Abstract
OBJECTIVE:
To investigate the factors associated with sensory and motor recovery after the repair of upper limb peripheral nerve injuries.
DATA SOURCES:
The online PubMed database was searched for English articles describing outcomes after the repair of median, ulnar, radial, and digital nerve injuries in humans with a publication date between 1 January 1990 and 16 February 2011.
STUDY SELECTION:
The following types of article were selected: (1) clinical trials describing the repair of median, ulnar, radial, and digital nerve injuries published in English; and (2) studies that reported sufficient patient information, including age, mechanism of injury, nerve injured, injury location, defect length, repair time, repair method, and repair materials. SPSS 13.0 software was used to perform univariate and multivariate logistic regression analyses and to investigate the patient and intervention factors associated with outcomes.
MAIN OUTCOME MEASURES:
Sensory function was assessed using the Mackinnon-Dellon scale and motor function was assessed using the manual muscle test. Satisfactory motor recovery was defined as grade M4 or M5, and satisfactory sensory recovery was defined as grade S3+ or S4.
RESULTS:
Seventy-one articles were included in this study. Univariate and multivariate logistic regression analyses showed that repair time, repair materials, and nerve injured were independent predictors of outcome after the repair of nerve injuries (P < 0.05), and that the nerve injured was the main factor affecting the rate of good to excellent recovery.
CONCLUSION:
Predictors of outcome after the repair of peripheral nerve injuries include age, gender, repair time, repair materials, nerve injured, defect length, and duration of follow-up.
Keywords: nerve regeneration, peripheral nerve injury, outcome predictors, nerve repair, upper limb, univariate analysis, prognosis, 863 Program, neural regeneration
Introduction
Peripheral nerve injuries may have important effects on a patient's life. The posttraumatic stress experienced after traumatic hand and forearm injuries results in a similar Impact of Event Scale score to that of survivors of the sinking of the cruise ship Estonia[1]. When upper limb motor and sensory function are altered, the patient's return to work may be jeopardized. Despite great improvements in treatment, recovery after the repair of peripheral nerve injuries is often disappointing and difficult to predict. For both patients and physicians, it is necessary to evaluate the likelihood of recovery based on patients and intervention factors, to enable realistic expectations and appropriate rehabilitation. There is increasing evidence that a number of factors are associated with the motor and sensory recovery after peripheral nerve injuries. For example, repair of nerve compression injuries has better outcomes than repair of nerve rupture injuries. Currently, the main factors thought to be associated with outcomes after the repair of peripheral nerve injuries are the age of the patient, mechanism of injury, nerve injured, injury location, defect length, repair time, repair method, operation technique, and repair materials. However, despite numerous studies of outcomes after the repair of peripheral nerve injuries, there is no agreement regarding the independent predictors of a good prognosis, and the dose-effect relationship of the predictors has not been quantified. Although some excellent reviews have been published[2], few of them performed meta-analyses[3,4], and they focused mainly on median and ulnar nerve injuries.
A relatively large number of studies have reported detailed individual patient data, enabling us to investigate the independent predictors of motor and sensory recovery. We performed a systematic literature search for clinical trials that described outcomes after the repair of upper limb peripheral nerve injuries, collected the relevant data from these studies, and used univariate and multivariate logistic regression analyses to analyze the relationships of various factors with outcomes after the repair of peripheral nerve injuries.
Data and Methods
Literature retrieval
A literature search was performed for English language articles in Medline, PubMed, Embase, Ovid, Google Scholar, and the Cochrane Library that described outcomes after the repair of median, ulnar, radial, and proper digital nerve injuries. Relevant articles were manually retrieved. The keywords used were “median nerve, ulnar nerve, radial nerve, upper extremity, fingers, nerve repair, or nerve regeneration”. The search was limited to studies on humans. The publication date ranged from 1 January 1990 to 16 February 2011.
Inclusion and exclusion criteria
Inclusion criteria
The inclusion criteria were: (1) clinical trials describing outcomes after the repair of median, ulnar, radial, and digital nerve injuries published in English; and (2) studies that reported sufficient patient information, including age, mechanism of injury, nerve injured, injury location, defect length, repair time, repair method, and repair materials. As few controlled clinical trials were identified, some case reports were included to increase the comprehensiveness of the literature review.
Exclusion criteria
Animal experiments, studies with repeated information, and studies with unrelated objectives were excluded. Articles that did not report whether M5 to M4 motor function or S4 to S3+ sensory function were achieved after repair were also excluded.
Quality evaluation
Two researchers independently searched the literature according to the inclusion and exclusion criteria, and read the titles and abstracts of the retrieved articles. After excluding papers that were obviously not relevant to the topic of this study, the full texts of the remaining articles were read to determine whether they met the criteria for inclusion. The results of the two researchers were compared. In cases of differences of opinion, agreement was achieved after discussion or a third researcher made a decision regarding inclusion of the article.
Main outcome measures
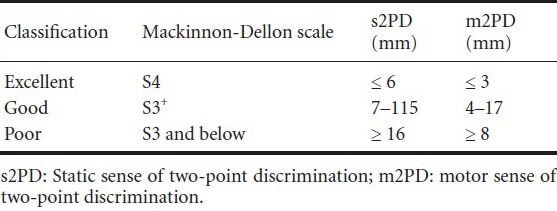
Sensory nerve function was graded using the Mackinnon-Dellon scale (Table 1), muscle strength was graded using the manual muscle test, and motor nerve function was evaluated according to the criteria of the Nerve Injuries Committee of the British Medical Research Council (Table 2)[4,5,6]. In this study, satisfactory motor recovery was defined as grade M4 or M5, and satisfactory sensory recovery was defined as grade S3+ or S4, which are the most common used criteria.
Table 1.
Classification of sensory recovery according to the Mackinnon-Dellon scale
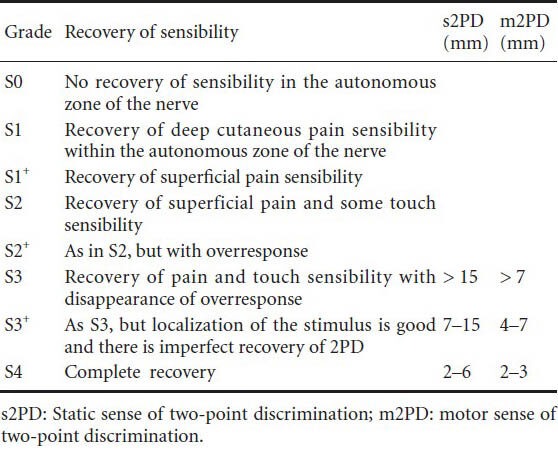
Table 2.
Classification of the degree of recovery according to the Mackinnon-Dellon scale
Statistical analysis
Data including age, gender, mechanism of injury, injury location, repair time, repair materials, nerve injured, and defect length were extracted from the included articles. Measurement data are represented as mean values, and count data as percentages. For binary variables, the odds ratio (OR) and 95% confidence interval (CI) were calculated. Factors associated with outcomes after the repair of nerve injures were determined by univariate and multivariate logistic regression analyses. All analyses were performed using SPSS 13.0 software (SPSS, Chicago, IL, USA).
Results
Data retrieval analysis
A total of 1,861 articles were initially retrieved. Of these, 126 were selected for review of the full text after primary screening, and 67 were judged to meet the criteria for inclusion in the present study[7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73].
Data retrieval results
Using a specially designed data collection table, one researcher collected and entered the data, and the other researcher verified the data. Missing information was obtained by contacting the corresponding author of the article by mail or telephone. The data for pure sensory nerve injuries and mixed nerve injuries were analyzed separately. Factors associated with outcomes after the repair of upper limb peripheral nerve injuries were examined (Tables 3–8).
Table 3.
Articles describing pure sensory nerve injuries
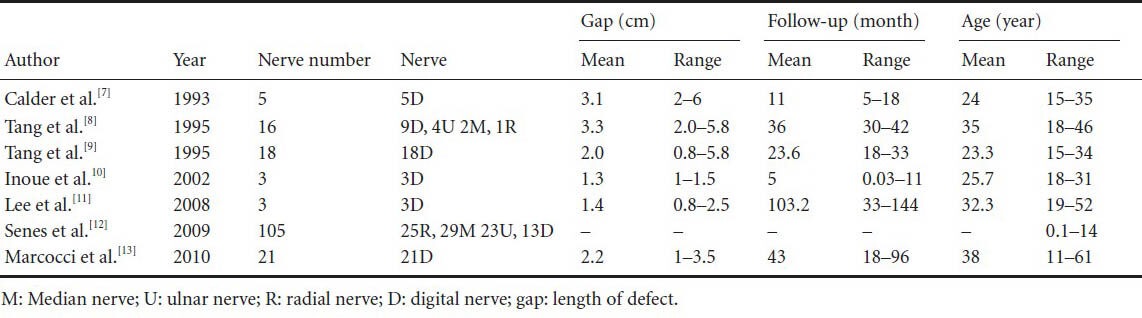
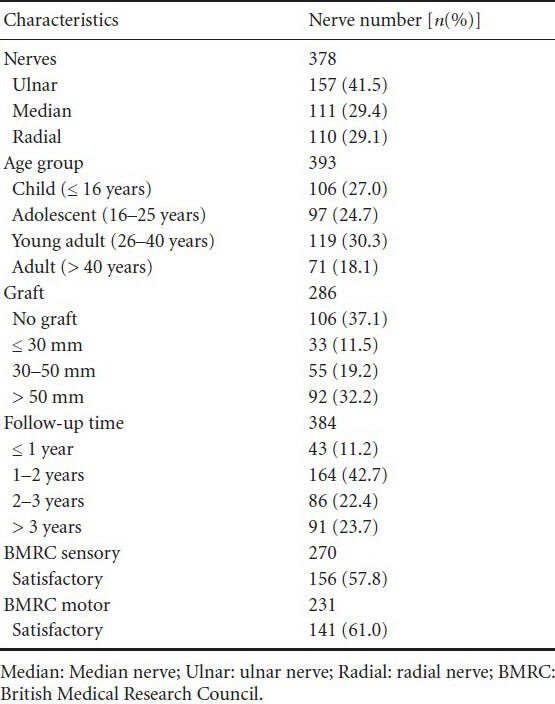
Table 8.
Rates [n1/n2, n1(%)] of good to excellent motor and sensory recovery after the repair of mixed nerve injuries according to the factors studied[14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73]
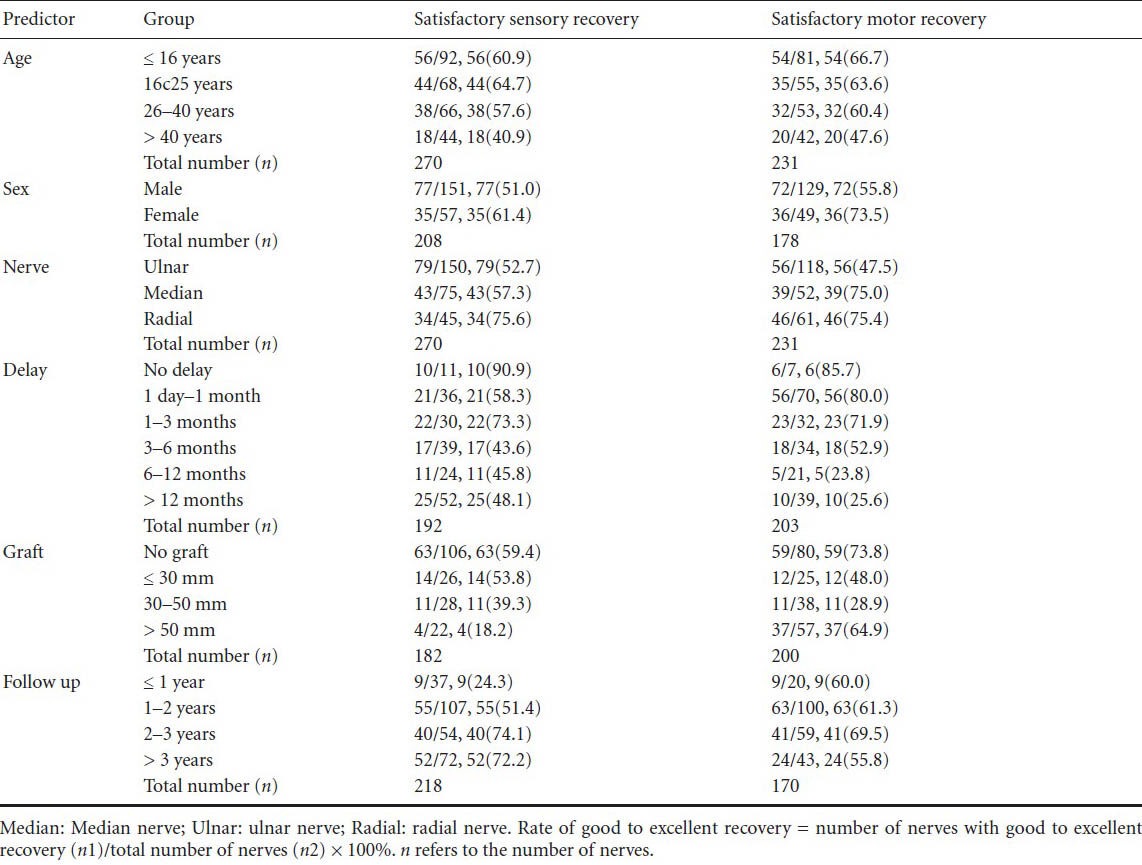
Table 4.
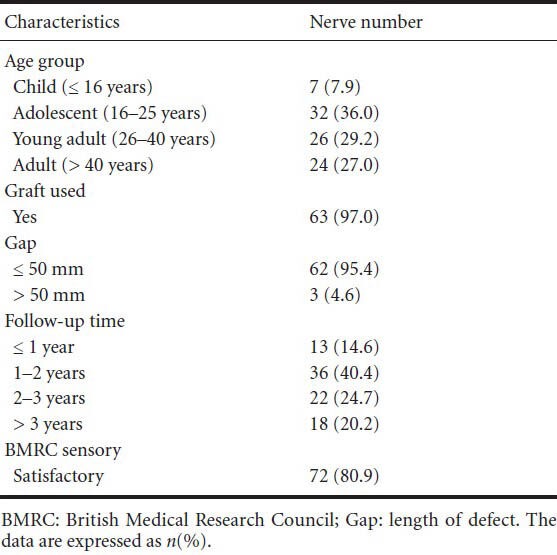
Table 5.
Rates of good to excellent recovery after the repair of pure sensory nerve injuries according to the factors studied[7,8,9,10,11,12,13]
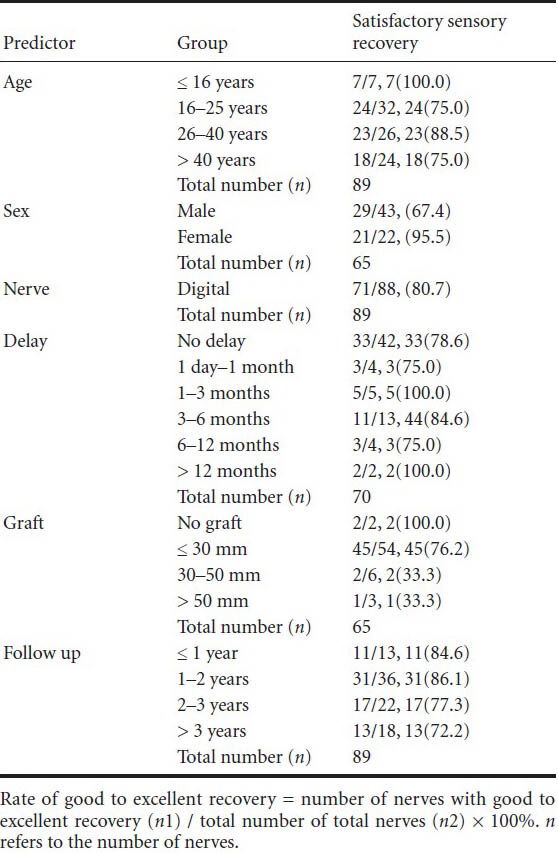
Table 6.
Articles describing mixed nerve injuries[14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73]
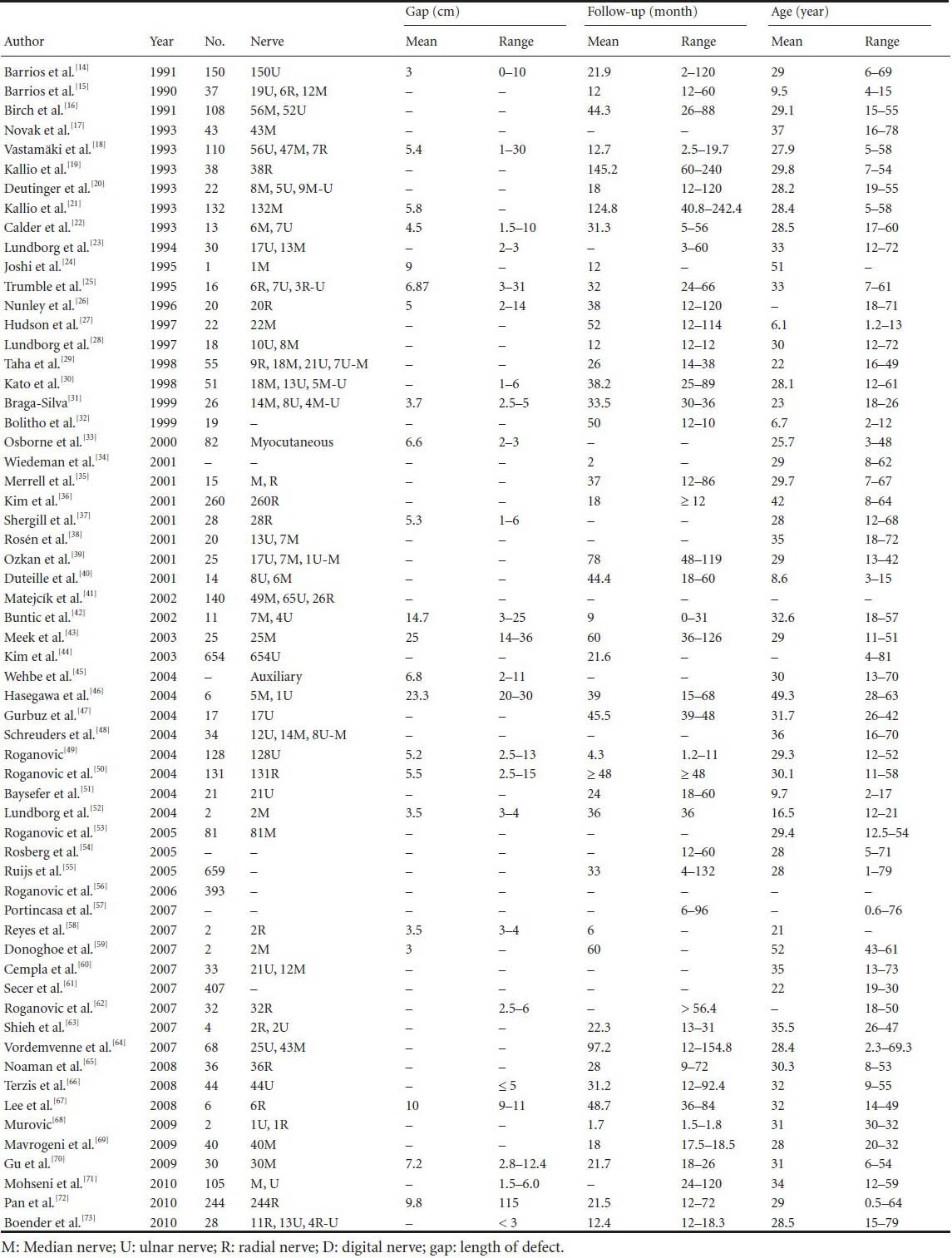
Table 7.
Summary of data extracted from articles describing mixed nerve injuries[14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73]
Factors affecting sensory recovery after the repair of pure sensory and mixed nerve injuries
Impact of patient and intervention factors on sensory recovery after the repair of pure sensory nerve injuries is shown in (Table 9).
Table 9.
Analysis of the impact of intervention factors on sensory recovery after the repair of pure sensory nerve injuries
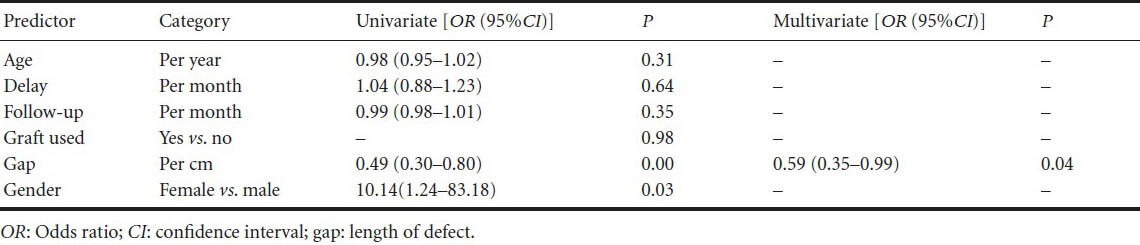
Univariate regression analyses for determining the factors associated with functional recovery after the repair of pure sensory nerve injuries
Univariate linear regression analyses showed that the length of the nerve defect (OR = 0.49, 95%CI: 0.30–0.80, P < 0.05) and gender (OR = 10.14, 95%CI: 1.24–83.18, P < 0.05) were significantly associated with good to excellent recovery after the repair of pure sensory nerve injuries. For a 1-cm increase in the defect length, the OR for good to excellent recovery was 0.49. For female gender compared with male gender, the OR for good to excellent recovery was 10.14.
Multivariate regression analysis for determining the independent predictors of functional recovery after the repair of pure sensory nerve injuries
Multivariate linear regression analysis showed that the length of the nerve defect was an independent predictor of good to excellent recovery after the repair of pure sensory nerve injuries (P = 0.04). For a 1-cm increase in the defect length, the OR for good to excellent recovery was 0.59.
Factors affecting functional recovery after the repair of mixed nerve injuries
Impact of intervention factors on functional recovery after the repair of mixed nerve injuries is shown in Tables 10, 11.
Table 10.
Analysis of factors associated with sensory recovery after the repair of mixed nerve injuries
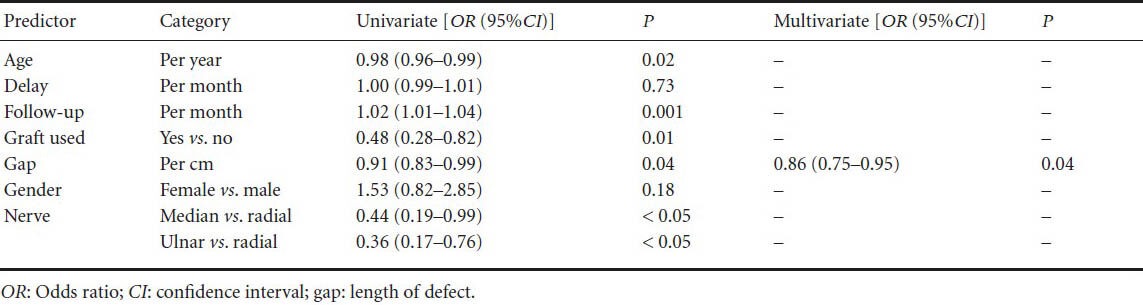
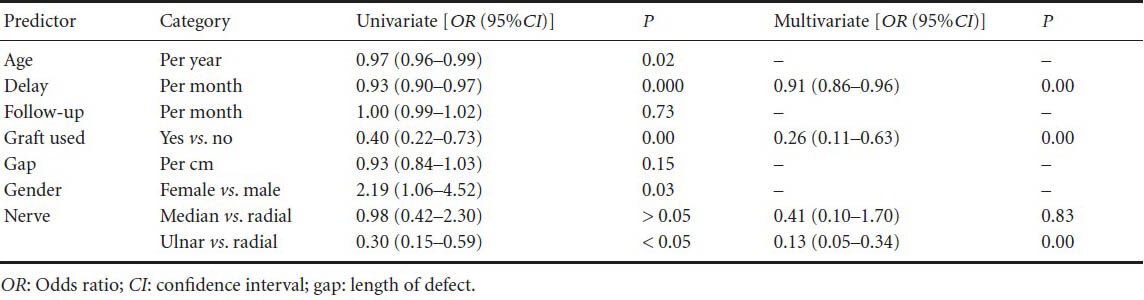
Table 11.
Analysis of factors associated with motor recovery after the repair of mixed nerve injuries
Univariate and multivariate conditional linear regression analyses for sensory recover
Univariate analyses with α = 0.05 showed that age, follow-up period, repair using a graft, defect length, and nerve injured were significantly associated with good to excellent sensory recovery after the repair of mixed nerve injuries (Table 10). For a 1-year increase in age, the OR for good to excellent recovery was 0.98 (95%CI: 0.96–0.99, P < 0.05). For a 1-month increase in the duration of follow-up, the OR for good to excellent recovery was 1.02 (95%CI: 1.01–1.04, P < 0.05). For repair using a graft versus direct repair using only sutures, the OR for good to excellent recovery was 0.48 (95%CI: 0.28–0.82, P < 0.05). For a 1-cm increase in the length of the defect, the OR for good to excellent recovery was 0.91 (95%CI: 0.83–0.99, P < 0.05). For repair of the median nerve versus the radial nerve, the OR for good to excellent recovery was 0.44 (95%CI: 0.19–0.99, P < 0.05); and for repair of the ulnar nerve versus the radial nerve, the OR for good to excellent recovery was 0.36 (95%CI: 0.17–0.76, P < 0.05).
Multivariate analysis showed that a shorter defect length was an independent predictor of good to excellent recovery (P < 0.05).
Univariate and multivariate conditional linear regression analyses for motor recovery
Univariate analyses with α = 0.05 showed that age, repair time, repair using a graft, gender, and nerve injured were significantly associated with good to excellent motor recovery after the repair of mixed nerve injuries (Table 11). For a 1-year increase in age, the OR for good to excellent recovery was 0.97 (95%CI: 0.96–0.99, P < 0.05). For a 1-month increase in the time from injury to repair, the OR for good to excellent recovery was 0.93 (95%CI: 0.90–0.97, P < 0.05). For repair using a graft versus direct repair using only sutures, the OR for good to excellent recovery was 0.40 (95%CI: 0.22–0.73, P < 0.05). For female gender versus male gender, the OR for good to excellent recovery was 2.19 (95%CI: 1.06–4.52, P < 0.05). For repair of the ulnar nerve versus repair of the radial nerve, the OR for good to excellent recovery was 0.30 (95%CI: 00.15–0.59, P < 0.05).
Multivariate analysis showed that repair time, repair materials, and nerve injured were independent predictors of good to excellent recovery. The nerve injured was the main factor predicting outcome. For repair of the ulnar nerve versus repair of the radial nerve, the OR for good to excellent recovery was 0.13 (95%CI: 0.05–0.34, P < 0.05), indicating that radial nerve repair had a better prognosis than ulnar nerve repair.
Discussion
In 1972, Brown reported that the factors associated with outcomes after the repair of nerve injuries were: (1) the nerve injured; (2) the age of the patient; (3) the level of the injury; (4) the length of the defect; (5) associated injuries; (6) surgical technique; and (7) the time of surgery. Evidence from subsequent clinical studies has mostly supported Brown's findings.
However, published reports vary widely in quality. The impact of any one factor can only be accurately determined when the impact of other factors has been controlled or eliminated. Unfortunately, isolation of one variable is difficult in clinical studies. We therefore conducted this literature review to clarify the impact of various factors on postoperative outcomes. We used the Mackinnon-Dellon scale to assess sensory function and the British Medical Research Council scale to assess motor function, which is the most widely accepted method of assessing outcomes after repair of peripheral nerve injuries. As the techniques of peripheral nerve injury repair have not changed much since the introduction of microsurgical techniques in the 1960s, operation techniques probably did not influence our results.
Age
Age has been reported to be associated with sensory recovery after the repair of nerve injuries[74,75], with younger patients having better outcomes than older patients. Lohmeyer et al.[76] conducted a postoperative follow-up study of 90 patients (mean age 41 years, age range 4–88 years) with 101 upper limb nerve injuries. They found significant differences in outcomes between patients aged < 20 years and those aged > 20 years (P = 0.01), and reported that nerve regeneration was poorest in patients aged > 50 years. In the present study, univariate analyses of factors affecting outcomes after the repair of mixed nerve injuries showed that a 1-year increase in age had an OR for good to excellent sensory recovery of 0.98, and an OR for good to excellent motor recovery of 0.97. This may be because children have a stronger regenerative capacity, require a shorter length of nerve regeneration because of their relatively short limbs, have a shortened duration of re-innervation because of axon growth, and have less atrophy. Functional recovery was reported to be significantly poorer in older patients, who have weaker regenerative and compensatory capacity. The relatively poor nutritional status and local circulation also reduce the capacity for nerve regeneration in adults[77]. Segalman et al.[78] considered that the better outcomes in younger patients resulted from better axonal regeneration and greater adaptability. Older patients may have fewer receptors because of age-related changes of the central nervous system, resulting in younger patients having better sensitivity than older patients[79].
Gender
In the present study, univariate analyses showed that female gender had an OR for good to excellent recovery after the repair of pure sensory nerve injuries of 10.14 compared with male gender, but had an OR for good to excellent recovery of motor function after the repair of mixed nerve injuries of 2.19 compared with male gender. No previously published studies have reported the impact of gender on functional recovery after the repair of peripheral nerve injuries. Gender may have an impact on nerve regeneration, but no animal experiments or clinical studies have examined this possibility, and our findings may reflect other factors that are related to gender. This study did not analyze data such as the nature of the injury and postoperative adjuvant treatment, and these factors may differ according to gender. For example, most women perform only light manual labor, and may therefore have milder injuries then men. Women may also have better compliance with postoperative adjuvant treatments such as neurotropic drugs and functional exercises than men. Further analysis should be performed to examine these possibilities. However, the results of this study indicate that women have a higher likelihood of good to excellent postoperative rehabilitation than men after the repair of peripheral nerve injuries.
Injured nerve
Outcomes differ after the repair of injuries to different nerves even if the type of injury, extent of injury, location of injury, and method of repair are the same. Outcomes after repair are relatively poor for the median and ulnar nerves compared with the radial nerve, and motor recovery is better after repair of median nerve injuries than after repair of ulnar nerve injuries[38,80,81]. In the present study, median and ulnar nerve sensory recovery had ORs for good to excellent sensory recovery of 0.44 and 0.36, respectively, compared with radial nerve sensory recovery; and the ulnar nerve had an OR for good to excellent motor recovery of 0.30 compared with radial nerve motor recovery. Murovic et al.[68] reported that the rates of good to excellent results after the repair of radial, median, and ulnar nerve injuries were 86%, 75%, and 56%, respectively. Ruijs et al.[4] reported that the rate of motor recovery was 71% lower after the repair of ulnar nerve injuries than median nerve injuries. For the same degree of injury, the outcomes after repair are generally best for the radial nerve, followed by the median nerve and then the ulnar nerve. Outcomes after the repair of radial nerve injuries are relatively good because the radial nerve has a larger number of motor nerve fibers and a shorter distance for nerve regeneration than the median and ulnar nerves. Outcomes after the repair of ulnar nerve injuries are the worst because the ulnar nerve innervates a small volume of muscle with a small muscle fiber size. After loss of innervation, the muscle fibers rapidly degenerate and atrophy. The motor and sensory parts of the ulnar nerve exchange fibers with one another and descend in a mixed pattern, resulting in a low apposition rate after interruption. Recovery is therefore better after repair of a pure sensory nerve injury than after repair of a mixed nerve injury. The results of the present study show that sensory recovery was better than motor recovery after the repair of mixed nerve injuries, and that a 1-year increase in age had an OR for good to excellent recovery of 0.97.
Repair time
The results of the present study show that outcomes after the repair of nerve injuries were associated with the time from the injury to the repair. This confirms the results of previous studies that reported an unfavorable prognosis after a delay in repair of more than 6 or 12 months[81]. Earlier repair is associated with better outcomes. If one-stage repair of the injured nerve is possible, new nerve fibers can quickly grow into the distal end of the nerve. If the nerve is not repaired for a long time after the injury, scarring may occur in the distal end of the nerve or the ingrowth of new nerve fibers may be obstructed by collapse of the endoneurial sheaths. Even if there is new nerve fiber ingrowth, the original morphology and function cannot be restored[82]. Moreover, long-term loss of innervation results in degeneration and atrophy of the muscle fibers and the terminal receptors in the skin. Outcomes after repair of mixed nerve injuries are worse after a greater delay. In the present study, univariate analyses showed that a 1-month increase in the time from injury to repair had an OR for good to excellent motor recovery of 0.93. It has been reported that a delay in repair of 6 days results in a 1% loss of function, and that the speed of nerve regeneration is about 1 mm/day[83]. Outcomes are poorer when the repair is delayed by more than 1 year because muscle atrophy becomes irreversible at 1.5–2 years after the loss of innervation. Barrios et al.[15] suggested that nerve repair should be performed within 3 months of the injury, and that the time from injury to repair should not exceed 1 year.
Length of the nerve graft
Sunderland et al.[84] showed that tension on sutured nerves may result in circulatory disturbance that affects nerve fiber regeneration and functional recovery. If the nerve defect is > 2 cm after repositioning of the joints, the defect should be repaired using a nerve transplant. However, the length of the transplanted nerve also affects functional recovery, and outcomes are better after short-segment nerve grafting than after long-segment nerve grafting. In the present study, univariate analyses showed that a 1-cm increase in the length of the nerve repair material for pure sensory nerve injuries had an OR for good to excellent sensory recovery of 0.49. For the repair of mixed nerve injuries, repair using a nerve graft had an OR for good to excellent motor recovery of 0.4 compared with direct repair using sutures, and a 1-cm increase in graft length had an OR for good to excellent sensory recovery of 0.91. Multivariate analysis showed that graft length was an independent predictor of outcome. A 1-cm increase in the graft length had an OR for good to excellent recovery after the repair of pure sensory nerve injuries of 0.59. Haase et al.[85] reported that outcomes were optimal when the length of autologous nerve graft used for repair was < 5 cm.
Duration of follow-up
Peripheral nerves regenerate slowly, and functional improvement may continue for a long time. The timing of outcome evaluation after the repair of peripheral nerve injuries is therefore very important. For a 1-month increase in the duration of the follow-up period after the repair of mixed nerve injuries, the OR for sensory recovery was 1.02. However, there is no consensus regarding the most appropriate duration of follow-up for the assessment of maximum recovery after the repair of peripheral nerve injuries. Ruijs et al.[4] reported that significant functional recovery could be assessed at 3 years after the repair of median and ulnar nerve injuries. However, Rosén and Lundborg[38] considered that functional recovery should be assessed after 5 years. Functional recovery generally improves with an increased duration of follow-up. If the duration of follow-up is too short, the final recovery of function cannot be assessed. A minimum follow-up duration of 1 to 2 years is generally required, and the time of the last functional evaluation should be 2 to 3 years after repair in children and adolescents and 5 years after repair in adults.
Other factors predicting recovery
It is known that the experience of the surgeon has an impact on functional recovery after the repair of nerve injuries, but it was not possible to take this factor into consideration in the present study. Not all variables were known for every patient, such as the nature and extent of injury, injury site, materials used for repair, adjuvant treatment, and local and general conditions of the patient; and it was therefore not possible to include all patients in the data analysis. In a meta-analysis, it is preferable to consider all the factors that may affect outcomes, but few reports provided all the required information. Therefore, only the factors described above were analyzed in this study.
Nature and extent of injury
The soft tissue injuries surrounding the nerve injuries differed among patients. High-energy blunt trauma was often associated with serious bone and soft tissue injuries. Outcomes may be poor after the repair of nerve injuries if the tissue bed is in poor condition. In extensive crush injuries, there may be a significant area of damaged tissue, resulting in poor local perfusion after the debridement of dead tissue. Murovic[68] studied 1,837 patients with upper extremity nerve injuries and found that the rate of good to excellent results after knife injuries was 91% after the repair of median and radial nerve injuries, and 73% after the repair of ulnar nerve injuries. Secer et al.[86] studied 455 patients with gunshot or shrapnel injuries to the ulnar nerve and found that the rate of good to excellent results was < 32%. Crush injuries cause a relatively extensive area of tissue damage, resulting in poor outcomes after the repair of nerve injuries.
Injury site
When the injury is close to the proximal end of the nerve, functional recovery after nerve repair is poor. If the injury is close to the distal end, functional recovery after nerve repair is good. There are a number of possible reasons for this. (1) If the location of the injury is too close to the neurons, massive neuronal necrosis may occur, which may seriously affect functional recovery. (2) Functional recovery depends on regeneration of nerve fibers from the location of the injury to the nerve ending. More proximal injuries therefore take a longer time to regenerate. Muscle regeneration occurs after an extended period of denervation, resulting in increased difficulty in restoring function after re-innervation. Degenerative changes in the skin receptors result in even poorer postoperative functional recovery[87]. (3) The proximal segment of the nerve tract is often composed of mixed nerve bundles, and the risk of crossover growth between sensory and motor nerve fibers is therefore high. At the distal end, the nerve has already divided into sensory and motor tracts, and perineural suturing can be performed between the ends of the motor and sensory tracts to achieve satisfactory functional recovery. Secer et al.[86] studied 455 patients with ulnar nerve injuries and found that the rate of good to excellent results was 15.06% in high-level injuries, 29.60% in mid-level injuries, and 49.68% in low-level injuries.
Repair materials
Autologous nerve tissue is the most commonly used material for nerve grafting, and is generally considered to result in good outcomes. However, no large study has compared outcomes after the use of different repair materials. Other materials used for the repair of nerve injuries include non-degradable silicone tubes, polytetrafluoroethylene pipes, polyethylene pipes, nerve conduits made of biodegradable artificial materials including polyglycolic acid, poly(DL-lactide-epsilon-caprolactone) and collagen, and vein, skeletal muscle, and acellular nerve allografts[88,89,90]. Previous studies have reported various efficacies for these materials. Reported good neural recovery rates include 86% using polyglycolic acid (mean length 1.7 cm, range 0.5–3.0 cm; Mackinnon and Dellon[91], 1990); 76.5% using Neurotube (range 1.0–4.0 cm; Battiston et al.[92], 2005); 88% using NeuraGen (range 1.0–2.0 cm; Bushnell et al.[93], 2008); and 75% using NeuraGen (average 3.8 cm; range1.2–6.6 mm; Lohmeyer et al.[94], 2009). We previously reported good neural recovery rates in 65.28% of cases using human acellular nerve grafts[5,6], which is somewhat lower than in other studies. However, these studies had smaller sample sizes and used different statistical methods than the present study, making direct comparisons difficult. Although non-inferiority was not proven by examination of static sense of two-point discrimination examination, we concluded that use of human acellular nerve grafts for the repair of nerve injuries results in good or excellent functional recovery in 51.98–78.93% of cases. The reported outcomes after repair of nerve injuries using different materials vary greatly, and further studies analyzing these outcomes are needed.
Adjuvant therapy
Currently, drugs used to promote nerve regeneration after the repair of peripheral nerve injuries include the vitamin B family (vitamin B1, B6, and B12)[95], cytidine diphosphate choline, dibazol, and nerve growth factor[96]. Postoperative physical therapy[97], hyperbaric oxygen therapy[98], and functional exercise[41] also contribute to nerve regeneration and functional recovery. However, the therapeutic effectiveness of these methods after the repair of peripheral nerve injuries has not yet been determined.
Local and general conditions
Poor local wound conditions such as infection, excessive scar tissue, and a poor soft tissue bed also prevent nerve regeneration after repair. Prpa et al.[99] considered that the soft tissue bed plays an important role in nerve graft revascularization, and suggested that neovascularization from the soft tissue bed is the primary mechanism underlying the restoration of blood flow in such grafts. Recovery of neurological function is also related to nutritional status and mental state. Enhancement or improvement of the patient's nutritional status promotes nerve regeneration. Furthermore, the surgeon's experience with microsuturing techniques affects the recovery of nerve function. Factors associated with outcomes after the repair of peripheral nerve injuries that are under the control of the surgeon include the timing of nerve repair, materials used for nerve repair, postoperative medications, and rehabilitation.
Limitations
There were some limitations to our study. First, there are few randomized controlled trials describing functional recovery after different nerve repair techniques, which might have contributed to the heterogeneity in the analysis process. Such heterogeneity was dealt with by either choosing a good model for calculation, or by excluding or combining some studies. Second, modifications of repair techniques may result in different individual outcomes, but should not change the results of the overall meta-analysis. Third, for studies that did not directly describe functional recovery after repair or detailed descriptions of outcomes after the repair of median and ulnar nerve injuries, an effort was made to extract data from the content of the article or the article was excluded from this study. Fourth, most of the included studies had a small sample size, lacked statistical analysis, or had a low level of evidence (level III or IV). Fifth, this paper is limited to data collected 2 years ago. Finally, we excluded articles that did not present individual data, which may have caused selection bias if other predictors of recovery were present in the excluded patients. It was not possible to include only studies with a large sample size or high level of evidence as this would have made our sample size too small. The sample size was very small in some included studies, such as those by Lee and Shieh[11] (3 cases); Calder and McAllister[7] (5 cases); Inoue et al.[10] (3 cases); and Reyes et al.[58] (2 cases). Inclusion of these cases may therefore have resulted in selection bias. It would have been preferable to include only randomized controlled trials in this analysis. However, our literature search only identified a few randomized controlled trials, and we therefore performed this alternative type of systematic analysis. Although this research combines information from trials with very different patient characteristics and designs, it still provides useful information regarding the factors associated with outcomes after the repair of peripheral nerve injuries. Further studies are required to focus on factors such as the nerve injured. Despite these limitations, useful conclusions can be drawn from the present study.
Conclusion
Factors that predict outcomes after the repair of peripheral nerve injuries in the upper limb include age, gender, repair time, repair materials, defect length, duration of follow-up, and nerve injured. The impact of these predictors on the outcome varies. Functional recovery of peripheral nerve injuries is multifaceted, and different factors may affect outcome in different patients.
Acknowledgments:
We would like to thank Qi J, Xiao LB, Hu J and Li ZY (Department of Microsurgery, the First Affiliated Hospital of Sun Yat-sen University, China) for their excellent assistance.
Footnotes
Funding: This study was supported by the National High-Technology Research and Development Program of China (863 Program), No. 2012A A020507; 985 Program of Sun Yat-sen University, No. 90035-3283312; Specialized Research Fund for the Doctoral Program of Higher Education, No. 20120171120075; and Doctoral Start-up Project of the Natural Science Foundation of Guangdong Province, No. S201204006336.
Conflicts of interest: None declared.
Peer review: This study showed that the factors affecting functional recovery of peripheral nerve injury are multifaceted, as for a certain patient, one or more factors may affect the prognosis. Through the analysis on the injured nerve, we determined the effect of various factors on sensory and motor function prognosis in the upper extremity nerve and established a dose-effect relationship, which can be applied to estimate the prognosis of upper extremity nerve injury.
Copyedited by Elgin M, Chen SL, Wang PJ, Wang J, Yang Y, Li CH, Song LP, Zhao M
References
- [1].Jaquet J, Kalmijn S, Kuypers P, et al. Early psychological stress after forearm nerve injuries: a predictor for long term functional outcome and return to productivity. Ann Plast Surg. 2002;49(1):82–90. doi: 10.1097/00000637-200207000-00013. [DOI] [PubMed] [Google Scholar]
- [2].Vanderhooft E. Functional outcomes of nerve grafts for the upper and lower extremities. Hand Clin. 2000;16(1):93–104. [PubMed] [Google Scholar]
- [3].Yang M, Rawson JL, Zhang EW, et al. Comparisons of outcomes from repair of median nerve and ulnar nerve defect with nerve graft and tubulization: a meta-analysis. J Reconstr Microsurg. 2011;27(8):451–460. doi: 10.1055/s-0031-1281526. [DOI] [PubMed] [Google Scholar]
- [4].Ruijs AC, Jaquet JB, Kalmijn S, et al. Median and ulnar nerve injuries:a meta-analysis of predictors of motor and sensory recovery after modern microsurgical nerve repair. Plast Reconstr Surg. 2005;116(2):484–494. doi: 10.1097/01.prs.0000172896.86594.07. [DOI] [PubMed] [Google Scholar]
- [5].He B, Zhu Q, Chai Y, et al. Safety and efficacy evaluation of a human acellular nerve graft as a digital nerve scaffold: a prospective, multicentre controlled clinical trial. J Tissue Eng Regen Med. 2013 doi: 10.1002/term.1707. [DOI] [PubMed] [Google Scholar]
- [6].He B, Zhu QT, Chai YM, et al. Outcomes with the use of human acellular nerve graft for repair of digital nerve defects: a prospective, multicenter, controlled clinical trial. J Tissue Eng Regen Med. 2012;6(Suppl 1):76. doi: 10.1002/term.1707. [DOI] [PubMed] [Google Scholar]
- [7].Calder JS, McAllister RM. Interpreting the results of unilateral digital nerve repair. J Hand Surg Br. 1993;18(6):797–799. doi: 10.1016/0266-7681(93)90248-e. [DOI] [PubMed] [Google Scholar]
- [8].Tang JB. Vein conduits with interposition of nerve tissue for peripheral nerve defects. J Reconstr Microsurg. 1995;11(1):21–26. doi: 10.1055/s-2007-1006506. [DOI] [PubMed] [Google Scholar]
- [9].Tang JB, Shi D, Zhou H. Vein conduits for repair of nerves with a prolonged gap or in unfavourable conditions: an analysis of three failed cases. Microsurgery. 1995;16(3):133–137. doi: 10.1002/micr.1920160303. [DOI] [PubMed] [Google Scholar]
- [10].Inoue S, Ogino T, Tsutida H. Digital nerve grafting using the terminal branch of posterior interosseous nerve: a report of three cases. Hand Surg. 2002;7(2):305–307. doi: 10.1142/s0218810402001035. [DOI] [PubMed] [Google Scholar]
- [11].Lee YH, Shieh SJ. Secondary nerve reconstruction using vein conduit grafts for neglected digital nerve injuries. Microsurgery. 2008;28(6):436–440. doi: 10.1002/micr.20517. [DOI] [PubMed] [Google Scholar]
- [12].Senes FM, Campus R, Becchetti F, et al. Upper limb nerve injuries in developmental age. Microsurgery. 2009;29(7):529–535. doi: 10.1002/micr.20660. [DOI] [PubMed] [Google Scholar]
- [13].Marcoccio I, Vigasio A. Muscle-in-vein nerve guide for secondary reconstruction in digital nerve lesions. J Hand Surg Am. 2010;35(9):1418–1426. doi: 10.1016/j.jhsa.2010.05.019. [DOI] [PubMed] [Google Scholar]
- [14].Barrios C, de Pablos J. Surgical management of nerve injuries of the upper extremity in children: 15-year survey. J Pediatr Orthop. 1991;11(5):641–645. [PubMed] [Google Scholar]
- [15].Barrios C, Amillo S, de Pablos J, et al. Secondary repair of ulnar nerve injury: 44 cases followed for 2 years. Acta Orthop Scand. 1990;61(1):46–49. doi: 10.3109/17453679008993065. [DOI] [PubMed] [Google Scholar]
- [16].Birch R, Raji AR. Repair of median and ulnar nerves. Primary suture is best. J Bone Joint Surg Br. 1991;73(1):154–157. doi: 10.1302/0301-620X.73B1.1991753. [DOI] [PubMed] [Google Scholar]
- [17].Novak CB, Mackinnon SE, Kelly L. Correlation of two-point discrimination and hand function following median nerve injury. Ann Plast Surg. 1993;31(6):495–498. doi: 10.1097/00000637-199312000-00003. [DOI] [PubMed] [Google Scholar]
- [18].Vastamäki M, Kallio PK, Solonen KA. The results of secondary microsurgical repair of ulnar nerve injury. J Hand Surg Br. 1993;18(3):323–326. doi: 10.1016/0266-7681(93)90053-i. [DOI] [PubMed] [Google Scholar]
- [19].Kallio PK, Vastamäki M, Solonen KA. The results of secondary microsurgical repair of radial nerve in 33 patients. J Hand Surg Br. 1993;18(3):320–322. doi: 10.1016/0266-7681(93)90052-h. [DOI] [PubMed] [Google Scholar]
- [20].Deutinger M, Girsch W, Burggasser G, et al. Peripheral nerve repair in the hand with and without motor sensory differentiation. J Hand Surg Am. 1993;18(3):426–432. doi: 10.1016/0363-5023(93)90085-H. [DOI] [PubMed] [Google Scholar]
- [21].Kallio PK, Vastamäki M. An analysis of the results of late reconstruction of 132 median nerves. J Hand Surg Br. 1993;18(1):97–105. doi: 10.1016/0266-7681(93)90205-t. [DOI] [PubMed] [Google Scholar]
- [22].Calder JS, Norris RW. Repair of mixed peripheral nerves using muscle autografts: a preliminary communication. Br J Plast Surg. 1993;46(7):557–564. doi: 10.1016/0007-1226(93)90105-k. [DOI] [PubMed] [Google Scholar]
- [23].Lundborg G, Rosen B, Abrahamson SO, et al. Tubular repair of the median nerve in the human forearm. Preliminary findings. J Hand Surg. 1994;19(3):273–276. doi: 10.1016/0266-7681(94)90068-x. [DOI] [PubMed] [Google Scholar]
- [24].Joshi N, Mir X, Busquets R, et al. Contralateral median nerve autograft. Acta Orthop Belg. 1995;61(4):323–326. [PubMed] [Google Scholar]
- [25].Trumble TE, Kahn U, Vanderhooft E, et al. A technique to quantitate motor recovery following nerve grafting. J Hand Surg Am. 1995;20(3):367–372. doi: 10.1016/S0363-5023(05)80089-9. [DOI] [PubMed] [Google Scholar]
- [26].Nunley JA, Saies AD, Sandow MJ, et al. Results of interfascicular nerve grafting for radial nerve lesions. Microsurgery. 1996;17(8):431–437. doi: 10.1002/(SICI)1098-2752(1996)17:8<431::AID-MICR3>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- [27].Hudson DA, Bolitho DG, Hodgetts K. Primary epineural repair of the median nerve in children. J Hand Surg Br. 1997;22(1):54–56. doi: 10.1016/s0266-7681(97)80017-4. [DOI] [PubMed] [Google Scholar]
- [28].Lundborg G, Rosén B, Dahlin L, et al. Tubular versus conventional repair of median and ulnar nerves in the human forearm: early results from a prospective, randomized, clinical study. J Hand Surg Am. 1997;22(1):99–106. doi: 10.1016/S0363-5023(05)80188-1. [DOI] [PubMed] [Google Scholar]
- [29].Taha A, Taha J. Results of suture of the radial, median, and ulnar nerves after missile injury below the axilla. J Trauma. 1998;45(2):335–339. doi: 10.1097/00005373-199808000-00021. [DOI] [PubMed] [Google Scholar]
- [30].Kato H, Minami A, Kobayashi M, et al. Functional results of low median and ulnar nerve repair with intraneural fascicular dissection and electrical fascicular orientation. J Hand Surg Am. 1998;23(3):471–482. doi: 10.1016/S0363-5023(05)80465-4. [DOI] [PubMed] [Google Scholar]
- [31].Braga-Silva J. The use of silicone tubing in the late repair of the median and ulnar nerves in the forearm. J Hand Surg Br. 1999;24(6):703–706. doi: 10.1054/jhsb.1999.0276. [DOI] [PubMed] [Google Scholar]
- [32].Bolitho DG, Boustred M, Hudson DA, et al. Primary epineural repair of the ulnar nerve in children. J Hand Surg Am. 1999;24(1):16–20. doi: 10.1053/jhsu.1999.jhsu25a0016. [DOI] [PubMed] [Google Scholar]
- [33].Osborne AW, Birch RM, Munshi P, et al. The musculocutaneous nerve. J Bone Joint Surg Br. 2000;82(8):1140–1142. doi: 10.1302/0301-620x.82b8.10791. [DOI] [PubMed] [Google Scholar]
- [34].Wiedeman JE, Zierold D, Klink BK. Machete injuries in Haiti. Mil Med. 2001;166(11):1023–1025. [PubMed] [Google Scholar]
- [35].Merrell GA, Barrie KA, Katz DL, et al. Results of nerve transfer techniques for restoration of shoulder and elbow function in the context of a meta-analysis of the English literature. J Hand Surg Am. 2001;26(2):303–314. doi: 10.1053/jhsu.2001.21518. [DOI] [PubMed] [Google Scholar]
- [36].Kim DH, Kam AC, Chandika P, et al. Surgical management and outcome in patients with radial nerve lesions. J Neurosurg. 2001;95(4):573–583. doi: 10.3171/jns.2001.95.4.0573. [DOI] [PubMed] [Google Scholar]
- [37].Shergill G, Bonney G, Munshi P, et al. The radial and posterior interosseous nerves. Results of 260 repairs. J Bone Joint Surg Br. 2001;83(5):646–649. doi: 10.1302/0301-620x.83b5.11312. [DOI] [PubMed] [Google Scholar]
- [38].Rosén B, Lundborg G. The long term recovery curve in adults after median or ulnar nerve repair: a reference interval. J Hand Surg Br. 2001;26(3):196–200. doi: 10.1054/jhsb.2001.0567. [DOI] [PubMed] [Google Scholar]
- [39].Ozkan T, Ozer K, Gülgönen A. Restoration of sensibility in irreparable ulnar and median nerve lesions with use of sensory nerve transfer: long-term follow-up of 20 cases. J Hand Surg Am. 2001;26(1):44–51. doi: 10.1053/jhsu.2001.20156. [DOI] [PubMed] [Google Scholar]
- [40].Duteille F, Petry D, Dautel G, et al. A comparison between clinical results and electromyographic analysis after median or ulnar nerve injuries in children's wrists. Ann Plast Surg. 2001;46(4):382–386. doi: 10.1097/00000637-200104000-00005. [DOI] [PubMed] [Google Scholar]
- [41].Matejcík V. Surgical treatment of peripheral nerve injuries in upper extremities. Acta Chir Plast. 2002;44(3):80–85. [PubMed] [Google Scholar]
- [42].Buntic RF, Buncke HJ, Kind GM, et al. The harvest and clinical application of the superficial peroneal sensory nerve for grafting motor and sensory nerve defects. Plast Reconstr Surg. 2002;109(1):145–151. doi: 10.1097/00006534-200201000-00024. [DOI] [PubMed] [Google Scholar]
- [43].Meek MF, Coert JH, Wong KH. Recovery of touch after median nerve lesion and subsequent repair. Microsurgery. 2003;23(1):2–5. doi: 10.1002/micr.10087. [DOI] [PubMed] [Google Scholar]
- [44].Kim DH, Han K, Tiel RL, et al. Surgical outcomes of 654 ulnar nerve lesions. J Neurosurg. 2003;98(5):993–1004. doi: 10.3171/jns.2003.98.5.0993. [DOI] [PubMed] [Google Scholar]
- [45].Wehbe J, Maalouf G, Habanbo J, et al. Surgical treatment of traumatic lesions of the axillary nerve. A retrospective study of 33 cases. Acta Orthop Belg. 2004;70(1):11–18. [PubMed] [Google Scholar]
- [46].Hasegawa T, Nakamura S, Manabe T, et al. Vascularized nerve grafts for the treatment of large nerve gap after severe trauma to an upper extremity. Arch Orthop Trauma Surg. 2004;124(3):209–213. doi: 10.1007/s00402-003-0617-6. [DOI] [PubMed] [Google Scholar]
- [47].Gurbuz H, Aktas S, Calpur OU. Clinical evaluation of ulnar nerve repair at wrist level. Arch Orthop Trauma Surg. 2004;124(1):49–51. doi: 10.1007/s00402-003-0587-8. [DOI] [PubMed] [Google Scholar]
- [48].Schreuders TA, Roebroeck ME, Jaquet JB, et al. Long-term outcome of muscle strength in ulnar and median nerve injury: comparing manual muscle strength testing, grip and pinch strength dynamometers and a new intrinsic muscle strength dynamometer. J Rehabil Med. 2004;36(6):273–278. doi: 10.1080/16501970410033677. [DOI] [PubMed] [Google Scholar]
- [49].Roganovic Z. Missile-caused ulnar nerve injuries: outcomes of 128 repairs. Neurosurgery. 2004;55(5):1120–1129. doi: 10.1227/01.neu.0000142353.92119.fe. [DOI] [PubMed] [Google Scholar]
- [50].Roganovic Z, Petkovic S. Missile severances of the radial nerve. Results of 131 repairs. Acta Neurochir (Wien) 2004;146(11):1185–1192. doi: 10.1007/s00701-004-0361-x. [DOI] [PubMed] [Google Scholar]
- [51].Baysefer A, Izci Y, Akay KM, et al. Surgical outcomes of ulnar nerve lesions in children. A retrospective clinical study. Pediatr Neurosurg. 2004;40(3):107–111. doi: 10.1159/000079851. [DOI] [PubMed] [Google Scholar]
- [52].Lundborg G, Rosén B, Dahlin L, et al. Tubular repair of the median or ulnar nerve in the human forearm: a 5-year follow-up. J Hand Surg Br. 2004;29(2):100–107. doi: 10.1016/j.jhsb.2003.09.018. [DOI] [PubMed] [Google Scholar]
- [53].Roganovic Z. Missile-caused median nerve injuries: results of 81 repairs. Surg Neurol. 2005;63(5):410–418. doi: 10.1016/j.surneu.2004.08.007. [DOI] [PubMed] [Google Scholar]
- [54].Rosberg HE, Carlsson KS, Höjgård S, et al. Injury to the human median and ulnar nerves in the forearm--analysis of costs for treatment and rehabilitation of 69 patients in southern Sweden. J Hand Surg Br. 2005;30(1):35–39. doi: 10.1016/j.jhsb.2004.09.003. [DOI] [PubMed] [Google Scholar]
- [55].Ruijs AC, Jaquet JB, Kalmijn S, et al. Median and ulnar nerve injuries: a meta-analysis of predictors of motor and sensory recovery after modern microsurgical nerve repair. Plast Reconstr Surg. 2005;116(2):484–494. doi: 10.1097/01.prs.0000172896.86594.07. [DOI] [PubMed] [Google Scholar]
- [56].Roganovic Z, Pavlicevic G. Difference in recovery potential of peripheral nerves after graft repairs. Neurosurgery. 2006;59(3):621–633. doi: 10.1227/01.NEU.0000228869.48866.BD. [DOI] [PubMed] [Google Scholar]
- [57].Portincasa A, Gozzo G, Parisi D, et al. Microsurgical treatment of injury to peripheral nerves in upper and lower limbs: a critical review of the last 8 years. Microsurgery. 2007;27(5):455–462. doi: 10.1002/micr.20382. [DOI] [PubMed] [Google Scholar]
- [58].Reyes O, Sosa IJ, Santiago J, et al. A novel technique leading to complete sensory and motor recovery across a long peripheral nerve gap. P R Health Sci J. 2007;26(3):225–228. [PubMed] [Google Scholar]
- [59].Donoghoe N, Rosson GD, Dellon AL. Reconstruction of the human median nerve in the forearm with the neurotube. Microsurgery. 2007;27(7):595–600. doi: 10.1002/micr.20408. [DOI] [PubMed] [Google Scholar]
- [60].Cempla J, Pieniazek M, Pelczar-Pieniazek M. Regimen and results of physiotherapy in patients following surgical treatment of ulnar nerve injury. Ortop Traumatol Rehabil. 2007;9(5):499–510. [PubMed] [Google Scholar]
- [61].Secer HI, Daneyemez M, Gonul E, et al. Surgical repair of ulnar nerve lesions caused by gunshot and shrapnel: results in 407 lesions. J Neurosurg. 2007;107(4):776–783. doi: 10.3171/JNS-07/10/0776. [DOI] [PubMed] [Google Scholar]
- [62].Roganovic Z, Ilic S, Savic M. Radial nerve repair using an autologous denatured muscle graft: comparison with outcomes of nerve graft repair. Acta Neurochir (Wien) 2007;149(10):1033–1038. doi: 10.1007/s00701-007-1269-z. [DOI] [PubMed] [Google Scholar]
- [63].Shieh SJ, Lee JW, Chiu HY. Long-term functional results of primary reconstruction of severe forearm injuries. J Plast Reconstr Aesthet Surg. 2007;60(4):339–348. doi: 10.1016/j.bjps.2006.10.006. [DOI] [PubMed] [Google Scholar]
- [64].Vordemvenne T, Langer M, Ochman S, et al. Long-term results after primary microsurgical repair of ulnar and median nerve injuries. A comparison of common score systems. Clin Neurol Neurosurg. 2007;109(3):263–271. doi: 10.1016/j.clineuro.2006.11.006. [DOI] [PubMed] [Google Scholar]
- [65].Noaman H, Khalifa AR, El-Deen MA, et al. Early surgical exploration of radial nerve injury associated with fracture shaft humerus. Microsurgery. 2008;28(8):635–642. doi: 10.1002/micr.20542. [DOI] [PubMed] [Google Scholar]
- [66].Terzis JK, Kokkalis ZT. Outcomes of secondary reconstruction of ulnar nerve lesions: our experience. Plast Reconstr Surg. 2008;122(4):1100–1110. doi: 10.1097/PRS.0b013e3181858f67. [DOI] [PubMed] [Google Scholar]
- [67].Lee YH, Chung MS, Gong HS, et al. Sural nerve autografts for high radial nerve injury with nine centimeter or greater defects. J Hand Surg Am. 2008;33(1):83–86. doi: 10.1016/j.jhsa.2007.10.004. [DOI] [PubMed] [Google Scholar]
- [68].Murovic JA. Upper-extremity peripheral nerve injuries: a Louisiana State University Health Sciences Center literature review with comparison of the operative outcomes of 1837 Louisiana State University Health Sciences Center median, radial, and ulnar nerve lesions. Neurosurgery. 2009;65(Suppl 4):A11–A17. doi: 10.1227/01.NEU.0000339130.90379.89. [DOI] [PubMed] [Google Scholar]
- [69].Mavrogenis AF, Spyridonos SG, Antonopoulos D, et al. Effect of sensory re-education after low median nerve complete transection and repair. J Hand Surg Am. 2009;34(7):1210–1215. doi: 10.1016/j.jhsa.2009.04.014. [DOI] [PubMed] [Google Scholar]
- [70].Gu B, Xie F, Jiang H, et al. Repair of electrically injured median nerve with the aid of somatosensory evoked potential. Microsurgery. 2009;29(6):449–455. doi: 10.1002/micr.20631. [DOI] [PubMed] [Google Scholar]
- [71].Mohseni MA, Pour JS, Pour JG. Primary and delayed repair and nerve grafting for treatment of cut median and ulnar nerves. Pak J Biol Sci. 2010;13(6):287–292. doi: 10.3923/pjbs.2010.287.292. [DOI] [PubMed] [Google Scholar]
- [72].Pan CH, Chuang DC, Rodríguez-Lorenzo A. Outcomes of nerve reconstruction for radial nerve injuries based on the level of injury in 244 operative cases. J Hand Surg Eur Vol. 2010;35(5):385–391. doi: 10.1177/1753193409360283. [DOI] [PubMed] [Google Scholar]
- [73].Boender ZJ, Ultee J, Hovius SE. Cognitive capacity: no association with recovery of sensibility by Semmes Weinstein test score after peripheral nerve injury of the forearm. J Plast Reconstr Aesthet Surg. 2010;63(2):354–359. doi: 10.1016/j.bjps.2008.10.010. [DOI] [PubMed] [Google Scholar]
- [74].Efstathopoulos D, Gerostathopoulos N, Misitzis D, et al. Clinical assessment of primary digital nerve repair. Acta Orthop Scand Suppl. 1995;264:45–47. doi: 10.3109/17453679509157166. [DOI] [PubMed] [Google Scholar]
- [75].Tadjalli HE, McIntyre FH, Dolynchuk KN, et al. Digital nerve repair: relationship between severity of injury and sensibility recovery. Ann Plast Surg. 1995;35(1):36–40. [PubMed] [Google Scholar]
- [76].Lohmeyer JA, Sommer B, Siemers F, et al. Nerve injuries of the upper extremity-expected outcome and clinical examination. Plast Surg Nurs. 2009;29(2):88–93. doi: 10.1097/01.PSN.0000356867.18220.73. [DOI] [PubMed] [Google Scholar]
- [77].Lundborg G. Brain plasticity and hand surgery: an overview. J Hand Surg (Br) 2000;25(3):242–252. doi: 10.1054/jhsb.1999.0339. [DOI] [PubMed] [Google Scholar]
- [78].Segalman KA, Cook PA, Wang BH, et al. Digital neurorrhaphy after the age of 60 years. J Reconstr Microsurg. 2001;17(2):85–88. doi: 10.1055/s-2001-12695. [DOI] [PubMed] [Google Scholar]
- [79].Weber RA, Breidenbach WC, Brown RE, et al. A randomized prospective study of polyglycolic acid conduits for digital nerve reconstruction in humans. Plast Reconstr Surg. 2000;106(5):1036–1045. doi: 10.1097/00006534-200010000-00013. [DOI] [PubMed] [Google Scholar]
- [80].Amillo S, Mora G. Surgical management of neural injuries associated with elbow fractures in children. J Pediatr Orthop. 1999;19(5):573–577. [PubMed] [Google Scholar]
- [81].Kabak S, Halici M, Baktir A, et al. Results of treatment of the extensive volar wrist lacerations: ‘the spaghetti wrist’. Eur J Emerg Med. 2002;9(1):71–76. doi: 10.1097/00063110-200203000-00017. [DOI] [PubMed] [Google Scholar]
- [82].Hobson MI, Brown R, Green CJ, et al. Inter-relationships between angiogenesis and nerve regeneration: a histochemical study. Br J Plast Surg. 1997;50(2):125–131. doi: 10.1016/s0007-1226(97)91325-4. [DOI] [PubMed] [Google Scholar]
- [83].Gu YD. To improve the diagnosis and treatment of peripheral nerve injuries. J Chin Orthop Trauma. 2003;5:1–4. [Google Scholar]
- [84].Sunderland S. 2nd Ed. Edinburgh: Churchi-ll Livingstone, UK; 1978. Nerve and Nerve Injuries. [Google Scholar]
- [85].Haase J, Bjerre P, Simesen K. Median and ulnar nerve transections treated with microsurgical interfascicular cable grafting with autogenous sural nerve. J Neurosurg. 1980;53(1):73–84. doi: 10.3171/jns.1980.53.1.0073. [DOI] [PubMed] [Google Scholar]
- [86].Secer HI, Daneyemez M, Tehli O, et al. The clinical, electrophysiologic, and surgical characteristics of peripheral nerve injuries caused by gunshot wounds in adults: a 40-year experience. Surg Neurol. 2008;69(2):143–152. doi: 10.1016/j.surneu.2007.01.032. [DOI] [PubMed] [Google Scholar]
- [87].Enin LD, Nozdrachev AD, Chumasov EI. Dynamics of the restoration of the function of the skin receptor apparatus after cryogenic damage to the sciatic nerve. Patol Fiziol Eksp Ter. 1997;4:6–8. [PubMed] [Google Scholar]
- [88].Meek MF, Coert JH. Clinical use of nerve conduits in peripheralnerve repair: review of the literature. J Reconstr Microsurg. 2002;18(2):97–109. doi: 10.1055/s-2002-19889. [DOI] [PubMed] [Google Scholar]
- [89].Bell JH, Haycock JW. Next generation nerve guides: materials, fabrication, growth factors, and cell delivery. Tissue Eng Part B Rev. 2012;18(2):116–128. doi: 10.1089/ten.TEB.2011.0498. [DOI] [PubMed] [Google Scholar]
- [90].Aberg M, Ljungberg C, Edin E, et al. Clinical evaluation of a resorbable wrap-around implant as an alternativeto nerve repair: a prospective, assessor-blinded, randomised clinical study of sensory, motor and functional recovery after peripheral nerve repair. J Plast Reconstr Aesthet Surg. 2009;62(11):1503–1509. doi: 10.1016/j.bjps.2008.06.041. [DOI] [PubMed] [Google Scholar]
- [91].Mackinnon SE, Dellon AL. Clinical nerve reconstruction with a bioabsorbable polyglycolic acid tube. Plast Reconstr Surg. 1990;85(3):419–424. doi: 10.1097/00006534-199003000-00015. [DOI] [PubMed] [Google Scholar]
- [92].Battiston B, Geuna S, Ferrero M, et al. Nerve repair by means of tubulization: literature review and personal clinical experience comparing biological and synthetic conduits for sensory nerve repair. Microsurgery. 2005;25(4):258–267. doi: 10.1002/micr.20127. [DOI] [PubMed] [Google Scholar]
- [93].Bushnell BD, McWilliams AD, Whitener GB, et al. Early clinical experience with collagen nerve tubes in digital nerve repair. J Hand Surg Am. 2008;33(7):1081–1087. doi: 10.1016/j.jhsa.2008.03.015. [DOI] [PubMed] [Google Scholar]
- [94].Lohmeyer J JA, Siemers F, Machens HG, et al. The clinical use of artificial nerve conduits for digital nerve repair: a prospective cohort study and literature review. J Reconstr Microsurg. 2009;25(1):55–61. doi: 10.1055/s-0028-1103505. [DOI] [PubMed] [Google Scholar]
- [95].Watanabe T, Kaji R, Oka N, et al. Ultra-high dose methylcobalamin promotes nerve regeneration in experimental acrylamide neuropathy. J Neurol Sci. 1994;122(2):140–143. doi: 10.1016/0022-510x(94)90290-9. [DOI] [PubMed] [Google Scholar]
- [96].Barinaga M. Neurotrophic factors enter the clinic. Science. 1994;264(5160):772–774. doi: 10.1126/science.8171331. [DOI] [PubMed] [Google Scholar]
- [97].Bond TJ, Lundy J. Physical therapy following peripheral nerve surgeries. Clin Podiatr Med Surg. 2006;23(3):651–666. doi: 10.1016/j.cpm.2006.04.006. [DOI] [PubMed] [Google Scholar]
- [98].Sanchez EC. Hyperbaric oxygenation in peripheral nerve repair and regeneration. Neurol Res. 2007;29(2):184–198. doi: 10.1179/016164107X181824. [DOI] [PubMed] [Google Scholar]
- [99].Prpa B, Huddleston PM, An KN, et al. Revascularization of nerve grafts: a qualitative and quantitative study of the soft-tissue bed contributions to blood flow in canine nerve grafts. J Hand Surg Am. 2002;27(6):1041–1047. doi: 10.1053/jhsu.2002.36996. [DOI] [PubMed] [Google Scholar]


