Abstract
Most studies addressing the specificity of meridians and acupuncture points have focused mainly on the different neural effects of acupuncture at different points in healthy individuals. This study examined the effects of acupuncture on brain function in a pathological context. Sixteen patients with ischemic stroke were randomly assigned to true point group (true acupuncture at right Waiguan (SJ5)) and sham point group (sham acupuncture). Results of functional magnetic resonance imaging revealed activation in right parietal lobe (Brodmann areas 7 and 19), the right temporal lobe (Brodmann area 39), the right limbic lobe (Brodmann area 23) and bilateral occipital lobes (Brodmann area 18). Furthermore, inhibition of bilateral frontal lobes (Brodmann area 4, 6, and 45), right parietal lobe (Brodmann areas 1 and 5) and left temporal lobe (Brodmann area 21) were observed in the true point group. Activation in the precuneus of right parietal lobe (Brodmann area 7) and inhibition of the left superior frontal gyrus (Brodmann area 10) was observed in the sham group. Compared with sham acupuncture, acupuncture at Waiguan in stroke patients inhibited Brodmann area 5 on the healthy side. Results indicated that the altered specificity of sensation-associated cortex (Brodmann area 5) is possibly associated with a central mechanism of acupuncture at Waiguan for stroke patients.
Keywords: nerve regeneration, acupuncture, Waiguan (SJ5), brain injury, ischemic stroke, functional magnetic resonance imaging, Brodmann area, sham point, 973 Program, neural regeneration
Introduction
Considering that acupoints are the basis of acupuncture and moxibustion, to study the mechanisms of acupuncture and moxibustion, we should first investigate the effects at a single acupoint. Early studies concerning the specificity of meridians and acupuncture points have mainly focused on tissue structure, biophysics, pathological reaction, function, and clinical curative effects[1,2,3,4,5]. The proposal of a meridians- and acupuncture-points brain-related theory has provided a new direction for the study of the specificity of meridians and acupuncture points[6]. Simultaneously, modern imaging techniques such as functional magnetic resonance imaging (fMRI) is developing rapidly and provides an effective means to study these issues.
Previous studies have suggested that acupuncture at meridians and acupuncture points can induce both activation and inhibition in functional brain areas[7,8,9,10,11]. Acupuncture at Neiguan (PC6) has been confirmed to activate bilateral temporal and frontal lobes of healthy elderly people[9]. Another study verified that the amplitude of low frequency fluctuations was significantly higher in the cerebral cortex (frontal lobe, temporal lobe, parietal lobe, and occipital lobe), brainstem, and cerebellum of normal people after acupuncture at Zusanli (ST36) in a resting state. Chen et al.[11] performed fMRI and found that acupuncture at Daling (PC7) activated Brodmann area (BA) 6, BA22, and BA46 in the frontal and temporal lobes of healthy people.
However, the relationship between meridians and acupuncture points and the brain under pathological conditions remains unknown. Yeo et al.[12] verified activation in substantia nigra and caudate nucleus of patients with Parkinson's disease after acupuncture at Yanglingquan (GB34). Using functional imaging, Yi et al.[13] confirmed that after acupuncture at Taichong (LR3), fractional amplitude of low frequency fluctuations was noticeably less in the left frontal lobe (BA10) of patients suffering from depression. Fractional amplitude of low frequency fluctuations was positively correlated with Hamilton Depression Rating Scale scores, showing a potential association between acupuncture at Taichong and depression.
Although numerous studies concerning the correlation of meridians/acupuncture points and brain activity have been conducted, powerful evidence and a complete theoretical system remain lacking. For example, stroke is a very common affliction in the clinic, and while the clinical therapeutic effects of acupuncture for stroke victims have been confirmed[14,15,16,17], current knowledge still cannot fully explain the underlying mechanism. A previous study has confirmed that the mechanism might be associated with specific activation/inhibition of brain areas by acupuncture at meridians and acupuncture points[18]. Because acupuncture at Waiguan (SJ5) has been shown to effectively improve sequelae of stroke such as hemiplegia and sensory disturbance, it is commonly selected as a target point for research[7,19]. However, few studies have compared changes in brain activity after acupuncture at Waiguan and sham points.
Therefore, this study focused on the effects of acupuncture on brain function in ischemic stroke patients, and compared the effects between Waiguan and sham points. fMRI revealed morphological changes in stroke patients and cerebral blood flow. This study investigated how acupuncture at Waiguan affects specific brain areas of patients in a pathological state, and explored possible therapeutic mechanisms.
Results
Quantitative analysis of subjects and baseline comparison
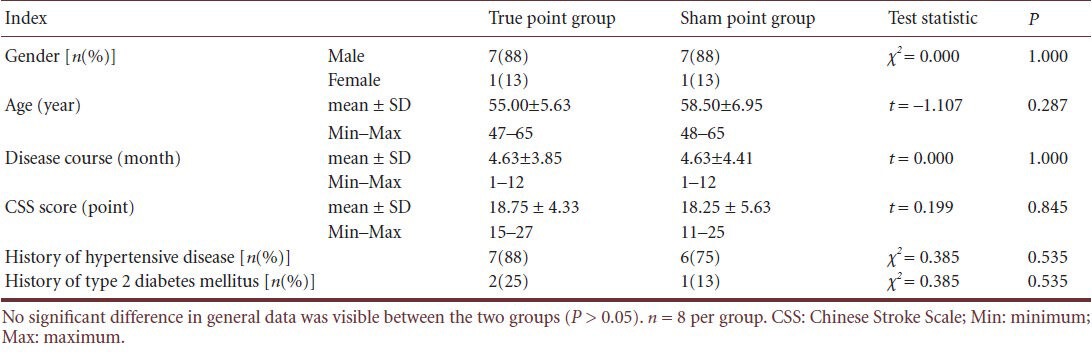
Sixteen ischemic stroke patients were randomly assigned to either a true point group (true acupuncture at right Waiguan) or a sham point group (sham acupuncture). All patients were included in the final analysis. No significant difference in general data was visible between the two groups (P > 0.05; Table 1).
Table 1.
Comparison of demographic data of patients across groups
Effects of acupuncture at Waiguan on brain areas of patients with ischemic stroke
As exhibited in Tables 2 and 3, as well as Figures 1 and 2, activations in the right precuneus (BA7 and BA19), right middle and superior temporal gyri (BA39), right posterior cingulate cortex (BA23), and bilateral cuneus of the occipital lobe (BA18) were visible after acupuncture at right Waiguan of ischemic stroke patients. Simultaneously, inhibition of the right inferior frontal gyrus (BA45), right precentral gyrus (BA1, BA4 and BA6), postcentral gyrus (BA5), left paracentral lobule (BA6), and left middle temporal gyrus (BA21) was also detected.
Table 2.
Brain regions that increased activity during acupuncture at Waiguan (SJ5)
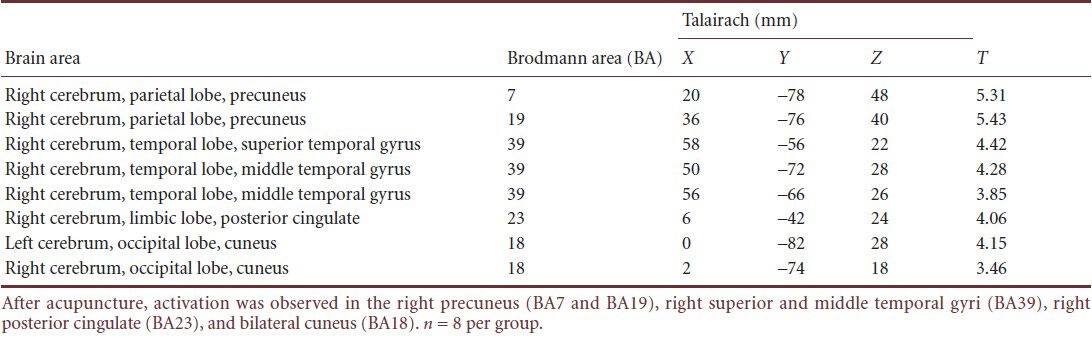
Table 3.
Brain regions that decreased activity during acupuncture at Waiguan (SJ5)
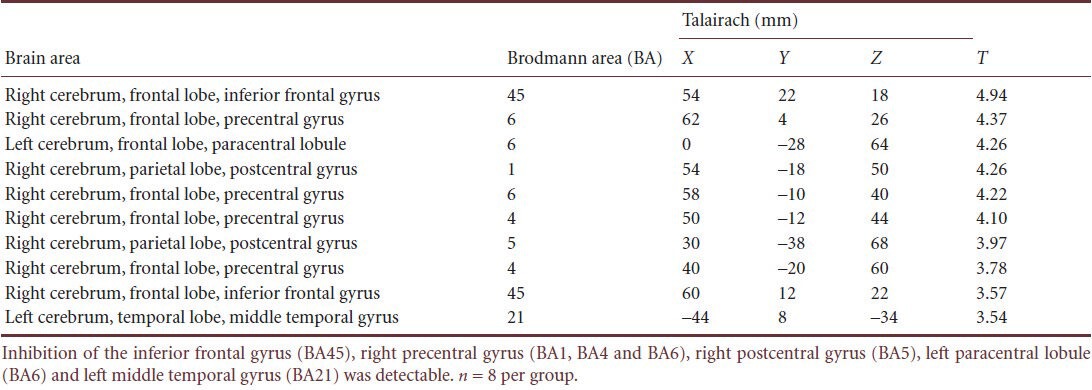
Figure 1.
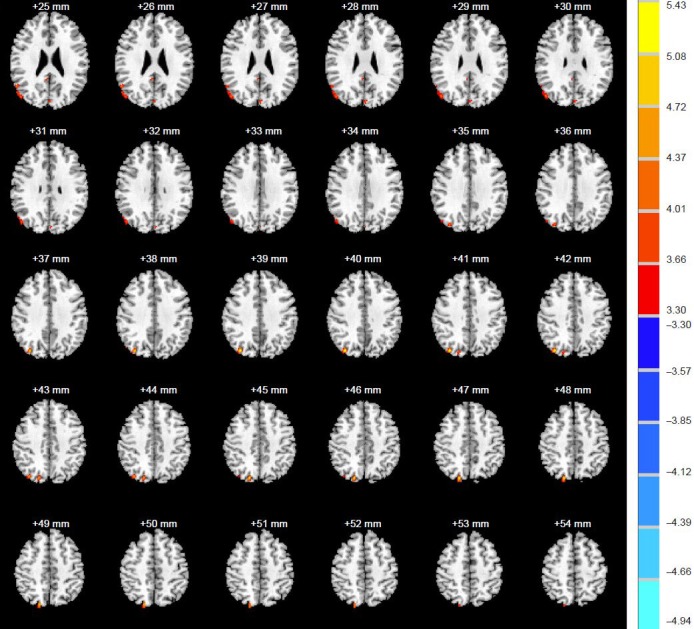
Excitatory effects of acupuncture at Waiguan (SJ5) on brain activity of stroke patients.
During acupuncture, activation was observed in the right precuneus, superior and middle temporal gyri, posterior cingulate, and bilateral cuneus. Blue represents inhibition. Red represents activation. Color bar on the right side: darker color indicates lower absolute T-values.
Figure 2.
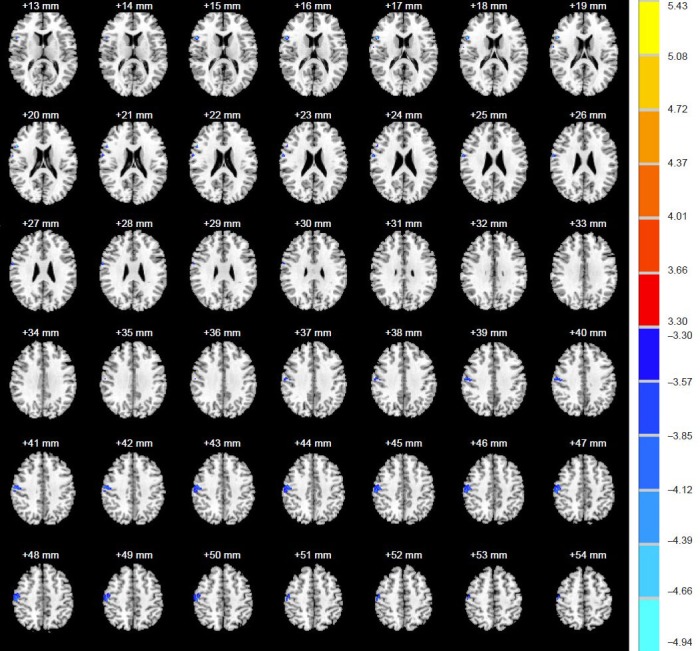
Inhibitory effects of acupuncture at Waiguan on brain activity of stroke patients.
During acupuncture, inhibition was detected in the inferior frontal gyrus, precentral gyrus, postcentral gyrus, left paracentral lobule and middle temporal gyrus. Blue represents inhibition. Red represents activation. Color bar on the right side: darker color indicates lower absolute T-values.
Effects of sham acupuncture on brain areas of ischemic stroke patients
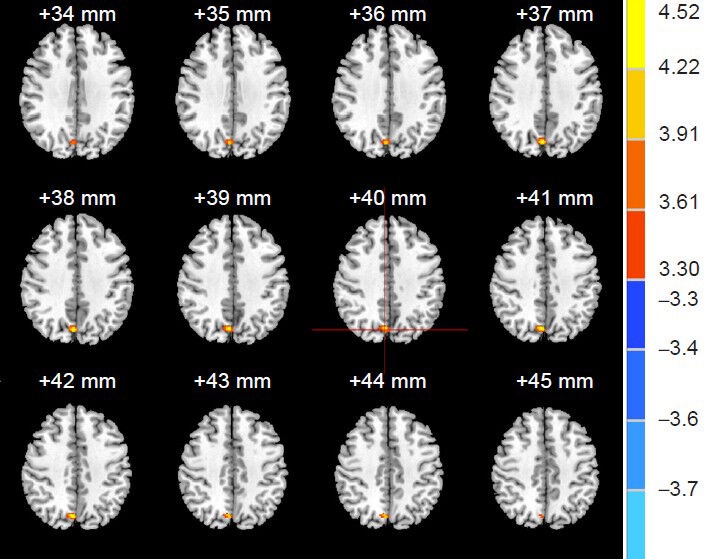
Activation of right BA7 and inhibition of left BA10 were ob- served after sham acupuncture (Table 4; Figures 3 and 4).
Table 4.
Effects of sham acupuncture on the brain activity of stroke patients
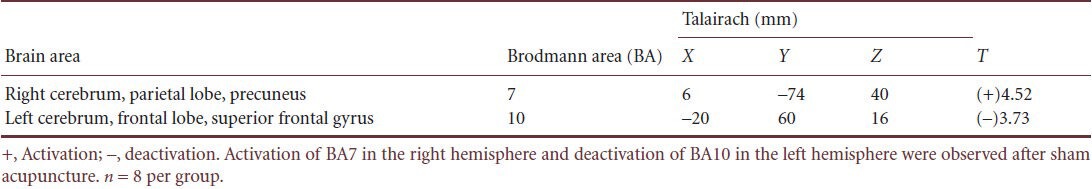
Figure 3.
Excitatory effects of sham acupuncture brain activity of stroke patients.
Increased activity was observed in right Brodmann area 7 during sham stimulation. Blue represents inhibition. Red represents activation. Color bar on the right side: darker color indicates smaller absolute T-values.
Figure 4.
Inhibitory effects of sham acupuncture on brain activity of stroke patients.
Decreased activity was observed in left Brodmann area 10 during sham acupuncture. Blue represents inhibition. Red represents activation. Color bar on the right side: darker color indicates lower absolute T-values.
Brain activity of stroke patients that differed depending of the acupuncture site (Waiguan or the sham point)
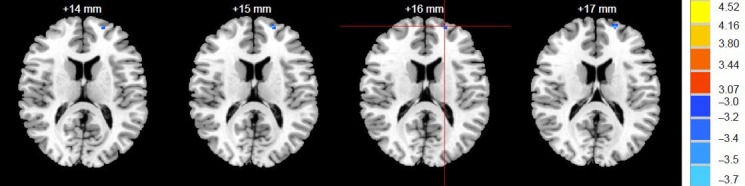
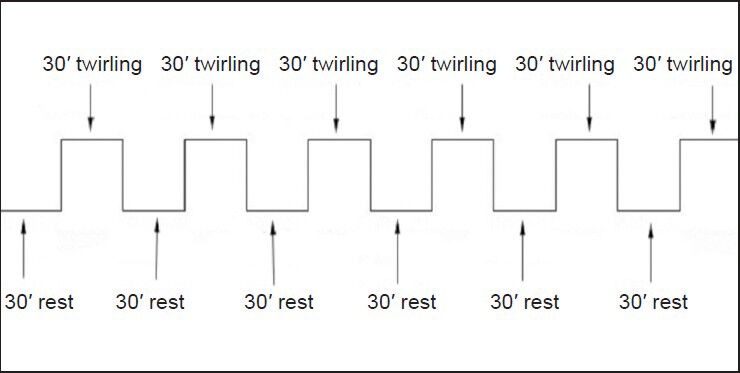
Compared with the sham point group, acupuncture at Waiguan significantly inhibited right BA5. No regions were significantly activated more during acupuncture at Waiguan than at the sham point (Table 5, Figure 5).
Table 5.
Differences of deactivation of brain areas of stroke patients undergoing acupuncture at Waiguan (SJ5) and sham acupuncture
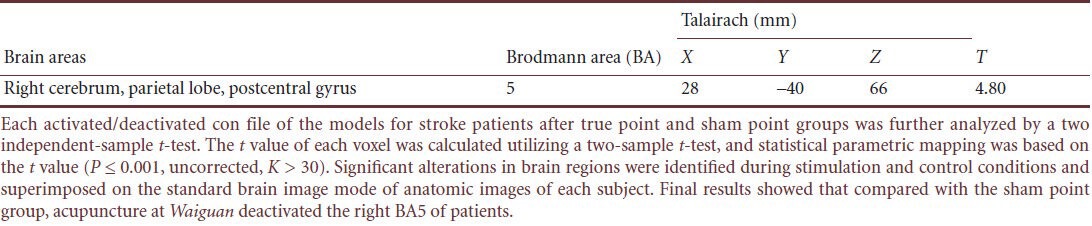
Figure 5.
Differences in brain activity of stroke patients undergoing acupuncture at true point or sham point.
Compared with the sham point group, acupuncture at Waiguan (SJ5) inhibited right Brodmann area 5. Activity did not significantly increase in any region. Blue represents inhibition. Red represents activation. Color bar on the right side: darker color indicates lower absolute T-values.
Discussion
Previous studies that have investigated the specificity of meridians and acupoints used many points, compared findings across subjects, lacked powerful evidence for their conclusions, and had relatively scattered focuses. This study chose a specific acupuncture point (Waiguan) based on the specific therapeutic effects for stroke patients, focused on comparing changes in brain activity (assessed by fMRI) between stimulation at Waiguan and a sham point, and then explored the possible central mechanism.
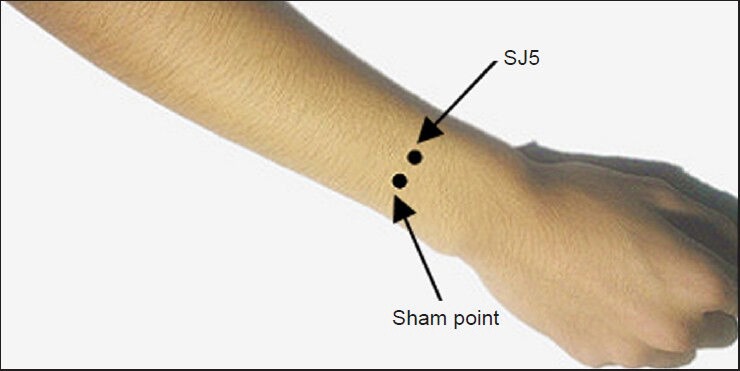
fMRI is based on alterations in oxyhemoglobin and deoxyhemoglobin, and detects brain activity in real time[20,21]. By comparing time periods in which the needles were twirled (stimulation) and when they were not moving (baseline), we could find brain regions that were more active during stimulation (higher BOLD signal during twirling), as well as those that were less active during stimulation (lower BOLD signal during twirling).
Experimental results showed that both acupuncture at Waiguan and sham acupuncture activated/deactivated several brain regions in patients with ischemic stroke. This is probably because whether at rest or doing a specific task, different brain areas exert their functions by interacting and coordinating with each other, and thus constitute a network[22]. Additionally, infarct foci were primarily in the left hemisphere. However, when compared with sham acupuncture, the specificity of acupuncture at Waiguan mainly reflected a significant reduction in BOLD signal in right BA5. That is, deoxyhemoglobin contents increased in regional blood, and this kind of change in blood oxygen saturation was associated with decreased blood flow[20,21,23]. A previous study suggested that acupuncture therapy could effectively improve blood perfusion surrounding the ischemic foci of the brain[24]. Another study confirmed that acupuncture at Waiguan in ischemic stroke patients activates brain areas in the hemisphere ipsiateral to the acupuncture site more than it does in people with undamaged brains. Moreover, the activated areas were similar to those on the affected side. This possibly resulted from improved cerebral blood circulation and promoting compensation on the healthy side[25]. BA5 is in parietal association cortex, mainly receives projections from somatosensory cortex, and participates in integrated information processing of somatic sensation. It is closely associated with tactility and space perception, and helps maintain coordination of the body during spatial activities[26]. Thus, we presume that noticeable inhibition of right BA5 possibly reflected the relative elevation of the functions of the left-brain areas. Compared with the sham point, effects of Waiguan were possibly concentrated in the healthy regions of the brain. Cerebral blood flow was reduced on the healthy side. This was consistent with the function-improving effects of acupuncture at Waiguan on the affected side.
However, this study did not demonstrate that acupuncture at Waiguan increased cerebral blood flow on the affected side compared with sham acupuncture. We presumed the reasons are as follows: (1) effects of Waiguan were possibly centralized on the healthy side. In the clinic, combining Waiguan with other points effectively improved blood perfusion surrounding the ischemic foci. (2) The sample size was relatively small and the ratio of men to women was not the same across groups. Additionally, individual difference was great. For these reasons, alterations in cerebral blood flow on the affected side were likely obscured. Because of limited conditions, pathological changes in the subjects in this study mainly occurred in the left basal ganglia. The focus range was large, and individual difference was great. This study only explored the activated/deactivated brain areas of ischemic stroke patients after acupuncture at Waiguan, and did not deeply investigate the specificity of the default network. The present study lacked clinical data on acupuncture at Waiguan alone for ischemic stroke, but only analyzed the differences of Waiguan and sham point in a pathological state. Further studies should find ways to overcome these limitations.
In summary, compared with a sham point, Waiguan acupuncture noticeably inhibited BA5 contralateral to lesions, and this is possibly a central mechanism underlying the therapeutic effect of Waiguan acupuncture in ischemic stroke patients.
Subjects and Methods
Design
A concurrent randomized controlled study.
Time and setting
Experiments were performed in the MRI Image Center, Nanfang Hospital, China from October 2008 to August 2010.
Subjects
Sixteen ischemic stroke patients were enrolled from the First Affiliated Hospital, Guangzhou University of Chinese Medicine, Guangzhou, China.
Inclusion criteria: (1) Patients were in accordance with diagnostic criteria of the Cardiovascular Health Study[27]. CT or MRI examination revealed infarct foci mainly in the left basal ganglia, with right hemiataxia (upper extremity strength and/or lower extremity strength, Chinese Stroke Scale ≥ 4 points[28]) and sensory disability; (2) patients were right handed; (3) aged between 40 and 65 years old; (4) received other therapy (Chinese medicine or western medicine) within 1 month before the experiment as well as during the experiment; (5) were non-smokers with regular eating habits that did not include excessive consumption of tea or coffee; (6) had normal sleep and (7) normal body structure (body mass index between 18.5 and 23.9; and (8) and were in a stabilized condition.
Exclusion criteria: (1) patients had a disease course longer than 1 year; (2) were pregnant or lactating; (3) could not enter an MRI because of metal implants such as heart stents or prosthetic valves; (4) had disturbed consciousness or a mental disorder; (5) suffered from obvious pain (including dysmenorrhea) or took drugs within 3 months such as analgesic or antipsychotic drugs that affect cerebral metabolism; (6) had other organ diseases that affected movement, such as cerebral hemorrhage, severe organ dysfunction, malignant hypertension, severe infection, pathological changes in the brainstem or cerebellum, or malignant tumor; (7) had undergone acupuncture treatment within four weeks of the experiment; or (8) had experienced a condition that is a contraindication for acupuncture such as hemophilia, thrombocytopenia, or other coagulation disorders.
In accordance with the Administrative Regulations on Medical Institution, formulated by State Council of China[29], the protocols and risks were informed to subjects before the experiment, and all patients signed the informed consent.
Methods
Acupuncture
Acupuncture at Waiguan: in accordance with Name and location of Acupoints (GB12346-90)[30], acupuncture was performed at the right Waiguan of stroke patients. Precise localization was as follows: on the line of Yang Pond and the olecranon of the dorsal forearm, 2 cun above the transverse striation of the dorsal wrist (the distance between the transverse line in the elbow of flat olecranon and the transverse striation in the palmar wrist was 12 cun), between ulna and radius (Figure 6). After sterilizing with iodine and alcohol, a tube needling technique was used. Tubes were purchased from DONGBANG AcuPrime, UK and silver needles were purchased from Zhongyan Taihe, Beijing, China (0.3 mm × 40.0 mm). After removal of a tube, a needle was vertically punctured at 15 ± 2 mm. After the needle was sensed, the needle was twirled at an angle of ± 180° and a frequency of 60 times/min to induce mild increasing and attenuating sensations. The acupuncture process was designed using a block method, with twirling and non-twirling stimulation alternated in 30-second blocks, and a total stimulation time of 6 minutes (Figure 7).
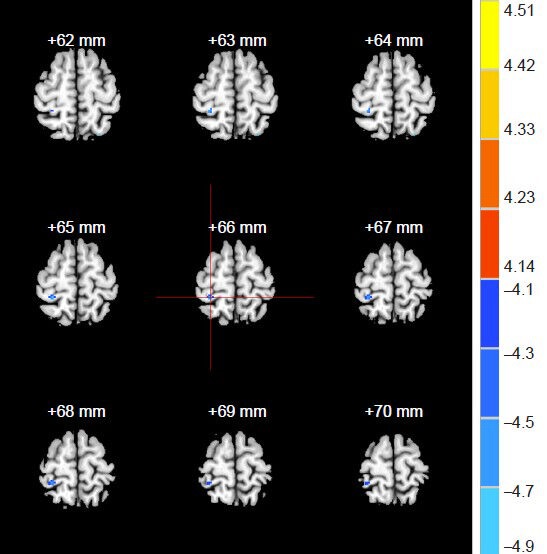
Figure 6.
Localization of acupuncture at Waiguan (SJ5) and the sham point on the right arm.
Figure 7.
The acupuncture stimulation protocol at Waiguan (SJ5).
Twirling (stimulation) and non-twirling (rest) alternated in 30-second blocks, with a total stimulation time of 6 minutes.
Sham acupuncture
The sham point was on a level with Waiguan, the midpoint of the circulating route of the forearm of Shaoyang Sanjiao Meridian of the Hand and Taiyang Small Intestine Meridian of the Hand (Figure 6). The procedure was the same as that of Waiguan.
fMRI
fMRI scanning was conducted with a 3.0 T MRI scanner (GE, Bethesda, MD, USA) and a standard head coil. The subjects used earplugs (Aearo Co., Hartford, CT, USA) and were blindfolded with an eyeshade (Xinhua Tourism Co., Hangzhou, China). Each subject rested on the bed for 5–10 minutes before the scan. Three dimensional (3D) anatomical images were collected with a T1-weighted 3D gradient echo-pulse fast spin sequence prior to acupuncture, with an axial view T1 fluid-attenuated-inversion-recovery scan. Precise parameters were as follows: time of inversion, 920 milliseconds; repetition time, 2,300 milliseconds; echo time, 21 milliseconds; slice thickness, 6.0 mm; gap 1.0 mm for 20 layers for 2 minutes 45 seconds; field of view, 24 cm × 18 cm; matrix, 320 × 256; number of excitations = 2; echo train length, 9; and band width, 50.
Collection of blood oxygenation level-dependent (BOLD) functional images was carried out during acupuncture with a single provocation echo-planar imaging sequence with a gradient echo/echo-planar imaging/90 (90° pulse) (repetition time, 3,000 milliseconds; echo time, 20 milliseconds; flip angle, 90°; slice thickness, 6.0 mm; slice gap, 1.0 mm; field of view, 24 cm × 24 cm; matrix, 96 × 96; number of excitations = 1; phase per location, 130, 2,600 phases for 6 minutes and 30 seconds).
3D scanning was followed by an axial view 3D T1 fast-spoiled gradient echo/20 T1 450. Detailed parameters are as follows: repetition time, 4.6 milliseconds; echo time, 3.3 milliseconds; flip angle, 20°; field of view, 24 cm × 18 cm; matrix, 256 × 256; number of excitations = 1; band width, 25; slice thickness, 1.2–0.6 mm; for 248 layers in 6 minutes and 2 seconds.
Data analysis
The fMRI data were processed using statistical parametric mapping 2 (SPM2) software (downloaded from http://www.fil.ion.ac.uk/). Slight movement of the head was corrected. The images were normalized to the standard brain template of the Montreal Neurological Institute space and smoothed spatially to reduce errors produced during imaging construction and to eliminate tiny differences in brain structures among subjects.
Statistical analysis
Measurement data were expressed as mean ± SD. Numeration data were expressed as ratio. The smoothed data were analyzed with a generalized linear model voxel by voxel. The T value of each voxel was calculated utilizing two-sample t-tests, and statistical parametric mapping was based on the T value (P ≤ 0.001, uncorrected, K > 30). Significant alterations in brain regions were identified during stimulation and control conditions and superimposed on the standard brain image mode of anatomic images of each subject. The activated/deactivated con files output by the models for true point and sham point groups were further analyzed by a two-independent sample t-test. Central coordinates from statistical parameters determined with SPM software package were reproduced and input in Talairach Client (download from http://www.talairach.org/client.html) to obtain the BA range of the functional areas of the brain and the anatomical location, which were corrected by a physician from the neurological medicine department in accordance with clinical experience and anatomic knowledge. A value of P < 0.05 was considered statistically significant.
Acknowledgments:
We are very grateful to all ischemic stroke patients and their family members, as well as Chen YP and Tang SS from MRI Image Center, Nanfang Hospital, China.
Footnotes
Funding: This study was supported by the State Plan for Development of Basic Research in Key Areas (973 Program) in China, No. 2006CB504505, 2012CB518504; the Key Subject Construction Project of “211 Engineering” III Stage of Guangdong Province in China; the Guangdong Provincial “College Students’ Innovative Experiment Plan” Project in China, No. 1212112038.
Conflicts of interest: None declared.
Peer review: This study explored the difference of activated brain areas after acupuncture at Waiguan and sham point for stroke, further explained the specificity of meridians and acupuncture points and the nature of the point, and established foundations for establishing the theory of acupuncture effects on the brain and application models and for setting up complete action mechanism of acupuncture.
Copyedited by Phillips A, Tang Y, Zhang ZJ, Wang J, Qiu Y, Li CH, Song LP, Zhao M
References
- [1].Liu YQ, Ma LX, Xing JM, et al. Does traditional chinese medicine pattern affect acupoint specific effect? Analysis of data from a multicenter, randomized, controlled trial for primary dysmenorrhea. J Altern Complement Med. 2013;19(1):43–49. doi: 10.1089/acm.2011.0404. [DOI] [PubMed] [Google Scholar]
- [2].Chang SL, Tsai CC, Lin JG, et al. Involvement of serotonin in the hypoglycemic response to 2 Hz electroacupuncture of zusanli acupoint (ST36) in rats. Neurosci Lett. 2005;379(1):69–73. doi: 10.1016/j.neulet.2004.12.057. [DOI] [PubMed] [Google Scholar]
- [3].Lee B, Shim I, Lee H, et al. Morphine-induced locomotor response and Fos expression in rats are inhibited by acupuncture. Neurol Res. 2010;32(Suppl 1):107–110. doi: 10.1179/016164109X12537002794444. [DOI] [PubMed] [Google Scholar]
- [4].Wang G, Han J, Litscher G, et al. System identification algorithm analysis of acupuncture effect on mean blood flux of contralateral hegu acupoint. Evid Based Complement Alternat Med 2012. 2012 doi: 10.1155/2012/951928. 951928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Li DH, Jing XH, Yang LJ, et al. Effects of acupuncture on the expression of Cx43 in different acupoints of rats. Zhongguo Zhen Jiu. 2012;32(5):431–434. [PubMed] [Google Scholar]
- [6].Lai XS, Huang Y. A cerebral functional definition on the specificity of acupoints, needling sensation and association of acupoints based on the “acupoints-brain relation hypothesis”. Zhongguo Zhen Jiu. 2007;27(10):777–780. [PubMed] [Google Scholar]
- [7].Huang Y, Li LT, Lai XS, et al. Functional brain magnetic resonance imaging in healthy people receiving acupuncture at Waiguan versus Waiguan plus Yanglingquan points: a randomized controlled trial. Zhong Xi Yi Jie He Xue Bao. 2009;7(6):527–531. doi: 10.3736/jcim20090607. [DOI] [PubMed] [Google Scholar]
- [8].Claunch JD, Chan ST, Nixon EE, et al. Commonality and specificity of acupuncture action at three acupoints as evidenced by FMRI. Am J Chin Med. 2012;40(4):695–712. doi: 10.1142/S0192415X12500528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Fu P, Jia JP, Zhu J, et al. Effects of acupuncture at Neiguan (PC 6) on human brain functional imaging in different functional states. Zhongguo Zhen Jiu. 2005;25(11):784–786. [PubMed] [Google Scholar]
- [10].Chen X, Chen J, Liu B. Central modulating mechanism of ST36 (Zusanli) acupuncturing on amplitude of low-frequency fluctuation in resting-state. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2010;30(10):1030–1035. [PubMed] [Google Scholar]
- [11].Chen P, Zhao BX, Qin W, et al. Study on the mechanism of acupuncture at Daling (PC 7) for mental diseases by fMRI. Zhongguo Zhen Jiu. 2008;28(6):429–432. [PubMed] [Google Scholar]
- [12].Yeo S, Lim S, Choe IH, et al. Acupuncture stimulation on GB34 activates neural responses associated with Parkinson's disease. CNS Neurosci Ther. 2012;18(9):781–90. doi: 10.1111/j.1755-5949.2012.00363.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Yi Y, Xu FM, Xie HW. Correlation between the liver meridian and the frontal lobe in depression by needling at taichong (LV3): a resting-state fMRI study. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2011;31(8):1044–1050. [PubMed] [Google Scholar]
- [14].Long YB, Wu XP. A meta-analysis of the efficacy of acupuncture in treating dysphagia in patients with a stroke. Acupunct Med. 2012;30(4):291–297. doi: 10.1136/acupmed-2012-010155. [DOI] [PubMed] [Google Scholar]
- [15].Zhao XF, Du Y, Liu PG, et al. Acupuncture for stroke: evidence of effectiveness, safety, and cost from systematic reviews. Top Stroke Rehabil. 2012;19(3):226–233. doi: 10.1310/tsr1903-226. [DOI] [PubMed] [Google Scholar]
- [16].Wang LH, Wang ZY, Kang XZ, et al. Comparative study on effects of different acupuncture manipulation methods at Neiguan (PC 6) on hand spasm in the patient of stroke. Zhongguo Zhen Jiu. 2008;28(7):503–506. [PubMed] [Google Scholar]
- [17].Chen XJ, Fang Z. Clinical experiences on acupuncture for treatment of cerebellar ataxia after stroke. Zhongguo Zhen Jiu. 2009;29(11):903–903. [PubMed] [Google Scholar]
- [18].Li G, Yang ES. An fMRI study of acupuncture-induced brain activation of aphasia stroke patients. Complement Ther Med. 2011;19(Suppl 1):S49–59. doi: 10.1016/j.ctim.2010.11.004. [DOI] [PubMed] [Google Scholar]
- [19].Hsu SF, Chen CY, Ke MD, et al. Variations of brain activities of acupuncture to TE5 of left hand in normal subjects. Am J Chin Med. 2011;39(4):673–686. doi: 10.1142/S0192415X11009111. [DOI] [PubMed] [Google Scholar]
- [20].Ogawa S, Lee TM, Nayak AS, et al. Oxygenation-sensitive contrast in magnetic resonance imaging of rodent brain at high magnetic fields. Magn Reson Med. 1990;14(1):68–78. doi: 10.1002/mrm.1910140108. [DOI] [PubMed] [Google Scholar]
- [21].Ogawa S, Lee TM, Kay AR, et al. Brain magnetic resonance imaging with contrast dependent on blood oxygenation. Proc Natl Acad Sci U S A. 1990;87(24):9868–9872. doi: 10.1073/pnas.87.24.9868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Su SJ, Zhao XF, Wang S. Application of cerebral function imaging in research on the acupoints specificity. Zhongguo Zhen Jiu. 2010;30(4):293–295. [PubMed] [Google Scholar]
- [23].Zhao XH. Hangzhou: Zhejiang Daxue, China; 2006. A fMRI study of deactivation and default mode network activity in human brain. [Google Scholar]
- [24].Lee JD, Chon JS, Jeong HK, et al. The cerebrovascular response to traditional acupuncture after stroke. Neurorndiology. 2003;45(11):780–784. doi: 10.1007/s00234-003-1080-3. [DOI] [PubMed] [Google Scholar]
- [25].Chen JQ, Huang Y, Lai XS, et al. Acupuncture at Waiguan (TE5) influences activation/deactivation of functional brain areas in ischemic stroke patients and healthy people: a functional MRI study. Neural Regen Res. 2013;8(3):226–232. doi: 10.3969/j.issn.1673-5374.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Bear MF, Connors BW, Paradiso MA. 2nd ed. Beijing: Higher Education Press, China; 2004. Neuroscience: Exploring the Brain. [Google Scholar]
- [27].Price TR, Psaty BM, O’Leary D, et al. Assessment of cerebrovascular disease in the Cardiovascular Health Study. Ann Epidemiol. 1993;3:504–507. doi: 10.1016/1047-2797(93)90105-d. [DOI] [PubMed] [Google Scholar]
- [28].Sun TK, Chiu SC, Yeh SH, et al. Assessing reliability and validity of the Chinese version of the stroke scale: scale development. Int J Nurs Stud. 2006;43:457–463. doi: 10.1016/j.ijnurstu.2005.07.004. [DOI] [PubMed] [Google Scholar]
- [29].State Council of the People's Republic of China. Administrative Regulations on Medical Institution. 1994-09-01 [Google Scholar]
- [30].General Administration of Quality Supervision, Inspection and Quarantine, the Standardization Administration, People's Republic of China. Name and location of Acupoints: Chinese National Standards. 2006 [Google Scholar]
- [31].Nopperncy U, Price CJ. Functional imaging of the semantic system: Retrieval of sensory-experienced and verbally learned knowledge. Brain Lang. 2003;84(1):120–133. doi: 10.1016/s0093-934x(02)00525-4. [DOI] [PubMed] [Google Scholar]


