention group benefitted from a family support intervention comprising two stages. The first stage was performed 2-4 days after the infant's admission[21] and included informational and observational phases. In the informational phase, parents attended a 60-min face-to-face training session about the environment, equipment, and medical staff of the NICU, care procedures (e.g. venipuncture), characteristics of premature infants (e.g. appearance, behavior, and physical signs), common medical terminology in the NICU, possible feelings of parents during their infant's hospitalization, and methods of participation in infant care (e.g. kangaroo mother care). After the training session, the parents were provided with two books and an educational booklet. The training booklet had been designed by the researchers according to the parents’ needs. It consisted of six sections with different colors and illustrations for ease of use. The first–sixth parts of the booklet contained information about the NICU, premature infants’ characteristics, premature infant care, self-care, preparations for discharge from the NICU, and the common terms and abbreviations used in the NICU, respectively. In the observational phase, which was implemented right after the informational phase, the parents visited the NICU and the researcher presented necessary information about the environment and procedures.
Two to four days later, the second stage (support provision) was started, i.e. the parents received psychological training and obtained the opportunity to share their feelings and experiences with other parents of premature infants during a 2-h session.
Moreover, throughout the course of the study, the researcher paid regular visits to the hospital to ask the parents whether they had used the booklets, to encourage them to actively participate in infant care, and to answer their questions. In the absence of the researcher, the parents could ask their questions on the phone. Although the hospital allowed the fathers to visit their infants only for 30 min on even days, arrangements were made to eliminate such limitations.
Demographic information was collected by asking questions to parents. The Parental Stressor Scale-NICU (PSS-NICU, 2011) was used to assess the stress levels of parents of premature infants hospitalized in the NICU. The questionnaire consisted of 26 items in three subscales of NICU environment (5 items), infant appearance and behaviors and special treatment (14 items), and relationship with infants and accepting parental role (7 items). It measured the stress levels caused by various stressors from the perspective of parents.[26,27] The items were scored on a six-point Likert scale (“Have never dealt with it,” “No stress,” “Little stress,” “Moderate level of stress,” “High level of stress,” and “Extremely high level of stress”). Questions answered as “Have never dealt with it” were considered as missing data. In the presence of stress, classification scores for each item ranged from 0 to 4. Therefore, the minimum and maximum total scores were zero and 104, respectively; also, the maximum score for the first subscale was 20, for the second subscale was 56, and for the third subscale was 28, and the minimum scores were zero, respectively. The obtained scores were multiplied by 100 and divided by 104, and thus, the maximum score was 100 and the minimum was zero. Also, the score for each subscale was multiplied by 100 and divided by the maximum score of it.
The content validity of translated questionnaire was established by face validation. To determine reliability, after data collection, the Cronbach's alpha was calculated (α = 0.87 for the whole questionnaire and α = 0.77, 0.77, and 0.86 for the NICU environment, infant appearance and behaviors and special treatment, and relationship with infants and accepting parental role subscales, respectively). We considered the scores of each couple (an infant's father and mother) as one unit. Data were analyzed with descriptive and inferential statistics (paired and independent t-tests) in SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). Matching of demographic variables in the two groups was assessed by employing Chi-square and Mann–Whitney tests.
RESULTS
The two groups were not significantly different in terms of the parents’ demographics and infant characteristics [Table 1].
Table 1.
Demographic characteristics of mothers, fathers, and their infants in the intervention and control groups
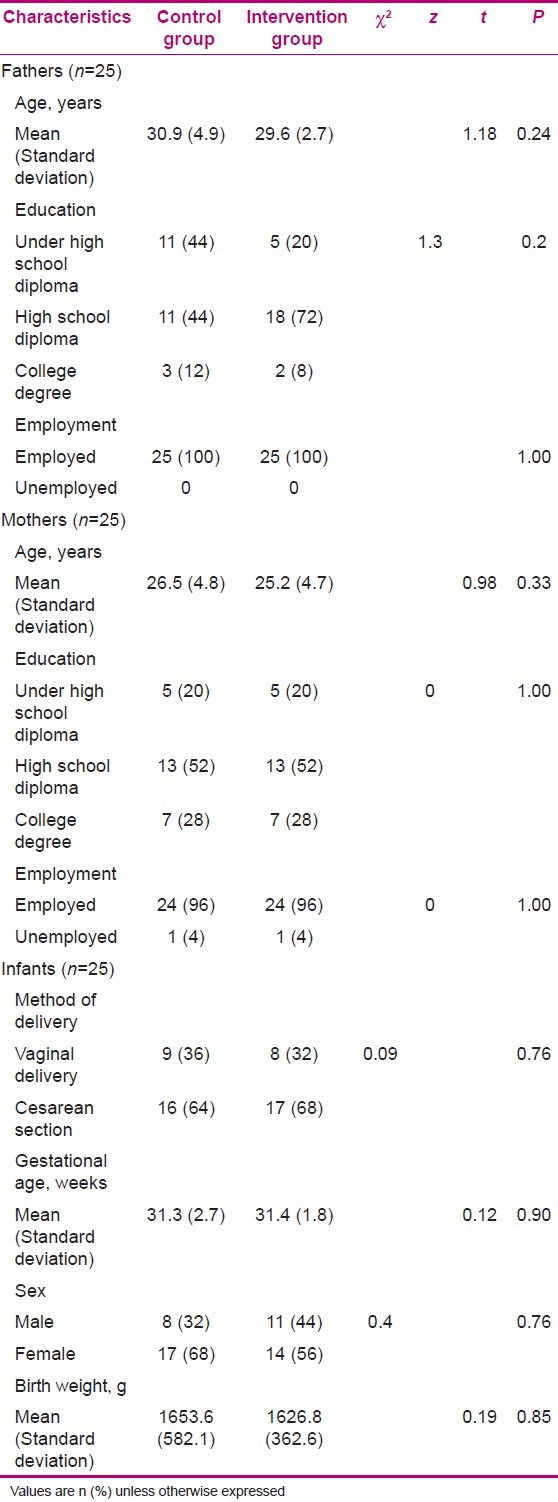
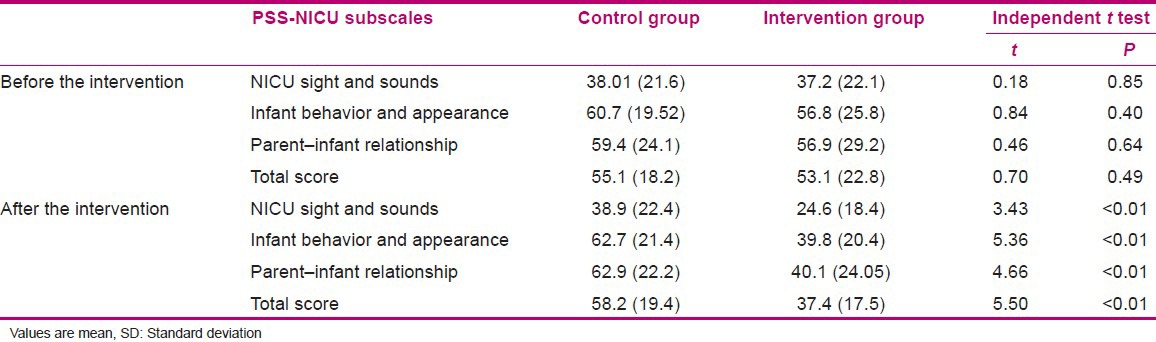
Table 2 compares the two groups with regard to the mean scores of parental stress in total and the three subscales of PSS-NICU before and after the intervention. As it is seen, there was no significant difference between pre- and post-test PSS-NICU scores in the control group (P = 0.21 for total scores and P = 0.75, 0.32, and 0.10 for the subscales of NICU sights and sounds, infant behavior and appearance, and parent–infant relationship, respectively). In the intervention group, however, the total scores of PSS-NICU and the scores of all three subscales showed significant reduction after the intervention compared to baseline values (P < 0.001 for all).
Table 2.
Scores of parents on the parental stressor scale-neonatal intensive care unit and its subscales
DISCUSSION
Our findings showed the efficacy of the intervention in decreasing stress among both mothers and fathers of infants in the NICU. Similarly, Kaaresen et al. showed reduced stress in both parents in the experiment group compared to parents in the control group.[28] Melnyk et al. showed that Creating Opportunities for Parent Empowerment (COPE) could significantly reduce the mean scores of “infant behavior” and “staff behavior” among mothers. However, the mothers’ mean scores in the subscales of “NICU sights and sounds” and “parent–infant relationship” had no significant reduction. In addition, the fathers’ mean scores did not significantly change in any of the four subscales. While the mean total score of maternal stress was also significantly lower than the control group (P = 0.05), there was no significant difference in stress between fathers in the intervention and control groups.[21] Turan et al. reported that the mean scores of mothers in the control and intervention groups had significant differences in the subscales of NICU sights and sounds and parent–infant relationship, but were not significantly different in the subscale of infant behavior and appearance. Besides, the two groups were not significantly different in terms of fathers’ scores in any of the subscales. Likewise, while the mothers’ total stress scores were significantly different between the two groups, such a difference was not observed in case of fathers’ scores.[20] Jafari et al. reduced maternal stress by utilizing COPE.[23] Blanch D’Souza et al. found an inverse relationship between stress and nursing support for the mothers of preterm infants (r = −0.199, P = 0.05).[14] In a study by Ahn and Kim, educational support could reduce stress levels in the fathers of infants in the NICU, but failed to significantly affect maternal stress.[25]
Inconsistencies between the present study and previous research can be justified by the fact that despite individual differences, both parents have to deal with environmental stressors and their infant's hospitalization. As they interact with each other, one's stress will influence the other. In contrast to previous research, we considered both parents as a single unit and examined their stress together. On the other hand, previous studies have mainly focused on educational programs. Nonetheless, nursing support can help parents manage the crisis better. In addition, talking with them will provide an emotional environment where parents can express their feelings.[25] Therefore, we attended to not only training but also emotional support. Religious and ideological differences could also have been responsible for differences between our findings and those of others. As Ekas et al. stated, religion and spiritual trends are effective factors in attaining more reliability and reducing mental suffering.[29] Furthermore, since the parents were allowed to call the researcher at any time, they had the opportunity for communication and continuous education.
CONCLUSION
According to our findings, parental support programs where educational and emotional aspects are simultaneously covered can reduce the stress of both parents. Meanwhile, further studies to assess parents’ stress, needs, and adaptation to altered parental role in various situations are warranted. Barriers to performing family support in the NICU are also another field for further research. Finally, future studies are recommended to include follow-up care in their support program.
This study also had some limitations. Several factors such as the characteristics of the infant, parents, and environmental factors could affect parental process. This study could not consider all the possible effects on parental process and the parent–child interaction and, also, the subsequent impact on parental stress.
ACKNOWLEDGMENTS
This article is an extract of a thesis approved by Isfahan University of Medical Sciences, Isfahan, Iran. Hereby, we are grateful to all participants and the esteemed nurses and staff of Shahid Beheshti Hospital Clinical Research Center. We also appreciate Mr. Hassanzadeh, who helped us by statistical consulting, and the research council of Isfahan University of Medical Sciences, who supported us financially.
Footnotes
Source of Support: Isfahan university of medical science
Conflict of Interest: Nil.
REFERENCES
- 1.Lumsden H, Holmes D. 1th ed. London: Hooder Arnold; 2010. Care of the Newborn by ten teachers; p. 6. [Google Scholar]
- 2.Mathews TJ, Arialdi M, Michelle JK, Donna M, Guyer B. Annual summary of Vital Statistics. J Pediatr. 2011;127:146–57. doi: 10.1542/peds.2010-3175. [DOI] [PubMed] [Google Scholar]
- 3.Ebrahimi S, Haghbin S, PoorMahmoodi A. Incidence and etiologic factors of prematurity. J Armaghane Danesh. 2000;20-19:35–41. [Google Scholar]
- 4.Kellam B, Bhatia J. Sound spectral analysis in the intensive care nursery: Measuring high-frequency sound. J Pediatr Nurs. 2008;23:317–23. doi: 10.1016/j.pedn.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 5.Holditch-Davis D, Bartlett TR, Blickman AL, Miles MS. Posttraumatic stress symptoms in mothers of premature infants. J Obstet Gynecol Neonatal Nurs. 2003;32:161–71. doi: 10.1177/0884217503252035. [DOI] [PubMed] [Google Scholar]
- 6.Shaw RJ, Deblois T, Ikuta L, Ginzburg K, Fleisher B, Koopman C. Acute stress disorder among parents of infants in the neonatal intensive care nursery. Psychosomatics. 2006;47:206–12. doi: 10.1176/appi.psy.47.3.206. [DOI] [PubMed] [Google Scholar]
- 7.Ringland PC. Posttraumatic stress disorder and the NICU graduate mother. J Neonatal Nurs. 2008;4:14–7. [Google Scholar]
- 8.Zelkowitz P, Papageorgiou A, Bardin C, Wang T. Persistent maternal anxiety affects the interaction between mothers and their very low birth weight children at 24 month. J Early Hum Dev. 2009;85:51–8. doi: 10.1016/j.earlhumdev.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 9.Carter JD, Mulder AF, Bartram AF, Darlow BA. Infants in a neonatal intensive care unit: Parental response. Arch Dis Child Fetal Neonatal Ed. 2005;90:F109–13. doi: 10.1136/adc.2003.031641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gale G, Franck SL, Kools S, Lynch M. Parents’perceptions of their infant's pain experience in the NICU International. J Nurs Stud. 2004;41:51–8. doi: 10.1016/s0020-7489(03)00096-8. [DOI] [PubMed] [Google Scholar]
- 11.Broedsgaard A, Wagner L. How to facilitate parents and their premature infant for the transition home. Int Nurs Rev. 2005;52:196–203. doi: 10.1111/j.1466-7657.2005.00414.x. [DOI] [PubMed] [Google Scholar]
- 12.Feijo L, Hernandez-Reif M, Field T, Burns W, Valley-Gray S, Simco E. Mothers’ depressed mood and anxiety levels are reduced after massaging their preterm infants. Infant Behav Dev. 2006;29:476–80. doi: 10.1016/j.infbeh.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 13.Parker L. Mothers’ experience of receiving counseling/psychotherapy on a neonatal intensive care unit (NICU) J Neonatal Nurs. 2011;179:182–9. [Google Scholar]
- 14.Blanch D’Souza SR, Karkada S, Lewis LE, Mayya S, Guddattu V. Relationship between stress, coping and nursing support of parents of preterm infant admitted to tertiary level neonatal intensive care units of Karnataka, India: A cross-sectional survey. J Neonatal Nurs. 2009;15:152–8. [Google Scholar]
- 15.Trombin E, Surcinell P, Piccioni A, Alessandroni R, Faldella G. Environment factors associated with stress in mothers of preterm newborns. J Acta Paediatr. 2008;97:894–8. doi: 10.1111/j.1651-2227.2008.00849.x. [DOI] [PubMed] [Google Scholar]
- 16.Heerman JA, Wilson ME, Wilhelm PA. Mothers in the NICU: Outsiders to partners. J Pediatr Nurs. 2005;31:176–200. [PubMed] [Google Scholar]
- 17.Davis L, Edwards H, Mohay H, Wollin J. The impact of very premature birth on the psychological health of mothers. Early Hum Dev. 2003;73:61–70. doi: 10.1016/s0378-3782(03)00073-2. [DOI] [PubMed] [Google Scholar]
- 18.Hutti MH. Social and professional support needs of families after perinatal loss. J Obstet Gynecol Neonatal Nurs. 2004;34:630–8. doi: 10.1177/0884217505279998. [DOI] [PubMed] [Google Scholar]
- 19.Aagaard H, Hall EO. Mothers’ experience of having preterm infant in the nepnatal care unit: A meta- synthesis. J Pediatr Nurs. 2008;23:26–35. doi: 10.1016/j.pedn.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 20.Turan T, Basbakkal Z, Ozbek S. Effect of nursing intervention on stressor of parents of premature infant in neonatal intensive care unit. J Clin Nurs. 2008;17:2856–66. doi: 10.1111/j.1365-2702.2008.02307.x. [DOI] [PubMed] [Google Scholar]
- 21.Melnyk BM, Feinstein NF, Alpert-Gillis L, Fairbanks E, Crean HF, Sinkin RA, et al. Reducing premature infants’ length of stay and improving parents’ Mental health outcomes with the Creating Aportunities for Parent Empowerment (COPE) Neonatal intensive care unit program: A randomized, controlled trial. J Pediatr. 2006;118:1414–27. doi: 10.1542/peds.2005-2580. [DOI] [PubMed] [Google Scholar]
- 22.Byers JF, Lowman LB, Francis J, Kaigle L, Lutz NH, Waddell T, et al. A Quasi-experimental Trial on Individualized, Developmentally Supportive Family-Centered Care. J Obstet Gynecol Neonatal Nurs. 2006;35:105–15. doi: 10.1111/j.1552-6909.2006.00002.x. [DOI] [PubMed] [Google Scholar]
- 23.Jafari MS, Karahroudy FA, Rasuli M, Zayeri F. Effectiveness of “Parent Empowerment” program on anxiety and stress in mothers who have preterm infants hospitalized in NICUs. J Iran Inst Health Sci Res. 2010;11:240–4. [Google Scholar]
- 24.Browne VJ, Talmi A. Family-based intervention to enhance infant-parent relationships in the neonatal intensive care unit. J Pediatr Psychol. 2005;30:667–77. doi: 10.1093/jpepsy/jsi053. [DOI] [PubMed] [Google Scholar]
- 25.Ahn YM, Kim NH. Parental perception of neonates, parental stress and education for NICU parents. J Asian Nurs Res. 2007;1:199–210. doi: 10.1016/S1976-1317(08)60022-5. [DOI] [PubMed] [Google Scholar]
- 26.Miles MS, Funk SG, Carlson J. Parental Stressor Scale: Neonatal intensive care unit. Nurs Res. 1993;42:148–52. [PubMed] [Google Scholar]
- 27.Miles MS, Holditch-Davis D, Burchinal M, brunssen S. Maternal role attainment with medically fragile infants: The process over the first year of life. J Res Nurs Health. 2011;34:20–34. doi: 10.1002/nur.20419. [DOI] [PubMed] [Google Scholar]
- 28.Kaaresen PI, Ronning JA, Tunby J. A randomized controlled trial of an early intervention program in low birth weight children: Outcome at 2 years. Early Hum Devt. 2008;84:201–9. doi: 10.1016/j.earlhumdev.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Ekas NV, Whitman TL, Shivers C. Religiosity, Spirituality, and Socioemotional functioning in mothers of children with autism spectrum disorder. J Autism Dev Disord. 2009;39:706–19. doi: 10.1007/s10803-008-0673-4. [DOI] [PubMed] [Google Scholar]


