Abstract
Background:
More than 40 oral manifestations of human immunodeficiency virus (HIV) infection have been recorded and between 70% and 90% of persons with HIV infection will have at least one oral manifestation at some time during the course of their disease. Oral health-care workers (OHCWs) are therefore, key players in the prevention and management of HIV-infection.
Aim:
The aim of this study was toassess the perceptions of the OHCWs from a Teaching Hospital in Nigeria toward HIV transmission in dental practice and occupational risk.
Subjects and Methods:
A cross-sectional study. A self-administered questionnaire was used for data collection. A total of 113 OHCWs comprising students, house officers, resident doctors, dental nurses and consultants participated. Analysis was by Statistical Package for the Social Sciences version 17 (SPSS Inc., Chicago, IL, USA). Data analysis included descriptive statistics (frequency distribution and cross tabulation).
Results:
More than half 64/113 (56%) of the respondents were in the age group 20-30 years and females 68/113 (60%). Though 88% (100/113) of the respondents demonstrated a good knowledge about HIV transmission, 82/113 respondents (72%) disagreed that the risk of HIV transmission in the dental clinic was very low. 82.4% (93/113) did not know that saliva contains anti-HIV activity while 46% (52/113) agreed that pure saliva does not contain the virus except when contaminated by blood. 86.7% (98/113) of the OHCWs disagreed that dental professionals have a lower risk of being infected with HIV compared with other health-care providers.
Conclusion:
The OHCWs studied manifested some inaccurate perception of occupational risks as regards HIV transmission in dental practice. This could lead to potential stigma and discrimination of people living with HIV/acquired immune deficiency syndrome and thus hindering efforts geared at curtailing the spread of the virus.
Keywords: Dental practice, Human immunodeficiency virus transmission, Occupational risk
Introduction
The acquired immune deficiency syndrome (AIDS) is a major cause of death in Africa today and it is estimated that 80% of the over 40 million people living with human immunodeficiency virus (HIV)/AIDS (PLWHA) world-wide are residing in sub-Saharan countries.[1] In Nigeria, AIDS was first reported in 1986 following the positive diagnosis of a 13-years-old hawker.[1] Nigeria represents a significant population of PLWHA.[2] HIV and AIDS have profoundly affected every aspect of the public health sector and the infection constitutes an unparalleled public health challenge.[3]
Health-care workers are key players in the prevention and management of HIV-infection.[4] This includes oral health-care workers (OHCWs) who have a significant role to play in the overall health-care delivery to patients with HIV/AIDS.[1] More than 40 oral manifestations of HIV infection have been recorded and between 70% and 90% of persons with HIV infection will have at least one oral manifestation at some time during the course of their disease.[5] Therefore, PLWHA have special needs for dental care[6] and the number of patients with HIV/AIDS who receive dental care is increasing.[7] Many of the oral lesions that may develop with HIV infection cause significant pain and discomfort and the failure to obtain appropriate dental care may be life-threatening in some cases. In general speaking, oral manifestations of HIV infection are important diagnostic signs, with certain lesions signaling progression of the illness. The oral manifestations of HIV infection are in addition to the normal range of oral diseases common to the general population, which also require treatment.[7]
HIV is primarily transmitted through sexual contact, parental exposure to contaminated blood and blood products and perinatally from infected mothers to their infants. Transmission by blood and blood products essentially occur through the use of contaminated needles or sharp objects and also through transfusion with contaminated blood. Adequate knowledge and effective anti-transmission measures such as taking universal precautions in the handling of blood and other body fluids are important factors in minimizing the risk of HIV transmission in the health-care setting.[8] The unique nature of most oral health procedures, instrumentation and patient-care settings requires specific strategies and protocols aimed at preventing the transmission of HIV/AIDS between oral health-care providers and patients as well as between patients themselves.[3]
Occupational exposure of HIV has been intensively studied and monitored. Percutaneous, mucous membrane and cutaneous exposures to contaminated body fluids constitute possible sources of viral exposure in many health-care settings.[9] Viruses can be transmitted in health-care settings including dentistry, albeit rarely, notably where standard infection control measures are not implemented. Available information indicates that the risk of HIV transmission in the dental office is very low.[10] There is general agreement that there can be some risk of HIV transmission from an HIV-infected health-care professional to a patient, but it is small and may be minimized by the use of standard infection-control measures.[10] When compared with other health-care providers, dental professionals have a lower risk of being infected with HIV, due to the decreased amount of viral load in saliva, which contains anti-HIV activity though another author reported that “Pure saliva does not contain viruses unless contaminated by blood.”[11] Therefore; the possibility of HIV transmission in the oral health-care setting is very rare. In view of this information, this study aimed to assess the perceptions of the OHCWs from a Teaching Hospital in Nigeria toward HIV transmission in dental practice and occupational risk.
Subjects and Methods
It was a descriptive cross-sectional study involving OHCWs of a Teaching Hospital in Lagos, Nigeria. The hospital is a major referral center for the people in Lagos State and its environs. Patients seen here comprise a heterogeneous group of people of various ethnic and socio-economic groups. Most cadres of OHCWs are represented here. The Dean of the Faculty of Dentistry granted permission for the study. For the purpose of this study, an OHCW was defined as a person who by virtue of normal duties, obligations and/or training has some form of clinical contact with patients in the clinics. By clinical contact, the administrative staff, cleaners, security guards and dental technologists were excluded. Therefore, those fulfilling the inclusion criteria for this study were consultants, resident doctors, house officers, final year dental students, dental nurses, dental therapists, dental surgery assistants or dental health technicians.
A self-administered questionnaire adapted from similar validated instruments from previous studies and pre-tested on OHCWs in the Government Dental Center, Jos was used for data collection. The questionnaire had a brief introduction explaining the purpose of the study and requesting the participation of the respondents. It also contained sections on the demography of the respondents, general knowledge on HIV/AIDS, transmission of the virus, knowledge on occupational risks and questions on the attitudes of the OHCWs toward people living with HIV/AIDS (PLWHA). The retrieved questionnaires were vetted and entered into a computer. Data entry and statistical analysis were performed with the Statistical Package for the Social Sciences for Windows version 17.0 (SPSS Inc., Chicago, IL, USA). Data analysis included descriptive statistics (frequency distribution and cross tabulation).
Results
A total of 113 OHCWs participated. Their demographic characteristics are summarized in Table 1. Many (100/113, 88%) of the respondents demonstrated a good knowledge of the different routes of HIV transmission. However, 9% (11/113) thought contact with the vomit of an infected patient, casual kissing 10/113 (8%) and exposure of intact skin to infected blood and body fluids (47/113, 41.6%) could lead to HIV infection [Table 2]. The respondent's opinion about possessing adequate knowledge on the transmission of HIV is shown in Figure 1.
Table 1.
Demography of respondents
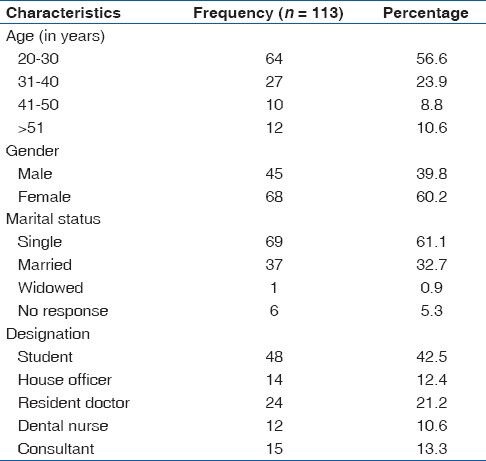
Table 2.
The knowledge of the different methods of HIV transmission by the respondents
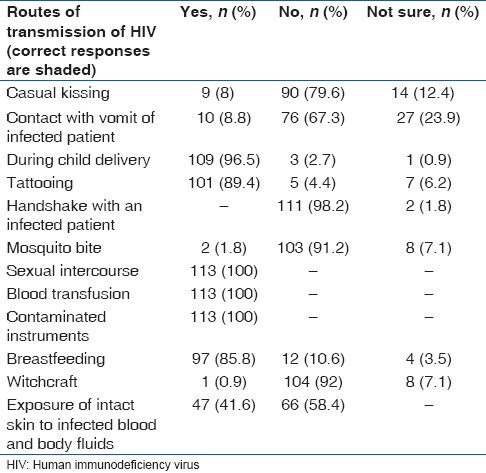
Figure 1.
Respondent's belief that they have adequate knowledge about the transmission of human immunodeficiency virus
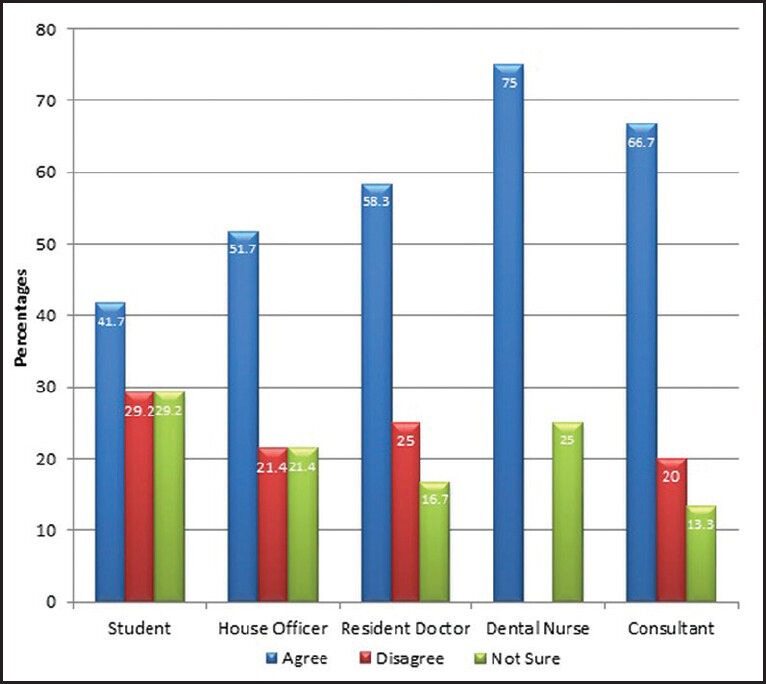
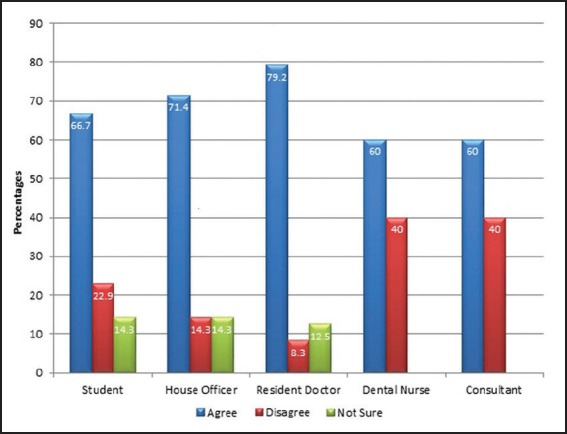
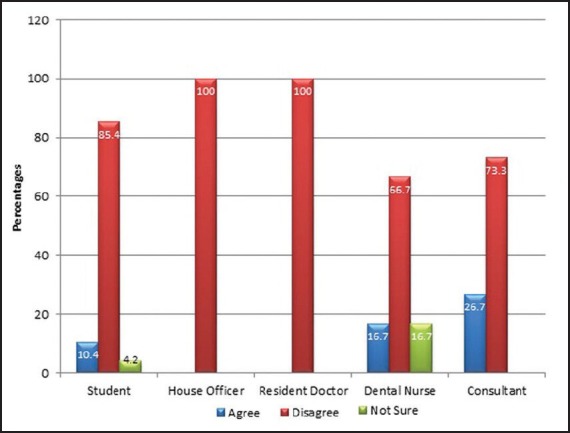
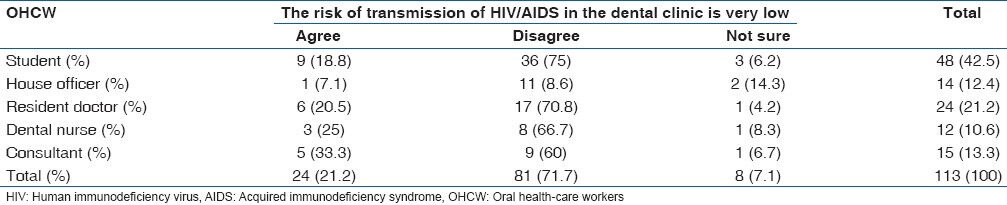
Though 52/113 (46%) of the OHCWs agreed that pure saliva does not contain the virus except when contaminated by blood, 82.4% (93/113) did not know that the saliva contains anti-HIV activity. 85/113 (75.2%) disagreed that PLWHA should be quarantined or isolated nevertheless; most agreed that the statuses of the patients should be boldly written on the front page of their clinical files [Figure 2]. 86.7% (98/113) of the OHCWs disagreed that dental professionals have a lower risk of being infected with HIV compared to other health-care providers [Figure 3]. Most of the respondents 93/113 (82.3%) noted that they needed “special” trainings on the management of PLWHA. This proportion includes 91% (33/36) of the resident doctors and dental nurses though 60% (68/113) of the respondents had attended at least a seminar or workshop on the management of HIV/AIDS. Table 3 shows the designation of the OHCWs and their knowledge of the risk of HIV transmission in the dental clinic. 75/113 (66%) respondents were of the view that the available infection control procedures available in the hospital may not be sufficient to avoid the transmission of the virus.
Figure 2.
Respondent's view when asked whether patients with human immunodeficiency virus/acquired immune deficiency syndrome should have their status boldly written on their case notes
Figure 3.
Dental professionals have a lower risk of being infected with human immunodeficiency virus compared to other health-care providers
Table 3.
OHCW and their knowledge of the risk of HIV transmission in the dental clinic
Discussion
The OHCWs studied manifested some inaccurate perception of occupational risks as regards HIV transmission in dental practice. As the numbers of people with HIV infection and AIDS increase, so will the contribution required from dental practitioners.[12] It can be expected that the number of patients with HIV/AIDS who will receive dental care will continue to increase.[7] Dental care is therefore of great importance in the care of these patients[6] and the role of OHCWs in meeting the health-care needs of patients infected with HIV/AIDS is imperative.[7] Nonetheless, the oral health-care environment has become a helpful setting for early detection as most lesions of HIV infection present orally during the first stages of the disease.[13] Ignorance of the risk of HIV transmission during dental procedures may have led many dentists to refuse to treat HIV-positive individuals. In addition, infected dental professionals have sometimes been prevented from practicing dentistry. Some factors, which might be responsible for these misconceptions are the inaccurate perception of occupational risk, i.e., over estimating the chances of acquiring an infection from the dental practice, poor attendance at dedicated seminars or workshops on the management of HIV/AIDS. This is confirmed by the desires of the respondents that they needed “special” trainings on the management of PLWHA. Since HIV/AIDS is still endemic in this country and its oral manifestations a very common presentation, it can be expected that there would be the need for OHCWs to address these concerns. As such, efforts to demystify the myths concerning HIV in oral health should be pursued to encourage a selfless, discrimination free service to the population of patients living with HIV/AIDS.
Reports had shown in samples of health-care professionals including physicians, midwives, nurses, medical students and nursing auxiliaries that scientific knowledge about transmissibility of HIV infection was poor: Transmission was believed possible by living together without having sex (7%), by breastfeeding a HIV-positive child (9%), by using toilets after a HIV-positive patient (13%) and by blood donation (76%).[4,14] In Saudi Arabia, not only did many physicians have misinformation about modes of transmission of HIV (e.g., 13.8% identified mosquito bites and 49.7% implicated casual kissing), 33.8% were unaware that tattooing is a known mode of transmission.[15] This study also confirms such reports as some of the respondents erroneously affirmed that exposure of intact skin to infected blood and body fluids, casual kissing and mosquito bites are sources of HIV transmission. Reports of studies on oral health-care providers in the Pacific showed that the major reasons for their unwillingness to provide care to PLWHA was fear of HIV transmission in the dental clinics, inadequate infection control procedures in the clinics to prevent cross transmission and that they lacked knowledge about HIV patient management in dental clinics.[16] The respondents in this study were also of the view that the infection control procedures available in the hospital may not be sufficient to avoid the transmission of the virus.
At the 6th World Workshop on Oral Health and Disease in AIDS, which took place from 21 to 24 April 2009 in Beijing, China, the participants from over 30 countries having analyzed the scientific evidence that has become available over the last 20 years relating to the transmission of HIV in the dental setting from oral health-care professionals to patients; noted and considered the inconsistencies in the regulation of the ability of an HIV positive oral health-care professional to continue the practice. They concluded that the evidence now supports the view that oral health-care professionals with HIV do not pose a risk of transmission to patients in the dental setting (provided adequate universal infection control practices are followed).[17]
The fact that the study did not cover the entire intended study population (due to outside and rotational postings to other departments) is a limitation of the study in the sense that the response from the other (unavailable) OHCWs could have had some significant influence on the findings. The study is also limited to an institution in Lagos and therefore cannot be said to be representative of all OHCWs in the state and by extension, in the country. Nevertheless, it had been able to give a snapshot of the knowledge of OHCWs in a Teaching Hospital on dental practice, HIV transmission and occupational risks
Conclusion
This study has shown that there are still some misconceptions about the true nature and transmission of the HIV among OHCWs. The poor knowledge of the respondents in this study concerning the low risk of HIV transmission and lower risk comparatively between the dental care worker and other health-care professional could lead to potential stigma and discrimination of PLWHA and thus hindering efforts geared at curtailing the spread of the virus. Continuous in-service training should be instituted to dispel misconceptions about HIV transmission in dental practice.
Acknowledgment
I want to thank all the OHCWs who volunteered to participate in this study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Adedigba MA, Ogunbodede EO, Fajewonyomi BA, Ojo OO, Naidoo S. Gender differences among oral health care workers in caring for HIV/AIDS patients in Osun State, Nigeria. Afr Health Sci. 2005;5:182–7. doi: 10.5555/afhs.2005.5.3.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sadob AE, Fawole AO, Sadoh WE, Oladimeji AO, Sotiloye OS. Attitude of health-care workers to HIV/AIDS. Afr J Reprod Health. 2006;10:39–46. [PubMed] [Google Scholar]
- 3.Greeff M, Phetlhu R. The meaning and effect of HIV/AIDS stigma for people living with AIDS and nurses involved in their care in the North West province, South Africa. Curationis. 2007;30:12–23. doi: 10.4102/curationis.v30i2.1066. [DOI] [PubMed] [Google Scholar]
- 4.Hentgen V, Jaureguiberry S, Ramiliarisoa A, Andrianantoandro V, Belec M. Knowledge, attitude and practices of health personnel with regard to HIV/AIDS in Tamatave (Madagascar) Bull Soc Pathol Exot. 2002;95:103–8. [PubMed] [Google Scholar]
- 5.Ogunbodede EO, Folayan MO, Adedigba MA. Oral health-care workers and HIV infection control practices in Nigeria. Trop Doct. 2005;35:147–50. doi: 10.1258/0049475054620707. [DOI] [PubMed] [Google Scholar]
- 6.Wiltshire AD, Ross MW, Brimlow DL. Empathic communication between dental professionals and persons living with HIV and AIDS. J Dent Educ. 2002;66:86–93. [PubMed] [Google Scholar]
- 7.Cohen LA, Romberg E, Grace EG, Barnes DM. Attitudes of advanced dental education students toward individuals with AIDS. J Dent Educ. 2005;69:896–900. [PubMed] [Google Scholar]
- 8.Askarian M, Hashemi Z, Jaafari P, Assadian O. Knowledge about HIV infection and attitude of nursing staff toward patients with AIDS in Iran. Infect Control Hosp Epidemiol. 2006;27:48–53. doi: 10.1086/500002. [DOI] [PubMed] [Google Scholar]
- 9.Nigerian Institute of Medical Research. Published by Niyi Faniran (Nig) Ent; 2006. Report on the ‘Human Capacity Development for Treatment, Care and Support of PLWHA's in Nigeria’: 2004-2005. [Google Scholar]
- 10.Scully C, Greenspan JS. Human immunodeficiency virus (HIV) transmission in dentistry. J Dent Res. 2006;85:794–800. doi: 10.1177/154405910608500903. [DOI] [PubMed] [Google Scholar]
- 11.Gooch BF, Cardo DM, Marcus R, McKibben PS, Cleveland JL, Srivastava PU, et al. Percutaneous exposures to HIV-infected blood. Among dental workers enrolled in the CDC Needlestick Study. J Am Dent Assoc. 1995;126:1237–42. doi: 10.14219/jada.archive.1995.0358. [DOI] [PubMed] [Google Scholar]
- 12.McCartan BE, Samaranayake LP. Oral care of HIV infected patients: The knowledge and attitudes of Irish dentists. J Ir Dent Assoc. 1991;37:41–3. [PubMed] [Google Scholar]
- 13.Erasmus S, Luiters S, Brijlal P. Oral Hygiene and dental student's knowledge, attitude and behaviour in managing HIV/AIDS patients. Int J Dent Hyg. 2005;3:213–7. doi: 10.1111/j.1601-5037.2005.00137.x. [DOI] [PubMed] [Google Scholar]
- 14.Jovic-Vranes A, Jankovic S, Vukovic D, Vranes B, Miljus D. Risk perception and attitudes towards HIV in Serbian health care workers. Occup Med (Lond) 2006;56:275–8. doi: 10.1093/occmed/kql019. [DOI] [PubMed] [Google Scholar]
- 15.Mahfouz AA, Alakija W, al-Khozayem AA, al-Erian RA. Knowledge and attitudes towards AIDS among primary health care physicians in the Asir Region, Saudi Arabia. J R Soc Health. 1995;115:23–5. doi: 10.1177/146642409511500108. [DOI] [PubMed] [Google Scholar]
- 16.Comfort AO, Vandana M, Cuttress T, Tuisuva J, Morse Z, Maimanuku L. Attitude/practices of oral healthcare provider to management of HIV/AIDS patients in the Pacific. Pac Health Dialog. 2004;11:26–30. [PubMed] [Google Scholar]
- 17.Flint SR, Croser D, Reznik D, Glick M, Naidoo S, Coogan M. HIV transmission in the dental setting and the HIV-infected oral health care professional: Workshop 1C. Adv Dent Res. 2011;23:106–11. doi: 10.1177/0022034511400075. [DOI] [PubMed] [Google Scholar]


