Abstract
Acupuncture is used extensively in China for the treatment of stroke and other neurological disorders. The National Institutes of Health recommends acupuncture as an adjunctive therapy for stroke recovery. This study included patients with post-stroke detrusor overactivity who were treated in the Department of Neurology, Fourth Hospital of Harbin Medical University, China. Subjects received either electroacupuncture or sham electroacupuncture at points Baliao [including bilateral Shangliao (BL31), bilateral Ciliao (BL32), bilateral Zhongliao (BL33), and bilateral Xialiao (BL34)] and Huiyang (BL35). Our results showed that electroacupuncture significantly improved cystometric capacity and bladder compliance, decreased detrusor leak point pressure, ameliorated lower urinary tract symptoms, and decreased the risk of upper urinary tract damage. These findings indicate that electroacupuncture at points Baliao and Huiyang is an effective treatment for post-stroke detrusor overactivity.
Keywords: neural regeneration, acupuncture and moxibustion, stroke, urodynamics, detrusor overactivity, rehabilitation, grants-supported paper, neuroregeneration
Research Highlights
(1) This randomized, double-blind, placebo-controlled study evaluated the clinical effectiveness of electroacupuncture for the treatment of post-stroke detrusor overactivity, assessed by voiding diaries and measurements of maximum cystometric capacity, bladder compliance, and detrusor leak point pressure. The effectiveness of patient blinding was assessed to verify the reliability of the results.
(2) The control group received sham electroacupuncture, as recommended by the World Health Organization. This ensured that the control group interventions were similar to the treatment group interventions. We used points Baliao, which are closely associated with the sacral micturition center.
(3) Electroacupuncture significantly improved cystometric capacity and bladder compliance, decreased detrusor leak point pressure, ameliorated lower urinary tract symptoms, and decreased the risk of upper urinary tract damage. Electroacupuncture is an effective treatment for post-stroke detrusor overactivity.
INTRODUCTION
Detrusor overactivity is common after stroke, and is characterized by frequent micturition and urinary incontinence. After stroke, 40–60% of patients experience urinary incontinence in the acute phase, and 20% still experience urinary incontinence after 6 months[1]. Detrusor overactivity adversely affects improvement in other neurological functions, and is the leading cause of upper urinary tract damage. Management of post-stroke detrusor overactivity is therefore animportant aspect of rehabilitation care[2]. However, the optimal treatment for post-stroke urinary incontinence remains unclear. Several treatments are currently used, such as an indwelling urinary catheter or external urine collecting device, oral medication, behavior training, pelvic floor muscle exercises, pelvic floor electrostimulation, biofeedback, intracavity drug perfusion, and electrical nerve stimulation. However, compliance is poor with an indwelling urinary catheter or external collecting device[3,4]. Oral medication and intracavity drug perfusion are associated with various complications[5,6,7,8,9,10,11,12,13,14], and the effectiveness of behavior training[15], pelvic floor muscle exercises[16,17,18], pelvic floor electrostimulation[13,16,17], biofeedback[17], and electrical nerve stimulation[19,20] are unclear. Further investigation is therefore needed in order to establish an effective therapy for detrusor overactivity that has minimal side effects.
Acupuncture is easy to perform, has minimal side effects, and is widely accepted. It has been used in China for over 3 000 years, and is gradually becoming more accepted in other parts of the world[21]. In China, acupuncture is frequently used to treat stroke and other neurological disorders[22,23,24], and is recommended as an adjunctive therapy for stroke recovery by the National Institutes of Health[25,26,27]. Traditional acupuncture has been used to treat urinary incontinence for a long time. Acupuncture at points Huiyang (BL35), Shenshu (BL23), and Sanyinjiao (SP6) can improve post-stroke detrusor overactivity including low bladder compliance-induced urinary urgency, frequent micturition, and urinary incontinence[28].
A voiding diary that records the frequency of urination and urinary incontinence over 24 days can objectively record the severity of lower urinary tract symptoms[29,30,31,32]. Urodynamic testing involves measurement of urine flow and pressure, and performance of electromyography to evaluate urinary tract function[16,33,34,35,36,37]. Urodynamic testing can provide physicians with the information required for diagnosis of disease and evaluation of treatment outcomes.
This randomized, double-blind, placebo-controlled study compared outcomes after electroacupuncture and sham electroacupuncture, to assess the effectiveness of electroacupuncture for the treatment of detrusor overactivity. Detrusor overactivity was assessed by voiding diaries and urodynamic testing. We investigated the effects of electroacupuncture on maximum cystometric capacity, bladder compliance, detrusor leak point pressure, risk of upper urinary tract damage, frequency of urination, and urinary incontinence.
RESULTS
Quantitative analysis of sbjects
Eighty-three patients with post-stroke detrusor overactivity who were treated in the Department of Neurology, Fourth Hospital of Harbin Medical University, China from June 2008 to June 2012 were considered for inclusion. Of these, 17 were excluded because they rejected acupuncture treatment (n = 2), transportation associated with participation in the study was inconvenient (n = 7), they were unwilling to participate (n = 1), their family did not want them to participate (n = 2), or they met the study's exclusion criteria (n = 5). The remaining 66 patients were included in the study. The subjects were randomly assigned to the electroacupuncture group or the sham electroacupuncture group. The selection process is shown in Figure 1.
Figure 1.
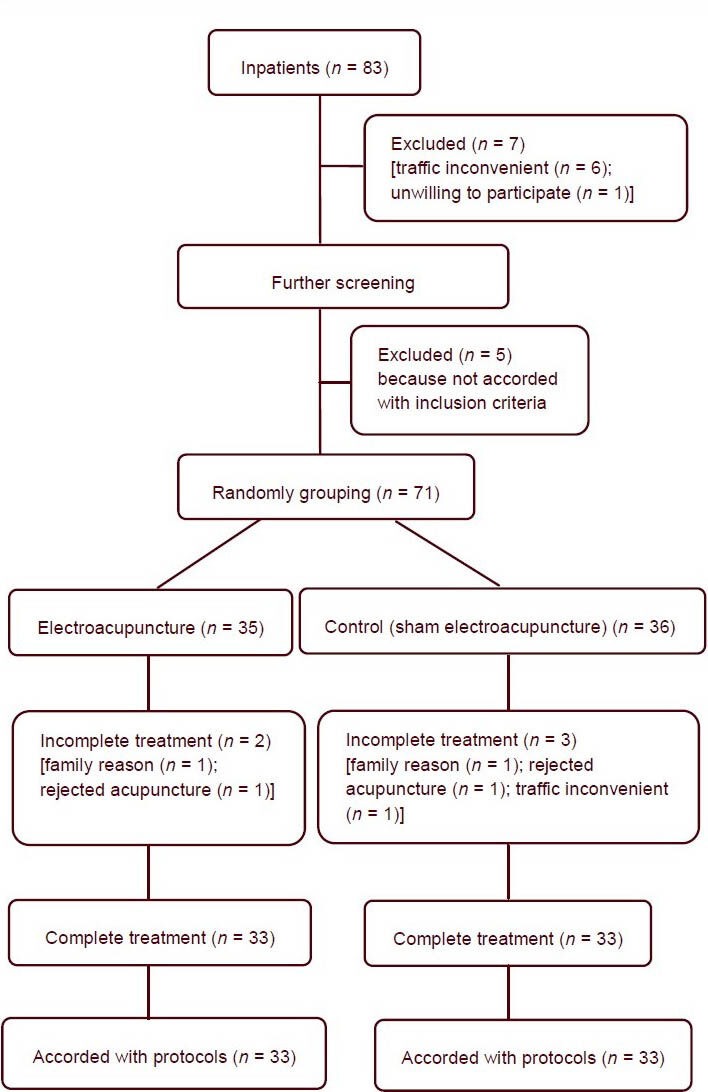
Flowchart showing the subject selection process.
Baseline characteristics of subjects
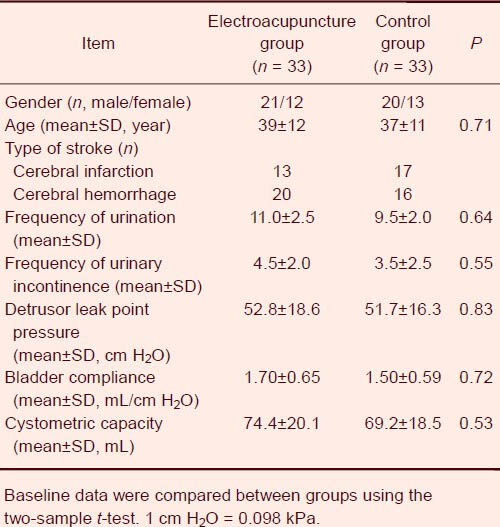
The two groups were comparable in terms of gender, age, and baseline detrusor leak point pressure, maximum cystometric capacity, bladder compliance, frequency of urination, and frequency of urinary incontinence (all P > 0.05). The causes of detrusor overactivity were similar between the two groups: 13 cases of cerebral infarction and 20 cases of cerebral hemorrhage in the electroacupuncture group; and 17 cases of cerebral infarction and 16 cases of cerebral hemorrhage in the control group (Table 1).
Table 1.
Clinical characteristics of patients in the electroacupuncture and control groups
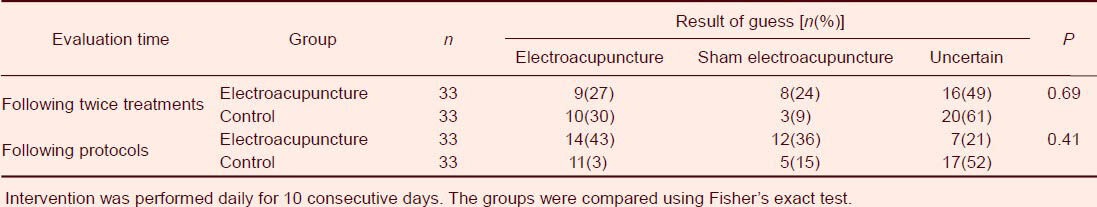
Effectiveness of patient blinding
Concealment of grouping from the patients was successful. After two days of intervention, 53% of subjects in the electroacupuncture group and 62% in the control group indicated that they did not know whether they had received electroacupuncture or sham electroacupuncture, and only 25% of subjects correctly indicated which intervention they had received. The answers to the concealment questionnaire were not significantly different between the two groups (Fisher's exact test, P = 0.69). After the completion of intervention, only 33% of subjects correctly indicated which intervention they had received, and the answers to the concealment questionnaire were not significantly different between the two groups (Fisher's exact test, P = 0.41; Table 2).
Table 2.
Effectiveness of patient blindness
Detrusor overactivity after intervention
Immediately after the completion of intervention, the maximum cystometric capacity and bladder compliance were higher than before intervention, and detrusor leak point pressure was lower than before intervention, in both the electroacupuncture and control groups. The maximum cystometric capacity and bladder compliance were significantly higher in the electroacupuncture group than in the control group (both P < 0.01), and detrusor leak point pressure was significantly lower in the electroacupuncture group than in the control group (P = 0.04).
These parameters were still significantly different between the two groups after at least 5 months (P < 0.01, P < 0.01, and P < 0.05, respectively). The maximum cystometric capacity, bladder compliance, and detrusor leak point pressure were not significantly different between the first post-intervention measurement (immediately after treatment) and the second post-intervention measurement (at 5 months after treatment) (P = 0.82, P = 0.75, and P = 0.69, respectively). We concluded that these parameters were improved immediately after electroacupuncture, and then remained stable for at least 5 months. The frequency of urination and urinary incontinence were significantly lower after electroacupuncture than before treatment (P = 0.03 and P = 0.01, respectively), but these differences were not observed in the control group (P = 0.71 and P = 0.68, respectively). The frequency of urination and urinary incontinence were significantly lower in the electroacupuncture group than in the control group immediately after intervention (P = 0.03 and P = 0.03, respectively), and these differences remained significant after at least 5 months (P = 0.04 and P = 0.01, respectively; Figure 2).
Figure 2.
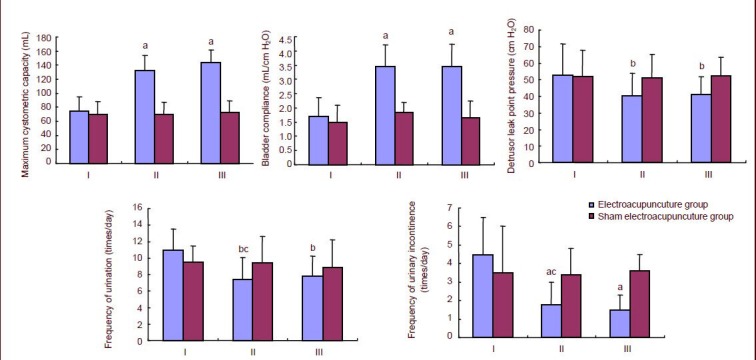
Results of urodynamic testing before and after electroacupuncture and sham electroacupuncture.
Data are expressed as mean ± SD. Intergroup differences were compared using the two-sample t-test for groups with unequal variance, and intragroup differences were compared using the paired t-test. aP< 0.01, bP< 0.05, vs. control group; cP< 0.05, vs. before electroacupuncture. 1 cm H2O = 0.098 kPa.
I: Before electroacupuncture; II: after electroacupuncture; III: 3 months after electroacupuncture.
DISCUSSION
This randomized, double-blind, placebo-controlled clinical trial evaluated the effectiveness of electroacupuncture for the treatment of post-stroke detrusor overactivity.
In patients with normal sensation, the maximum cystometric capacity is the volume at which they feel that urination can no longer be delayed (they feel a strong need to void)[38]. Bladder compliance reflects the relationship between change in bladder volume and change in detrusor pressure[39]. Detrusor leak point pressure is the lowest bladder pressure (in the absence of detrusor contraction) at which leakage occurs via the urethra. A detrusor leak point pressure of > 40 cm H2O is a risk factor for upper urinary tract damage[40]. In the current study, electroacupuncture significantly increased maximum cystometric capacity and bladder compliance, and decreased detrusor leak point pressure, in patients with post-stroke detrusor overactivity. These changes continued for at least 3 months after the completion of intervention. The mean maximum cystometric capacity increased by 59 mL, bladder compliance increased by 1.8 mL/cm H2O, and detrusor leak point pressure decreased by 12.8 cm H2O. The increased maximum cystometric capacity and bladder compliance would be expected to reduce the frequency of urination and urinary incontinence, and thereby improve quality of life. Urine output is usually 50–100 mL/hour in adults. The increased maximum cystometric capacity after electroacupuncture in this study could theoretically prolong the time until the patient needs to urinate by 1 hour. This was confirmed by the results of the study. The frequencies of urination and urinary incontinence were reduced by 3.6 and 2.7 times per day, respectively, in subjects who received electroacupuncture. This improvement was maintained at least 5 months, demonstrating the prolonged effectiveness of electroacupuncture. In a bladder with good compliance, the pressure is usually maintained at 20–40 cm H2O. In a bladder with low compliance because of a neurogenic abnormality, the pressure increases excessively as urine volume increases, which interferes with urine drainage from the upper urinary tract to the bladder, causing upper urinary tract damage. This upper urinary tract damage is a severe complication of post-stroke detrusor overactivity. Bladder compliance and detrusor leak point pressure are important indicators of the risk of upper urinary tract damage[41].
Bladder compliance and detrusor leak point pressure are important indicators of the risk of upper urinary tract damage[41]. Safe bladder capacity is usually associated with detrusor pressure of < 40 cm H2O in the absence of detrusor contraction or increased abdominal pressure, provided there is no vesicoureteral reflux. Safe bladder capacity is lower if reflux occurs at a lower detrusor pressure[42]. The bladder capacity corresponding to detrusor leak point pressure is the cystometric capacity[42]. The difference between the cystometric capacity and safe bladder capacity increases when detrusor leak point pressure is > 40 cm H2O, and long periods of intravesical pressure > 40 cm H2O increase the risk of upper urinary tract damage[43]. Detrusor overactivity or low bladder compliance can significantly increase bladder pressure beyond the safe range during urine storage. The International Continence Society proposed that protection of the upper urinary tract should be the main aim of treatment for neurogenic detrusor overactivity, and that bladder pressure should stay in the safe range during urine storage and urination[38,44,45,46]. In this study, mean bladder compliance increased significantly by 1.8 mL/cm H2O, and mean detrusor leak point pressure decreased by 12.8 cm H2O, after electroacupuncture. These changes were still observed at 5 months after treatment. These results show that electroacupuncture effectively reduces detrusor leak point pressure and increases bladder compliance for at least 5 months. The changes in detrusor leak point pressure, bladder compliance, and maximum cystometric capacity after electroacupuncture effectively reduced the risk of upper urinary tract damage, decreased the frequency of urination and urinary incontinence, and improved quality of life. However, sham electroacupuncture did not have these effects.
Our results are consistent with those of several previous studies that evaluated the effectiveness of acupuncture for the treatment of neurogenic detrusor overactivity. Cheng and colleagues[28] found that patients who received electroacupuncture at points Zhongji (CV3), Guanyuan (CV4), and Ciliao (UB32) significantly shortened the time for neurogenic bladder rehabilitation. Earlier electroacupuncture treatment requires shorter time required for rehabilitation.
Earlier electroacupuncture was associated with earlier achievement of balanced bladder function. In other studies, acupuncture at points Huiyang, Shenshu (BL23), and Sanyinjiao (SP6) significantly improved urinary urgency, frequency, and incontinence resulting from poor detrusor function and low bladder compliance[47,48]. Acupuncture is a minimally invasive technique, and skillful acupuncture can produce a strong placebo effect[49,50,51,52,53,54]. Although these prospective clinical studies demonstrated that traditional Chinese acupuncture was effective for the treatment of some neurogenic bladder problems, they did not include a sham acupuncture control group, which limited the usefulness of the results. To date, there are no universally accepted guidelines for control group intervention in clinical trials of acupuncture. The World Health Organization recommends several methods: (1) no treatment; (2) standard treatment; (3) sham transcutaneous electrical nerve stimulation; (4) sham acupuncture; and (5) acupuncture at other sites. The method selected should have similar psychological effects to true acupuncture, but should result in minimal or no corresponding physiological effects[55]. A variety of sham acupuncture methods have been used, including placebo acupuncture, superficial acupuncture (micro-acupuncture), and acupuncture at sham points[56]. The present study used placebo acupuncture at sham points[57]. In patients who underwent sham acupuncture, the needle was not inserted into the skin, but was attached to a 1 cm diameter ring that was attached to the acupoint with surgical tape to keep it in place. The subjects were told that the fixation device for the needle increased the curative effect. Sham electrical stimulation was then applied. This study used placebo acupuncture as first described by Streitberger and Kleinhenz, which has previously been used in subjects with various conditions including stroke[49,50,51,52,53,58,59,60,61,62] and is regarded to be a suitable control group intervention in clinical trials[63]. In this study, the sham acupuncture used in the control group was suitable, because most of the subjects thought that they were receiving electroacupuncture during the intervention. After the intervention, some patients correctly guessed that they had received sham acupuncture because their urinary symptoms had not improved significantly. Superficial acupuncture, where the needle is inserted superficially into the sham acupoint without causing needle sensation[64], may produce physiological effects because the sham acupoint is close to the true acupoint.
In this study, the subjects all had a history of cerebral infarction or cerebral hemorrhage, but the sites of the lesion were different in the two groups, and the numbers of subjects with lesions at specifics sites were small. Therefore, we did not analyze the relationships between lesion site and the response to intervention. This is a limitation of the study.
This randomized, placebo-controlled clinical trial found that electroacupuncture significantly increased maximum cystometric capacity and bladder compliance, decreased detrusor leak point pressure, improved lower urinary tract symptoms, and decreased the risk of upper urinary tract damage in patients with post-stroke detrusor overactivity. Electroacupuncture is therefore a useful treatment for post-stroke detrusor overactivity. Although the sample size was small, and the selection of the control group was not perfect, the results indicate that further clinical trials with a similar design but larger sample size are warranted.
SUBJECTS AND METHODS
Design
A randomized, double-blind, placebo-controlled clinical trial with a small sample size.
Time and setting
This study was performed at the Department of Neurology and Department of Urinary Surgery, Fourth Hospital of Harbin Medical University, China from June 2008 to June 2012.
Subjects
Patients with post-stroke detrusor overactivity were recruited from the Department of Neurology, Fourth Hospital of Harbin Medical University in China. The subjects and their families were informed of the study objective and procedures at enrolment. After the follow-up testing, they were informed of the intervention they had received by telephone.
The inclusion criteria were: (1) aged 20–50 years, with acute stroke diagnosed by a physician and cerebral hemorrhage or infarction observed on cranial CT or MRI; (2) stable condition, and mobile in a wheelchair or undergoing rehabilitation, for at least 6 months; (3) no indwelling urinary catheter.
The exclusion criteria were: (1) previous acupuncture treatment; (2) pregnant or planning pregnancy; (3) implanted pacemaker; (4) implanted neurostimulator; (5) cardiac arrhythmia; (6) epilepsy; (7) severe heart, brain, lung, or other major organ disease; (8) acid-base or electrolyte imbalance; (9) history of severe kidney disease, hydronephrosis, bladder stoma, sphincterotomy, or severe exaggeration of autonomic nervous system reflexes; (10) urinary tract infection; (11) cognitive disorder; and (12) acupuncture syncope.
Sixty-six patients with a mean age of 39 years (age range 20–50 years, 43 males, and 23 females) were included in the study. The experimental protocols were conducted in accordance with the Administrative Regulations on Medical Institutions, issued by the State Council of China[65].
Methods
Data were collected at three time points: prior to intervention, during intervention, and at follow-up after intervention.
Use of the concealment questionnaire: the concealment of double blinded group was reliable. Fisher exact test was used to analyze the reliability.
Prior to intervention
Subjects were asked to keep a urination diary for at least 3 consecutive days. Urodynamic testing was performed at 1 week and at 1 month after the time of the diary. All participants were interviewed in the Department of Neurology and informed of the study objective and methods, and provided written informed consent. Subjects were randomly assigned to the electroacupuncture group or the control group. To ensure that the proportions of patients with severe urinary frequency and incontinence were similar in both groups, these parameters were taken into consideration during group assignment. The group of each subject was recorded, and the record was placed in an opaque envelope and sent to the investigator. The investigator opened the envelope and informed the acupuncturist of the group assignment. The subjects and evaluators were blinded to the group assignment. The effectiveness of subject blinding was assessed using a questionnaire modified from a previously described method[64] after the second intervention (electroacupuncture or sham electroacupuncture). Subjects were asked to guess which group they were assigned to, with the following possible answers: (1) I am in the electroacupuncture group; (2) I am in the control group; (3) I am not sure. If the subject selected answer 1 or 2, they were asked to indicate the strength of their opinion using a 5-point Likert scale.
Intervention
Subjects underwent 10 interventions (electroacupuncture or sham electroacupuncture) over 2 weeks, administered by professional acupuncturists who had performed clinical acupuncture for more than 20 years.
Electroacupuncture: Considering the differences among patients, individualized acupuncture was administered in combination with traditional Chinese acupuncture methods[66,67,68]. This combined method has frequently been used in previous studies[53,54,69,70,71]. According to modern acupuncture methods, points Baliao [including bilateral Shangliao (BL31), bilateral Ciliao (BL32), bilateral Zhongliao (BL33), and bilateral Xialiao (BL34)] and Huiyang, which are closely associated with the sacral micturition center, were selected (Figure 3A, Table 3). The patient was placed in the lateral or prone position. The entire procedure was performed under sterile conditions. The target skin was sterilized using 75% ethanol, and stainless steel 30-gauge acupuncture needles (Guizhou Andi Medicated Instruments, Guizhou, China) were inserted medially and obliquely into points Baliao and Huiyang. The needles were inserted to a depth of 3.5–4.0 cm at points Baliao, at the first to fourth dorsal sacral foramina, and to a depth of 3.5–5.0 cm at point Huiyang. De qi (a sensation of numbness and distension at the needling site) was achieved by manual stimulation. Electroacupuncture (30–40 Hz, continuous wave) was performed at points Xialiao and Huiyang. Electroacupuncture was then performed at the remaining points using the HM6805-2 Acupoint Pulse Therapy Instrument (20–30 mA; Sichuan Hengming Technology Development, Sichuan, China). The stimulation intensity was adjusted to achieve rhythmic muscle contractions in the anus and perineal region, and be tolerable to the patient (Figure 3B). After the completion of acupuncture, the acupuncturist left and the patient rested on the bed. Electroacupuncture was performed daily for 10 consecutive days, and the needles were inserted for 20 minutes each time. Only one set of interventions was administered.
Figure 3.
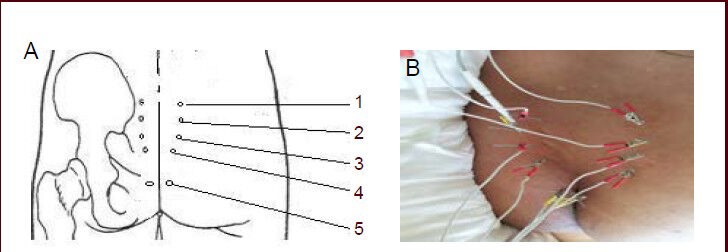
Electroacupuncture at points Baliao and Huiyang.
Points Baliao included bilateral Shangliao (BL31), bilateral Ciliao (BL32), bilateral Zhongliao (BL33), and bilateral Xialiao (BL34).
(A)The 10 points used for the treatment of post-stroke detrusor overactivity.
(B) After needle sensation, the wires were connected for electrical stimulation. 1–5: Points Shangliao, Ciliao, Zhongliao, Xialiao, and Huiyang.
Table 3.
Electroacupuncture points
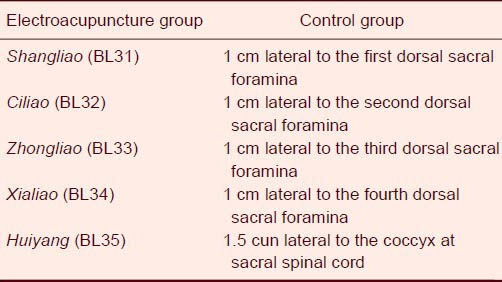
Sham electroacupuncture: The needles were attached to 1 cm diameter rings, which were attached to the subject using surgical tape to keep them in place. The positions of the patient and acupuncturist, procedures, duration of stimulation, and timing of interventions were identical to the procedures in the electroacupuncture group. The needles were attached to positions 1 cm lateral to the acupoints. Sham acupuncture needles did not pierce the skin. The electrical wire used for sham electroacupuncture was broken, so it could not conduct electricity. After the intervention, the acupuncturist left and the patient rested on the bed. The needles were left in position for 20 minutes each time. Sham electroacupuncture was performed daily for 10 consecutive days. The positions of the sham electroacupuncture points are shown in Table 3.
To minimize possible effects on the results if subjects correctly guessed their groups, the subjects were asked not to communicate with each other during treatment, and they were told that the attachment ring and tape were used to increase the accuracy of needling. The procedures were standardized as much as possible in both groups.
A urination diary was kept for 3 consecutive days after the completion of intervention, and urodynamic testing was conducted at 1 week and at 1 month after the completion of intervention.
Follow-up
Subjects were followed up at 3 months after the completion of intervention. They did not undergo further intervention during this 3-month period. Follow-up included a urination diary for 3 consecutive days, and urodynamic testing at 1 week and at 1 month.
Urination diary
The frequency of urination and urinary incontinence were recorded for at least 3 consecutive days.
Urodynamic testing
Urodynamic testing was conducted according to the AUA/SUFU guidelines[37] using a urodynamic testing system (Laborie Medical Technologies, Beijing, China). Any medications that might affect urodynamic or neuromuscular function were discontinued 1 week before testing. During testing, the room was kept warm and quiet. Subjects were informed of the examination goals and procedures, to minimize anxiety. Testing was immediately discontinued if subjects became anxious, or developed a headache or other adverse autonomic nervous system responses. The pressure sensor was connected to the host computer, and the perfusion system was examined to ensure that there was no air in the pressure sensor or the pressure transmission tube. The pressure sensor and perfusion pump were then calibrated. After urination, the patient was placed in a semi-reclining position. After sterilization, a sterile double-lumen cystometry tube was gently inserted into the urethra (one lumen for infusion of normal saline, and one lumen for measuring bladder pressure). An electrode (Laborie Medical Technologies) was attached to the external anal sphincter for electromyography. A 6 F ordinary cystometry tube was inserted 10–15 cm into the rectum. The pressure sensor was placed at the level of the upper margin of the pubic symphysis and set to zero. Each testing tube was thoroughly washed to minimize the effects of drug solutions on the urethra, and air bubbles were removed. The pump was connected, and normal saline at 35°C was infused into the bladder at 20 mL/min. The volume at the first desire to void and bladder compliance were recorded. The detrusor leak point pressure was defined as the minimum detrusor pressure when leakage of urine occurred during bladder filling, in the absence of detrusor contraction or increased abdominal pressure. The examiners and subjects were blinded to the grouping of subjects.
Statistical analysis
Experimental data were expressed as mean ± SD and analyzed using SAS V8 software (SAS Institute Inc., Cary, NC, USA). The baseline characteristics of subjects were compared between groups using the two-sample t-test. Mean maximum cystometric capacity, bladder compliance, detrusor leak point pressure, and frequency of urination and urinary incontinence were compared between groups at the beginning and end of treatment and at the 3-month follow-up using the two-sample t-test for groups with unequal variance. The paired t-test was used for intragroup analysis. A P value of < 0.05 was considered statistically significant.
Footnotes
Yan Liu, Master, Associate chief physician.
Funding: This study was supported by the Postdoctoral Foundation of Heilongjiang Province, No. LRB2008-384.
Conflicts of interest: None declared.
Ethical approval: This study was approved by the Medical Ethics Committee of Fourth Hospital, Harbin Medical University, China.
(Reviewed by Elgin M, Norman C, Xu YD, Zhao JX)
(Edited by Yu J, Su LL, Li CH, Song LP)
REFERENCES
- [1].Pettersen R. Incontinence after stroke. Tidsskr Nor Laegeforen. 2007;127(10):1383–1386. [PubMed] [Google Scholar]
- [2].Jordan LA, Mackey E, Coughlan K, et al. Continence management in acute stroke: a survey of current practices in Australia. J Adv Nurs. 2011;67(1):94–104. doi: 10.1111/j.1365-2648.2010.05480.x. [DOI] [PubMed] [Google Scholar]
- [3].Bright E, Cotterill N, Drake M, et al. Developing a validated urinary diary: phase 1. Neurourol Urodyn. 2012;31(5):625–633. doi: 10.1002/nau.21254. [DOI] [PubMed] [Google Scholar]
- [4].Vella M, Duckett J, Basu M. The predictive value of pre-treatment cystometry in the outcome of women with mixed incontinence treated with duloxetine. Eur J Obstet Gynecol Reprod Biol. 2010;151(2):221–223. doi: 10.1016/j.ejogrb.2010.04.006. [DOI] [PubMed] [Google Scholar]
- [5].Bradley CS, Brown JS, Van Den Eeden SK, et al. Urinary incontinence self-report questions: reproducibility and agreement with bladder diary. Int Urogynecol J. 2011;22(12):1565–1571. doi: 10.1007/s00192-011-1503-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Staskin D, Khullar V, Michel MC, et al. Effects of voluntary dose escalation in a placebo-controlled, flexible-dose trial of fesoterodine in subjects with overactive bladder. Neurourol Urodyn. 2011;30(8):1480–1485. doi: 10.1002/nau.21099. [DOI] [PubMed] [Google Scholar]
- [7].Rocha FT, Bruschini H, Figueiredo JA, et al. Use of an inflatable silicone balloon improves the success rate of bladder autoaugmentation at long-term followup. J Urol. 2011;185(6 Suppl):2576–2581. doi: 10.1016/j.juro.2011.01.029. [DOI] [PubMed] [Google Scholar]
- [8].Herschorn S, Gajewski J, Ethans K, et al. Efficacy of botulinum toxin A injection for neurogenic detrusor overactivity and urinary incontinence: a randomized, double-blind trial. J Urol. 2011;185(6):2229–2235. doi: 10.1016/j.juro.2011.02.004. [DOI] [PubMed] [Google Scholar]
- [9].van Leijsen SA, Hoogstad-van Evert JS, Mol BW, et al. The correlation between clinical and urodynamic diagnosis in classifying the type of urinary incontinence in women. A systematic review of the literature. Neurourol Urodyn. 2011;30(4):495–502. doi: 10.1002/nau.21047. [DOI] [PubMed] [Google Scholar]
- [10].Lie KY, Wong MY, Ng LG. Botulinum toxin a for idiopathic detrusor overactivity. Ann Acad Med Singapore. 2010;39(9):714–715. [PubMed] [Google Scholar]
- [11].Kaya S, Akbayrak T, Beksaç S. Comparison of different treatment protocols in the treatment of idiopathic detrusor overactivity: a randomized controlled trial. Clin Rehabil. 2011;25(4):327–338. doi: 10.1177/0269215510385481. [DOI] [PubMed] [Google Scholar]
- [12].Marencak J, Cossons NH, Darekar A, et al. Investigation of the clinical efficacy and safety of pregabalin alone or combined with tolterodine in female subjects with idiopathic overactive bladder. Neurourol Urodyn. 2011;30(1):75–82. doi: 10.1002/nau.20928. [DOI] [PubMed] [Google Scholar]
- [13].Gaillet S, Bardot P, Bernuz B, et al. Five years follow-up study and failures analysis of Botulinum toxin repeated injections to treat neurogenic detrusor overactivity. Prog Urol. 2012;22(17):1064–1070. doi: 10.1016/j.purol.2012.10.006. [DOI] [PubMed] [Google Scholar]
- [14].Dıraçoğlu D, Vural M, Karan A, et al. Effectiveness of dry needling for the treatment of temporomandibular pain: a double-blind, randomized, placebo controlled study. J Back Musculoskelet Rehabil. 2012;25(4):285–290. doi: 10.3233/BMR-2012-0338. [DOI] [PubMed] [Google Scholar]
- [15].Schreiner L, dos Santos TG, Knorst MR, et al. Randomized trial of transcutaneous tibial nerve stimulation to treat urge urinary incontinence in older women. Int Urogynecol J. 2010;21(9):1065–1070. doi: 10.1007/s00192-010-1165-6. [DOI] [PubMed] [Google Scholar]
- [16].Gousse AE, Kanagarajah P, Ayyathurai R, et al. Repeat intradetrusor injections of onabotulinum toxin a for refractory idiopathic overactive bladder patients: a single-center experience. Female Pelvic Med Reconstr Surg. 2011;17(5):253–257. doi: 10.1097/SPV.0b013e31822f816f. [DOI] [PubMed] [Google Scholar]
- [17].Watanabe M, Yamanishi T, Honda M, et al. Efficacy of extended-release tolterodine for the treatment of neurogenic detrusor overactivity and/or low-compliance bladder. Int J Urol. 2010;17(11):931–936. doi: 10.1111/j.1442-2042.2010.02635.x. [DOI] [PubMed] [Google Scholar]
- [18].Hsiao SM, Chang TC, Wu WY, et al. Comparisons of urodynamic effects, therapeutic efficacy and safety of solifenacin versus tolterodine for female overactive bladder syndrome. J Obstet Gynaecol Res. 2011;37(8):1084–1091. doi: 10.1111/j.1447-0756.2010.01493.x. [DOI] [PubMed] [Google Scholar]
- [19].Lúcio AC, Campos RM, Perissinotto MC, et al. Pelvic floor muscle training in the treatment of lower urinary tract dysfunction in women with multiple sclerosis. Neurourol Urodyn. 2010;29(8):1410–1413. doi: 10.1002/nau.20941. [DOI] [PubMed] [Google Scholar]
- [20].Reynolds WS, Dmochowski RR, Lai J, et al. Patterns and Predictors of Urodynamics Use in the United States. J Urol. 2013;189(5):1791–1796. doi: 10.1016/j.juro.2012.11.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ted Kaptchuk. 2nd ed. Chicago: McGraw-Hill; 2000. The Web That Has No Weaver: Understanding Chinese Medicine. [Google Scholar]
- [22].Xu X. Acupuncture in an outpatient clinic in China: a comparison with the use of acupuncture in North America. South Med J. 2001;94(8):813–816. [PubMed] [Google Scholar]
- [23].Napadow V, Kaptchuk TJ. Patient characteristics for outpatient acupuncture in Beijing, China. J Altern Complement Med. 2004;10(3):565–572. doi: 10.1089/1075553041323849. [DOI] [PubMed] [Google Scholar]
- [24].Hopwood V. Acupuncture in stroke recovery: a literature review. Complementary Therap Med. 1996;4(4):258–263. [Google Scholar]
- [25].Naeser MA. Acupuncture in the treatment of paralysis due to central nervous system damage. J Altern Complement Med. 1996;2(1):211–248. doi: 10.1089/acm.1996.2.211. [DOI] [PubMed] [Google Scholar]
- [26].Park J, Hopwood V, White AR, et al. Effectiveness of acupuncture for stroke: a systematic review. J Neurol. 2001;248(7):558–563. doi: 10.1007/s004150170132. [DOI] [PubMed] [Google Scholar]
- [27].Acupuncture. NIH Consens Statement. 1997;15(5):1–34. [PubMed] [Google Scholar]
- [28].Cheng PT, Wong MK, Chang PL. A therapeutic trial of acupuncture in neurogenic bladder of spinal cord injured patients--a preliminary report. Spinal Cord. 1998;36(7):476–480. doi: 10.1038/sj.sc.3100689. [DOI] [PubMed] [Google Scholar]
- [29].Coyne KS, Margolis MK, Hsieh R, et al. Validation of the urinary sensation scale (USS) Neurourol Urodyn. 2011;30(3):360–365. doi: 10.1002/nau.21005. [DOI] [PubMed] [Google Scholar]
- [30].Vande Walle J, Rittig S, Bauer S, et al. Practical consensus guidelines for the management of enuresis. Eur J Pediatr. 2012;171(6):971–983. doi: 10.1007/s00431-012-1687-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Al-Ghazo MA, Ghalayini IF, Al-Azab R, et al. Urodynamic detrusor overactivity in patients with overactive bladder symptoms. Int Neurourol J. 2011;15(1):48–54. doi: 10.5213/inj.2011.15.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Miller JM, Guo Y, Rodseth SB. Cluster analysis of intake, output, and voiding habits collected from diary data. Nurs Res. 2011;60(2):115–123. doi: 10.1097/NNR.0b013e3182097813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Al-Ghazo MA, Ghalayini IF, Al-Azab R, et al. Urodynamic detrusor overactivity in patients with overactive bladder symptoms. Int Neurourol J. 2011;15(1):48–54. doi: 10.5213/inj.2011.15.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Bright E, Drake MJ, Abrams P. Urinary diaries: evidence for the development and validation of diary content, format, and duration. Neurourol Urodyn. 2011;30(3):348–352. doi: 10.1002/nau.20994. [DOI] [PubMed] [Google Scholar]
- [35].Nager CW, Kraus SR, Kenton K, et al. Urodynamics, the supine empty bladder stress test, and incontinence severity. Neurourol Urodyn. 2010;29(7):1306–1311. doi: 10.1002/nau.20836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Fitz FF, Costa TF, Yamamoto DM, et al. Impact of pelvic floor muscle training on the quality of life in women with urinary incontinence. Rev Assoc Med Bras. 2012;58(2):155–159. [PubMed] [Google Scholar]
- [37].Winters JC, Dmochowski RR, Goldman HB, et al. Urodynamic studies in adults: AUA/SUFU guideline. J Urol. 2012;188(6 Suppl):2464–2472. doi: 10.1016/j.juro.2012.09.081. [DOI] [PubMed] [Google Scholar]
- [38].Stöhrer M, Blok B, Castro-Diaz D, et al. EAU guidelines on neurogenic lower urinary tract dysfunction. Eur Urol. 2009;56(1):81–88. doi: 10.1016/j.eururo.2009.04.028. [DOI] [PubMed] [Google Scholar]
- [39].Consortium for Spinal Cord Medicine. Bladder management for adults with spinal cord injury: a clinical practice guideline for health-care providers. J Spinal Cord Med. 2006;29(5):527–573. [PMC free article] [PubMed] [Google Scholar]
- [40].Ozkan B, Demirkesen O, Durak H, et al. Which factors predict upper urinary tract deterioration in overactive neurogenic bladder dysfunction? Urology. 2005;66(1):99–104. doi: 10.1016/j.urology.2005.02.009. [DOI] [PubMed] [Google Scholar]
- [41].Nosseir M, Hinkel A, Pannek J. Clinical usefulness of urodynamic assessment for maintenance of bladder function in patients with spinal cord injury. Neurourol Urodyn. 2007;26(2):228–233. doi: 10.1002/nau.20319. [DOI] [PubMed] [Google Scholar]
- [42].Woderich R, Fowler CJ. Management of lower urinary tract symptoms in men with progressive neurological disease. Curr Opin Urol. 2006;16(1):30–36. [PubMed] [Google Scholar]
- [43].Walsh PC, Retik AB, Vaughan C, et al. Campbell's Urology. Philadephia: Saunders; 2002. [Google Scholar]
- [44].Samson G, Cardenas DD. Neurogenic bladder in spinal cord injury. Phys Med Rehabil Clin N Am. 2007;18(2):255–274. doi: 10.1016/j.pmr.2007.03.005. vi. [DOI] [PubMed] [Google Scholar]
- [45].Consortium for Spinal Cord Medicine. Bladder management for adults with spinal cord injury: a clinical practice guideline for health-care providers. J Spinal Cord Med. 2006;29(5):527–573. [PMC free article] [PubMed] [Google Scholar]
- [46].Abrams P, Andersson KE, Birder L, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29(1):213–240. doi: 10.1002/nau.20870. [DOI] [PubMed] [Google Scholar]
- [47].Ye YM, Liu ZS, Yang ZY, et al. Analysis of urodynamics in acupuncture treatment of the urinary incontinence after cerebrovascular accident. Zhongguo Zhenjiu. 2000;20(11):645–646. [Google Scholar]
- [48].Liu ZS, Liu BY. Clinical study on electroacupuncture treatment of senile imperative urinary incontinence. Zhongguo Zhenjiu. 2001;21(10):579–578. [Google Scholar]
- [49].Takakura N, Takayama M, Kawase A, et al. Tapping-in Method (Skin Penetration Technique) with a Placebo Needle for Double-Blind Acupuncture Trials. J Altern Complement Med. doi: 10.1089/acm.2012.0056. in press. [DOI] [PubMed] [Google Scholar]
- [50].Rebhorn C, Breimhorst M, Buniatyan D, et al. The efficacy of acupuncture in human pain models: a randomized, controlled, double-blinded study. Pain. 2012;153(9):1852–1862. doi: 10.1016/j.pain.2012.05.026. [DOI] [PubMed] [Google Scholar]
- [51].Ferayorni A, Yniguez R, Bryson M, et al. Needle-free jet injection of lidocaine for local anesthesia during lumbar puncture: a randomized controlled trial. Pediatr Emerg Care. 2012;28(7):687–690. doi: 10.1097/PEC.0b013e31825d210b. [DOI] [PubMed] [Google Scholar]
- [52].Kim HM, Cho SY, Park SU, et al. Can acupuncture affect the circadian rhythm of blood pressure? A randomized, double-blind, controlled trial. J Altern Complement Med. 2012;18(10):918–923. doi: 10.1089/acm.2011.0508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Cheuk DK, Yeung WF, Chung KF, et al. Acupuncture for insomnia. Cochrane Database Syst Rev. 2012;9:CD005472. doi: 10.1002/14651858.CD005472.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].He J, Zheng M, Zhang M, et al. Acupuncture for mumps in children. Cochrane Database Syst Rev. 2012;9:CD008400. doi: 10.1002/14651858.CD008400.pub2. [DOI] [PubMed] [Google Scholar]
- [55].Herr-Wilbert IS, Imhof L, Hund-Georgiadis M, et al. Assessment-guided therapy of urinary incontinence after stroke. Rehabil Nurs. 2010;35(6):248–253. doi: 10.1002/j.2048-7940.2010.tb00055.x. [DOI] [PubMed] [Google Scholar]
- [56].Herr-Wilbert IS, Imhof L, Hund-Georgiadis M, et al. Assessment-guided therapy of urinary incontinence after stroke. Rehabil Nurs. 2010;35(6):248–253. doi: 10.1002/j.2048-7940.2010.tb00055.x. [DOI] [PubMed] [Google Scholar]
- [57].Pettersen R. Incontinence after stroke. Tidsskr Nor Laegeforen. 2007;127(10):1383–1386. [PubMed] [Google Scholar]
- [58].White P, Lewith G, Hopwood V, et al. The placebo needle, is it a valid and convincing placebo for use in acupuncture trials? A randomised, single-blind, cross-over pilot trial. Pain. 2003;106(3):401–409. doi: 10.1016/j.pain.2003.08.013. [DOI] [PubMed] [Google Scholar]
- [59].Fink M, Gutenbrunner C, Rollnik J, et al. Credibility of a newly designed placebo needle for clinical trials in acupuncture research. Forsch Komplementarmed Klass Naturheilkd. 2001;8(6):368–372. doi: 10.1159/000057254. [DOI] [PubMed] [Google Scholar]
- [60].Fink M, Rollnik JD, Bijak M, et al. Needle acupuncture in chronic poststroke leg spasticity. Arch Phys Med Rehabil. 2004;85(4):667–672. doi: 10.1016/j.apmr.2003.06.012. [DOI] [PubMed] [Google Scholar]
- [61].Samson G, Cardenas DD. Neurogenic bladder in spinal cord injury. Phys Med Rehabil Clin N Am. 2007;18(2):255–274. doi: 10.1016/j.pmr.2007.03.005. vi. [DOI] [PubMed] [Google Scholar]
- [62].Tekin L, Akarsu S, Durmuş O, et al. The effect of dry needling in the treatment of myofascial pain syndrome: a randomized double-blinded placebo-controlled trial. Clin Rheumatol. 2013;32(3):309–315. doi: 10.1007/s10067-012-2112-3. [DOI] [PubMed] [Google Scholar]
- [63].Kleinhenz J, Streitberger K, Windeler J, et al. Randomised clinical trial comparing the effects of acupuncture and a newly designed placebo needle in rotator cuff tendinitis. Pain. 1999;83(2):235–241. doi: 10.1016/s0304-3959(99)00107-4. [DOI] [PubMed] [Google Scholar]
- [64].Kalish LA, Buczynski B, Connell P, et al. Stop Hypertension with the Acupuncture Research Program (SHARP): clinical trial design and screening results. Control Clin Trials. 2004;25(1):76–103. doi: 10.1016/j.cct.2003.08.006. [DOI] [PubMed] [Google Scholar]
- [65].Administrative Regulations on Medical Institution; 1994. Sep 01, State Council of the People's Republic of China. [Google Scholar]
- [66].Manber R, Schnyer RN, Lyell D, et al. Acupuncture for depression during pregnancy: a randomized controlled trial. Obstet Gynecol. 2010;115(3):511–520. doi: 10.1097/AOG.0b013e3181cc0816. [DOI] [PubMed] [Google Scholar]
- [67].Giordano J, Garcia MK, Strickland G. Integrating Chinese traditional medicine into a U.S. public health paradigm. J Altern Complement Med. 2004;10(4):706–710. doi: 10.1089/acm.2004.10.706. [DOI] [PubMed] [Google Scholar]
- [68].Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet. 1998;352(9125):364–365. doi: 10.1016/S0140-6736(97)10471-8. [DOI] [PubMed] [Google Scholar]
- [69].Rogha M, Rezvani M, Khodami AR. The effects of acupuncture on the inner ear originated tinnitus. J Res Med Sci. 2011;16(9):1217–1723. [PMC free article] [PubMed] [Google Scholar]
- [70].Amezaga Urruela M, Suarez-Almazor ME. Acupuncture in the treatment of rheumatic diseases. Curr Rheumatol Rep. 2012;14(6):589–597. doi: 10.1007/s11926-012-0295-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Shao JS, Zhang LS, Zhang JH, et al. Introduction of lesson plans on acupoints Anatomy writing by Yan Zhenguo. Shanghai Zhongyiyao Daxue Xuebao. 2010;3:5–8. [Google Scholar]


