Abstract
Shaoyang acupoints are the most frequently used in migraine treatment. However, the central analgesic mechanism remains poorly understood. Studies have demonstrated that single stimulus of the verum acupuncture in healthy subjects can induce significant connectivity or activity changes in pain-related central networks compared with sham acupuncture. However, these findings are not indicative of the central analgesic mechanism of acupuncture at Shaoyang acupoints. Thus, we recruited 100 migraine sufferers and randomly assigned them into five groups: Shaoyang uncommon acupoint, Shaoyang common acupoint, Yangming uncommon acupoint, non-acupoint control, and blank control groups. Subjects were subjected to evaluation of curative effects and functional MRI prior to and after 10 and 20 acupuncture treatments. All subjects were diagnosed by physicians and enrolled following clinical physical examination. Subjects were observed during 1–4 weeks after inclusion. At the fifth week, the first clinical evaluation and resting functional MRI were conducted. The Shaoyang mon acupoint, Shaoyang common acupoint, Yangming uncommon acupoint, and non-acupoint control grousp then were treated with acupuncture, five times per week, 20 times in total over 4 weeks. The second and third clinical evaluations and resting functional MRI screenings were conducted following 10 and 20 acupuncture treatments. The blank control group was observed during the 5 to 8 week period, followed by clinical evaluation and resting functional MRI. The aim of this study was to examine changes in brain functional activity and central networks in subjects with migraine undergoing acu-puncture at Shaoyang uncommon acupoints. This study provides a further explanation of the central analgesic mechanism by which acupuncture at Shaoyang acupoints treats migraine.
Keywords: neural regeneration, acupuncture and moxibustion, migraine, acupuncture, analgesia, central response, functional MRI, sessions of acupuncture, continuous central activity, study design, grants-supported paper, neuroregeneration
Research Highlights
-
(1)
We searched 137 related articles in Science Citation Index database, with only three related to imaging of acupuncture for patients. Furthermore, we did not find any functional MRI studies of pa-tients with migraine.
-
(2)
The searched 137 articles focused on characteristics of central immediate responses to puncture, but no central mechanism regarding the cumulative effects of acupuncture was reported by functional MRI studies.
-
(3)
We will use functional MRI to explore the central analgesic mechanism of the cumulative effects of acupuncture for migraine.
INTRODUCTION
Migraine is a common complaint worldwide that typically manifests as repeated episodes of moderate or severe pulsating hemilateral headache, often accompanied by nausea, phonophobia, or photophobia. National epidemiological investigations have reported a prevalence in adults of 4.2–14.6% in China[1] and approximately 12% in Western countries[2]. Migraine also presents with a sex-related prevalence, with 16–18% of females and 6–8% of males affected[3,4]. Almost 90% of migraine patients experience moderate or severe pain, 75% have to limit their daily activities, and 33% are confined to bed during migraine attacks[5]. As a result, effective therapies are required by both patients and practitioners.
Acupuncture is widely used by Chinese and other Oriental populations for analgesia, and has been gradually accepted as a complementary analgesic therapy in the West. Clinical data suggest that acupuncture can be at least as effective as migraine prophylactic drugs with fewer adverse events, and also relieve acute or chronic migraine symptoms[6,7,8,9,10]. In traditional Chinese acupuncture theory and practice, acupoints on Shaoyang meridians (Sanjiao Meridian and Gallbladder Meridian) are the classical targets for migraine treatment. Thus, acupuncture, especially puncturing Shaoyang acupoints, may become a recommended treatment for migraine sufferers.
Functional MRI has been increasingly applied to detect central mechanisms of acupuncture analgesia. For example, in healthy subjects undergoing experimental induced pain, our previous study indicated that both verum acupuncture (puncturing verum acupoints) and sham acupuncture (puncturing sham acupoints) could modulate amygdala-associated brain networks that regulate pain sensation and modulation; however, verum acupuncture induced a higher level of correlations among this network[11].
Other studies have also demonstrated that verum acupuncture can increase the connectivity of the default mode network with the pain and sensorimotor network and with pain-related brain regions[12], and elicit significant activation in the affective components of the pain matrix[13]. Furthermore, Li et al[9] and Linde et al[14] suggested that acupuncture may delay suffering from migraines. Although signal changes in pain-related brain areas were induced both in verum acupuncture and sham acupuncture, some of the brain regions showed strong functional connectivity during the post-verum acupuncture period[15,16]. This provides an explanation for the efficacy of vernum acupuncture during the post-needling period for migraine treatment.
However, previous functional MRI studies were performed on healthy subjects with pain tasks to observe central responses induced by a single acupuncture stimulus. It remains unclear whether there are different central responses in migraine patients and healthy subjects, and whether there are different brain responses evoked by a single acupuncture stimulus versus repeated acupuncture treatment.
Additionally, acupoints of Shaoyang meridians are the most frequently applied for treating migraine in traditional Chinese style acupuncture. Our previous study supported the superior effect of Shaoyang acupoints, which involved central regulation via brain regions related to the pons-pain matrix, in migraine subjects when compared with stimulating other meridians[17]. Moreover, on Shaoyang meridians, some acupoints are more frequently used in migraine treatment than others. However, it remains unclear whether the analgesic mechanism induced by acupoints of Shaoyang meridians differs from that by acupoints of other meridians, and whether commonly used acupoints of Shaoyang meridians differ from that by uncommonly used Shaoyang meridians.
Thus, the aim of the present study was to determine whether migraine sufferers exhibit: (1) different central analgesic responses induced by sessions of verum acupuncture versus sham acupuncture; (2) different functional brain responses evoked by puncturing acupoints on Shaoyang meridians versus acupoints on other meridians; and (3) different brain responses aroused by puncturing commonly used acupoints versus uncommonly used acupoints on Shaoyang meridians.
SUBJECTS AND METHODS
Design
A clinical study of neuroimaging.
Time and setting
The experiments were conducted from April 2010 to December 2012. Laboratory examinations and acupuncture treatment were performed in the Third Hospital affiliated to Chengdu University of Traditional Chinese Medicine, Chengdu, Sichuan Province, China. Functional MRI scanning was conducted in Huaxi MR Research Center, Chengdu, Sichuan Province, China.
Subjects
This trial has been registered on www.clinicaltrial.gov and its identifier ID is NCT01152632. The trial is still in the status of patient recruitment. We expect to publish the trial design to pursue cooperation with global scholars. This study was performed in compliance with the Administrative Regulations on Medical Institution made by the State Council of China[18].
Participants will be recruited from outpatients of the Third Teaching Hospital and students of Chengdu University of Traditional Chinese Medicine with migraine. After laboratory examinations and definite clinical diagnosis, all potential participants will be informed about the possible risks associated with acupuncture (bleeding, hematoma, and fainting), and will be requested to sign the informed consent forms and told that they may withdraw at any time, without any penalty or loss of benefits for participating. Ultimately, 100 volunteers will be included and randomly allocated into five groups: three verum acupoint groups and two control groups. Verum acupoint groups include Shaoyang common acupoint, Shaoyang uncommon acupoint, and Yangming uncommon acupoint groups. Two control groups involve a non-acupoint group and a blank control group. There will be 20 subjects in each group.
The study will last for 8 weeks. In weeks 1 to 4, participants will be required to fill in headache diaries as baseline. Subjects in the verum acupoint groups will then receive 20 sessions of manual acupuncture treatment, and three functional MRI screenings and efficacy evaluations in weeks 5 to 8. Subjects in the blank control group will only receive three functional MRI scans and efficacy evaluations, but no acupuncture. Acupuncture treatment frequency will be 10 sessions over each 2-week period. The first functional MRI screening and clinical evaluation will be performed prior to the first acupuncture treatment, followed the second and third functional MRI scans and efficacy evaluations at the tenth and twentieth acupuncture treatments, respectively (Figure 1).
Figure 1.
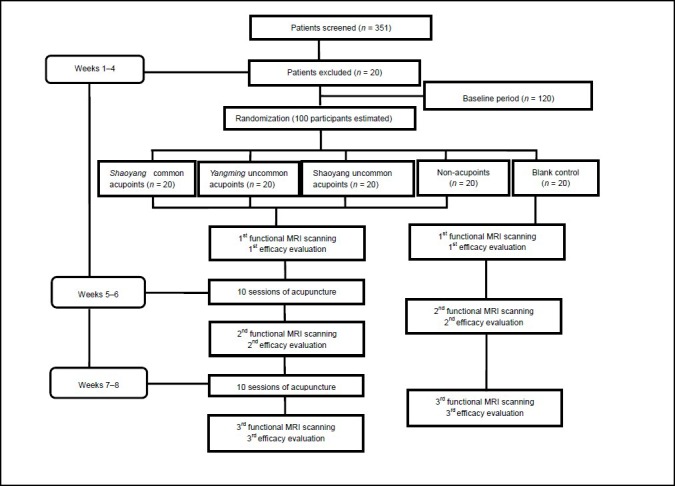
Trial flow.
Inclusion criteria
Subjects will be enrolled if they: (1) are right-handed; (2) are aged between 17 and 45 years; (3) match diagnostic criteria of migraine without aura made by the International Classification of Headache Society in 2004 (lateral headache without organic disorders)[19]; (4) are at least 6 months from the first onset; (5) have had at least one attack during the last month; (6) exhibit moderate or severe headache intensity in Visual Analogue Scale (VAS)[20]; and (7) exhibit low or mild anxiety and depression assessed by Self-rating Anxiety Scale (SAS)[21] and Self-Rating depressive Scale (SDS)[22].
Exclusion criteria
Subjects will be excluded if they: (1) have headache aroused by hypertension, brain trauma, or organic disorders; (2) exhibit serious illness including cancers; (3) have serious dysmenorrhea, pregnancy, lactation, or planned pregnancy; (4) experienced administration of psychotropic substances in the last 3 months and vasoactive drugs in the last 2 weeks; or (5) have contraindications of functional MRI scanning.
Dropout criteria
Subjects will be recognized as dropouts if they are: (1) absent from the first functional MRI screening; or (2) do not receive five treatments before the second functional MRI scan or ten treatments before the third functional MRI scan.
Methods
Interventions
Location of acupoints and non-acupoints and their standard operation procedures are shown in Figure 2 and Table 1. Throughout the trial period, all volunteers will receive non-steroidal anti-inflammatory drugs if necessary (the drug dose and brands will be recorded clearly in headache diaries).
Figure 2.
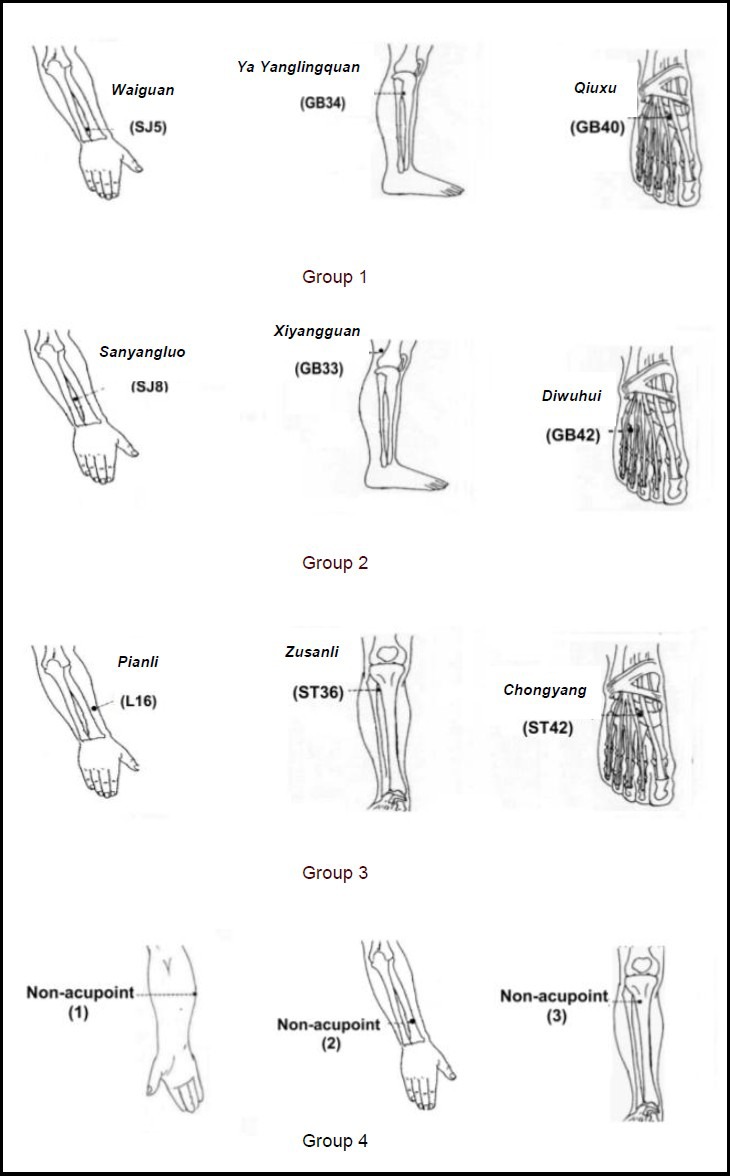
Location of acupoints and non-acupoints.
Group 1: Commonly used acupoints of Shaoyang meridians.
Group 2: Uncommonly used acupoints of Shaoyang meridians.
Group 3: Commonly used acupoints of Yangming meridians.
Group 4: Non-acupoints (1–3).
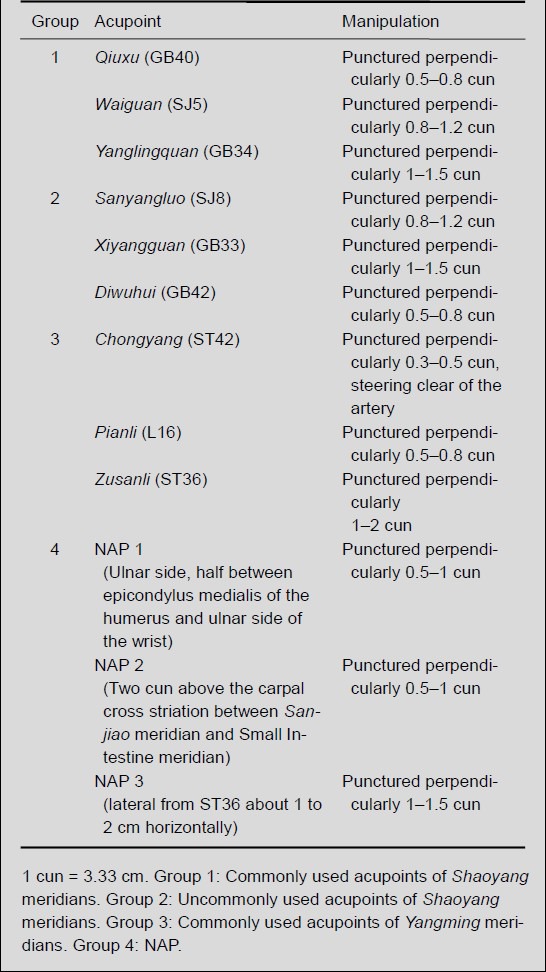
Table 1.
Standard operation procedures of acupoints and non-acupoints (NAP)
Verum acupuncture interventions
Verum acupoints include Yanglingquan (GB34), Qiuxu (GB40), and Waiguan (SJ5) in the Shaoyang common acupoint group; Xiyangguan (GB33), Diwuhui (GB42), and Sanyangluo (SJ8) in the Shaoyang uncommon acupoint group; Zusanli (ST36), Chongyang (ST42), and Pianli (L16) in the Yangming uncommon acupoint group. During weeks 5 to 8, 20 sessions of manual acupuncture treatment, approximately five times per week, will be performed on bilateral acupoints by an acupuncture doctor with 5 years of acupuncture training and 1 year of practical experience. Needles will be sterile, gauge 32, lengths of 25 mm and 40 mm, and single-use (Suzhou Medical Appliance Co., Ltd., Jiangsu, China). The manipulation will be conducted using standard operation procedures, as follows. After needle insertion, lifting, thrusting, and rotating will be continued until “deqi” sensations appear. The needle will be maintained for 30 minutes, during which manipulations will be conducted twice.
Control interventions
The two control interventions will be sham acupuncture and blank control. The manipulation of sham acupuncture will be conducted as described above. In this study, we will select non-acupoints reported in previous studies, including non-acupoint 1, non-acupoint 2, and non-acupoint 3[23,24,25,26,27,28,29]. The blank control group will be used to observe whether migraine patients can exhibit self-healing during experimentation.
Clinical evaluations
Each participant will be required to fill in an 8-week headache diary and a copy of a case report form, from which all efficacy evaluation data will be obtained.
In the headache diaries, headache frequency, headache intensity, each attack duration, and days off work will be recorded. The diaries will also record migraine triggers, headache location and accompanying symptoms, side effects brought on by acupuncture, and analgesic medication intake including brands and doses.
In the case report forms, basic information of each patient will be collected including birth date, body mass, height, career, education degree, the latest menstruation date, and migraine history. Headache days, average pain intensity, anxiety, and depression will be evaluated at the end of weeks 4, 6, and 8. Quality of life will be assessed at the end of weeks 4 and 8.
Primary outcomes
Primary outcomes include headache days and pain intensity at the end of weeks 4, 6, and 8. Headache days will be obtained from headache diaries with a total of 7 days of records. Pain intensity will be assessed by migraine VAS from number 1 to 10, where pain intensity “x=0” represents no pain, pain intensity “x” (1≤ × <4) represents mild pain (little impact on everyday activities), “x” (4≤ × < 7) represents moderate pain (significant impact on everyday activities), and “x” (7≤ × ≤10) represents severe pain (incapacity to perform daily activities). Considering individual bias to mild pain, only patients with moderate and severe headache will be included.
Secondary outcomes
All secondary outcomes will be obtained from records of headache diaries and case report forms, as follows: (1) headache frequency and each attack duration at the end of weeks 4, 6, and 8; (2) days off work because of headache and life quality at the end of weeks 4 and 8; (3) anxiety and depression situation through SAS and SDS at the end of weeks 4, 6, and 8; and (4) side effects due to acupuncture, and analgesic medication intake at the end of weeks 4, 6, and 8.
Functional MRI procedures
Preparation: During 24 hours prior to the scanning, patients will be required to maintain their regular lifestyle and not consume coffee, tea, alcohol, and tobacco. During functional MRI screening, subjects will be instructed to remove metal, cards, cellphones, or any other prohibited materials, and lie quietly on the examination couch wearing eyeshades and earplugs.
Functional MRI scanning: Functional MRI screenings will be performed on a 3.0 T magnetic resonance scanner (Siemens 3.0 T Trio Tim, Munich, Germany), as follows: strengthened three-dimensional anatomic images parameters of repetition time/echo time = 1 900 ms/2.26 ms, slices = 30; matrix size = 128 × 128, field of view = 256 × 256 mm2, slice thickness = 1 mm. The blood oxygenation-level dependent images will be acquired as repetition time/echo time = 2 000 ms/30 ms, flip angle = 90°, slices = 30; matrix size = 128 × 128 mm2, field of view = 240 × 240, slice thickness = 5 mm.
Data analysis
Clinical data analysis: We will test the following null hypothesis with a significance level of P < 0.05. H0: “There is no difference between groups”, H1: “There is a difference between groups”. Data distribution (normal or skewed) will be assessed. For normal distribution data (homogeneity of variances), analysis of variance for repeated measures will be employed for numerical variables and Chi-square test for categorical variables. Skewed distribution data will be transformed to be normal, or a test will be used. Clinical data analysis will be conducted using SPSS 13.0 statistics software (SPSS, Chicago, IL, USA).
Functional MRI image analysis: After data preprocessing conducted on SPM5 software (statistical parametric mapping; Wellcome Department of Cognitive Neurology, London, UK), regional homogeneity and functional connectivity analysis will be performed to detect the modulation of different acupuncture interventions on pain-related functional networks at three time-points (prior to acupuncture, and after the tenth and twentieth acupuncture treatment).
DISCUSSION
This aim of this study is to examine the central mechanism of acupuncture for pain modulation. Although there are numerous neuroimaging studies on acupuncture, only 3 of 137 clinical trials have examined the central responses of acupuncture in patients, none of which applied multiple acupuncture treatment sessions. Hence, the two novel components of our study are: (1) migraine patients will be used as observation subjects rather than healthy subjects, and (2) multiple acupuncture treatment sessions will be used rather the single acupuncture stimulus.
Because of the innovative study design, we have attempted to improve the experimental quality and reduce external interference to functional MRI scanning. First, the verum acupoints will be identified according to their frequency in traditional Chinese acupuncture ancient literature (many without English versions) and clinical Chinese trials. Non-acupoints will be selected by methods stated in previous studies, and include those lateral to acupoints, between two meridians, or between physical landmarks (without clarified acupoints)[20,21,22,23,24,25,26]. Second, “deqi” sensation is considered to be crucial to efficacy in traditional Chinese acupuncture. In the present study, sham acupuncture manipulations are usually required to conduct superficial stimuli with or without “deqi” sensations, resulting in some deficiencies. This method has great similarity with the traditional Chinese acupuncture technique of “shallow needling”, a puncturing method on the skin level recorded in “(Huangdi's) Internal Classic”. The superficial stimuli may excite sensory nerve peripherals below the skin, and eventually induce some acute effects. Therefore, this type of sham acupuncture is not the correct comparison to verum acupuncture. On the other hand, sensations induced by verum acupuncture and superficial sham acupuncture will produce difficulty in blinding patients. In our experiments, each manipulation on both verum acupoints and non-acupoints will require “deqi” sensations of soreness, numbness, heaviness, or fullness. Third, the treatment frequency of acupuncture is considered comparable to drug dose by Chinese acupuncturists. As a result, participants will be required to receive at least 10 treatments over a 4-week duration.
Bias factors will be well controlled throughout our experimental design. An independent practitioner will be responsible for randomization allocation and concealment, and will not be involved in any other parts of this trial. Because of difficulties in blinding the acupuncturists, blinding will be performed in a separate treatment room. The evaluator and statistician will also be blinded to allocation of patients.
Functional MRI image acquisition can be easily affected by external factors. Thus, we will control this in our study, as follows. Acupuncture manipulation prior to scanning will be conducted by the fixed acupuncturists in case any interference comes from manipulations of different practitioners. Furthermore, to reduce the impact of the mental status of the patients, practitioners will be trained to evaluate patient anxiety and depression in advance, and to inform patients of light, noise, and temperature during screening prior to the first scanning.
In summary, in migraine sufferers, this functional MRI trial protocol will be used to examine (1) different brain functional networks induced by a 4-week duration of verum acupuncture versus sham acupuncture; and (2) different functional brain networks evoked by continuous stimuli on acupoints of Shaoyang meridians versus other meridians, and commonly used acupoints versus others on Shaoyang meridians.
Acknowledgments:
We thank Tian J, Sun JB, Yuan K, and Dong MH from Xidian University in Xi’an, Shaanxi Province, China for assistance in data acquisition and analysis. We also thank Gong QY from West China Center of Medical Sciences in China for technical support.
Footnotes
Funding: This experiment was supported by the National Basic Research Program of China (973 Program), No. 2012CB518501, and the Key Project of the National Natural Science Foundation of China, No. 30930112/C190301.
Conflicts of interest: None declared.
Ethical approval: The ethical validity of this study has been assessed and approved by the Ethical Committee of Chengdu University of Traditional Chinese Medicine (No.2010KL-004), China and it complies with the Declaration of Helsinki.
(Reviewed by Dean J, Stow A, Cui J, Jiang GH)
(Edited by Wang J, Su LL, Li CH, Song LP, Liu WJ, Zhao M)
REFERENCES
- [1].Wang SJ, Liu HC, Fuh JL, et al. Prevalence of headaches in a Chinese elderly population in Kinmen: age and gender effect and cross-cultural comparisons. Neurology. 1997;49(1):195–200. doi: 10.1212/wnl.49.1.195. [DOI] [PubMed] [Google Scholar]
- [2].Hagen K, Zwart JA, Vatten L, et al. Prevalence of migraine and non-migrainous headache-head-HUNT, a large population-based study. Cephalalgia. 2000;20(10):900–906. doi: 10.1046/j.1468-2982.2000.00145.x. [DOI] [PubMed] [Google Scholar]
- [3].Diamond S, Bigal ME, Silberstein S, et al. Patterns of diagnosis and acute and preventive treatment for migraine in the United States: results from the american migraine prevalence and prevention study. Headache. 2007;47(3):355–363. doi: 10.1111/j.1526-4610.2006.00631.x. [DOI] [PubMed] [Google Scholar]
- [4].Göbel H, Petersen-Braun M, Soyka D. The epidemiology of headache in Germany: a nationwide survey of a representative sample on the basis of the headache classification of the international headache society. Cephalalgia. 1994;14(2):97–106. doi: 10.1046/j.1468-2982.1994.1402097.x. [DOI] [PubMed] [Google Scholar]
- [5].Ferrari MD. The economic burden of migraine to society. Pharmacoeconomics. 1998;13(6):667–676. doi: 10.2165/00019053-199813060-00003. [DOI] [PubMed] [Google Scholar]
- [6].Linde K, Allais G, Brinkhaus B, et al. Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev. 2009;1:CD001218. doi: 10.1002/14651858.CD001218.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Allais G, De Lorenzo C, Quirico PE, et al. Acupuncture in the prophylactic treatment of migraine without aura: a comparison with flunarizine. Headache. 2002;42(9):855–861. doi: 10.1046/j.1526-4610.2002.02203.x. [DOI] [PubMed] [Google Scholar]
- [8].Sun Y, Gan TJ. Acupuncture for the management of chronic headache: a systematic review. Anesth Analg. 2008;107(6):2038–2047. doi: 10.1213/ane.0b013e318187c76a. [DOI] [PubMed] [Google Scholar]
- [9].Li Y, Liang F, Yang X, et al. Acupuncture for treating acute attacks of migraine: a randomized controlled trial. Headache. 2009;49(6):805–816. doi: 10.1111/j.1526-4610.2009.01424.x. [DOI] [PubMed] [Google Scholar]
- [10].Vickers AJ, Rees RW, Zollman CE, et al. Acupuncture for chronic headache in primary care: large, pragmatic, randomized trial. BMJ. 2004;328(7442):744. doi: 10.1136/bmj.38029.421863.EB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Qin W, Tian J, Bai L, et al. FMRI connectivity analysis of acupuncture effects on an amygdala-associated brain network. Mol Pain. 2008;4:55. doi: 10.1186/1744-8069-4-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Dhond RP, Yeh C, Park K, et al. Acupuncture modulates resting state connectivity in default and sensorimotor brain networks. Pain. 2008;136(3):407–418. doi: 10.1016/j.pain.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Chae Y, Lee H, Kim H, et al. The neural substrates of verum acupuncture compared to non-penetrating placebo needle: an fMRI study. Neurosci Lett. 2009;450(2):80–84. doi: 10.1016/j.neulet.2008.11.048. [DOI] [PubMed] [Google Scholar]
- [14].Linde K, Streng A, Jürgens S, et al. Acupuncture for patients with migraine: a randomized controlled trial. JAMA. 2005;293(17):2118–2125. doi: 10.1001/jama.293.17.2118. [DOI] [PubMed] [Google Scholar]
- [15].Liu J, Qin W, Guo Q, et al. Divergent neural processes specific to the acute and sustained phases of verum and sham acupuncture. J Magn Reson Imaging. 2011;33(1):33–40. doi: 10.1002/jmri.22393. [DOI] [PubMed] [Google Scholar]
- [16].Liu J, Qin W, Guo Q, et al. Distinct brain networks for time-varied characteristics of acupuncture. Neurosci Lett. 2010;468(3):353–358. doi: 10.1016/j.neulet.2009.11.031. [DOI] [PubMed] [Google Scholar]
- [17].Li XZ, Liu XG, Song WZ, et al. Effect of acupuncture at acupoints of the Shaoyang Meridian on cerebral glucose metabolism in the patient of chronic migraine. Zhongguo Zhen Jiu. 2008;28(11):854–859. [PubMed] [Google Scholar]
- [18].Administrative Regulations on Medical Institution; 1994. Sep 01, State Council of the People's Republic of China. [Google Scholar]
- [19].International Headache Society. International classification of headache disorders, ICHD-2. Cephalalgia. 2004;17(suppl 19):24–34. [Google Scholar]
- [20].Edgar EE, Adler R. Methodological problems in the mea-surement of pain: a comparison between the verbal rating scale and the visual analogue scale. Pain. 1975;1(4):379–384. doi: 10.1016/0304-3959(75)90075-5. [DOI] [PubMed] [Google Scholar]
- [21].Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- [22].Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- [23].Brinkhaus B, Hummelsberger J, Kohnen R, et al. Acupuncture and Chinese herbal medicine in the treatment of patients with seasonal allergic rhinitis: a randomized-controlled clinical trial. Allergy. 2004;59(9):953–960. doi: 10.1111/j.1398-9995.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- [24].Biernacki W, Peake MD. Acupuncture in treatment of stable asthma. Respir Med. 1998;92(9):1143–1145. doi: 10.1016/s0954-6111(98)90409-7. [DOI] [PubMed] [Google Scholar]
- [25].Fireman Z, Segal A, Kopelman Y, et al. Acupuncture treatment for irritable bowel syndrome: a double-blind controlled study. Digestion. 2001;64(2):100–103. doi: 10.1159/000048847. [DOI] [PubMed] [Google Scholar]
- [26].Fink M, Wolkenstein E, Karst M, Gehrke A. Acupuncture in chronic epicondylitis: a randomized controlled trial. Rheumatology (Oxford) 2002;41(2):205–209. doi: 10.1093/rheumatology/41.2.205. [DOI] [PubMed] [Google Scholar]
- [27].Smith C, Crowther C, Beilby J. Acupuncture to treat nausea and vomiting in early pregnancy: a randomized controlled trial. Birth. 2002;29(1):1–9. doi: 10.1046/j.1523-536x.2002.00149.x. [DOI] [PubMed] [Google Scholar]
- [28].Shapira MY, Berkman N, Ben-David G, et al. Short-term acupuncture therapy is of no benefit in patients with moderate persistent asthma. Chest. 2002;121(5):1396–1400. doi: 10.1378/chest.121.5.1396. [DOI] [PubMed] [Google Scholar]
- [29].Chang CH, Huang JL, Ting CT, et al. Atropine-Induced HRV alteration is not amended by electroacupuncture on Zusanli. Am J Chin Med. 2005;33(2):307–314. doi: 10.1142/S0192415X05002928. [DOI] [PubMed] [Google Scholar]


