Abstract
Hepatic encephalopathy (HE) is a neuropsychiatric complication of cirrhosis or acute liver failure. Currently, HE is regarded as a continuous cognitive impairment ranging from the mildest stage, minimal HE to overt HE. Hyperammonaemia and neuroinflammation are two main underlying factors which contribute to the neurological alterations in HE. Both structural and functional impairments are found in the white mater and grey mater involved in HE. Although the investigations into HE pathophysiological mechanism are enormous, the exact pathophysiological causes underlying HE remain controversial. Multimodality magnetic resonance imaging (MRI) plays an important role in helping to understand the pathological process of HE. This paper reviews the up-to-date multimodality MRI methods and predominant findings in HE patients with a highlight of the increasingly important role of blood oxygen level dependent functional MRI.
Keywords: Hepatic encephalopathy, Magnetic resonance imaging, Magnetic resonance spectroscopy, Diffusion weighted imaging, Default-mode network, Blood oxygenation level dependent functional magnetic resonance imaging
Core tip: Multimodality magnetic resonance (MR) imaging is an effective and feasible research tool to uncover the pathophysiological mechanism of hepatic encephalopathy (HE). Among these MR imaging techniques, functional MR imaging method can be the most promising tool for studying HE. Nevertheless, the combination of functional MR imaging and other advanced MR techniques can be helpful to understand HE in the future.
INTRODUCTION
Hepatic encephalopathy (HE) is a neuropsychiatric disorder in patients with cirrhosis or after porto-systemic shunt procedure with pathophysiological and structural alterations. HE manifestations consist of a wide spectrum of neuropsychiatric and cognitive impairments from subclinical disturbance to stupor and coma[1,2]. HE is viewed as a continuous spectrum ranging from minimal HE (MHE) to overt HE (OHE), rather than distinct stages[1]. HE is a reversible condition after successful liver transplantation as the best method to cure advanced liver disease[3,4].
The identification of MHE remains a major challenge for clinicians, mainly due to the intrinsic shortcomings of psychometric tests because these tests are easily affected by the individual’s age, education, and extemporaneous neural status. Critical flicker frequency (CFF) posses the advantages of both language independence and moderate diagnostic accuracy for MHE, thus it is recommended as an adjunct (but not replacement) to psychometric testing[5]. In addition, it is believed that MHE develops before major neuropathological destruction occurs[6]. Hence, reliable and objective imaging biomarkers are necessary to complement these clinical tests to help identify or diagnose MHE and monitor the effects of therapy. Fortunately, these can be provided by various advanced magnetic resonance (MR) imaging tools. Here we review the multimodality MR imaging used in HE diagnosis, clarification of its pathophysiological mechanism, and its follow-up, with focus on new utilities or findings to date.
CLASSIFICATION OF HE
Based on etiology and severity of HE, the Working Party at the 11th World Congresses of Gastroenterology held in Vienna in 1998 recommended the nomenclature and three types of HE[7]. Type A, HE related to acute liver failure; type B, HE related to porto-systemic bypass without intrinsic hepatocellular disease; and type C, HE related to cirrhosis and portal cirrhosis and portal hypertension or porto-systemic shunts. Type C HE can be classified into 3 sub-categories: episodic, chronic, and minimal HE. The properties of episodic HE are confusional syndrome, acute onset, and fluctuant severity. Chronic HE includes relapsing HE (frequent episodes of acute HE) and persistent HE (not reverse despite adequate treatment). MHE is the mildest form of HE. In recent years, the investigation into MHE has been attracting more and more attention.
MHE refers to encephalopathy associated with cirrhosis or porto-systemic shunts or even with extrahepatic portal venous obstruction, and manifests subtly abnormal cognitive and/or neurophysiologic functions without clinically overt symptoms of HE[1]. The prevalence of MHE is estimated to vary from 30% to 84%[6]. The diagnosis of MHE still lacks gold standard, although a battery of psychometric tests have been used to detect neurocognitive impairment. However, neuropsychological tests cannot provide information about the cerebral regions involved. Compared with clinical manifestations of OHE, such as personality change, disorientation, and consciousness disorders, which may contribute to the increased risk of death of cirrhotic patients, MHE impairs executive functioning, working memory and health-related quality of life[8-10]. It has shown that patients with MHE are more likely to get driving problems[11]. In addition, MHE or previous bouts of OHE can be used to predict the subsequent development of OHE as well[9,12].
PATHOGENESIS OF HE
One widely accepted hypothesis for HE is hyperammonemia[13-15]. Hyperammonemia leads to excess uptake of ammonia by astrocytes representing the principal target. Increased ammonia and glutamate are converted to form abundant glutamine under the catalysis of glutamine synthase, which contributes to increased osmotic pressure. Moreover, astrocyte swelling may not happen immediately due to the existence of osmotic-regulatory mechanisms by depletion of intracellular osmolytes until decompensation. As decompensation continues, astrocytes undergo morphologic changes leading to Alzheimer type 2 astrocytosis.
In fact, HE appears to be a much more complicated process that is related to multiple synergistic precipitating factors[16,17]. These factors mainly include hyponatraemia, proinflammatory cytokines, ammonia and benzodiazepines which may induce the insult of astrocyte osmotic balance. Astrocyte swelling and brain edema may be a common pathway in the pathogenesis of HE[14-17]. However, hyperammonaemia and neuroinflammation are two main underlying factors which contribute to the neurological alterations in HE, even without the presence of cerebral edema. In fact, it is now believed that cytotoxic edema does not play an important role in MHE[18]. Changes of multiple neurotransmitter systems can lead to impaired neuronal communication in HE. That process results in various cognitive and motor impairments in HE even before cerebral structural alterations happen[19,20].
APPLICATION AND INTERPRETATION OF MULTIMODALITY MR IMAGING IN HE
Structural MR findings
MR imaging is regarded as the very useful tool for providing a broad range of structural and functional assessments of HE. It aids more understanding of the pathophysiology of HE with the advanced techniques, although other imaging approaches, such as positron emission tomography (PET), also demonstrate direct evidence for the pathogenesis of severe liver disease and MHE[1,2]. In acute HE, characteristic diffuse cortical overt brain edema can be seen on T2-weighted and fluid-attenuated inversion recovery (FLAIR) sequences, while cortical restricted diffusion is presented as high signal intensity on diffusion weighted imaging (DWI) and low signal intensity on apparent diffusion coefficient (ADC) map which indicates cytotoxic edema (Figure 1). However, the involvement of parietal, frontal, temporal, or occipital cortex has been found as an uncommon finding[18,21]. On the other hand, as far as chronic HE is concerned, apart from the well-known high signal intensity on T1-weighted MR imaging in bilateral basal ganglia, high signal intensity along the hemispheric white matter in or around the corticospinal tract on FLAIR T2-weighted images has been reported, which mimics the MR imaging findings of amyotrophic lateral sclerosis, due to mild brain edema beyond the threshold for detection on standard or conventional MR imaging.
Figure 1.
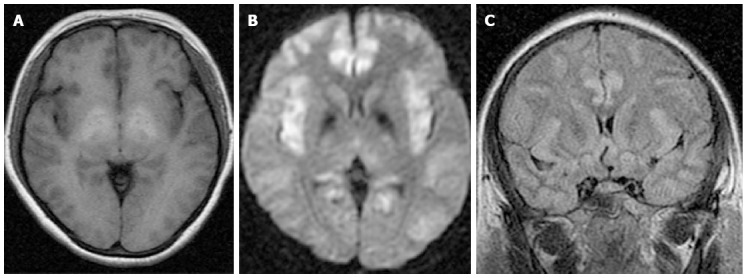
Acute hepatic encephalopathy in a 44-year-old female with hepatitis B virus-related cirrhosis. A: T1 weighted image shows high signal intensity of bilateral globus pallidus; B: T2 Fluid Attenuated Inversion Recovery image shows diffused cortical edema; C: Axial diffusion weighted image shows diffuse cortical high signal intensity corresponding to diffuse cortical edema.
Recently, some advanced MR analysis algorithms have been used to investigate brain structural changes in HE patients. Voxel-based morphometry (VBM) is a useful, unbiased and automatic research tool in accurately detecting the focal and global structural changes in both the grey matter and white matter. This method has been widely used in various central nervous system diseases[22]. Currently, a consensus has been reached as a decreased grey matter volume in cirrhosis patients. In a study by Guevara et al[23], a significant loss in brain density in many areas of the grey matter was found in patients with cirrhosis, which pointed to regional brain atrophy. Apart from the reduction of regional grey matter volume, Zhang et al[24] also found the increased thalamus volume in cirrhotic patients, which was not associated with HE progression, and multiple covariate regression results suggested that Child-Pugh score was a major factor to affect grey matter volume, while porto-systemic shunt mainly affected white matter volume. Recently, Tao et al[25] concluded that increased thalamic volume could be a potentially objective imaging biomarker for predicting seizures due to MHE with the area under the receiver operating characteristic curve of 0.827. Compared with cortical volume, cortical integrity has drawn less attention. Cortical thickness analysis with subvoxel resolution can be used to study cortical integrity in patients with MHE by Montoliu et al[26]. In their study, cortical surface-based analysis techniques were used to investigate patterns of cortical thinning in MHE patients. This technique is a kind of computational neuroanatomy analysis techniques applied to high-resolution cerebral MRI, which is helpful in detecting neocortical mantle. Finally, a focal thinning of the superior temporal cortex and precuneus in MHE patients compared with non-MHE patients and controls was found in this study. In terms of cortical morphological analysis, VBM techniques and cortical thickness analysis reveal signatures of the cortical mantle with different precisions, however, the former carries out a better matching of homologous cortical regions. In addition, white matter abnormalities are common in cirrhotic patients, and VBM is also used in measurement of white matter macroscopic alterations in HE patients. Guevara et al[23] found a loss of white matter density in patients with cirrhosis, thus, they considered that it might represent a loss of axons secondary to the loss of neurons. Zhang et al[24] found increased whiter matter volume, with the extent of affected brain volume greater in HE patients than in non-HE patients with cirrhosis. Moreover, white matter abnormalities would progress during the course of the disease, which was greater in patients with a history of HE, and persisted several months after liver transplantation[23]. Currently, voxel-based diffusion tensor imaging (DTI)[27] or tract-based spatial statistics (TBSS) analysis[6] was combined to further assess the microstructural integrity alteration of the white matter (Figure 2).
Figure 2.
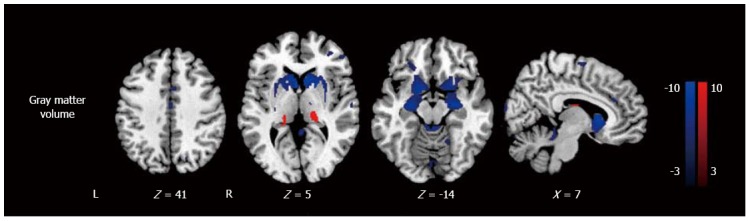
Voxel based morphometry analysis of patients with minimal hepatic encephalopathy and healthy controls. Minimal hepatic encephalopathy patients show grey matter volume losses in the frontal and temporal cortices, caudate, putamen, amygdale, paracentral lobule, anterior and middle cingulate cortices, supplementary motor area, and increased volume in the thalamus. From reference [6] (with permission). L: Left; R: Right.
As iron is a cofactor of enzymes participating in metabolism of some neurotransmitters, iron plays a vital role in brain metabolism. Abnormal deposition of iron in some specific brain regions correlates with the severity of neurocognitive impairments in patients with Alzheimer’s disease and multiple sclerosis by using susceptibility weighted imaging (SWI) or T2*WI MR sequence[28,29]. T2*WI MR imaging can detect subtle iron deposition changes in the brain[29]. Liu et al[30] found that MHE was associated with abnormal iron deposition in the frontal-basal ganglia-thalamocortical circuits by measuring the phase value derived from corrected phase image (CPI). Their research demonstrated that there was significantly decreased phase value in the frontal cortical-basal ganglia circuits of MHE patients, which correlated with neurocognitive impairments by using T2*-weighted gradient echo imaging. This study may point to the potential role of iron in the pathophysiological mechanism of HE. SWI can more sensitively detect iron than T2*WI, however, no study has been reported in HE, to the best of our knowledge.
DWI AND DTI
DWI can be used to quantitatively assess the mobility of water molecules in human body. DWI has been widely employed in the central nervous system since 1990s[31]. The diffusion of water molecules abides by the principles of Brownian motion. Under an unconstrained circumstance, taking cerebrospinal fluid as an example, the movement of water molecules is random and thus equal in all directions (isotropic); while in the context of restricted environments, such as axonal myelin sheaths, water molecules tend to move parallel to, rather than perpendicular to, the white matter tracts[32]. Therefore, the motion is restricted in some directions (anisotropic). DWI can detect this subtle alteration in water molecule movement. On the basis of differently weighted diffusion-weighted images, a measure of diffusion can be calculated; ADC images can be derived from. The ADC represents tissue water diffusivity and is impacted by interactions between water molecules and their surrounding environment.
DTI can be established after the acquisition of diffusion data in a minimum of six non-collinear directions. DTI can provide detailed information on the microstructure within an imaging voxel, including fractional anisotropy and mean diffusivity[33], which can be applied to evaluate white matter integrity in different brain regions. In addition, with the help of advanced fiber tracking algorithms, 3D visualization of neural tracts can be generated to allow a direct view of white matter connectivity. Many researchers have indicated that both cytotoxic edema and interstitial edema coexist varying in degree or proportion according to the onset of HE, that is, cytotoxic edema take a predominant role in acute HE, whereas interstitial edema is more overt in chronic one. Furthermore, DWI and DTI can be used in assessing the effectiveness after manitol infusion therapy and in monitoring HE after transjugular intrahepatic portosystemic shunt (TIPS)[34,35]. Most previous DTI studies applied the region of interest (ROI) based analysis in assessing brain changes of HE, however, for a diffuse disease like HE, whole brain analysis seems to be more ideal. Qi et al[6] employed a novel tool, TBSS based DTI, for investigating the white matter of HE patients, which had a minimum of the registration error and personal evaluation bias.
MR SPECTROSCOPY
The most commonly used isotopes for MR spectroscopy (MRS) study in HE are 1H and 31P. 31P MRS can detect phosphomonoesters, inorganic phosphate, phosphodiesters, phosphocreatine, γNTP, αNTP and βNTP resonances. Although these biomarkers reflect cell membrane synthesis and degradation pathways and energy metabolism information in the brain, little research consensus has been achieved owning to relatively rare 31P MRS studies and more complicate application of MR technique compared with widely used 1H MRS in HE study.
As a well-known noninvasive technique, 1H MRS can be utilized to provide information on brain metabolites such as choline (Cho), creatine (Cr), N-acetyl aspartate (NAA), glutamine and glutamate (Glx), as well as osmolytes such as myoinositol (mIns) and taurine. Currently, there is a consensus on characteristic triad of 1H MRS findings in HE (e.g., intracellular Cho and mIns depletion as well as Glx accumulation), which correlates with neuropsychiatric impairment in HE patients. 1H MRS findings supported the astrocyte swelling hypothesis. In brief, hyperammonia accounts for the significant elevation of astrocyte intracellular glutamine, which triggers organic osmolyte depletion (lower Cho/Cr and mIns/Cr) in patients with cirrhosis, and the increase of glutamate and glutamine signals, to compensate for glial glutamine accumulation (higher Glx/Cr) in order to maintain osmotic homeostasis. However, astrocyte swelling may occur as a consequence of decompensation of this volume-regulatory mechanisms followed by neural-glial disturbance.
Among these 1H-MRS variables, mIns seems to be a more sensitive biomarker in the early detection of HE[36,37]. In a study by Mardini et al[38], they administered an oral amino acid mixture to resemble haemoglobin caused by gastrointestinal bleeding as a challenge to induce hyperammonaemia. Notably, 1H MRS findings exhibited a significant reduction in mIns concentration after the challenge, whereas no statistically significant difference was found in Cho, Glx and NAA. The rapid fall of mIns correlated with a compensatory mechanism to counteract glutamine accumulation. Thus, mIns alteration may be the fastest reaction to a subtle change of astrocyte water content. Cho is a component of phosphocholine and glycerophosphorylcholine, which are related to cell membrane activation. Cho is an important component for the synthesis of acetylcholine, which may be associated with memory, recognition and emotions as an important neurotransmitter. Cho/Cr reduction may underlie the cognition impairment in HE[37].
Most MRS studies found no significant changes of NAA in patients with cirrhosis, which may indicate no significant impairment of neurons during the progression of HE. It was considered previously that neuronal changes in HE was absent or unimportant in explaining the alteration of neuropsychiatric status. However, there is neuropathological evidence for significant neuronal cell loss in the brain of HE patients. For instance, dopaminergic and serotoninergic neuronal systems as well as Purkinje cells are proved to lose in HE in postmortem studies[39]. Some VBM and cortical surface-based analysis studies indirectly support the insult of the grey matter in HE patients[23,26].
Clinically, 1H-MRS has been employed as a useful tool to monitor the metabolite reversibility after successful liver transplantation and effective treatment accompanied by improvement of neurologic manifestations[40]. However, the recovery of various metabolites follows different time courses. One recent study found that there was no change of Glx/Cr, Cho/Cr, mIns/Cr, or NAA/Cr ratios in pre- and post-oral L-ornithine L-aspartate therapy[41].
The current limitations of widely used one-dimensional 1H-MRS in HE had two aspects, namely, spectral overlap of various metabolites resonating within a narrow spectral range, such as glutamine and glutamate, and invisibility of low concentration metabolites. Some novel MRS techniques appear to be able to address above-mentioned issues to some extent. Two-dimensional 1H-MRS finding was consistent with typical findings by one-dimensional 1H-MRS in HE patients with enhanced spectral resolution which can not only distinguish the spectral overlap metabolites, but also detect J-coupled metabolites, such as aspartate, taurine, and gamma-aminobutyric acid[36]. Moreover, the utility of higher magnetic field strength systems (3T or higher) can increase the spectral resolution with a shortened acquisition time.
MR PERFUSION IMAGING
It is well known that cerebral blood flow (CBF) changes in HE patients, and the CBF is redistributed from cortical areas to the basal ganglia structures, causing a heterogeneous distribution of CBF, which is established mainly by PET or single-photon emission computed tomography studies[42]. Decrease of CBF in diffuse cortical areas and the elevation of CBF in bilateral basal ganglia accounted for the accumulation of manganese, which shows high signal intensity on T1 weighted images[42]. Moreover, CBF increase in basal ganglia is correlated with clinical signs of HE[43]. Some MR perfusion imaging techniques can be used to quantitatively detect CBF. Li et al[44] investigated hemodynamic changes in brain basal ganglia in patients with MHE using dynamic susceptibility contrast (DSC)-enhanced MR perfusion imaging in 12 MHE patients and 10 healthy controls. Increased CBF in the basal ganglia and thalamus were found in patients with MHE.
Compared with DSC-MR perfusion imaging, arterial spin-labeling (ASL) MR perfusion imaging appears to be a more rational choice in detecting the CBF changes in HE patients due to the absence of potentially harmful MR contrast agent. In a study by Zheng et al[45], they assessed CBF changes in cirrhotic patients after TIPS by using ASL MRI in which a “bolus” of tagged blood was employed as an endogenous contrast agent. They exhibited that 7 out of 9 patients experienced a global CBF increase, while the remaining 2 had a global CBF decrease by 16% and 31%, respectively, who suffered from multiple episodes of OHE during follow-up. In another study, Zheng et al[46] further studied short- and long-term effects of TIPS on CBF in patients with cirrhosis. In this longitudinal study, the baseline CBF level was established by performing ASL MRI 1-9 d before TIPS, and the follow-up MR examinations were performed about 1 wk, 3 mo, 6-9 mo and 12-18 mo after TIPS. They found that CBF measured at different time points after TIPS insertion showed different patterns, and a sharp decline of relative CBF in the 1 wk to 3 mo period after TIPS insertion indicated that a high event rate of HE might relate with the unadaptable CBF in patients undergoing TIPS insertion. Moreover, Zheng et al[47] investigated the CBF changes in MHE patients, non-HE and healthy controls by using ASL MR perfusion imaging, and found that CBF of the right putamen was of the highest sensitivity (93.8%) and moderate specificity (75.0%) for characterization of MHE when using the cutoff value of 50.57 mL/min per 100 g, which indicated that CBF measured by ASL MRI can be a useful imaging marker for differentiating MHE from non-HE patients.
BLOOD OXYGENATION LEVEL DEPENDENT FUNCTIONAL MRI (BOLD fMRI)
BOLD fMRI is increasingly used in HE studies in recent years. BOLD signal is derived from the intrinsic intravascular susceptibility contrast agent deoxyhemoglobin, and is correlated with the proportion of deoxyhemoglobin/oxyhemoglobin and CBF. BOLD fMRI has supplanted dynamic susceptibility contrast imaging as the most prevalent method of fMRI for most cognitive neuroscience studies since 20 years ago[48]. Nowadays, BOLD fMRI has many utilities in various clinical fields, for instance, presurgical planning, treatment evaluation, clinical assessment, and psychiatric diagnosis[48]. Nevertheless, BOLD fMRI has been playing a vital role in cognitive neuroscience. Herein, we summary the research progress of BOLD fMRI in HE studies in recent years according to task-related fMRI and resting-state fMRI.
Task-related fMRI
As far as we know, only a few studies used task-related fMRI to investigate the neural basis of cognitive dysfunciton in HE patients. Zafiris et al[49] first studied neural mechanism underlying impaired visual judgment in HE patients by using task-related fMRI. They investigated 9 cirrhosis subjects without OHE and 10 healthy controls as well by using fMRI with CFF as the task. Compared to healthy controls, visual judgment-related BOLD activation was decreased in the right inferior parietal cortex (IPL) in cirrhosis patients. Moreover, the subjects exhibited impaired neural interaction between IPL and the parietooccipital cortex, the intraparietal sulcus, the anterior cingulate cortex (ACC), the right prefrontal cortex (PFC), the medial temporal lobe, and the extrastriate cortex V5. In particular, an enhanced coupling between IPL and the postcentral cortex was claimed. This study pointed to the existence of an early impaired and compensatory neural mechanism during visual judgment in cirrhosis patients without OHE. Zhang et al[8] carried out another study on neural mechanism of cognitive control impairment in cirrhosis by using block-designed fMRI paradigm with a modified Stroop task using Chinese characters. A cohort of 14 cirrhosis patient without OHE and 14 healthy controls were recruited in this study. There were two tasks involved in different conflict levels. Subjects were allowed to practice incongruous word-naming task (easier task) before the MRI was performed, while they were blinded to the content of incongruous color-naming task (harder task). They concluded that the impairment of the ACC-PFC-parietal lobe-TFG circuit was the neural mechanism underlying cognitive control impairment in cirrhotic patients. Most recently, Liao et al[50] explored the neural basis of spatial working memory impairment in MHE patients using n-back task related BOLD-fMRI. They found a neural network activation in bilateral PFC, bilateral premotor area, supplementary motor area and bilateral parietal areas, which may explain the neural basis of spatial working memory impairment[50]. McPhail et al[41] performed a block design task-related fMRI aiming at measuring neural activation during treatment (oral L-ornithine L-aspartate) of MHE in a longitudinal study. Their study found that posterior cingulate, ventral medial PFC and visual cortex showed increased function after successful HE treatment.
Resting-state fMRI
Currently, investigators have shifted their attention to brain activities in the resting state in HE patients. Resting-state functional connectivity has revealed a number of networks (resting-state networks) which are consistently found in healthy subjects and represent specific patterns of synchronous activity. These networks persist during task performance and sleep and under sedation. Using both ROI based analysis and independent component analysis (ICA), a number of resting-state networks are found: the default mode network (DMN), the sensorimotor component, the executive control component, up to three visual components, two lateralized fronto-parietal components, the auditory component and the temporo-parietal component[51]. These resting-state networks consist of anatomically separated, but functionally connected regions displaying a high level of correlated BOLD signal activity.
Nowadays the most studied network is the DMN, including the medial PFC, rostral anterior cingulate, posterior cingulate, and precuneus. DMN is known to have high metabolic activity during rest and is relatively de-activated during cognitively demanding tasks, such as visual and auditory attention, language processing, memory, and motoric activity. Zhang et al[52] used the reverse subtraction method to investigate the task-related deactivation to observe the DMN in patients with hepatic cirrhosis. They found that an abnormal deactivation mode may exist in hepatic cirrhosis patients. After this, with the awareness of the potential of uncovering the pathophysiological mechanisms underlying HE by studying DMN, a number of studies have been conducted by Zhang et al[53] and other groups. In a standard resting-state fMRI, that is, the participants are required to rest with their eyes closed and keep their heads still and not to think of anything in particular during MR imaging scans lasting typically a few minutes, Zhang et al[53] employed ICA method to retrieve DMN components in the patients with HE, and found significantly reduced functional connectivity in the right middle frontal gyrus, left precuneus, and left posterior cingulate cortex (PCC) in the patients with HE. Z scores of the left angular gyrus and left PCC were found to have a negative correlation with venous blood ammonia levels in the HE group.
Accumulating resting-state fMRI evidence suggests that an alteration of cortico-striato-thalamic pathway may play an important role in HE. Zhang et al[54] studied the patterns of whole-brain functional connectivity in patients with MHE by defining connectivity of interest (COI) as significantly changed connectivity of every two ROIs compared with controls for further analysis (Figure 3). All 22 COIs related to subcortical ROIs (bilateral putamen, pallidum, and thalamus) were weaker in patients with MHE. Of 29 cortical COIs, 22 connectivities were weaker and 7 were stronger in patients with MHE. In addition, nearly all COIs with significant differences correlated with neuropsychological impairment. In particular, impairment in the basal ganglia-thalamocortical circuit could play an important role in mediating neurocognitive dysfunction, especially for psychomotor speed and attention deficits in patients with MHE. Additionally, some studies used ROI method to investigate the functional connectivity of the above-mentioned circuit in HE patients and further demonstrated the abnormal circuit in HE[55-57]. For example, Qi et al[58] found that MHE patients had disrupted thalamic functional connectivity which indicated reduced integrity of thalamic resting state network in MHE by using an ROI-based method.
Figure 3.
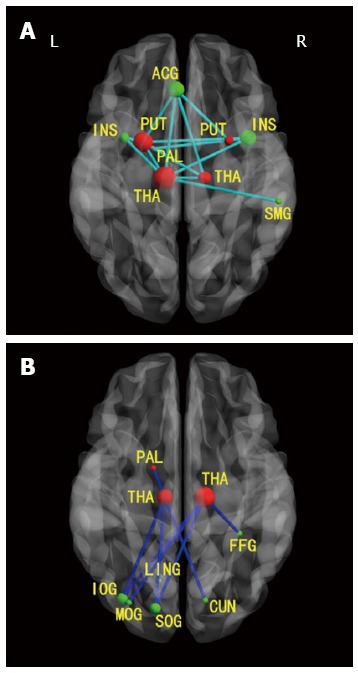
Axial magnetic resonance images show functional connectivities in patients with minimal hepatic encephalopathy between cortical and subcortical regions. A: Decreased positive functional connectivities between cortical and subcortical regions; B: Decreased negative functional connectivities between cortical and subcortical regions. Green nodes: Cortical ROIs; red nodes: Subcortical ROIs; light blue lines: Decreased positive connectivities in patients with minimal HE; dark blue lines: Decreased negative connectivities in patients with minimal HE. R: Right; L: Left; ACG: Anterior cingulum gyrus; SMG: Supramarginal gyrus; PUT: Putamen; PAL: Pallidum; THA: Thalamus; CUN: Cuneus; LING: Lingual gyrus; SOG: Superior occipital gyrus; MOG: Middle occipital gyrus; IOG: Inferior occipital gyrus; FFG: Fusiform gyrus; INS: Insula. From reference [54] (with permission).
Rather than above-mentioned studies on brain network functional connectivity, a “small-world” network model can quantify the effectiveness of information transfer among widely distributed brain regions. The human brain is organized intrinsically as highly modular small-world architectures. In this model, the information transfer is highly efficient, which has been attributed to the brain’s network organization. Hsu et al[59] applied small-world topology to assess the alteration of functional connectivity in HE patients. They found that HE patients showed abnormal small-world properties, which were related to HE grade. The balance between local specialization and global integration of brain functional activity was disrupted in HE patients.
Resting-state fMRI can be used to monitor or predict progression of HE. Qi et al[60] demonstrated that patients with HE had diffuse abnormalities in intrinsic brain activity with amplitude of low frequency fluctuations (ALFF), based on whole-brain functional analysis algorithms (Figure 4). The levels of decreased ALFF in the DMN and increased ALFF in the posterior insular cortex are dependent on the severity of HE, suggesting continuous impairment of the DMN and a compensatory role of the insula during the progression of HE. Chen et al[9] studied resting-state functional connectivity within DMN in patients with MHE and a history of OHE, and found that previous OHE rather than current MHE might be primarily related to brain dysfunction in patients with latent OHE.
Figure 4.
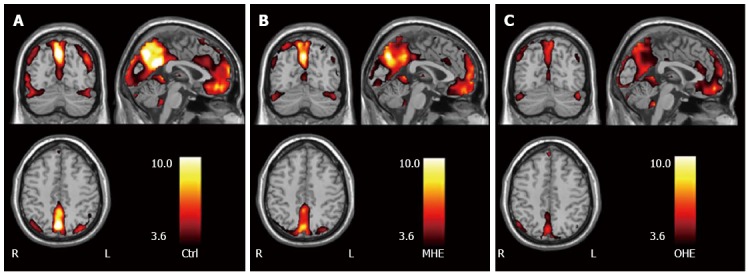
Amplitude of low frequency fluctuation maps in groups of healthy control subjects, patients with minimal hepatic encephalopathy, and patients with overt hepatic encephalopathy. Group of MHE and group of OHE vs control subjects, P < 0.05. Within each group (A: Group of Ctrl; B: Group of MHE; C: Group of OHE), posterior cingulated cortex and precuneus, medial prefrontal cortex, inferior parietal lobe, and occipital areas show high amplitude of low frequency fluctuation values. Color scale indicates t values. From reference [60] (with permission). Ctrl: Control subjects; MHE: Minimal hepatic encephalopathy; OHE: Overt hepatic encephalopathy. L: Left; R: Right.
Resting-state fMRI was also used to investigate dynamic changes of brain function following TIPS and it can predict the development of HE following TIPS. ALFF can be applied as a marker in monitoring dynamic changes of intrinsic brain activity in cirrhotic patients after TIPS[61]. Hence, resting-state fMRI with ALFF analysis may be a noninvasive modality to detect the progression of HE, which was reported by Chen et al[62] in one investigation of low-grade HE.
MULTIMODALITY MRI
fMRI is a promising tool in studying HE, and it can have a flourishing prospect in near future. However, the combination of fMRI and other MR techniques, such as DTI, can provide some new insights into the understanding of pathological mechanism of brain function changes in patients with HE[63-65]. Investigators combined DTI and resting-state fMRI to investigate brain changes in MHE in a single institution study[63] and found that MHE patients have both disturbed structural and functional connectivities within the DMN. The decreased functional connectivity was also detected between some regions without abnormal structural connectivity, suggesting that the former may be more sensitive in detecting the early abnormalities of MHE. This study does not support the idea that cerebral edema play a major role in HE, and, thus, extends our understanding of the pathophysiology of MHE. With the help of fMRI and DTI as well, Lin et al[64] found that reduction of functional connectivity of DMN is heavier in patients with overt HE than in those without HE and MHE. One study by Chen et al[65] also indicated that both functional and structural impairments were evident after apparent recovery from OHE, suggesting that brain dysfunction induced by HE persisted after clinical resolution by combining both VBM and ROI-based fMRI.
The MR imaging findings and potential applications of these advanced MR techniques in brain changes of cirrhotic patients are summarized in Table 1.
Table 1.
Imaging techniques applied in the diagnosis and investigation of hepatic encephalopathy
| MR technique | MR findings or applications |
| Structural MRI | Diffuse cortical overt brain edema on T2WI and fluid attenuated inversion recovery in acute HE; Bilateral basal ganglia high signal intensity on T1WI in chronic HE; Regional gray matter volume reduction, increased thalamus volume and white matter abnormality |
| T2* weighted imaging | Abnormal iron deposition in the frontal-basal ganglia-thalamocortical circuits |
| Diffusion weighted imaging | High signal intensity in subcortical areas and low apparent diffusion coefficient in acute HE; |
| High apparent diffusion coefficient in chronic HE | |
| Diffusion tensor imaging | Increased mean diffusivity and decreased fractional anisotropy in chronic HE |
| 1H MR spectroscopy | Depletion of choline and myoinositol; |
| Accumulation of glutamine/glutamate | |
| Dynamic susceptibility contrast-enhanced MR perfusion imaging1 | Increased cerebral blood flow in the basal ganglia and thalamus |
| Arterial spin-labeling MR perfusion imaging1 | Increased cerebral blood flow; |
| To early diagnose HE or predict overt HE after transjugular intrahepatic porto-systemic shunt | |
| Task-related functional MRI1 | Attention, visual judgment and working memory impairment in HE |
| Resting-state functional MRI1 | Functional connection alteration of cortico-striato-thalamic pathway; |
| Abnormal small-world properties; | |
| Resting state network (especially default mode network) abnormalities: reduced functional connectivity in the right middle frontal gyrus, left precuneus, and left posterior cingulate cortex in the patients with HE |
Techniques mainly for research, currently. MRI: Magnetic resonance imaging; HE: Hepatic encephalopathy.
CONCLUSION
In summary, neuropsychiatric abnormalities of HE are from a combination of multiple synergistic precipitating factors. Multimodality MR imaging is an effective and feasible research tool to uncover the pathophysiological mechanism of HE, and it will play an increasingly important role in the early diagnosis, prognosis and monitoring of HE. In particular, the combination of fMRI and other advanced MR modalities such as DTI should be widely applied in this field to deepen our understanding of the whole story of HE.
Footnotes
Supported by Grants from National Natural Science Foundation of China, Nos. 30700194, 81171313, 81322020 and 81230032 (to Zhang LJ); and Program for New Century Excellent Talents in University, No. NCET-12-0260 (to Zhang LJ)
P- Reviewer: Felipo V, Hashimoto N, Maruyama H, Trifan A S- Editor: Ma YJ L- Editor: Wang TQ E- Editor: Zhang DN
References
- 1.Atluri DK, Prakash R, Mullen KD. Pathogenesis, diagnosis, and treatment of hepatic encephalopathy. J Clin Exp Hepatol. 2011;1:77–86. doi: 10.1016/S0973-6883(11)60126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang LJ, Zhong J, Lu GM. Multimodality MR imaging findings of low-grade brain edema in hepatic encephalopathy. AJNR Am J Neuroradiol. 2013;34:707–715. doi: 10.3174/ajnr.A2968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garcia-Martinez R, Rovira A, Alonso J, Jacas C, Simón-Talero M, Chavarria L, Vargas V, Córdoba J. Hepatic encephalopathy is associated with posttransplant cognitive function and brain volume. Liver Transpl. 2011;17:38–46. doi: 10.1002/lt.22197. [DOI] [PubMed] [Google Scholar]
- 4.Mattarozzi K, Cretella L, Guarino M, Stracciari A. Minimal hepatic encephalopathy: follow-up 10 years after successful liver transplantation. Transplantation. 2012;93:639–643. doi: 10.1097/TP.0b013e318244f734. [DOI] [PubMed] [Google Scholar]
- 5.Torlot FJ, McPhail MJ, Taylor-Robinson SD. Meta-analysis: The diagnostic accuracy of critical flicker frequency in minimal hepatic encephalopathy. Aliment Pharmacol Ther. 2013;37:527–536. doi: 10.1111/apt.12199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qi R, Zhang LJ, Zhong J, Zhu T, Zhang Z, Xu C, Zheng G, Lu GM. Grey and white matter abnormalities in minimal hepatic encephalopathy: a study combining voxel-based morphometry and tract-based spatial statistics. Eur Radiol. 2013;23:3370–3378. doi: 10.1007/s00330-013-2963-2. [DOI] [PubMed] [Google Scholar]
- 7.Mullen KD. Review of the final report of the 1998 Working Party on definition, nomenclature and diagnosis of hepatic encephalopathy. Aliment Pharmacol Ther. 2007;25 Suppl 1:11–16. doi: 10.1111/j.1746-6342.2006.03216.x. [DOI] [PubMed] [Google Scholar]
- 8.Zhang LJ, Yang G, Yin J, Liu Y, Qi J. Neural mechanism of cognitive control impairment in patients with hepatic cirrhosis: a functional magnetic resonance imaging study. Acta Radiol. 2007;48:577–587. doi: 10.1080/02841850701308378. [DOI] [PubMed] [Google Scholar]
- 9.Chen HJ, Jiao Y, Zhu XQ, Zhang HY, Liu JC, Wen S, Teng GJ. Brain dysfunction primarily related to previous overt hepatic encephalopathy compared with minimal hepatic encephalopathy: resting-state functional MR imaging demonstration. Radiology. 2013;266:261–270. doi: 10.1148/radiol.12120026. [DOI] [PubMed] [Google Scholar]
- 10.Ahluwalia V, Wade JB, Thacker L, Kraft KA, Sterling RK, Stravitz RT, Fuchs M, Bouneva I, Puri P, Luketic V, et al. Differential impact of hyponatremia and hepatic encephalopathy on health-related quality of life and brain metabolite abnormalities in cirrhosis. J Hepatol. 2013;59:467–473. doi: 10.1016/j.jhep.2013.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Felipo V, Urios A, Valero P, Sánchez M, Serra MA, Pareja I, Rodríguez F, Gimenez-Garzó C, Sanmartín J, Montoliu C. Serum nitrotyrosine and psychometric tests as indicators of impaired fitness to drive in cirrhotic patients with minimal hepatic encephalopathy. Liver Int. 2013;33:1478–1489. doi: 10.1111/liv.12206. [DOI] [PubMed] [Google Scholar]
- 12.Romero-Gómez M, Boza F, García-Valdecasas MS, García E, Aguilar-Reina J. Subclinical hepatic encephalopathy predicts the development of overt hepatic encephalopathy. Am J Gastroenterol. 2001;96:2718–2723. doi: 10.1111/j.1572-0241.2001.04130.x. [DOI] [PubMed] [Google Scholar]
- 13.Grover VP, Dresner MA, Forton DM, Counsell S, Larkman DJ, Patel N, Thomas HC, Taylor-Robinson SD. Current and future applications of magnetic resonance imaging and spectroscopy of the brain in hepatic encephalopathy. World J Gastroenterol. 2006;12:2969–2978. doi: 10.3748/wjg.v12.i19.2969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Butterworth RF. Hepatic encephalopathy: a central neuroinflammatory disorder? Hepatology. 2011;53:1372–1376. doi: 10.1002/hep.24228. [DOI] [PubMed] [Google Scholar]
- 15.Mardini H, Record C. Pathogenesis of hepatic encephalopathy: lessons from nitrogen challenges in man. Metab Brain Dis. 2013;28:201–207. doi: 10.1007/s11011-012-9362-2. [DOI] [PubMed] [Google Scholar]
- 16.Häussinger D, Schliess F. Pathogenetic mechanisms of hepatic encephalopathy. Gut. 2008;57:1156–1165. doi: 10.1136/gut.2007.122176. [DOI] [PubMed] [Google Scholar]
- 17.Görg B, Schliess F, Häussinger D. Osmotic and oxidative/nitrosative stress in ammonia toxicity and hepatic encephalopathy. Arch Biochem Biophys. 2013;536:158–163. doi: 10.1016/j.abb.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 18.Cauli O, Llansola M, Agustí A, Rodrigo R, Hernández-Rabaza V, Rodrigues TB, López-Larrubia P, Cerdán S, Felipo V. Cerebral oedema is not responsible for motor or cognitive deficits in rats with hepatic encephalopathy. Liver Int. 2013:Epub ahead of prin. doi: 10.1111/liv.12258. [DOI] [PubMed] [Google Scholar]
- 19.Felipo V. Hepatic encephalopathy: effects of liver failure on brain function. Nat Rev Neurosci. 2013;14:851–858. doi: 10.1038/nrn3587. [DOI] [PubMed] [Google Scholar]
- 20.McKinney AM, Lohman BD, Sarikaya B, Uhlmann E, Spanbauer J, Singewald T, Brace JR. Acute hepatic encephalopathy: diffusion-weighted and fluid-attenuated inversion recovery findings, and correlation with plasma ammonia level and clinical outcome. AJNR Am J Neuroradiol. 2010;31:1471–1479. doi: 10.3174/ajnr.A2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.U-King-Im JM, Yu E, Bartlett E, Soobrah R, Kucharczyk W. Acute hyperammonemic encephalopathy in adults: imaging findings. AJNR Am J Neuroradiol. 2011;32:413–418. doi: 10.3174/ajnr.A2290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kakeda S, Korogi Y. The efficacy of a voxel-based morphometry on the analysis of imaging in schizophrenia, temporal lobe epilepsy, and Alzheimer’s disease/mild cognitive impairment: a review. Neuroradiology. 2010;52:711–721. doi: 10.1007/s00234-010-0717-2. [DOI] [PubMed] [Google Scholar]
- 23.Guevara M, Baccaro ME, Gómez-Ansón B, Frisoni G, Testa C, Torre A, Molinuevo JL, Rami L, Pereira G, Sotil EU, et al. Cerebral magnetic resonance imaging reveals marked abnormalities of brain tissue density in patients with cirrhosis without overt hepatic encephalopathy. J Hepatol. 2011;55:564–573. doi: 10.1016/j.jhep.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 24.Zhang LJ, Qi R, Zhong J, Xu Q, Zheng G, Lu GM. The effect of hepatic encephalopathy, hepatic failure, and portosystemic shunt on brain volume of cirrhotic patients: a voxel-based morphometry study. PLoS One. 2012;7:e42824. doi: 10.1371/journal.pone.0042824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tao R, Zhang J, You Z, Wei L, Fan Y, Cui J, Wang J. The thalamus in cirrhotic patients with and without hepatic encephalopathy: a volumetric MRI study. Eur J Radiol. 2013;82:e715–e720. doi: 10.1016/j.ejrad.2013.07.029. [DOI] [PubMed] [Google Scholar]
- 26.Montoliu C, Gonzalez-Escamilla G, Atienza M, Urios A, Gonzalez O, Wassel A, Aliaga R, Giner-Duran R, Serra MA, Rodrigo JM, et al. Focal cortical damage parallels cognitive impairment in minimal hepatic encephalopathy. Neuroimage. 2012;61:1165–1175. doi: 10.1016/j.neuroimage.2012.03.041. [DOI] [PubMed] [Google Scholar]
- 27.Chen HJ, Wang Y, Zhu XQ, Cui Y, Chen YC, Teng GJ. White matter abnormalities correlate with neurocognitive performance in patients with HBV-related cirrhosis. J Neurol Sci. 2012;321:65–72. doi: 10.1016/j.jns.2012.07.056. [DOI] [PubMed] [Google Scholar]
- 28.Wang Y, Butros SR, Shuai X, Dai Y, Chen C, Liu M, Haacke EM, Hu J, Xu H. Different iron-deposition patterns of multiple system atrophy with predominant parkinsonism and idiopathetic Parkinson diseases demonstrated by phase-corrected susceptibility-weighted imaging. AJNR Am J Neuroradiol. 2012;33:266–273. doi: 10.3174/ajnr.A2765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Habib CA, Liu M, Bawany N, Garbern J, Krumbein I, Mentzel HJ, Reichenbach J, Magnano C, Zivadinov R, Haacke EM. Assessing abnormal iron content in the deep gray matter of patients with multiple sclerosis versus healthy controls. AJNR Am J Neuroradiol. 2012;33:252–258. doi: 10.3174/ajnr.A2773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu JY, Ding J, Lin D, He YF, Dai Z, Chen CZ, Cheng WZ, Wang H, Zhou J, Wang X. T2* MRI of minimal hepatic encephalopathy and cognitive correlates in vivo. J Magn Reson Imaging. 2013;37:179–186. doi: 10.1002/jmri.23811. [DOI] [PubMed] [Google Scholar]
- 31.Moseley ME, Kucharczyk J, Mintorovitch J, Cohen Y, Kurhanewicz J, Derugin N, Asgari H, Norman D. Diffusion-weighted MR imaging of acute stroke: correlation with T2-weighted and magnetic susceptibility-enhanced MR imaging in cats. AJNR Am J Neuroradiol. 1990;11:423–429. [PMC free article] [PubMed] [Google Scholar]
- 32.Chenevert TL, Brunberg JA, Pipe JG. Anisotropic diffusion in human white matter: demonstration with MR techniques in vivo. Radiology. 1990;177:401–405. doi: 10.1148/radiology.177.2.2217776. [DOI] [PubMed] [Google Scholar]
- 33.Jones DK. Fundamentals of diffusion MR imaging. In: Gillard J, Waldman A, Barker PB, editors. Clinical MR Neuroimaging. Cambridge: Cambridge University Press; 2005. pp. 54–85. [Google Scholar]
- 34.Saraswat VA, Saksena S, Nath K, Mandal P, Singh J, Thomas MA, Rathore RS, Gupta RK. Evaluation of mannitol effect in patients with acute hepatic failure and acute-on-chronic liver failure using conventional MRI, diffusion tensor imaging and in-vivo proton MR spectroscopy. World J Gastroenterol. 2008;14:4168–4178. doi: 10.3748/wjg.14.4168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Babington JR, Stahl JH, Coy DL. Reversible cytotoxic edema in a cirrhotic patient following TIPS. J Neuroimaging. 2009;19:391–393. doi: 10.1111/j.1552-6569.2009.00369.x. [DOI] [PubMed] [Google Scholar]
- 36.Binesh N, Huda A, Bugbee M, Gupta R, Rasgon N, Kumar A, Green M, Han S, Thomas MA. Adding another spectral dimension to 1H magnetic resonance spectroscopy of hepatic encephalopathy. J Magn Reson Imaging. 2005;21:398–405. doi: 10.1002/jmri.20291. [DOI] [PubMed] [Google Scholar]
- 37.Zhang LJ, Lu GM, Yin JZ, Qi J. Metabolic changes of anterior cingulate cortex in patients with hepatic cirrhosis: A magnetic resonance spectroscopy study. Hepatol Res. 2010;40:777–785. doi: 10.1111/j.1872-034X.2010.00681.x. [DOI] [PubMed] [Google Scholar]
- 38.Mardini H, Smith FE, Record CO, Blamire AM. Magnetic resonance quantification of water and metabolites in the brain of cirrhotics following induced hyperammonaemia. J Hepatol. 2011;54:1154–1160. doi: 10.1016/j.jhep.2010.09.030. [DOI] [PubMed] [Google Scholar]
- 39.Butterworth R. Neuronal cell death in hepatic encephalopathy. Metab Brain Dis. 2007;22:309–320. doi: 10.1007/s11011-007-9072-3. [DOI] [PubMed] [Google Scholar]
- 40.Naegele T, Grodd W, Viebahn R, Seeger U, Klose U, Seitz D, Kaiser S, Mader I, Mayer J, Lauchart W, et al. MR imaging and (1)H spectroscopy of brain metabolites in hepatic encephalopathy: time-course of renormalization after liver transplantation. Radiology. 2000;216:683–691. doi: 10.1148/radiology.216.3.r00se27683. [DOI] [PubMed] [Google Scholar]
- 41.McPhail MJ, Leech R, Grover VP, Fitzpatrick JA, Dhanjal NS, Crossey MM, Pflugrad H, Saxby BK, Wesnes K, Dresner MA, et al. Modulation of neural activation following treatment of hepatic encephalopathy. Neurology. 2013;80:1041–1047. doi: 10.1212/WNL.0b013e31828726e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McPhail MJ, Patel NR, Taylor-Robinson SD. Brain imaging and hepatic encephalopathy. Clin Liver Dis. 2012;16:57–72. doi: 10.1016/j.cld.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 43.Iwasa M, Kaito M, Adachi Y, Watanabe Y, Matsumura K, Takeda K. Cerebral blood flow in basal ganglia is correlated with clinical signs of hepatic encephalopathy in patients with liver cirrhosis. Am J Gastroenterol. 2002;97:763–764. doi: 10.1111/j.1572-0241.2002.05570.x. [DOI] [PubMed] [Google Scholar]
- 44.Li T, Li X, Zhou W, Cui X, Ma L. Dynamic susceptibility contrast-enhanced first-pass perfusion MR imaging in patients with subclinical hepatic encephalopathy. J Neuroradiol. 2012;39:290–294. doi: 10.1016/j.neurad.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 45.Zheng G, Zhang LJ, Wang Z, Qi RF, Shi D, Wang L, Fan X, Lu GM. Changes in cerebral blood flow after transjugular intrahepatic portosystemic shunt can help predict the development of hepatic encephalopathy: an arterial spin labeling MR study. Eur J Radiol. 2012;81:3851–3856. doi: 10.1016/j.ejrad.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 46.Zheng G, Zhang LJ, Cao Y, Pan Z, Qi RF, Ni L, Shi D, Fan X, Lu GM. Transjugular intrahepatic portosystemic shunt induced short- and long-term cerebral blood flow variations in cirrhotic patients: an arterial spin labeling MRI study. Metab Brain Dis. 2013;28:463–471. doi: 10.1007/s11011-013-9400-8. [DOI] [PubMed] [Google Scholar]
- 47.Zheng G, Zhang LJ, Zhong J, Wang Z, Qi R, Shi D, Lu GM. Cerebral blood flow measured by arterial-spin labeling MRI: a useful biomarker for characterization of minimal hepatic encephalopathy in patients with cirrhosis. Eur J Radiol. 2013;82:1981–1988. doi: 10.1016/j.ejrad.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 48.Rosen BR, Savoy RL. fMRI at 20: has it changed the world? Neuroimage. 2012;62:1316–1324. doi: 10.1016/j.neuroimage.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 49.Zafiris O, Kircheis G, Rood HA, Boers F, Häussinger D, Zilles K. Neural mechanism underlying impaired visual judgement in the dysmetabolic brain: an fMRI study. Neuroimage. 2004;22:541–552. doi: 10.1016/j.neuroimage.2004.01.038. [DOI] [PubMed] [Google Scholar]
- 50.Liao LM, Zhou LX, Le HB, Yin JJ, Ma SH. Spatial working memory dysfunction in minimal hepatic encephalopathy: an ethology and BOLD-fMRI study. Brain Res. 2012;1445:62–72. doi: 10.1016/j.brainres.2012.01.036. [DOI] [PubMed] [Google Scholar]
- 51.Rosazza C, Minati L. Resting-state brain networks: literature review and clinical applications. Neurol Sci. 2011;32:773–785. doi: 10.1007/s10072-011-0636-y. [DOI] [PubMed] [Google Scholar]
- 52.Zhang LJ, Yang G, Yin J, Liu Y, Qi J. Abnormal default-mode network activation in cirrhotic patients: a functional magnetic resonance imaging study. Acta Radiol. 2007;48:781–787. doi: 10.1080/02841850701422161. [DOI] [PubMed] [Google Scholar]
- 53.Zhang L, Qi R, Wu S, Zhong J, Zhong Y, Zhang Z, Zhang Z, Lu G. Brain default-mode network abnormalities in hepatic encephalopathy: a resting-state functional MRI study. Hum Brain Mapp. 2012;33:1384–1392. doi: 10.1002/hbm.21295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhang LJ, Zheng G, Zhang L, Zhong J, Wu S, Qi R, Li Q, Wang L, Lu G. Altered brain functional connectivity in patients with cirrhosis and minimal hepatic encephalopathy: a functional MR imaging study. Radiology. 2012;265:528–536. doi: 10.1148/radiol.12120185. [DOI] [PubMed] [Google Scholar]
- 55.Zhu XQ, Chen HJ, Wang Y, Cui Y, Teng GJ. Aberrant resting-state corticostriatal functional connectivity in cirrhotic patients with hyperintense globus pallidus on T1-weighted MR imaging. PLoS One. 2012;7:e48886. doi: 10.1371/journal.pone.0048886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Qi R, Zhang LJ, Zhong J, Zhang Z, Ni L, Jiao Q, Liao W, Zheng G, Lu G. Altered effective connectivity network of the basal ganglia in low-grade hepatic encephalopathy: a resting-state fMRI study with Granger causality analysis. PLoS One. 2013;8:e53677. doi: 10.1371/journal.pone.0053677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhang LJ, Qi R, Zhong J, Ni L, Zheng G, Xu J, Lu GM. Disrupted functional connectivity of the anterior cingulate cortex in cirrhotic patients without overt hepatic encephalopathy: a resting state fMRI study. PLoS One. 2013;8:e53206. doi: 10.1371/journal.pone.0053206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Qi R, Zhang LJ, Zhong J, Zhang Z, Ni L, Zheng G, Lu GM. Disrupted thalamic resting-state functional connectivity in patients with minimal hepatic encephalopathy. Eur J Radiol. 2013;82:850–856. doi: 10.1016/j.ejrad.2012.12.016. [DOI] [PubMed] [Google Scholar]
- 59.Hsu TW, Wu CW, Cheng YF, Chen HL, Lu CH, Cho KH, Lin WC, Lin CP. Impaired small-world network efficiency and dynamic functional distribution in patients with cirrhosis. PLoS One. 2012;7:e35266. doi: 10.1371/journal.pone.0035266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Qi R, Zhang L, Wu S, Zhong J, Zhang Z, Zhong Y, Ni L, Zhang Z, Li K, Jiao Q, et al. Altered resting-state brain activity at functional MR imaging during the progression of hepatic encephalopathy. Radiology. 2012;264:187–195. doi: 10.1148/radiol.12111429. [DOI] [PubMed] [Google Scholar]
- 61.Qi R, Zhang LJ, Zhong J, Wu S, Zhang Z, Zhong Y, Ni L, Zheng G, Jiao Q, Wu X, et al. Dynamic changes of intrinsic brain activity in cirrhotic patients after transjugular intrahepatic portosystemic shunt: a resting-state FMRI study. PLoS One. 2012;7:e46681. doi: 10.1371/journal.pone.0046681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chen HJ, Zhu XQ, Jiao Y, Li PC, Wang Y, Teng GJ. Abnormal baseline brain activity in low-grade hepatic encephalopathy: a resting-state fMRI study. J Neurol Sci. 2012;318:140–145. doi: 10.1016/j.jns.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 63.Qi R, Xu Q, Zhang LJ, Zhong J, Zheng G, Wu S, Zhang Z, Liao W, Zhong Y, Ni L, et al. Structural and functional abnormalities of default mode network in minimal hepatic encephalopathy: a study combining DTI and fMRI. PLoS One. 2012;7:e41376. doi: 10.1371/journal.pone.0041376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lin WC, Hsu TW, Chen CL, Wu CW, Lu CH, Chen HL, Li SH, Yeh PY, Cheng YF, Lin CP. Connectivity of default-mode network is associated with cerebral edema in hepatic encephalopathy. PLoS One. 2012;7:e36986. doi: 10.1371/journal.pone.0036986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chen HJ, Zhu XQ, Shu H, Yang M, Zhang Y, Ding J, Wang Y, Teng GJ. Structural and functional cerebral impairments in cirrhotic patients with a history of overt hepatic encephalopathy. Eur J Radiol. 2012;81:2463–2469. doi: 10.1016/j.ejrad.2011.10.008. [DOI] [PubMed] [Google Scholar]


