Sir,
Accidental needle stick and sharp object injuries carry major risk factors for blood-borne infections amongst health workers.[1,2] The blood-borne infections that are mostly contracted through occupational hazards are Hepatitis B virus (HBV), hepatitis C virus (HCV) and human immunodeficiency virus (HIV).[3] The risk of transmission of these diseases following percutaneous exposure among healthcare worker is high, with HBV at 37%, HCV at 39% and HIV at 4.4%.[3] Therefore, there is need for health workers to adhere to universal safety precautions in order to avoid injury from needles and other sharp instruments that have been exposed to body fluids or blood products. It is estimated that about 2 million needle stick injuries occur annually among health workers resulting in HBV, HCV, and HIV infections.[3,4] The incidence of needle stick and sharp object injuries varies among health workers globally, though believed to be underreported,[1,5] the percentage of health workers reporting these injuries in some recent studies ranged between 19% and 38%.[2,6,7,8] Among medical and nursing students who are also at a higher risk of blood-borne infection from unsafe practices related to needles and sharps, 11-33% reported injuries with sharp instruments while performing clinical duties,[9,10,11] and very few of them were aware of how sharps injuries are managed.[10,11]
Considering the high HIV prevalence of 11% in the study setting[12] and the risk the health workers are exposed to, it is assumed that health personnel who work with sharp instruments take adequate safety precautions. This study was aimed to understand who the victims of needle stick injury were and how the injuries occurred. This is to highlight where health education for health workers has to be improved and the safety precautions measures that should be provided in a district hospital setting. The study described the pattern of needle stick and sharp object injuries in Newcastle provincial hospital, South Africa over a 2 year period where universal precautions are used and sharp bins are provided for proper disposal of needles and sharp objects.
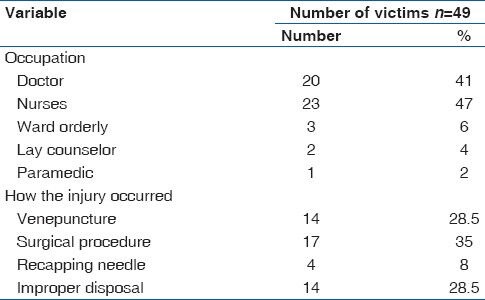
According to laid down policy, HIV enzyme-linked immunosorbent assay (ELISA) test is done and documented at baseline, 6 weeks, 3 months and 6 months in accidental needle stick and sharp object injuries. HIV prophylaxis is given to HIV negative health workers if source patient is positive or chances of being positive are very high. Test for HBV is done at baseline and repeated at 6 month. If the source patient has hepatitis B surface antigen (HBsAg) positive screen and health care worker has hepatitis B surface antibody (anti-HBs) >10 mUI/ml no further action is required. If source patient is positive and exposed healthcare worker has nil or anti-HBs <10 mUI/ml, Hepatitis B immunoglobulin and Hepatitis B vaccine are given immediately.[13] Medical records of all the health workers who sustained accidental needle stick and sharp object injuries in the hospital between January 2007 and December 2008 were reviewed in conjunction with the records at the occupational health unit of the hospital. A total of 49 health personnel reported this injury and their age, sex, occupation, history of previous needle stick injury and how the injury occurred were documented. The data were analyzed using a simple descriptive method with the Microsoft Excel program and the results were presented in tabular form. The median age of the victims was 33 years (range: 20 -62 years). Female were 34 (69%), 41 (84%) of the patients reported needle stick injury for the 1st time while 8 (16%) were reporting the second incident of such injury. Nurses (47%) and doctors (41%) were the professionals mostly affected, and most of the accidental injuries occurred while performing surgical procedures (34%). None of the source patients had HBsAg positive screen, the nine health workers whose risk of HIV exposure were high completed 28 days post-exposure prophylaxis of antiretroviral therapy. None of the health workers tested positive for HIV and HBV virus immediately following occupational exposure and on follow-up for 6 months to 1 year, none of them developed these infections.
As shown in Table 1 below, most of the injuries occurred while doing surgical procedure (34.6%) which is agreement with the literature.[2,6] Doctors and nurses were the groups mostly affected a reflection of the fact that they use sharp objects more than all other health workers in a hospital setting. It is amazing that some health workers were still recapping needles; this practice should be discouraged as sharp bins are provided for disposal of needles and sharp objects in the hospital. Improperly disposed needles were responsible for about 29% of the injuries which is a reflection of the attitude of the health workers in adhering to universal precautions in the work place. There should not be any needle stick injury as a result of improperly disposed needle because sharp bins are provided in the hospital and should be used for this purpose. In conclusion there is a need to provide health education on universal precautions for all health workers on regular basis so that they can always adhere to it, furthermore all health workers should take extra care while performing surgical procedures as they are more likely to be accidentally injured during this period.
Table 1.
Occupation of the victims and how they got injured
References
- 1.Becirovic S, Pranjic N, Sarajlic-Spahic S, Ahmetagic S, Huseinagic S. Assessment of reporting, attitudes and knowledge about the stab incidents and professional risk of viral infection among health care professionals in primary health care. Mater Sociomed. 2013;25:113–7. doi: 10.5455/msm.2013.25.113-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wicker S, Jung J, Allwinn R, Gottschalk R, Rabenau HF. Prevalence and prevention of needlestick injuries among health care workers in a German university hospital. Int Arch Occup Environ Health. 2008;81:347–54. doi: 10.1007/s00420-007-0219-7. [DOI] [PubMed] [Google Scholar]
- 3.Prüss-Ustün A, Rapiti E, Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. Am J Ind Med. 2005;48:482–90. doi: 10.1002/ajim.20230. [DOI] [PubMed] [Google Scholar]
- 4.Wilburn SQ, Eijkemans G. Preventing needlestick injuries among healthcare workers: A WHO-ICN collaboration. Int J Occup Environ Health. 2004;10:451–6. doi: 10.1179/oeh.2004.10.4.451. [DOI] [PubMed] [Google Scholar]
- 5.Voide C, Darling KE, Kenfak-Foguena A, Erard V, Cavassini M, Lazor-Blanchet C. Underreporting of needlestick and sharps injuries among healthcare workers in a Swiss University Hospital. Swiss Med Wkly. 2012;142:w13523. doi: 10.4414/smw.2012.13523. [DOI] [PubMed] [Google Scholar]
- 6.Mbaisi EM, Ng’ang’a Z, Wanzala P, Omolo J. Prevalence and factors associated with percutaneous injuries and splash exposures among health-care workers in a provincial hospital, Kenya, 2010. Pan Afr Med J. 2013;14:10. doi: 10.11604/pamj.2013.14.10.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kakizaki M, Ikeda N, Ali M, Enkhtuya B, Tsolmon M, Shibuya K, et al. Needlestick and sharps injuries among health care workers at public tertiary hospitals in an urban community in Mongolia. BMC Res Notes. 2011;4:184. doi: 10.1186/1756-0500-4-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jacob A, Newson-Smith M, Murphy E, Steiner M, Dick F. Sharps injuries among health care workers in the United Arab Emirates. Occup Med (Lond) 2010;60:395–7. doi: 10.1093/occmed/kqq039. [DOI] [PubMed] [Google Scholar]
- 9.Ozer ZC, Bektas HA. Needles stick injuries during education period in nursing students in Turkey. Procedia Soc. Behav Sci. 2012;46:3798–801. [Google Scholar]
- 10.Saleem T, Khalid U, Ishaque S, Zafar A. Knowledge, attitudes and practices of medical students regarding needle stick injuries. J Pak Med Assoc. 2010;60:151–6. [PubMed] [Google Scholar]
- 11.Varsou O, Lemon JS, Dick FD. Sharps injuries among medical students. Occup Med (Lond) 2009;59:509–11. doi: 10.1093/occmed/kqp103. [DOI] [PubMed] [Google Scholar]
- 12.Shisana O, Rehle T, Simbayi LC, Zuma K, Jooste S, Pillay-van-Wyk V, et al. Cape Town: HSRC Press; 2009. and the SABSSM III Implementation Team. South African national HIV prevalence, incidence, behaviour and communication survey 2008: A turning tide among teenagers? [Google Scholar]
- 13.Department of Health, KwaZulu. Natal Provincial Government. Policy and procedure protocol to be followed following accidental exposure to HIV and Hepatitis B. [Accessed on 2013 Oct 10]. Available from: http://www.kznhealth.gov.za/occhealth.htm .


