Abstract
One hundred and five patients with primary unipolar depression were randomly divided into three groups: drug group (Seroxat administration), acupuncture group (Seroxat plus acupuncture), and electroacupuncture group (Seroxat plus acupuncture plus electroacupuncture). Patients’ symptoms were evaluated using a psychometric questionnaire, the Symptom Checklist-90, before intervention and after 2, 4, 6 and 10 weeks of treatment. The individual factor scores and the total score from the Symptom Checklist-90 reduced in all three groups as treatment progressed. In the acupuncture and electroacupuncture groups, the total score and the factor scores for obsessive-compulsive symptoms, depression, and anxiety were significantly lower than those in the drug group. There was no significant difference in the factor scores or total scores between the acupuncture and electroacupuncture groups. Some factor scores in the electroacupuncture group, such as somatization, depression, hostility, and phobic anxiety, were increased at 10 weeks compared with the respective score immediately after the course of electroacupuncture at 6 weeks. Our findings indicate that administration of Seroxat alone or in combination with acupuncture/electroacupuncture can produce a significant effect in patients with primary unipolar depression. Furthermore, acupuncture/electroacupuncture has a rapid onset of therapeutic effect and produces a noticeable improvement in obsessive-compulsive, depressive and anxiety symptoms.
Keywords: nerve regeneration, acupuncture and moxibustion, electroacupuncture, selective serotonin reuptake inhibitor, Seroxat, primary unipolar depression, Symptom Checklist-90, anxiety, NSFC grant, neural regeneration
Introduction
Acupuncture is more effective than oral antidepressants in improving depressive symptoms[1]. Yeung et al.[2] further confirmed the validity of acupuncture therapy, once or twice per week, in patients with poor outcomes after antidepressant medications. Meanwhile, acupuncture therapy produces fewer side effects than tricyclic antidepressants[3]. The systemic reviews and meta-analysis by Zhang et al.[4] provide strong evidence for the efficacy and safety of acupuncture in the treatment of depression.
Despite the continued development of antidepressants and alternative/synergistic therapies, major depressive disorder has not been comprehensively recognized and treatment outcome is often insufficient[5]. An epidemiological study addressing depression showed that poor recognition and treatment are largely linked to the lack of an accurate assessment tool and to patients’ economic situation[6]. Previous studies from our research group found that treatment efficacy in depression is mainly evaluated according to changes (rate of reduction) in Hamilton Depression Rating Scale scores[7,8]. In addition, the Zung Self-Rating Depression Scale[9], Treatment Emergent Symptom Scale[10] and Montgomery-Asberg Depression Rating Scale[11] are often applied to assess treatment efficacy. We adopted a different index, the Symptom Checklist-90, in an effort to provide consistent assessment criteria for primary depression.
The Symptom Checklist-90 is a relatively brief self-report psychometric instrument (questionnaire) for the evaluation of a broad range of psychological problems and symptoms of psychopathology. It is also used to measure the progress and outcome of psychiatric and psychological treatment, or for research purposes. This scale has a large capacity, lists abundant symptoms, and accurately reflects subjects’ subjective symptoms. It is designed to assess individual psychological feelings, emotion, thinking, behavior, living habits, interpersonal relationships, diet and sleep, and other symptoms[12]. Although the Symptom Checklist-90 is well known, it is not the most widely used evaluation index.
In the present randomized controlled study, we compared the clinical efficacy of acupuncture/electroacupuncture combined with an antidepressant drug, with that of an antidepressant drug alone, using the Symptom Checklist-90.
Results
Quantitative analysis of participants
One hundred and five patients with primary unipolar depression were randomly allocated to three groups: drug group (Seroxat), acupuncture group (Seroxat + acupuncture) and electroacupuncture group (Seroxat + acupuncture + electroacupuncture). Each group comprised 35 patients. Two subjects in the drug group, four in the acupuncture group, and four in the electroacupuncture group were excluded because they failed to complete the treatment due to family relocation, job transfers or loss of contact during treatment. No available data were obtained and they were considered drop-outs.
Two subjects in the drug group, one in the acupuncture group and two in the electroacupuncture group discontinued treatment due to job transfers; two subjects in the acupuncture group were lost to follow-up. After 6 weeks of treatment, ten subjects in the drug group, five subjects in the acupuncture group and five subjects in the electroacupuncture group were uncooperative to the follow-up program and were also considered lost to follow-up. Some data acquired from these subjects were included in the intention-to-treat analysis.
Final numbers of subjects included in the statistical analysis were 33 in the drug group, 31 in the acupuncture group and 31 in the electroacupuncture group (Figure 1).
Figure 1.
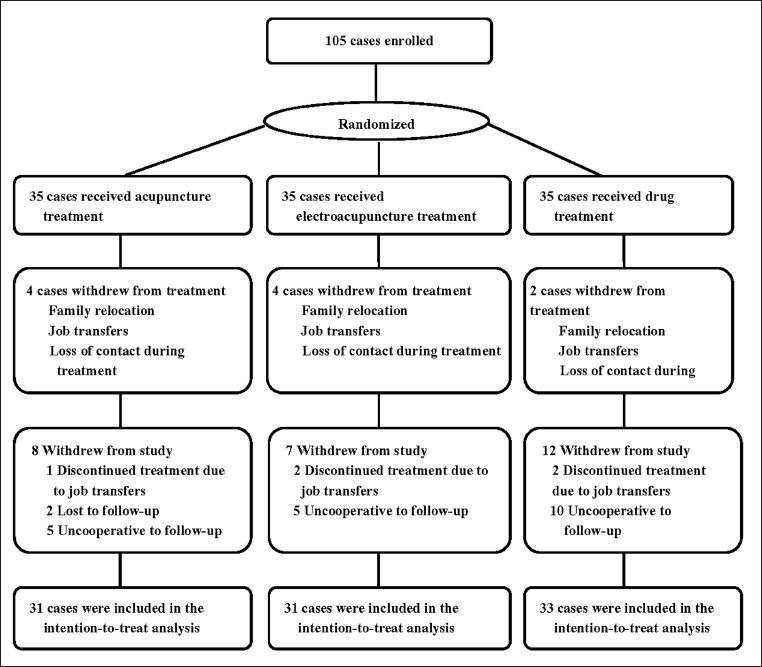
Flowchart of primary unipolar depressive patients included in the analysis.
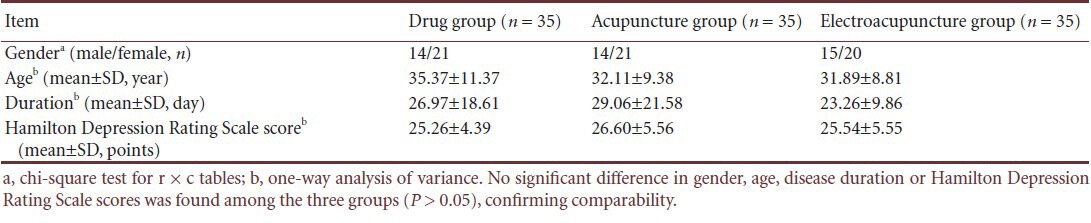
Baseline information
There were no significant differences in the gender, age, disease duration or Hamilton Depression Rating Scale scores among the three groups of 35 subjects enrolled initially (P > 0.05). This indicates that the grouping was balanced and data are comparable (Table 1).
Table 1.
Comparison of basic information of depressed patients in the three groups
Change in total Symptom Checklist-90 scores and factor scores in patients with primary unipolar depression before and after acupuncture/electroacupuncture combined with Seroxat
Comparison of somatization scores
One-way analysis of variance and covariance showed no significant differences among the three groups (P > 0.05) in somatization scores before treatment, at 2, 4 or 6 weeks after treatment, or at follow-up (10 weeks after treatment). Somatization scores steadily reduced as treatment time progressed, which indicated that somatization symptoms improved with treatment. One-way repeated measures analysis of variance showed that after 4, 6 and 10 weeks of acupuncture or electroacupuncture, somatization scores in the acupuncture and electroacupuncture groups were significantly lower than those before treatment (P < 0.05). In addition, somatization scores in the drug and acupuncture groups were lowest at 10 weeks, whereas in the electroacupuncture group the score was lowest at 6 weeks with a slight increase observed at 10 weeks (4 weeks after the end of the acupuncture course) (Table 2).
Table 2.
Effect of acupuncture/electroacupuncture combined with the Seroxat on Symptom Checklist-90 scores in patients with primary unipolar depression
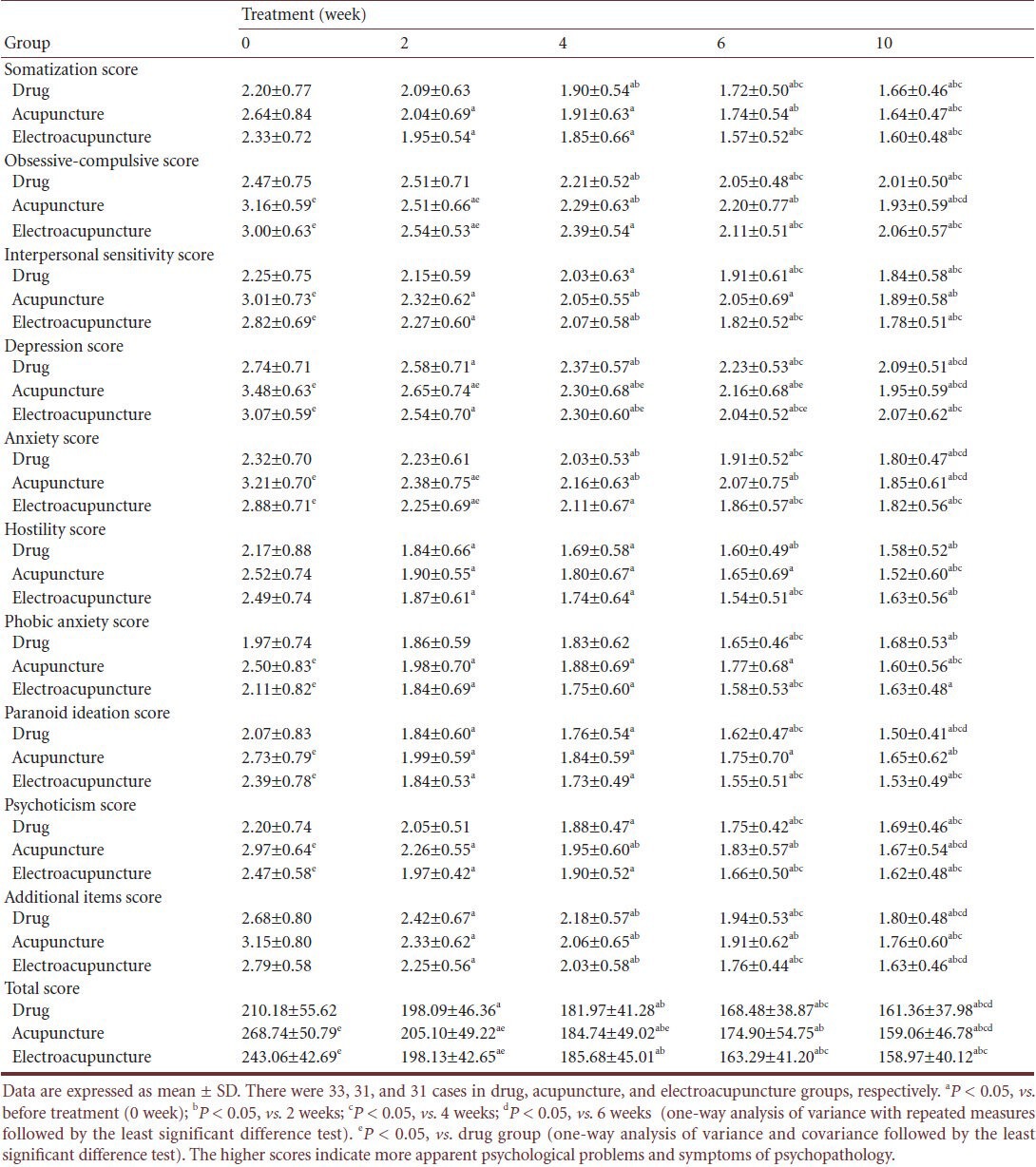
Comparison of obsessive-compulsive scores
One-way analysis of variance showed that obsessive-compulsive scores in the drug group were significantly lower than those in the acupuncture and electroacupuncture groups before treatment (P < 0.05), indicating that obsessive-compulsive symptoms were worse in those groups. Analysis of covariance revealed significant differences in obsessive-compulsive scores among the three groups at 2 weeks (P < 0.05). Furthermore, pairwise comparisons showed that the degree of improvement in the acupuncture and electroacupuncture groups was significantly better than that in the drug group (P = 0.002 and 0.022); after 4, 6 or 10 weeks of treatment, obsessive-compulsive scores had no differences among the three groups (P > 0.05). The obsessive-compulsive scores reduced steadily as the treatment progressed, indicating that obsessive-compulsive symptoms improved with treatment. One-way repeated measures analysis of variance showed that obsessive-compulsive scores at 4, 6 and 10 weeks in the acupuncture group and at 2, 4, 6 and 10 weeks in the electroacupuncture group were significantly lower than those before treatment (P < 0.05). In addition, obsessive-compulsive scores in all three groups were lowest at 10 weeks (Table 2).
Comparison of interpersonal sensitivity scores
One-way analysis of variance showed that interpersonal sensitivity scores in the drug group were significantly lower than those in the acupuncture and electroacupuncture groups before treatment (P < 0.05), indicating that interpersonal sensitivity symptoms were more apparent in the acupuncture and electroacupuncture groups. Analysis of covariance revealed no significant differences in interpersonal sensitivity scores among three groups at 2, 4, 6, or 10 weeks (P > 0.05). The interpersonal sensitivity scores reduced steadily as treatment progressed, indicating that interpersonal sensitivity symptoms improved with treatment. One-way repeated measures analysis of variance showed that interpersonal sensitivity scores at 4, 6, and 10 weeks in the drug group and at 2, 4, 6, and 10 weeks in the acupuncture and electroacupuncture groups were significantly lower than those before treatment (P < 0.05). In addition, interpersonal sensitivity scores in the three groups were lowest at 10 weeks (Table 2).
Comparison of depression scores
One-way analysis of variance showed that depression scores in the drug group were significantly lower than those in the acupuncture and electroacupuncture groups before treatment (P < 0.05), indicating that depression symptoms were more apparent in the acupuncture and electroacupuncture groups. Analysis of covariance revealed significant differences in depression scores among the three groups at 2, 4 and 6 weeks (P < 0.05). Furthermore, pairwise comparisons showed that the degree of improvement at 2, 4 and 6 weeks in the acupuncture group, and at 4 and 6 weeks in the electroacupuncture group, was significantly better than that in the drug group (P < 0.05); at 10 weeks, no difference was observed between depression scores in the three groups (P > 0.05). Depression scores steadily declined as the treatment time progressed, indicating that depression symptoms improved with treatment. One-way repeated measures analysis of variance showed that depression scores in all three groups were significantly lower at 2, 4, 6 and 10 weeks than before treatment (P < 0.05). In addition, depression scores in the drug and acupuncture groups were lowest at 10 weeks. The score for the electroacupuncture group was slightly higher at 10 weeks than at 6 weeks (Table 2).
Comparison of anxiety scores
One-way analysis of variance showed that anxiety scores in the drug group were significantly lower than those in the acupuncture and electroacupuncture groups before treatment (P < 0.05), indicating that anxiety symptoms were more evident in the two latter groups. Analysis of covariance revealed significant differences in anxiety scores among the three groups at 2 weeks (P < 0.05). Furthermore, pairwise comparisons showed that the degree of improvement in anxiety in the acupuncture and electroacupuncture groups at 2 weeks was significantly better than that of the drug group (P < 0.05); at 4, 6 and 10 weeks after treatment, no differences in anxiety scores were observed between the three groups (P > 0.05). One-way repeated measures analysis of variance showed that anxiety scores at 4, 6 and 10 weeks in the drug group, and at 2, 4, 6 and 10 weeks in the acupuncture and electroacupuncture groups, were significantly lower than before treatment (P < 0.05). In addition, anxiety scores for all three groups were lowest at 10 weeks (Table 2).
Comparison of hostility scores
One-way analysis of variance and covariance revealed no significant differences in hostility scores among the three groups before or after treatment (P > 0.05). As treatment time progressed, hostility scores in the three groups steadily reduced, indicating that hostility symptoms were improved after treatment. One-way repeated measures analysis of variance showed that hostility scores in the three groups were significantly lower at 2, 4, 6 and 10 weeks than before treatment (P < 0.05). In addition, the hostility scores in the drug and acupuncture groups were lowest at 10 weeks, although in the electroacupuncture group the score at follow-up was slightly higher than that at 6 weeks (Table 2).
Comparison of phobic anxiety scores
One-way analysis of variance showed that phobic anxiety scores in the drug group were significantly lower than those in the acupuncture and electroacupuncture groups before treatment (P < 0.05), indicating that phobic anxiety symptoms were worse in the acupuncture and electroacupuncture groups. Analysis of covariance revealed no significant differences in phobic anxiety scores among the three groups at 2, 4, 6 or 10 weeks (P > 0.05). The phobic anxiety scores reduced to varying degrees as the treatment progressed, which indicated that symptoms improved with treatment. One-way repeated measures analysis of variance showed that phobic anxiety scores at 6 and 10 weeks in the drug group, and at 2, 4, 6 and 10 weeks in the acupuncture and electroacupuncture groups, were significantly lower than those before treatment (P < 0.05). In addition, phobic anxiety scores in the acupuncture group reached a minimum at 10 weeks, whereas the scores at follow-up were slightly higher than those at 6 weeks in the drug and electroacupuncture groups (Table 2).
Comparison of paranoid ideation scores
One-way analysis of variance showed that paranoid ideation scores in the drug group were significantly lower than in the acupuncture and electroacupuncture groups before treatment (P < 0.05), indicating that paranoid ideation symptoms were apparent in the acupuncture and electroacupuncture groups. Analysis of covariance revealed no significant differences in paranoid ideation scores among the three groups at 2, 4, 6 or 10 weeks (P > 0.05). The paranoid ideation scores decreased steadily as treatment progressed, which indicated that paranoid ideation symptoms were improved after treatment. One-way repeated measures analysis of variance showed that paranoid ideation scores in all three groups were significantly lower at 2, 4, 6 and 10 weeks than before treatment (P < 0.05). In addition, scores were lowest at 10 weeks for all groups (Table 2).
Comparison of psychoticism scores
One-way analysis of variance showed that psychoticism scores in the drug group were significantly lower than those in the acupuncture and electroacupuncture groups before treatment (P < 0.05), indicating that psychoticism symptoms were more apparent in the acupuncture and electroacupuncture groups. Analysis of covariance revealed no significant differences in psychoticism scores among three groups after 2, 4, 6 or 10 weeks of treatment (P > 0.05). The psychoticism scores reduced steadily as the treatment time progressed, which indicated that psychoticism symptoms improved with treatment. One-way repeated measures analysis of variance showed that psychoticism scores at 4, 6 and 10 weeks in the drug group and at 2, 4, 6 and 10 weeks in the acupuncture and electroacupuncture groups were significantly lower than those before treatment (P < 0.05). In addition, the lowest scores were observed at 10 weeks (Table 2).
Comparison of additional item scores
One-way analysis of variance showed that additional item scores in the drug group were significantly lower than those in the acupuncture and electroacupuncture groups before treatment (P < 0.05), indicating that additional symptoms were apparent in the acupuncture and electroacupuncture groups. Analysis of covariance revealed no significant differences in additional item scores among the three groups at 2, 4, 6 or 10 weeks (P > 0.05). The additional item scores reduced as the treatment progressed, indicating that additional symptoms were improved after treatment. One-way repeated measures analysis of variance showed that additional item scores in all three groups were significantly lower at 2, 4, 6 and 10 weeks compared with those before treatment (P < 0.05). In addition, the lowest score for additional items was observed at 10 weeks (Table 2).
Comparison of total Symptom Checklist-90 scores
One-way analysis of variance showed that total scores of the Symptom Checklist-90 were significantly lower in the drug group than in the acupuncture and electroacupuncture groups before treatment (P < 0.05), indicating that general psychiatric symptoms were worse in the acupuncture and electroacupuncture groups than the drug group. Analysis of covariance revealed significant differences in total scores among the three groups at 2 and 4 weeks (P < 0.05). Furthermore, pairwise comparisons showed that the degree of total symptom improvement in the acupuncture group at 2 and 4 weeks and in the electroacupuncture group at 2 weeks was significantly better than that in the drug group (P < 0.05); after 6 and 10 weeks of treatment, total scores were not different between the three groups (P > 0.05). Total scores decreased as the treatment progressed, which indicated that total symptoms improved with treatment. One-way repeated measures analysis of variance showed that total scores of the Symptom Checklist-90 at 2, 4, 6 and 10 weeks were significantly lower in all three groups than before treatment (P < 0.05). In addition, the lowest total Symptom Checklist-90 scores were observed at 10 weeks (Table 2).
Adverse reactions
Three subjects in the drug group had mild insomnia, nausea and headaches. One subject in the acupuncture group had moderate loss of appetite. Two subjects in the electroacupuncture group had mild insomnia and dry mouth. No other subjects presented with adverse reactions.
Discussion
Depressive disorder is commonly accompanied by other psychiatric symptoms[13]. For example, anxiety (panic disorder, phobias, and generalized anxiety) is present in 40% of depressed patients[14] and personality disorders in 33% (compulsive 16%, paranoid 10% and schizoid personality disorder 7%)[14]. Depression is also closely related to physical illness; severe and chronic physical illnesses often lead to depressive disorders, and some medications can cause symptoms of depression[15]. Furthermore, comorbid conditions may reduce the clinical efficacy of antidepressants[16]. Therefore the above diseases should be taken into consideration when screening drugs and using an assessment scale.
The existing treatment options for major depressive disorder include medication, psychotherapy and social therapy. Medication is most commonly used and includes tricyclic antidepressants, tetracyclic antidepressants and new antidepressants such as selective serotonin and/or norepinephrine reuptake inhibitors. In many countries, selective serotonin reuptake inhibitors are the preferred antidepressant drug[17] because they are generally well tolerated, have a low discontinuation rate[18], and are simple to administer, which reduces the risk of inadequate doses in depressed patients. We adopted the selective serotonin reuptake inhibitor paroxetine (Seroxat) as the basic medicationin the present study because it has a strong effect on severe depression, obsessive-compulsive disorder, panic, generalized anxiety, social phobia and post-traumatic stress disorder; it also exhibits strong sedative effects[19].
However, adverse effects of selective serotonin reuptake inhibitors should be noted. With short-term treatment, gastrointestinal symptoms are commonly seen, such as nausea, vomiting, and diarrhea; in addition, restlessness, agitation, sleep disturbances, dizziness and headaches are also observed. Over the long term, patients may develop sexual dysfunction, such as loss of libido and anorgasmia[20]. Therefore, there remains a need for an alternative therapeutic strategy in the treatment of depression. The use of complementary or synergic therapy is increasing in Western medicine, but clinical studies investigating its effectiveness in anxiety and depression are lacking[21].
Acupuncture has been widely used in the clinical treatment of depressive disorders[22]. The pathogenesis of depression derives from the brain, but also involves the liver, heart, spleen, stomach and other organs. Acupuncture therapy aims to nourish the brain, replenish vitality, disperse liver stagnation, and smooth emotions[23,24]. Previous studies[25,26,27,28,29,30,31,32,33,34,35] concerning the location of acupoints in acupuncture treatment for primary depression showed that the main points are located in Du meridian, pericardium meridian, spleen meridian, liver meridian and stomach meridian; the common points are Baihui (DU20) and Yintang (EX-HN3). First, Du meridian[36] is responsible for regulating consciousness disease and organ lesions. Baihui[25] belongs to Du meridian and regulates mentality. Yintang[26] is responsible for nourishing the brain, replenishing vitality, and adjusting emotional disorder. Baihui and Yintang are collectively referred to as Baiyin point, which has been confirmed to be effective in the treatment of depression[27,28]. Second, hepatobiliary meridian can adjust brain function[29,30]. Dazhui (DU14)[30] also belongs to Du meridian and can be applied in the treatment of encephalopathy. Third, the heart dominates blood circulation; acupuncture at the heart reorganizes the triple energizer, calms the nerves, and benefits the diaphragm. Neiguan (PC6)[25] is the collateral point in pericardium meridian; acupuncture at Neiguan can regulate vital energy and anchor the mind. Sanyinjiao (SP6)[31] is the intersection point of Zutaiyin, Zujueyin and Zushaoyin, which is responsible for nourishing Yin, invigorating the spleen, reinforcing the liver, tonifying the kidney, and harmonizing the blood. Sanyinjiao is an important point in the treatment of primary insomnia. Finally, Zusanli (ST36)[32], Shenmen (HT7)[33], Shuaigu (GB8)[34] and Zhigou (SJ6)[35] are suggested for the treatment of anorexia, poor sleep, headaches or constipation. Therefore, the prescription acupoints of acupuncture/electroacupuncture treatment in the present study are Baihui, Yintang, Fengfu, Fengchi (bilateral), Dazhui, Neiguan (bilateral), and Sanyinjiao (bilateral); Zusanli is added for poor appetite or fatigue, Shenmen for poor sleep, Shuaigu for headache, and Zhigou for constipation.
Symptom Checklist-90 assessment results from the present study showed the following: (1) Both acupuncture/electroacupuncture and Seroxat have good therapeutic effects on primary unipolar depression. Symptom Checklist-90 total scores and factor scores were significantly decreased after treatment, indicating that the symptoms of depression were significantly improved. (2) Acupuncture/electroacupuncture combined with Seroxat had a rapid onset of therapeutic effect. Symptom Checklist-90 total scores after 2 weeks of acupuncture/electroacupuncture combined with Seroxat therapy were significantly lower than after Seroxat alone. (3) Acupuncture/electroacupuncture combined with Seroxat therapy significantly improved obsessive-compulsive symptoms and anxiety in patients with primary unipolar depression. Obsessive-compulsive and depressive symptoms were significantly improved after 2 weeks of acupuncture/electroacupuncture combined with Seroxat therapy, in comparison with Seroxat alone; the improvement of depression symptoms was observed at 2, 4 and 6 weeks after acupuncture and at 4 and 6 weeks after electroacupuncture. (4) Acupuncture plus Seroxat is equally effective as electroacupuncture plus Seroxat in the treatment of primary unipolar depression. (5) After discontinuation of acupuncture/electroacupuncture, some symptoms worsened in patients with primary unipolar depression. After 6 weeks of treatment, patients in three groups were given oral Seroxat alone for 4 weeks. The results at follow-up showed that Symptom Checklist-90 scores of somatization, depression, hostility and phobic anxiety in the electroacupuncture group, and phobic anxiety score in the drug group, were slightly increased compared with those at 6 weeks, but the difference was not statistically significant. (6) Acupuncture/electroacupuncture plus Seroxat is a safe treatment for primary unipolar depression, with few adverse effects.
The biological mechanisms underlying depression have been studied in the fields of genetics, neurobiology, endocrinology, electrophysiology and imaging[37], but remain incompletely elucidated. A number of studies confirm that structural changes of some brain areas (hippocampus, amygdala, cortex)[38] and an imbalance of neurotransmitters (serotonin and noradrenaline)[39,40] are closely linked with the pathogenesis of depression. Effective antidepressant treatment also underlines the contribution of these brain areas and neurotransmitters to the disorder. For example, Vaidya et al.[41] found that antidepressants enhance sprouting of axons and dendrites; Malberg et al.[42] showed that some antidepressants promote the development of hippocampal neurons; Sairanen et al.[43] highlighted that long-term antidepressants constructed a new neural network; and Brunello et al.[44] and Nutt et al.[45] showed that classical antidepressants block serotonin or norepinephrine reuptake to varying degrees. Acupuncture/electroacupuncture regulates monoamine neurotransmitters in the prefrontal cortex, increasing serotonin and norepinephrine levels and regulating the balance of serotonin and its main metabolite, 5-hydroxyindoleacetic acid[46]. Other actions include reducing damage to hippocampal neurons, upregulating hippocampal brain-derived neurotrophic factor and cyclic adenosine monophosphate-response element binding protein[47], and decreasing serum concentrations of corticosterone and adrenocorticotropic hormone[48], thus producing antidepressant effects.
In summary, both oral administration of Seroxat alone and the combined therapy of acupuncture/electroacupuncture plus Seroxat are effective treatments of primary unipolar depression. However, compared with either treatment alone, combined therapy significantly improves overall symptoms, and especially obsessive-compulsive, depressive, and anxiety symptoms.
Subjects and Methods
Design
A randomized controlled clinical trial.
Time and setting
Experiments were performed from December 2008 to October 2010 at the Department of Acupuncture and Moxibustion, School of Chinese Traditional Medicine, Southern Medical University; Naturopathy Center, Hospital of Integrated Chinese and Western Medicine, Southern Medical University; Department of Acupuncture and Moxibustion, Overseas Chinese Hospital; and the Department of Psychological and Behavioral Medicine, 999 Brain Hospital, China.
Subjects
Patients with primary unipolar depression were recruited by psychiatric physicians, and diagnoses were confirmed by attending physicians.
Diagnostic criteria
Primary unipolar depression was diagnosed by the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) for Mental and Behavioral Disorders, issued by the World Health Organization[49], as follows:
-
(1)
Three conditions of depressive episode: lasting for at least 2 weeks; no episodes of hypomania or mania; not caused by psychoactive substances or organic mental disorder.
-
(2)
Three core symptoms of depressive episodes: abnormally depressed mood for 2 weeks, not influenced by the environment; loss of interest or pleasure in usual activities of interest; lack of energy or fatigue.
-
(3)
Additional symptoms of depressive episodes: loss of self-confidence and self-esteem; unfounded remorse or excessive and inappropriate guilt; recurrent thoughts of death or suicide, or any kind of suicidal behavior; complaint or evidence of thought or attention decrease, such as indecision or hesitation; psychomotor activity changes, showing agitation or retardation (subjective feelings or objective evidence is available); any type of sleep disorders; appetite changes (decrease or increase), accompanied by a corresponding change in body mass.
-
(4)
Mild depressive episode (F32.0): at least two core symptoms and at least four core and additional symptoms.
-
(5)
Moderate depressive episode (F32.1): at least two core symptoms and at least six core and additional symptoms.
-
(6)
Severe depressive episode (F32.2): three core symptoms and eight core and additional symptoms.
Inclusion criteria
(1) Subjects aged 18–60 years, male or female; (2) meeting the diagnostic criteria of ICD-10 for mild and moderate depressive episodes (F32.0, F32.1); (3) Hamilton Rating Scale score ≥ 17 points[50] at acute phase of depression.
Exclusion criteria
(1) Subjects who had participated in other clinical trials within 4 weeks prior to experimentation; (2) subjects taking antidepressants or were in the elution period of antidepressant pharmacological action; (3) subjects with suicidal plans or behavior; (4) subjects with comorbid systemic diseases; (5) subjects with brain diseases; (6) subjects not candidates for acupuncture due to thrombocytopenia and hemophilia; (7) women who were pregnant, potentially pregnant or lactating; (8) postpartal and menopausal women; (9) subjects considered unable to cooperate with the treatment schedule or evaluation owing to psychosis or illiteracy.
Discontinuation criteria
(1) Subjects starting other forms of treatment during the study; (2) subjects who were intolerant or allergic to Seroxat, or who discontinued the medication due to adverse reactions; (3) subjects presenting with pathophysiological changes; (4) subjects who voluntarily quit the study or were lost to follow-up.
Forty-three males and 62 females aged 33.12 ± 9.95 (range 18–59) years with primary unipolar depression were excluded from enrollment upon initial screening. All the enrolled subjects gave written informed consent and voluntarily participated in the experiment. All experimental protocols were in strict accordance with the ethical requirements in the Declaration of Helsinki.
Methods
Treatment
Location of points: All the acupoints were selected according to the World Federation of Acupuncture-Moxibustion Societies (GB 12346-90)[52].
Baihui (DU20): Du meridian point, on the head, 5 cun above anterior hair line or the midpoint of the line between two ear apexes.
Yintang (EX-HN3): Extra point, on the forehead, between the two eyebrows.
Fengfu (DU16): Du meridian point, on the neck, 1 cun above posterior hair line, below external occipital protuberance, between trapezius muscles.
Fengchi (GB20): belongs to the Gall Bladder Channel of Foot-Shaoyang, on the neck, equal to Fengfu, between sternocleidomastoid and upper trapezius muscle.
Dazhui (DU14): Du meridian point, on posterior middle line, below the seventh cervical spine.
Neiguan (PC6): belongs to Pericardium Channel of Hand Jueyin, on palm side of the forearm, 2 cun above wrist transverse striation, between the long palmar muscle and flexor carpi radialis muscle tendon.
Sanyinjiao (SP6): belongs to the Spleen Channel of Foot-Taiyin, on the leg, 3 cun above the medial malleolus, at posterior medial angle of the tibia.
Zusanli (ST36): belongs to the Stomach Channel of Foot-Yangming, on anterior lateral leg, 3 cun below Dubi, one finger distant away from anterior border of tibia.
Shenmen (HT7): belongs to the Heart Channel of Hand-Shaoyin, at the transverse striation on the ulnar side of the palm side of the wrist, at radial side of the flexor carpi ulnaris.
Shuaigu (GB8): belongs to the Gall Bladder Channel of Foot-Shaoyang, on the head, 1.5 cun deep below the hair line, above the Angled Collateral.
Zhigou (SJ6): belongs to Triple Energizer Channel of Hand Shaoyang, at dorsal forearm, on the connection line between Yangchi and olecranon, 3 cun above the dorsal wrist transverse striation, between the ulna and radius.
Accident management: Needle position was changed if patients felt pain; hemostasis was allowed to occur when withdrawing the needle; acupuncture syncope and needle breakage are considered accidents.
Drug group: Patients were given oral Seroxat (National Medicine Permit No. H10950043; Sino-American Tianjin SmithKline and French Lab., Ltd., Tianjin, China)[51]. The dose was 10 mg per day on days 1 and 2, then 20 mg per day until the end of the experiment. The drug treatment lasted for 6 weeks (one course).
Acupuncture group: (1) Oral Seroxat, as drug group. (2) Hand acupuncture: the main points are Baihui, Yintang, Dazhui, Fengfu, Fengchi (bilateral), Neiguan (bilateral), Sanyinjiao (bilateral); coordinate points are Zusanli for poor appetite or fatigue, Shenmen for poor sleep, Shuaigu for headache, Zhigou for constipation. The stainless steel needle was provided by Suzhou Universal Acupuncture Medical Devices Co., Ltd., Suzhou, Jiangsu Province, China (specifications: 0.30 mm × 40 mm, 0.30 mm × 25 mm).
Electroacupuncture group: (1) Oral Seroxat, as drug group; (2) electroacupuncture treatment: acupuncture regimen as acupuncture group and electroacupuncture at Baihui and Yintang using LH-202H Han's acupoint stimulator (supervised by the Neuroscience Research Institute, Peking University, Beijing, China; produced by Beijing Hua Wei Industrial Development Company, Beijing, China). The waveform was disperse-dense wave, at 2 or 15 Hz frequency. The strength of the current depended on the patient's tolerance (slight skin jittering). The needle was in place for 30 minutes and twisted once at 15 minutes for 5–10 seconds. The electroacupuncture intervention was given on alternate days, three times a week, for 6 weeks (one course).
Follow-up
After 6 weeks of treatment, all the enrolled patients continued oral Seroxat (20 mg per day) for a further 4 weeks. Acupuncture and electroacupuncture interventions were terminated. After 4 weeks, all subjects were visited at the Outpatient Department or at home.
Symptom Checklist-90 assessment
This checklist consists of 90 items, each graded on a scale of 1–5 points, as follows: 1, no symptom; 2, very light symptom; 3, mild or moderate symptom; 4, severe symptom; 5, symptom extremely severe in frequency and intensity[12]. The primary symptoms are somatization, obsessive-compulsive traits, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, psychoticism, and a category of “additional items”. A positive diagnosis is determined upon total scores of more than 160 points, or any factor score of more than 2 points. Statistical indicators are total scores and factor scores before treatment and at 2, 4, 6 and 10 weeks after treatment.
Statistical analysis
The subjects with loss of data or with baseline information and evaluation results 2 weeks after treatment were included in the intention-to-treat analysis[53], that is, supplemented with the last observation carried forward. Data were analyzed using SPSS 13.0 software (SPSS, Chicago, IL, USA). Measurement data were expressed as mean ± SD. Intra-group comparisons were performed using one-way repeated measures analysis of variance, and pairwise comparisons using least significant difference test. Inter-group comparisons were performed using one-way analysis of variance or covariance followed by the least significant different test. P < 0.05 was considered statistically significant.
Footnotes
Funding: This study was supported by the National Science and Technology Support Program of China, No. 2006BAI12B05-2; the National Natural Science Foundation of China, No. 30672768; Key Discipline Construction Project of “211 Project” of Guangdong Province in China.
Conflicts of interest: None declared.
Copyedited by Murphy JS, Liang FX, Zhang L, Wang LM, Yang Y, Li CH, Song LP, Liu WJ, Zhao M
References
- [1].Röschke J, Wolf C, Müller MJ, et al. The benefit from whole body acupuncture in major depression. J Affect Disord. 2000;57(1-3):73–81. doi: 10.1016/s0165-0327(99)00061-0. [DOI] [PubMed] [Google Scholar]
- [2].Yeung AS, Ameral VE, Chuzi SE, et al. A pilot study of acupuncture augmentation therapy in antidepressant partial and non-responders with major depressive disorder. J Affect Disord. 2011;130(1-2):285–289. doi: 10.1016/j.jad.2010.07.025. [DOI] [PubMed] [Google Scholar]
- [3].Washington DC: American Psychiatric Press; 1994. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- [4].Zhang ZJ, Chen HY, Yip KC, et al. The effectiveness and safety of acupuncture therapy in depressive disorders: systematic review and meta-analysis. J Affect Disord. 2010;124(1-2):9–21. doi: 10.1016/j.jad.2009.07.005. [DOI] [PubMed] [Google Scholar]
- [5].Lecrubier Y. Widespread underrecognition and undertreatment of anxiety and mood disorders: results from 3 European studies. J Clin Psychiatry. 2007;68(Suppl 2):36–41. [PubMed] [Google Scholar]
- [6].Sartorius N, Baghai TC, Baldwin DS, et al. Antidepressant medications and other treatments of depressive disorders: a CINP Task Force report based on a review of evidence. Int J Neuropsychopharmacol. 2007;10(Suppl 1):S1–207. doi: 10.1017/S1461145707008255. [DOI] [PubMed] [Google Scholar]
- [7].Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6(4):278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- [8].Faries D, Herrera J, Rayamajhi J, et al. The responsiveness of the Hamilton Depression Rating Scale. J Psychiatr Res. 2000;34(1):3–10. doi: 10.1016/s0022-3956(99)00037-0. [DOI] [PubMed] [Google Scholar]
- [9].Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- [10].William Guy. Rockville: U.S. Department of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs; 1976. ECDEU Assessment Manual for Psychopharmacology. [Google Scholar]
- [11].Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- [12].Derogatis LR, Lipman RS, Rickels K, et al. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19(1):1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- [13].Pincus HA, Zarin DA, Tanielian TL, et al. Psychiatric patients and treatments in 1997: findings from the American Psychiatric Practice Research Network. Arch Gen Psychiatry. 1999;56(5):441–449. doi: 10.1001/archpsyc.56.5.441. [DOI] [PubMed] [Google Scholar]
- [14].Hasin DS, Goodwin RD, Stinson FS, et al. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- [15].Patten SB, Barbui C. Drug-induced depression: a systematic review to inform clinical practice. Psychother Psychosom. 2004;73(4):207–215. doi: 10.1159/000077739. [DOI] [PubMed] [Google Scholar]
- [16].Grunhaus L, Rabin D, Greden JF. Simultaneous panic and depressive disorder: response to antidepressant treatments. J Clin Psychiatry. 1986;47(1):4–7. [PubMed] [Google Scholar]
- [17].Ostacher MJ, Huffman J, Perlis R, editors. Cambridge: Cambridge University Press; 2005. Evidence-based Pharmacotherapy of Major Depressive Disorder. [Google Scholar]
- [18].Peretti S, Judge R, Hindmarch I. Safety and tolerability considerations: tricyclic antidepressants vs. selective serotonin reuptake inhibitors. Acta Psychiatr Scand Suppl. 2000;403:17–25. doi: 10.1111/j.1600-0447.2000.tb10944.x. [DOI] [PubMed] [Google Scholar]
- [19].Germann D, Ma G, Han F, et al. Paroxetine hydrochloride. Profiles Drug Subst Excip Relat Methodol. 2013;38:367–406. doi: 10.1016/B978-0-12-407691-4.00008-3. [DOI] [PubMed] [Google Scholar]
- [20].Ferguson JM. SSRI Antidepressant Medications: Adverse Effects and Tolerability. Prim Care Companion J Clin Psychiatry. 2001;3(1):22–27. doi: 10.4088/pcc.v03n0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Vander Watt G, Laugharne J, Janca A. Complementary and alternative medicine in the treatment of anxiety and depression. Curr Opin Psychiatry. 2008;21(1):37–42. doi: 10.1097/YCO.0b013e3282f2d814. [DOI] [PubMed] [Google Scholar]
- [22].Wu J, Yeung AS, Schnyer R, et al. Acupuncture for depression: a review of clinical applications. Can J Psychiatry. 2012;57(7):397–405. doi: 10.1177/070674371205700702. [DOI] [PubMed] [Google Scholar]
- [23].Schnyer RA, Flaws B. Boulder: Blue Poppy Press; 2007. Curing Depression Naturally: With Chinese Medicine. [Google Scholar]
- [24].Zhu ZH, Ding Z. Acupuncture and moxibustion treatment of anxiety neurosis and study on characteristics of acupoint selection. Zhongguo Zhen Jiu. 2008;28(7):545–548. [PubMed] [Google Scholar]
- [25].Huang QF. Exploration of the clinical regularity of acupuncture-moxibustion treatment for depression. Zhenjiu Tuina Yixue: Yingwen Ban. 2009;7(1):57–60. [Google Scholar]
- [26].Acar HV, Cuvaº O, Ceyhan A, et al. Acupuncture on yintang point decreases preoperative anxiety. J Altern Complement Med. 2013;19(5):420–424. doi: 10.1089/acm.2012.0494. [DOI] [PubMed] [Google Scholar]
- [27].You W, Shi YJ, Han YJ, et al. Effect of electroacupuncture of “Baihui” (GV 20)-“Yintang” (EX-HN 3) on the expression of glucocorticoid and glucocorticoid receptor mRNA of the chronic stress model rats. Zhen Ci Yan Jiu. 2010;35(4):261–266. [PubMed] [Google Scholar]
- [28].Zheng Y, Qu S, Wang N, et al. Post-stimulation effect of electroacupuncture at Yintang (EX-HN3) and GV20 on cerebral functional regions in healthy volunteers: a resting functional MRI study. Acupunct Med. 2012;30(4):307–315. doi: 10.1136/acupmed-2011-010123. [DOI] [PubMed] [Google Scholar]
- [29].Wang Y, Hu YP, Wang WC, et al. Clinical studies on treatment of earthquake-caused posttraumatic stress disorder using electroacupuncture. Evid Based Complement Alternat Med 2012. 2012 doi: 10.1155/2012/431279. 431279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Jiang JF, Xu L, Lin YH, et al. Anti-depression effect of acupuncture and moxibustion based on SSRIs medication. Zhongguo Zhen Jiu. 2012;32(3):219–223. [PubMed] [Google Scholar]
- [31].Sun H, Zhao H, Ma C, et al. Effects of Electroacupuncture on Depression and the Production of Glial Cell Line-Derived Neurotrophic Factor Compared with Fluoxetine: A Randomized Controlled Pilot Study. J Altern Complement Med. doi: 10.1089/acm.2011.0637. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Sun H, Zhao H, Zhang J, et al. Effect of acupuncture at Baihui (GV 20) and Zusanli (ST 36) on the level of serum inflammatory cytokines in patients with depression. Zhongguo Zhen Jiu. 2010;30(3):195–199. [PubMed] [Google Scholar]
- [33].Chen XH, Li Y, Kui Y, et al. Sleep disorder treated mainly with flying needling therapy: a clinical randomized controlled research. Zhongguo Zhen Jiu. 2013;33(2):97–100. [PubMed] [Google Scholar]
- [34].He QY, Liang J, Zhang Y, et al. Thirty-two subjects of vascular headache treated by acupuncture combined with Chinese herbal decoction. J Tradit Chin Med. 2009;29(4):253–257. doi: 10.1016/s0254-6272(09)60076-5. [DOI] [PubMed] [Google Scholar]
- [35].Pi M, Luo WS, Diao LH, et al. Electroacupuncture at Du channel and meridian of foot-Taiyang for hippocampal neurons in rats with depression. Neural Regen Res. 2007;2(6):365–368. [Google Scholar]
- [36].Guo LK, Zhang CX, Guo XF. Acupuncture combined with Chinese herbal medicine Plantain and Senna Granule in treatment of functional constipation: a randomized, controlled trial. Zhong Xi Yi Jie He Xue Bao. 2011;9(11):1206–1214. doi: 10.3736/jcim20111108. [DOI] [PubMed] [Google Scholar]
- [37].Peng DH, Fang YR. Clinical and pathogenesis researches on depressive disorder in China. Shanghai Jiaotong Daxue Xuebao: Yixue Ban. 2010;30(6):609–611. [Google Scholar]
- [38].LeDoux JE. Emotion circuits in the brain. Annu Rev Neurosci. 2000;23:155–184. doi: 10.1146/annurev.neuro.23.1.155. [DOI] [PubMed] [Google Scholar]
- [39].Spoont MR. Modulatory role of serotonin in neural information processing: implications for human psychopathology. Psychol Bull. 1992;112(2):330–350. doi: 10.1037/0033-2909.112.2.330. [DOI] [PubMed] [Google Scholar]
- [40].Watanabe A, Hasegawa S, Nishi K, et al. Chronic buspirone treatment normalizes regional serotonin synthesis in the olfactory bulbectomized rat brain: an autoradiographic study. Brain Res Bull. 2006;69(2):101–108. doi: 10.1016/j.brainresbull.2005.11.008. [DOI] [PubMed] [Google Scholar]
- [41].Vaidya VA, Siuciak JA, Du F, et al. Hippocampal mossy fiber sprouting induced by chronic electroconvulsive seizures. Neuroscience. 1999;89(1):157–166. doi: 10.1016/s0306-4522(98)00289-9. [DOI] [PubMed] [Google Scholar]
- [42].Malberg JE, Eisch AJ, Nestler EJ, et al. Chronic antidepressant treatment increases neurogenesis in adult rat hippocampus. J Neurosci. 2000;20(24):9104–9110. doi: 10.1523/JNEUROSCI.20-24-09104.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Sairanen M, O’Leary OF, Knuuttila JE, et al. Chronic antidepressant treatment selectively increases expression of plasticity-related proteins in the hippocampus and medial prefrontal cortex of the rat. Neuroscience. 2007;144(1):368–374. doi: 10.1016/j.neuroscience.2006.08.069. [DOI] [PubMed] [Google Scholar]
- [44].Brunello N, Mendlewicz J, Kasper S, et al. The role of noradrenaline and selective noradrenaline reuptake inhibition in depression. Eur Neuropsychopharmacol. 2002;12(5):461–475. doi: 10.1016/s0924-977x(02)00057-3. [DOI] [PubMed] [Google Scholar]
- [45].Nutt DJ. The neuropharmacology of serotonin and noradrenaline in depression. Int Clin Psychopharmacol. 2002;17(Suppl 1):S1–12. doi: 10.1097/00004850-200206001-00002. [DOI] [PubMed] [Google Scholar]
- [46].Zhang JB, Wang LL, Lv M, et al. Effects of acupuncture on monoamine neurotransmitter in frontal cortex of depressed model rats. Zhongguo Linchuang Kangfu. 2006;10(15):129–131. [Google Scholar]
- [47].Fu WB, Liu JH, Bai YF, et al. Effect of electroacupuncture on CREB-BDNF postreceptor signal transduction pathway in hippocampus of depression rats. Zhongguo Laonian Xue Zazhi. 2009;29(23):3038–3042. [Google Scholar]
- [48].Chen HD, Jin LQ, Lou R, et al. Effect of electroacupuncture and catgut embedding at point Baihui on behaviors and serum CORT and ACTH in a rat model of chronic stress-induced depression. Shanghai Zhenjiu Zazhi. 2010;29(4):244–247. [Google Scholar]
- [49].Geneva: WHO; 1993. World Health Organization Geneva. The ICD-10 Classification of Mental and Behavioural Disorders. [Google Scholar]
- [50].Leucht S, Fennema H, Engel R, et al. What does the HAMD mean? J Affect Disord. 2013;148(2-3):243–248. doi: 10.1016/j.jad.2012.12.001. [DOI] [PubMed] [Google Scholar]
- [51].Boyer WF, Feighner JP. An overview of paroxetine. J Clin Psychiatry. 1992;53 Suppl:3–6. [PubMed] [Google Scholar]
- [52].Beijing: WFAS; 2007. The World Federation of Acupuncture-Moxibustion Societies. GB 12346-90 Location of Points. [Google Scholar]
- [53].Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ. 1999;319(7211):670–674. doi: 10.1136/bmj.319.7211.670. [DOI] [PMC free article] [PubMed] [Google Scholar]


