Abstract
Background:
Many of the studies have investigated the prevalence and nature of self-medication. It is a common type of self-care behavior among the populace of various countries. World Health Organization promotes the practice of self-medication for effective and quick relief of symptoms without medical consultations to reduce the burden on health-care services, which are often understaffed and inaccessible in rural and remote areas.
Aim:
The aim of the study was to determine the extent and pattern of self-medication among the population (patients) attending pharmacies at study sites and to note the association of self-medication variables with demographic factors.
Subjects and Methods:
The present study was a community based cross sectional study aimed to gather information about the prevalence of self-medication in the rural town of Sahaswan, Uttar Pradesh from June 2012 to July 2012. The sample size comprised of 600 respondents. Data were collected through a prepared questionnaire. All descriptive data were coded, entered and analyzed using the statistical package for Social sciences program version 17.0 (Chicago, IL, USA). Descriptive data analysis was conducted and reported as frequencies and percentage.
Results:
The percentage of patients who were seeking self-medication was approximately 50% (300/600). Most of the patients were seeking self-medication for headache and other pain (23.3% [140/600]), fever (14.5% [87/600]), urinary tract infections (9.7% [58/600]) and respiratory tract infections (11.7% [70/600]). The drugs most commonly purchased for practicing self-medication were non-steroidal anti-inflammatory drugs (25.3% [152/600]), medications used for gastro intestinal problems (20.8% [125/600]) and antibiotics (16.7% [100/600]).
Conclusion:
Prevalence of self-medication was high primarily among illiterate males aged above 15 years with a low income. Patient health awareness programs, assistance by community pharmacists and pharmacist continuing education are necessary for controlling self-medication. There is a need for planning interventions to promote rational self-medication through mass medias such as newspaper, magazine and TV.
Keywords: Community pharmacies, Herbal drugs, Northern India, Over the counter, Self-medication
Introduction
Medication usage refers to the act of consuming medicines for prevention, diagnosis or treatment of diseases. Consumption of correct medication should be monitored by health-care personnel and patients and any harmful symptoms should be reported back to the health-care personnel who can further diagnose and prescribe the needed drugs to alleviate the unwanted symptoms. This is usually followed by filling of such drugs at the pharmacy by the pharmacist.[1,2] William Osler once said that “a desire to take medicine is perhaps a great feature which distinguishes man from animals.”[3]
Self-medication can be defined as the use of drugs to treat self-diagnosed disorders or symptoms, or the intermittent or continued use of a prescribed drug for chronic or recurrent disease or symptoms.[4] Self-medication is an age old practice. Some of the reasons for growth in self-medication are the urge of self-care, feeling of sympathy toward family members in sickness, lack of health services, poverty, ignorance, misbeliefs, extensive advertisement of drugs and availability of drugs in establishments other than pharmacies.
A patient with fever, cold, cough, diarrhea, indigestion or wound infection, might receive expert advice from friends or even total strangers in India about medicines, specially about usage of antibiotics.[5] Sale of antibiotics and prescription drugs which are part of schedule H, by a non-chemist and without a valid prescription are banned according to the Indian Drug and Cosmetics Act of 1945. In India,[1] a large number of people, when they fall sick, do not consult the physician. They either consult a drug store (retail pharmacy) and obtain medicine from the shelf, or consult a neighbor who may be having some tablets left over from his/her previous illness and thus procure the medicine from that neighbor.[6] At times, there is a possibility of nothing untoward happening upon following such advice, but it can still be quite dangerous.[5] Furthermore, the Indian pharmaceutical companies advertise drugs that provide sexual pleasure, prevent hair fall, diabetes, cancer, heart disease and disorder of menstrual flow. Pharmacy owners and chemist shops advertise the drugs that they stock, especially antibiotics to boost their sales. According to drugs and magic remedies act of 1954, Indian drug companies cannot advertise their products via media or in any other way.[1]
World Health Organization (WHO) promotes the practice of self-medication without medical consultations for effective and quick relief of symptoms to reduce the burden on health-care service centers, which are often understaffed and inaccessible in rural and remote areas.[3] Over the counter (OTC) drugs are a form of self-medication. The buyer diagnoses his/her own illness and buys a specific drug to treat it.[4] OTC products provide symptom relief for conditions that do not always require medical intervention. Self-medication has been used very widely to combat behavioral and psychological problems such as smoking. Pharmacists can help patients to choose the right OTC smoking cessation products to help them successfully quit smoking. Up to 300,000 people each year are able to reduce their risk of lung cancer, emphysema, stroke, heart attack and complications in pregnancy because of self-care products which are readily available, for example non-prescription nicotine helps people to quit smoking.[7] However, there is a lot of public and professional concern about the irrational use of drugs. In developing countries like India, easy availability of a wide range of drugs coupled with inadequate health services results in increased proportions of drugs being used as self-medication as opposed to drugs being prescribed by physicians. Although OTC drugs are meant for self-medication and are of proven efficacy and safety, their improper use due to lack of knowledge about their side effects and interactions could have serious implications, especially in extremes ages (children and old ages) and during special physiological conditions like pregnancy and lactation. There is always risk of unknown interactions between active ingredients present in OTC drugs and prescription medicines as well as increased risk of worsening of existing disease pathology.[8]
Previous studies have shown that the prevalence of antibiotic related self-medication to be 37% in rural India[1] and overall self-medication to be 31.3% in urban India.[9] Very few studies have focused on overall self-medication in rural areas in India. The present studies aims to (a) look at the self-medication practices among the rural population, (b) study the factors associated with self-medication and (c) identify the drug classes used for self-medication and the common ailments for which self-medication is sought. The purpose of this study was to determine the extent and pattern of self-medication among customers attending community pharmacies in a rural area Sahaswan in the state of Uttar Pradesh.
Subjects and Methods
A cross-sectional study was carried out at community pharmacies in a rural town Sahaswan, Uttar Pradesh, over a period of 42 days; from June to July 2012. Self-medication data were collected from well stocked licensed retail pharmacies located in Sahaswan, 6 pharmacies (out of 40 Pharmacy) was randomly selected as the study site. The inclusion criteria identified was the purchasing of medicines from the community pharmacies without prescription. The data was collected by conducting the interview with patients when they exited from the pharmacy. The questionnaire draft was adopted from our previous study[1] and modified accordingly based on input from our study population. The modified questionnaire was provided to around 40 patients and 6 pharmacists to confirm the understanding and acceptability. Changes were made and newly prepared questionnaire was used throughout the study. Questionnaires were filled by asking each question verbally to the customer in Hindi. Contents of the questionnaire were: Demographic details, how often customers practiced self-medication, sources from where they came to know about choices of drugs, reasons for practicing self-medication and perception about self-medication practice. Sample size calculation as recommended by the WHO document was done to determine the population required for the study. The WHO document recommends there should be 600 patients (20 facilities and 30 patients/prescriptions per facility) per survey.[4]. In this study, 6 pharmacies were used to procure data related to self-medication. Since the amount of time to get these interviews varied per shop 100 interviews per facility were conducted in 7 days. Initially 40 pharmacies were identified, than 20 pharmacies were screened which were located within the 2.5 mile radius. Out of the 20 pharmacies, 6 pharmacies were selected on the basis of stock maintenance, reputation, accessibility and sales turn over. An informed consent form was given to the customers.
Statistical analysis
All data were coded, entered and analyzed using the statistical package for Social sciences program version 17.0 (Chicago IL, USA). Descriptive data analysis was conducted and reported as frequencies and percentage to identify the socio demographic characteristics of the population practicing self-medication, there a sons for practicing self-medication, the different drug classes used for self-medication and the ailments treated through self-medication.
Results
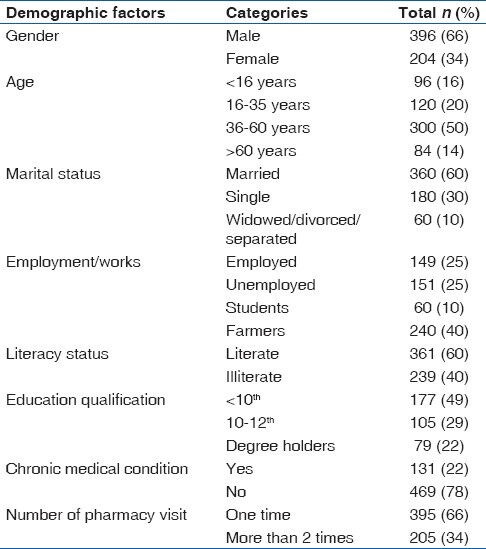
Out of 1600 subjects, 800 came to purchase medicines without prescription and out of those 800, 600 agreed to participate in the study. Response rate was 75% (600/800). Among the respondents, 66% (396/600) of the participants were males and 34% (204/600) were females. Demographic characteristics such as age, marital status, employment status, literacy status, educational level, occupation related to health-care, smoking habit and alcohol consumption were represented in Table 1. Majority of the respondents belonged to the age group of 36-60 years (50% [300/600]). 361 respondents [60% (361/600)] were literate, 60% (360/600) respondents were married and 40% (240/600) were farmers. 22% (131/600) subjects had chronic diseases and 66% (395/600) subjects visited the pharmacy at least once in seven days during the study period.
Table 1.
Demographic characters of the study data
Consumers’ frequency and perception about self-medication are presented in Table 2. 50% (300/600) of the study population were taking self-medication rarely, 33% (200/600) self-medicated occasionally and 17% (100/600) practiced self-medication weekly. Some of the primary reasons for practicing self-medication were high treatment costs in hospitals (40% [240/600]), simple nature of the disease (15% [90/600]) and knowledge about the disease and medication to be taken (15% [90/600]). When asked about the source of information for practicing self-medication, consumers stated that they primarily took advice from family, friends and neighbors [33% (198/600)], sought information from media (25% [150/600]) or from a pharmacist (22% [132/600]) respectively.
Table 2.
Customers frequency and perception about self-medication
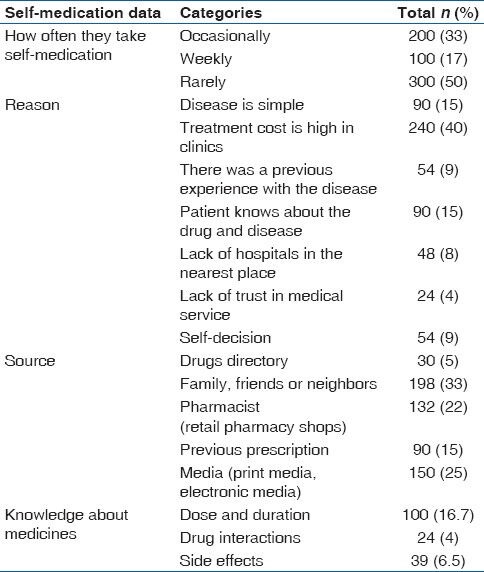
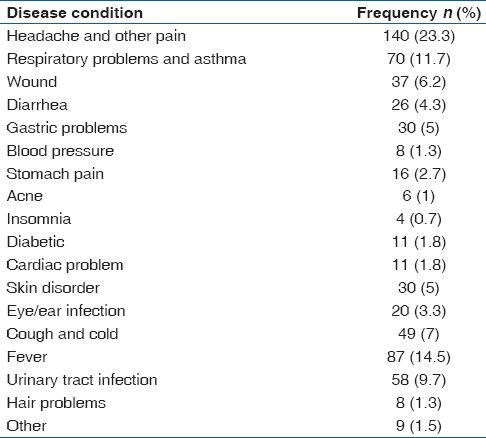
Table 3 shows most commonly used medications for self-medication: Non-steroidal anti-inflammatory drugs (NSAIDs) (25.3% [152/600]) antihistamines (19.7% [115/600]) with the most common being cetirizine (10% [60/600]) and pheniramine maleate (8% [48/600]), gastrointestinal drugs (20.8% [125/600]) with the most common being ranitidine (9.2% [55/600]) and antibiotics (16.7% [100/600]) with the most common being tetra cyclines (8.2% [49/600]). The ailments for which self-medication was practiced are represented in Table 4. These comprise of mainly headache and other pain (23.3% [140/600]), fever (14.5% [87/600]), urinary tract infection (9.7% [58/600]), cough and cold (7% [49/600]).
Table 3.
Frequencies of drug classes commonly used for self-medication
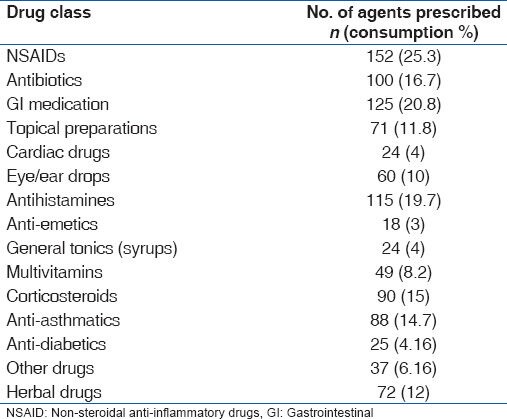
Table 4.
Frequencies of common ailments for which medicines were used
Discussion
The prevalence of self-medication among the study site population was high. In this study, self-medication was reported to be extensively practiced in about one third of the study sample. Similar studies were carried out in Erode[10] and Nepal[11] and the prevalence rate was found to be 62% and 59% respectively. The results of our study indicated that mostly males were practicing self-medication. Some of the reasons might be that the males in our study had higher purchasing power and were employed.[11] In other studies, the influence of gender on self-medication practice was inconclusive. In a study conducted in West Nepal males practiced self-medication more compared with females.[11] In another study conducted in Erode, South India; it was reported that both genders practiced self-medication to an equal extent.[10] High prevalence of self-medication that was found within the adult participants aged >15 years (84%) and their children (16%) could be explained by a number of factors, including the nature of the rural Indian population, illiteracy, lack of knowledge about side effects and other complications due to use of antibiotics and other medications. Highest proportion of subjects who practiced self-medication was aged between 36 and 60 years. This finding differed from other studies conducted at Erode, South India where the highest prevalence of self-medication was among respondents aged 26-40 years, at Nepal where the highest prevalence of self-medication was among respondents aged 20-39 years and Hong Kong where the highest prevalence of self-medication was among respondents aged 15-49 years.[12] The prevalence of self-medication in previous studies conducted in different parts of the world have ranged from 12.7% to 95%.[13,14] Since the characteristics of the study population and the health-care systems differ from country to country, results cannot be compared.
The reason cited for self-medication by responders in this study was that treatment cost was high in clinics and that the nature of the disease was simple. The reasons were similar to a previous study conducted by Ahmad et al.[1] and other previous studies as well.[10,15] Our results indicated that family, friends or neighbors, previous prescription and pharmacists were the source from where the respondents got information about the choice of drug for practicing self-medication. These results were similar to the studies conducted in east Hong Kong,[12] rural north India[1] and in Erode, South India respectively.[10] Even though, the majority of the people practicing self-medication rely on the information about medications on their friends, family or neighbors; few people are actually aware about the interactions and side-effects of the drugs that they take. Drug advertisements were also an important source of medication for practicing self-medication. Although patients’ use of advertised medicines could have important health benefits if used appropriately in the early stages of disease, many advertised products are life-style medications used for symptomatic treatments and even though they might relieve the discomfort, they might also result in increased complications and hospital admissions as a result of uncontrolled disease pathology. There is an increased need to promote awareness about the ill-effects of self-medications among middle aged to elderly people with limited literacy in India.
Present study also indicates low knowledge about dose and duration, drug interactions and side effects of commonly used drugs. Respondents knowledge about the above parameters were extracted by asking direct questions or by indirectly enquiring about drug use in sub-therapeutic dosage for inadequate period or over use of drugs or use of drugs with a potential to aggravate the existing pathology or concomitant drug use with potential interactions. Even in developed countries like United States, it has been seen that the misuse of non-prescription drugs causes tens of thousands of unnecessary hospitalizations each year.[16] In a drug utilization study in United States, it was found that medications that are contraindicated in pregnancy were used at unexpectedly high rate as OTC drugs in obstetric population.[17]
Headache and other pain and fever were the most common diseases for which respondents practiced self-medication. Paracetamol (with other medicine combinations such as diclofenac, ibuprofen, nimesulide and dicyclomine) and NSAIDS were the most common type of drugs used for self-medication. These results were similar to other studies conducted in other countries.[1,10,15] There may be two major problems regarding self-medication with analgesics. The first problem is the possible risk of nephropathy and the second problem is a possible drug-induced gastric ulceration. NSAIDS like nimesulide are nephrotoxic and either are banned or withdrawn from the market in several developed countries due to the occurrence of severe adverse events. Gastrointestinal medications were the 2nd most commonly used drugs for self-medication out of which ranitidine was the most commonly used followed by proton pump inhibitors These findings were similar to other studies conducted in rural North India[1] and Erode, South India.[10] Antibiotics (16.67%) were the 3rd most widely used medication and these were used to treat respiratory infections, diarrhea and other problems. This indicates the belief among the community that antibiotics can treat and eradicate any infections irrespective of their origin. It also revealed that the participants were unaware of the dangers and consequences of inappropriate use of antibiotics. Influenza and cold are self-limiting and do not need antibiotics.[1] A major problem with self-medication with antibiotics is the emergence of drug resistance particularly in developing countries.[18,19] Though many of the medications that people use for self-medication are pain killers and antibiotics, some of the medications were also used for managing chronic disease conditions such as BP, diabetes, cardiac problems, urinary tract infections, asthma and respiratory issues. This is alarming since intake of medications for chronic disease conditions is prohibited without physician supervision. In our study, 12% patients used herbal and homeopathic medications. There is a trend toward the use of herbal medications (Ayurvedics, Unani) and Homeopathic medications for acute and chronic illnesses. Moreover herbal and homeopathic medications are considered safe and devoid of adverse effects, but the risk of possible drug interactions is always prevalent with their use.[20] Misdiagnosing the illness by physicians, allergic reactions, intake of insufficient dosage, habituation to antacids, cough syrups and pain relievers, increased risk of stroke due to analgesic intake in patients with blood pressure and congenital anomalies and birth defects in unborn babies of pregnant women are some of the other disadvantages associated with self-medication.[21]
This is one of the few studies that look at the self-medication practiced by the people residing in a village in Northern India. There are fewer health-care facilities in rural areas compared to cities and hence there is a higher possibility that people perform self-medication. Also people residing in rural areas have a lower socioeconomic status compared to people residing in the city, which might explain the lack of funds for treatment in health clinics. Studies of pharmaceutical practice in India have called attention to the role played by pharmacists and pharmacy attendants in fostering self-medication and medicine experimentation among the public. It is argued that the economic rationale and the symbiotic relations that exist between doctors, medical representatives, medicine wholesalers and community pharmacies prevent ethical practice and impede appropriate drug distribution to the needy. The study is not without limitations. Its cross-sectional nature does not permit causal inferences. The data were based solely on self-report which increase the likelihood of recall bias.
The topic for the study, i.e., self-medication is a controversial topic. Government needs to establish a committee to check into pharmacies/chemist shops which are unlicensed, stop the illegal distribution of drugs and penalize the pharmacists/chemists practicing the same. There seems to be laws available for offenses, but lack of enforcement is a major hurdle in executing punishment in India. Future research should focus on interventions to create awareness about self-medication among Indians with limited literacy. The social and economic importance associated with self-medication should be understood by health-care providers as well as consumers. A collaborative relationship between patients, pharmacists and physicians can affect responsible self-medication.[22] Research should also look at how medication access can be improved for rural areas and how health-care professionals can improve awareness about the disadvantages of self-medication among the populace. Health policies should be developed and implemented to prevent the OTC sale of prescription medications.
Conclusion
The prevalence of self-medication in the community at the study site was high. This may reflect the trends in the entire rural part of Uttar Pradesh and North India as well. Self-medication was higher in people with less education or in people, who were illiterate, had low income, were males and those aged above 15 years. Pharmacists have to inform and educate customers. A forum or workshop should be organized for community pharmacists regularly to update and improve their knowledge. In simple ways, awareness about self-medication can be created through media such as newspaper, magazine and TV.
Acknowledgments
The authors are grateful to Dr. P. K. Manna, coordinator PharmD program, Annamalai University, for his constant encouragement, valuable insight and facilities at all stages of this work and all patients those are participated in our study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Ahmad A, Parimalakrishnan S, Patel I, Kumar NV, Balkrishnan TR, Mohanta GP. Evaluation of self-medication antibiotics use pattern among patients attending community pharmacies in rural India, Uttar Pradesh. J Pharm Res. 2012;5:765–8. [Google Scholar]
- 2.Banerjee I, Bhadury T. Self-medication practice among undergraduate medical students in a tertiary care medical college, West Bengal. J Postgrad Med. 2012;58:127–31. doi: 10.4103/0022-3859.97175. [DOI] [PubMed] [Google Scholar]
- 3.Phalke VD, Phalke DB, Durgawale PM. Self-medication practices in rural Maharashtra. Indian J Community Med. 2006;31:34–5. [Google Scholar]
- 4.World Health Organization; 2000. [Last accessed on 2011 Sep 30]. Guidelines for the regulatory assessment of medicinal products for use in self-medication. WHO/EDM/QSM/00.1. Available from: http://www.apps.who.int/medicinedocs/en/d/Js2218e/ [Google Scholar]
- 5.Li LJ, Wang PS. Self-medication with antibiotics: A possible cause of bacterial resistance. Med Hypotheses. 2005;65:1000–1. doi: 10.1016/j.mehy.2005.05.018. [DOI] [PubMed] [Google Scholar]
- 6.Barar FS. Dangers of self-medication. 2005. [Last accessed on 2011 Sep 30]. Available from: http://www.boloji.com .
- 7.You JH, Wong FY, Chan FW, Wong EL, Yeoh EK. Public perception on the role of community pharmacists in self-medication and self-care in Hong Kong. BMC Clin Pharmacol. 2011;11:19. doi: 10.1186/1472-6904-11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharma R, Verma U, Sharma CL, Kapoor B. Self medication among urban population of Jammu city. Indian J Pharmacol. 2005;37:37–45. [Google Scholar]
- 9.Lal V, Goswami A, Anand K. Self-medication among residents of urban resettlement colony, New Delhi. Indian J Public Health. 2007;51:249–51. [PubMed] [Google Scholar]
- 10.Samuel SS, Prakasam KC, Nandhakumar N. Assessment of selfmedication among patients attending community pharmacises in Erode, India. Int J Pharm Pharm Sci. 2011;3:258–62. [Google Scholar]
- 11.Shankar PR, Partha P, Shenoy N. Self-medication and non-doctor prescription practices in Pokhara valley, Western Nepal: A questionnaire-based study. BMC Fam Pract. 2002;3:17. doi: 10.1186/1471-2296-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.You JH, Wong FY, Chan FW, Wong EL, Yeoh EK. Public perception on the role of community pharmacists in self-medication and self-care in Hong Kong. BMC Clin Pharmacol. 2011;11:19. doi: 10.1186/1472-6904-11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kasilo OJ, Nhachi CF, Mutangadura EF. Epidemiology of household medications in urban Gweru and Harare. Cent Afr J Med. 1991;37:167–71. [PubMed] [Google Scholar]
- 14.Figueiras A, Caamaño F, Gestal-Otero JJ. Sociodemographic factors related to self-medication in Spain. Eur J Epidemiol. 2000;16:19–26. doi: 10.1023/a:1007608702063. [DOI] [PubMed] [Google Scholar]
- 15.Zafar SN, Syed R, Waqar S, Zubairi AJ, Vaqar T, Shaikh M, et al. Self-medication amongst university students of Karachi: Prevalence, knowledge and attitudes. J Pak Med Assoc. 2008;58:214–7. [PubMed] [Google Scholar]
- 16.World Health Organization (WHO) Drug information Clearly better? US consumers benefit from new non prescription drug labels. [Last accessed on 2013 Jun 6];Essent Drugs Monit. 1999 27:10. Available at: http://apps.who.int/medicinedocs/pdf/h1467e/h1467e.pdf . [Google Scholar]
- 17.Glover DD, Amonkar M, Rybeck BF, Tracy TS. Prescription, over-the-counter, and herbal medicine use in a rural, obstetric population. Am J Obstet Gynecol. 2003;188:1039–45. doi: 10.1067/mob.2003.223. [DOI] [PubMed] [Google Scholar]
- 18.Bronzwaer SL, Cars O, Buchholz U, Mölstad S, Goettsch W, Veldhuijzen IK, et al. A European study on the relationship between antimicrobial use and antimicrobial resistance. Emerg Infect Dis. 2002;8:278–82. doi: 10.3201/eid0803.010192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grigoryan L, Monnet DL, Haaijer-Ruskamp FM, Bonten MJ, Lundborg S, Verheij TJ. Self-medication with antibiotics in Europe: A case for action. Curr Drug Saf. 2010;5:329–32. doi: 10.2174/157488610792246046. [DOI] [PubMed] [Google Scholar]
- 20.Ruiz ME. Risks of self-medication practices. Curr Drug Saf. 2010;5:315–23. doi: 10.2174/157488610792245966. [DOI] [PubMed] [Google Scholar]
- 21.Times News Network. Dangers of self. medication. Times of India. 2012. [Last accessed on 2012 May 06]. Available from: http://www.articles.timesofindia.indiatimes.com/2012-05-09/bangalore/31641121_1_antimicrobial-resistance-prescription-drugs-antibiotics .
- 22.Jain P, Sachan A, Singla RK, Agrawal P. Statistical study on self medication pattern in haryana, India. Indo Global J Pharm Sci. 2012;2:21–35. [Google Scholar]


