Abstract
OBJECTIVE
Cardiac CT angiography (CTA) is commonly performed after coronary artery bypass grafting surgery (CABG) to assess graft patency, but the images also include parts of the lungs, abdomen, and mediastinum. The purpose of our study was to retrospectively assess the prevalence of unsuspected disease identified on cardiac CTA examinations after CABG and to determine their potential clinical significance.
MATERIALS AND METHODS
CTA was performed postoperatively in 259 patients (mean, 5.2 days), and 40 patients underwent a follow-up CT scan (mean, 12.7 months). Cardiac CTA was acquired using a 16-MDCT scanner with ECG-gating and bolus timing with a small field of view centered on the heart. Two thoracic radiologists assessed each examination in consensus. The prevalence of graft disease and incidental findings (cardiac and noncardiac) was established. The electronic medical record was reviewed. A finding was judged potentially significant if a therapeutic intervention or radiologic follow-up was deemed advisable on the basis of the cardiac CTA. Bypass graft occlusions were analyzed separately.
RESULTS
In the immediate postoperative period, 51 patients (19.7%) had at least one unsuspected, potentially significant finding. Twenty-four patients (9.3%) had a cardiac finding such as a ventricular pseudoaneurysm, ventricular perfusion deficit, or intracardiac thrombus, and 34 patients (13.1%) had a noncardiac finding including pulmonary embolism, lung cancer, or pneumonia. At least one bypass graft was occluded in 17 patients (6.6%) in the immediate postoperative period. In the later postoperative period, seven patients (17.5%) had a potentially significant unsuspected finding. Four patients (10.0%) had at least one graft occlusion.
CONCLUSION
Cardiac CTA after CABG revealed a high prevalence of unsuspected cardiac and noncardiac findings with potential clinical significance. Interpreters of these studies should be familiar with the spectrum of these abnormalities.
Keywords: bypass, cardiac imaging, CT coronary arteriography, lung diseases
ECG-gated cardiac CT, initially with electron beam CT (EBCT) and more recently with MDCT, is increasingly being used to evaluate the coronary arteries and to provide an assessment of noncoronary cardiac disease. Cardiac CT angiography (CTA) examinations are typically acquired with a small field of view focused on the heart, but portions of the lungs, pleura, chest wall, mediastinum, thoracic skeleton, and upper abdomen are often included as part of the examination. Although a wider field of view may be reconstructed from the raw data to assess for additional thoracic findings, these images are not typically used to evaluate the coronary arteries and bypass grafts.
A substantial rate of incidental findings necessitating therapeutic intervention or further radiologic evaluation has been found in patients undergoing coronary artery calcium scoring examinations without IV contrast with EBCT [1–3]. However, limited information exists regarding the prevalence of clinically significant incidental unsuspected findings in patients undergoing CTA [3–7]. The rate of incidental findings with MDCT may be higher because thinner reconstructions are used and IV contrast material is administered. In addition, previous incidental MDCT cardiac CTA studies have focused on patients suspected of having coronary artery disease. To our knowledge, no information currently exists on the rate of incidental findings in patients with known ischemic heart disease or following cardiac surgery. We retrospectively evaluated the frequency of unsuspected cardiac and noncardiac disease in patients who underwent cardiac CTA for routine assessment of coronary artery bypass graft (CABG) patency.
Materials and Methods
Patients
Patients who receive CABG at the University of Maryland Medical Center often undergo cardiac CTA to assess for graft patency as part of their routine postoperative care. From our radiology information system, we identified all individuals who underwent CTA after CABG surgery between October 2002 and March 2006. In the immediate postoperative period, 259 patients (mean age, 63.7 years; age range, 37–89 years; 73.4% men, 26.6% women) underwent a routine contrast-enhanced cardiac CTA examination. Surgical techniques included both off-pump (178 patients, 68.7%) and on-pump (69 patients, 26.6%) cardiac bypass and minimally invasive (six patients, 2.3%) or hybrid coronary bypass grafting (six patients, 2.3%). On average, examinations were performed on postoperative day 5.2 (range, 1–38). Of the original group, a subset of 40 patients underwent a routine follow-up cardiac CTA an average of 12.7 months (range, 2–22 months) after CABG as part of a research protocol for bypass graft patency. Patients who underwent scanning for nonroutine cardiopulmonary disease were excluded. An institutional review board exemption was granted for this study, and the study was performed in compliance with Health Insurance Portability and Accountability Act (HIPAA) regulations.
Image Acquisition
CT angiography was acquired using a 16-MDCT scanner (MX8000 IDT, Philips Medical Systems). For each patient, retrospective ECG-gated images were obtained through the entire chest during a single breath-hold beginning at the inferior margin of the heart and extending to the top of the lung apices (Fig. 1). Patients were advised to exhale slowly if they could not maintain breath-holding throughout the examination. The scanning protocol included collimation of 0.75 mm × 16 with section thickness of 1 mm. The scanning technique was 140 kVp and 350–500 mAs. The typical field of view was 250 mm with a matrix of 512 × 512. A pitch of 0.2–0.3 was used with a scanner rotation time of 0.42 second. Iodinated contrast material (120–150 mL) was injected through an 18- to 20-gauge angiocatheter into an antecubital vein at 3–4 mL/s. Automated bolus timing was performed using a threshold value of 150 H and a region of interest was placed over the ascending aorta. Beta blockade was typically provided as part of routine postoperative care. For accurate image acquisition, sinus rhythm was required, with a mean heart rate less than 100 beats per minute.
Fig. 1.
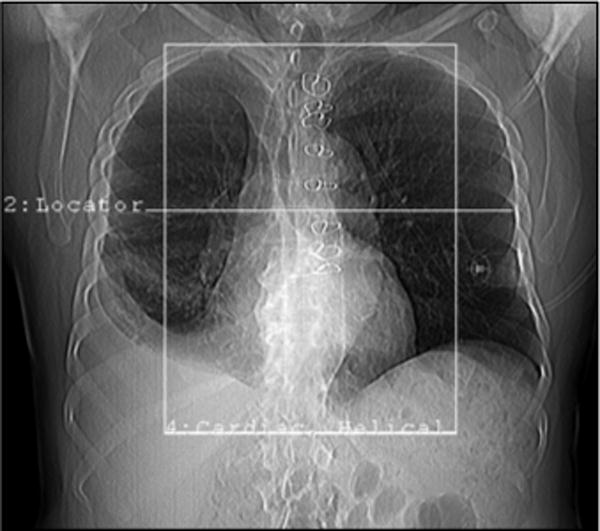
Scout topogram shows typical field of view used for each examination. To include entire course of internal mammary arteries, craniocaudad (z-axis) field of view is more cephalad than typical cardiac CT angiography.
Average scanning time was 30–40 seconds. All images were reconstructed with a small field of view centered on the heart. In each patient, a phase obtained at 75% of the R-R interval was reconstructed and used for primary analysis. Other phases were reconstructed in some patients but were not used for this analysis. The primary data were also reconstructed using curved planar reconstructions along the long axis of the bypass grafts. Wider field of view images (x, y direction) were not reconstructed from the raw data.
Image Interpretation and Review
Each examination was interpreted at the time of scanning by a thoracic radiologist. Axial CT images at 75% of the R-R interval and curved planar postprocessed images were predominantly used for image interpretation. Additional images retrospectively reconstructed at 10 phases of the cardiac cycle were also available if needed. The reviewer provided a qualitative assessment of the overall quality of the scan and reviewed all images on soft-tissue, mediastinal, lung, and bone windows. The patency of each graft was assessed. The grafts were graded as occluded or nonoccluded. When radial grafts were used, spasm was defined as a patent graft with diffuse narrowing. Relevant cardiac and noncardiac findings were described in the final report.
The primary author, a fellow in thoracic radiology with 6 months of cardiac CTA experience, retrospectively assessed each finalized report and reviewed the electronic medical record of each patient to determine the clinical relevance of each finding. A data sheet was generated that included the patient’s age, sex, postoperative day, status of the bypass grafts, and cardiac and noncardiac findings. A finding was defined as potentially significant if a therapeutic intervention was required or if further radiologic evaluation was deemed necessary by the interpreting radiologist. Cardiac disease was documented if the abnormality was paracardiac, pericardial, or within the heart itself. Noncardiac was classified as pulmonary, mediastinal, pleural, or involving the upper abdomen. Common and expected postsurgical findings (e.g., small pleural or pericardial effusions, pneumomediastinum, mild pulmonary edema, etc.) were not included. Findings of minimal clinical significance (e.g., goiter, hiatal hernia, etc.) and known disease (e.g., cardiomegaly, emphysema, etc.) based on information in the electronic medical record (history and physical, operative note, discharge summary, echocardiogram, clinic notes, previous radiology studies, etc.) were noted, but not included in the final analysis. Repeat findings on the immediate and late postoperative examinations were excluded from consideration on the second CT scan.
Some significant findings were defined according to following guidelines. A native coronary artery aneurysm was defined as a lumen diameter at least 1.5 times the size (> 6 mm) of a normal adjacent coronary artery segment (usually 2–4 mm). Pulmonary hypertension was designated if the main pulmonary artery diameter was greater than 3.1 cm. A small pericardial effusion was judged to be present if pericardial fluid did not completely encircle the heart. A moderate or large pericardial effusion was denoted by fluid completely encircling the heart.
Graft abnormalities were analyzed separately. All incidental findings and graft abnormalities were reviewed independently by two radiologists (the primary author and a second thoracic radiologist) to substantiate their presence and a final decision was based on consensus.
Statistical Analysis
Significant findings were divided into cardiac and noncardiac disease. The prevalence of each finding was calculated. The prevalence of bypass graft occlusion was determined.
Results
Fifty-one patients (19.7%) were found to have at least one potentially significant finding requiring therapeutic intervention or further radiologic evaluation. Among these, 24 patients (9.3%) had at least one cardiac finding and 34 patients (13.1%) had at least one noncardiac finding. Seven patients (2.3%) had both a cardiac and noncardiac finding. Five patients had two noncardiac findings (1.9%). Three patients had two cardiac findings (1.2%).
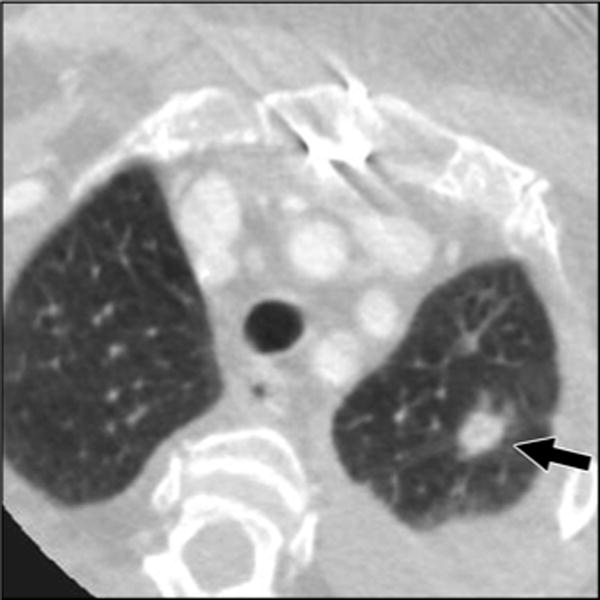
The most common cardiac findings were a moderate or large pericardial effusion (Fig. 2) (eight patients, 3.1%), intracardiac thrombus (Figs. 3 and 4) (six patients, 2.3%), and substantial paracardiac or mediastinal hemorrhage (six patients, 2.3%). Among noncardiac abnormalities, pulmonary nodule (nine patients, 3.5%), pneumonia (six patients, 2.3%), tracheal or lobar mucous plugging (six patients, 2.3%), and pulmonary embolism (Fig. 5) (five patients, 1.9%) were most frequent (Table 1).
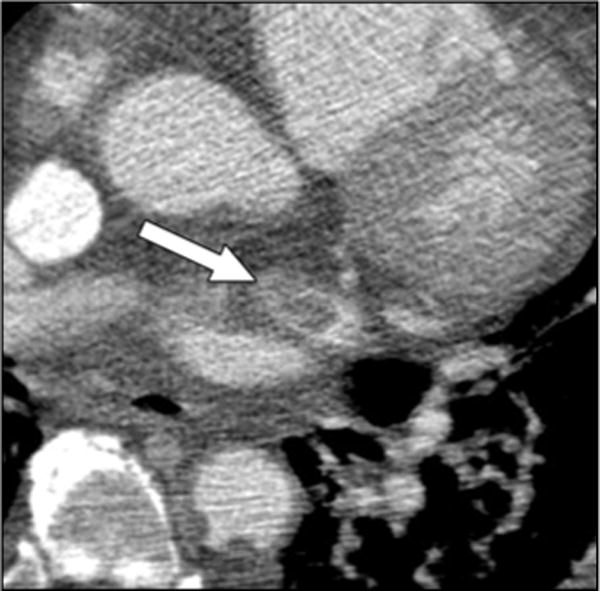
Fig. 2.

45-year-old man who underwent cardiac CT angiography 6 days after coronary bypass grafting surgery. Axial CT image shows anterior ventricular pseudoaneurysm (white arrow) and large hemopericardium (open arrow). Patient had good recovery after surgery.
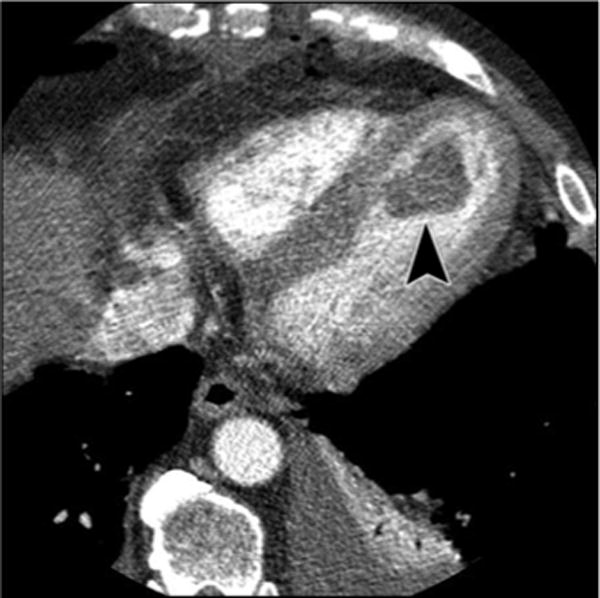
Fig. 3.
73-year-old man who underwent routine cardiac CT angiography 7 days after coronary bypass grafting surgery. Axial CT image shows thrombus in left atrial appendage (arrow). Intraoperative transesophageal echocardiogram showed no intracardiac thrombus (not shown).
Fig. 4.
67-year-old man who underwent coronary artery bypass grafting surgery after inferior myocardial infarction. Axial CT image from routine cardiac CT angiography 7 days after surgery shows unsuspected left ventricular thrombus (arrowhead).
Fig. 5.
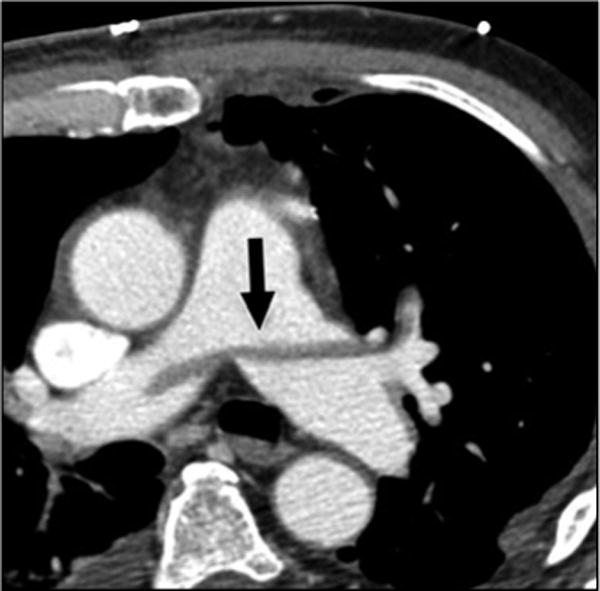
63-year-old symptomatic man who underwent routine cardiac CT angiography 2 days after coronary artery bypass grafting surgery. Axial CT image shows saddle pulmonary embolism (arrow).
TABLE I.
Significant and Unexpected Immediate Postoperative Findingsa
| Patients | Percent | Imaging Follow-Up | Treatment | |
|---|---|---|---|---|
|
| ||||
| Incidental noncardiac findings | ||||
| Pulmonary nodule | 9 | 3.5 | Four patients (follow-up chest CT) | One patient (lung carcinoma) |
| Pneumonia | 6 | 2.3 | Three patients (antibiotics) | |
| Large mucous plug | 6 | 2.3 | One bronchoscopy | |
| Pulmonary embolism | 5 | 1.9 | Three patients (anticoagulation) | |
| Aortic ulcer or aneurysm | 3 | 1.2 | Three patients (follow-up chest CT) | |
| Adrenal mass | 2 | 0.8 | Two patients (follow-up abdominal CT) | |
| Moderate pleural effusion | 2 | 0.8 | One patient (follow-up chest CT) | |
| Sternal dehiscence | 1 | 0.4 | Reoperation | |
| Mediastinitis | 1 | 0.4 | One patient (follow-up chest CT) | |
| Sarcoidosis | 1 | 0.4 | ||
| Pulmonary hypertension | 1 | 0.4 | ||
| Moderate-sized pneumothorax | 1 | 0.4 | ||
|
| ||||
| Incidental cardiac findings | ||||
| Moderate-to-large pericardial effusion | 8 | 3.1 | One patient (pericardial drain); one patient (reoperation); one patient (hospital readmission) | |
| Large mediastinal hematoma | 6 | 2.3 | One patient (follow-up chest CT) | One patient (reoperation); two patients (blood transfusion) |
| Left ventricular thrombus | 4 | 1.5 | One patient (anticoagulation) | |
| Left ventricular perfusion deficit | 3 | 1.2 | ||
| Left ventricular pseudoaneurysm | 2 | 0.8 | One patient (reoperation) | |
| Left atrial thrombus | 2 | 0.8 | One patient (anticoagulation) | |
| Right ventricular compression, pectus excavatum | 1 | 0.4 | ||
| Native coronary artery aneurysm | 1 | 0.4 | ||
| Apical left ventricular aneurysm | 1 | 0.4 | ||
Average postoperative time, 5.2 days.
On the basis of the CT interpretation, 15 patients (5.8%) had a documented clinical intervention and 12 patients (4.6%) had a radiologic follow-up. Two patients had both a clinical intervention and a radiologic follow-up. The remaining 26 patients (10.0%) were lost to follow-up or did not have further intervention to our best knowledge. Further interventions included repeat cardiac surgery (three patients, 1.2%), hospital readmission (one patient, 0.4%), insertion of a pericardial drainage catheter (one patient, 0.4%), lung carcinoma (one patient, 0.4%), anticoagulation (five patients, 1.9%), bronchoscopy for a large mucous plug (one patient, 0.4%), blood transfusion (two patients, 0.8%), and antibiotic treatment for pneumonia (three patients, 1.2%).
Of the nine pulmonary nodules that were found, one patient underwent pulmonary consultation, PET, and lung biopsy with a histologic diagnosis of lung carcinoma (Fig. 6). Three patients received follow-up chest CT revealing nodule stability. A fourth patient is scheduled for CT follow-up. Of the two adrenal masses, both patients received follow-up abdominal CT. One mass was diagnosed as a lipid-rich adrenal adenoma. The second adrenal mass remained indeterminate on follow-up abdominal CT. The patient has not undergone additional workup or therapy. The decision to transfuse two patients was based on the combination of the CT interpretations and the low hemoglobin levels. One of the patients who had large mucous plug underwent bronchoscopy for aspiration of the plug. We presume the remaining patients with mucous plugging received pulmonary toilet, but clinical documentation is not available for confirmation.
Fig. 6.
A 1.1-cm spiculated left upper lobe pulmonary nodule, (arrows) was discovered in 76-year-old man shortly after coronary bypass. Percutaneous lung biopsy revealed carcinoma.
Of the 40 patients who underwent a routine follow-up cardiac CTA in the late postoperative period (mean, 12.7 months), seven patients (17.5%) had an incidental and unsuspected finding. Among these, three patients (7.5%) had a cardiac finding and four patients (10%) had a noncardiac finding. These findings included a new left subclavian artery thrombus, pulmonary edema, apical left ventricular perfusion defect, moderate pericardial effusion, new central venous obstruction, and moderate-sized pleural effusion. All seven patients were treated conservatively.
With respect to bypass graft assessment, one or more bypass grafts were occluded in 17 patients (6.6%) in the immediate postoperative period and in four patients (10.0%) in the late postoperative period. All of the occluded grafts (Fig. 7) were saphenous vein grafts. One patient had two saphenous vein grafts occlude in the immediate period. None of the internal mammary artery grafts occluded. Spasm was a frequent finding with radial artery grafts, although none of these grafts were occluded. Graft patency was not confirmed with catheter angiography.
Fig. 7.
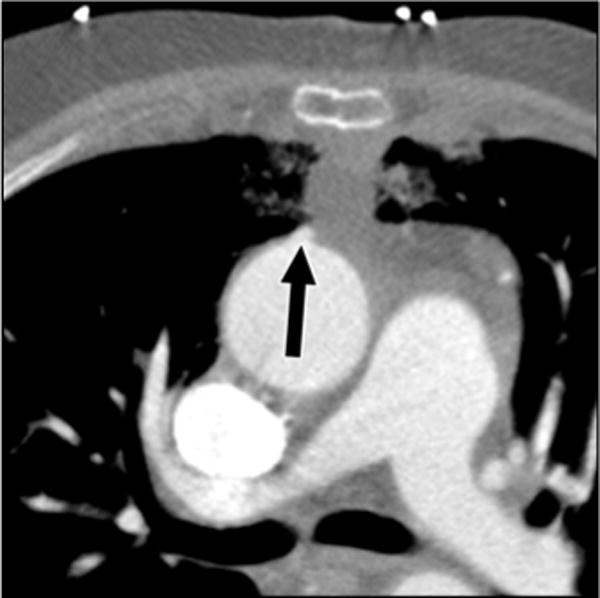
56-year-old woman with unsuspected thrombosed aortocoronary saphenous vein graft (arrow) 5 days after coronary artery bypass grafting procedure.
Discussion
Our study of a rather large cohort of patients suggests a frequency of unsuspected and potentially significant findings of approximately 20% in patients who undergo cardiac CTA both immediately and remotely after CABG. Several studies have assessed the frequency of incidental findings in the context of various types of cardiac-focused CT examinations [1–7].
A modest body of literature has been published concerning incidental findings on unenhanced EBCT scans obtained for coronary calcium scoring [1–3]. Horton et al. [1] reported that 7.8% of patients undergoing coronary calcium scoring required additional workup for noncardiac disease. In a later study, Schragin et al. [2] found 4.2% of patients required CT follow-up and 20.5% of examinations had at least one noncardiac finding, including one patient where the incidental finding was the cause of death. These studies differ from the current study in that they were performed with relatively thick sections (3 mm) and without the use of IV contrast material, precluding evaluation of cardiovascular and mediastinal structures. In addition, we studied postoperative patients after cardiovascular surgery, whereas many of the patients studied with EBCT were outpatients. This may explain the lower rate of abnormalities with potential clinical impact detected in the EBCT studies.
The prevalence of incidental findings was found to be higher with the use of IV contrast. Hunold et al. [3] examined patients who underwent a cardiac EBCT examination for calcium scoring or coronary angiography. Combining both incidental cardiac and noncardiac disease, they determined that 9.3% of patients required further radiologic investigation, and specific therapy was initiated in 22 patients (1.2%). Malignant disease was detected in three patients.
The rate of incidental disease was higher with the use of MDCT for coronary CTA. A recently published study by Haller et al. [4] showed that 4.8% of patients undergoing cardiac CTA with a small field of view had a major noncardiac finding and 19.9% of patients had a minor noncardiac finding. In two recent abstracts by Shafique et al. [5] and Onuma et al. [6], the rate of significant noncardiac findings requiring further investigation or treatment on contrast enhanced cardiac CTA examinations was 16% in both studies. A third abstract also showed a high prevalence (44%) of significant or potentially significant noncoronary disease [7]. The prevalence of noncardiac findings in those studies is similar to this evaluation. However, the rate of incidental cardiac findings in this study was much higher. Nearly every coronary bypass patient has known ischemic heart disease. Therefore, the discovery of complicating conditions, such as intracardiac thrombi, myocardial perfusion deficits, and ventricular aneurysms, from significant coronary artery disease is not surprising. In addition, large mediastinal or paracardiac hemorrhage was included in the cardiac category, another condition that occasionally occurs after coronary bypass.
The results of this investigation suggest that the rate of incidental disease detected on cardiac CTA examinations after major cardiovascular surgery in the inpatient or critical care setting is higher than in cardiac CTA examinations typically performed in the outpatient setting. Several issues may account for this discrepancy. One consideration is that the patient cohort in our study is presumably a higher risk group than the majority of patients who undergo cardiac CTA as outpatients. In an effort to evaluate the internal mammary arteries, the CABG CTA protocol extends more cephalic than a typical cardiac CTA examination. Including the superior thorax with a longer z-axis area of coverage allows additional abnormalities to be detected (Fig. 1). One mitigating factor that may have paradoxically lowered the prevalence of certain abnormalities is that common postoperative abnormalities such as atelectasis and effusions obscured significant abnormalities.
Another consideration is that the definition of what constitutes a clinically significant finding varies among different studies. Most studies, including this one, define “significant” or “potentially significant” if imaging follow-up or a therapeutic intervention was advised. However, to maintain as much clinical relevance as possible in a postoperative setting, we excluded known disease typically found on preoperative pulmonary function testing or echocardiography (i.e., emphysema or cardiomegaly), abnormalities of minimal significance (i.e., goiter and hiatal hernia), and expected postoperative conditions (i.e., pulmonary edema).
We chose to analyze bypass grafts separately because their assessment was the indication for the CTA, and thus a graft occlusion could not truly be called incidental. At least one failed graft occurred in 6.6% of patients in the immediate postoperative period and 10.0% of patients in the late postoperative period, indicating a significant attrition rate. Nearly all graft failures involved saphenous vein grafts and none occurred with internal mammary grafts. Although bypass graft occlusion was not routinely confirmed on catheter angiography, the rates of graft failure are concordant with the published literature [8]. It has been proposed that subacute premature saphenous vein graft failures (i.e., the additional grafts that occluded after the early postoperative period) are due to neointimal hyperplasia, which predominately affects venous but not arterial grafts [9, 10].
This study has important clinical ramifications. Bypass graft patency is a common indication for cardiac CTA, particularly among patients with recurrent symptoms after CABG. To our knowledge, this is the first study examining the rate of incidental findings on cardiac CTA examinations performed primarily on postoperative patients or those with known ischemic heart disease. Previous incidental studies have focused on outpatients or individuals with suspected coronary artery disease [1–7]. As a result, the rate of incidental cardiac disease was higher (9.3%). This highlights the need to evaluate extracoronary cardiac structures as well as the noncardiac anatomy on every cardiac CTA examination. In addition, cardiac CTA examinations performed after major cardiovascular surgery have the potential to detect treatable cardiac and noncardiac complications in a more timely fashion. This was evident from our investigation because we found a number of treatable conditions that were not clinically suspected at the time. Treatable disease included pulmonary embolism (Fig. 5), pneumonia, cardiac pseudoaneurysms (Figs. 2 and 8), intracardiac thrombi (Figs. 3 and 4), and mediastinal and pericardial hemorrhage.
Fig. 8.
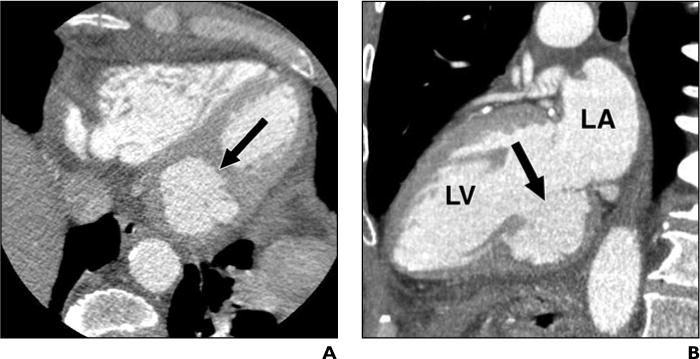
63-year-old asymptomatic man who underwent cardiac CT angiography 3 days after coronary bypass grafting surgery.
A, Axial CT image shows left ventricular aneurysm (arrow).
B, Oblique multiplanar reformatted image in vertical long axis projection confirms inferior ventricular pseudoaneurysm (arrow). LA = left atrium, LV = left ventricle.
This study has several important limitations. Bias was introduced because of the retrospective design of the study. We did not review studies without a reported unsuspected finding because there would have been no opportunity to act on these findings even if they were significant. In addition, long-term clinical and imaging follow-up were not available in many patients with a significant finding. We determined therapeutic intervention on the basis of clinical information in the electronic medical record, which usually includes the operative note, echocardiogram, cardiac catherization, discharge summary, and radiology reports. However, this system does not include every follow-up surgical, cardiology or primary care clinic note. Therefore, determining if a therapeutic intervention or specialty consult was ultimately performed or planned on the basis of the imaging interpretation alone was sometimes difficult. Thus, we chose the term “potentially significant.” Other published studies of incidental findings on cardiac CT also have incomplete or nonexistent follow-up, possibly for the same reasons.
Although our overall patient cohort was sizeable, the number of patients studied in the later postoperative period was low (n = 40), and incidental findings included in the first study were not duplicated in the second. Because our patient population recently had undergone major cardiovascular surgery and have known ischemic heart disease, we cannot generalize these findings for outpatients or patients with suspected coronary artery disease. Also, the raw data were not reconstructed to create a wider field of view (x, y direction) possibly allowing more incidental findings to be discovered. Finally, our diagnosis of graft occlusion was not confirmed on coronary angiography. Nevertheless, cardiac CTA has shown greater than 90% sensitivity and specificity for detection of graft occlusion using invasive angiography as a standard of reference [11–14].
In summary, cardiac CTA performed after CABG surgery is valuable to determine graft patency and also frequently detects clinically occult and potentially life-threatening abnormalities. All physicians interpreting cardiac CTA should be cognizant of both cardiac and noncardiac findings commonly present in patients after CABG surgery.
References
- 1.Horton KM, Post WS, Blumenthal RS, Fishman EK. Prevalence of significant noncardiac findings on electron-beam computed tomography coronary artery calcium screening examinations. Circulation. 2002;106:532–537. doi: 10.1161/01.cir.0000027136.56615.de. [DOI] [PubMed] [Google Scholar]
- 2.Schragin JG, Weissfeld JL, Edmundowicz D, Strollo D, Fuhrman CR. Non-cardiac findings on coronary electron beam computed tomography scanning. J Thorac Imaging. 2004;19:82–86. doi: 10.1097/00005382-200404000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Hunold P, Schmermund A, Seibel RM, Gronemeyer DH, Erbel R. Prevalence and clinical significance of accidental findings in electron beam tomographic scans for coronary artery calcification. Eur Heart J. 2001;22:1748–1758. doi: 10.1053/euhj.2000.2586. [DOI] [PubMed] [Google Scholar]
- 4.Haller S, Kaiser C, Buser P, Bongartz G, Bremerich J. Coronary artery imaging with contrast-enhanced MDCT: extracardiac findings. AJR. 2006;187:105–110. doi: 10.2214/AJR.04.1988. [DOI] [PubMed] [Google Scholar]
- 5.Shafique I, Shapiro EP, Stafford S, Bush DE. Noncoronary findings on multidetector CT coronary angiography. (abstr) Circulation. 2004;110(suppl 3):523. [Google Scholar]
- 6.Onuma Y, Tanube K, Hatori M, et al. Non-cardiac findings in coronary imaging with multi-detector computed tomography. J Am Coll Cardiol. 2006;48:402–406. doi: 10.1016/j.jacc.2006.04.071. [DOI] [PubMed] [Google Scholar]
- 7.Patel S, Woodrow A, Bogot N, et al. Non-coronary findings on 16-row multidetector CT coronary angiography. AJR. 2005;184(American Roentgen Ray Society 105th Annual Meeting Abstract Book suppl):3. [Google Scholar]
- 8.Fitzgibbon GM, Kafka HP, Leach AJ, Keon WJ, Hooper GD, Burton JR. Coronary bypass graft fate and patient outcome: angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J Am Coll Cardiol. 1996;28:616–626. doi: 10.1016/0735-1097(96)00206-9. [DOI] [PubMed] [Google Scholar]
- 9.Motwani JG, Topol EJ. Aortocoronary saphenous vein graft disease: pathogenesis, predisposition, and prevention. Circulation. 1998;97:916–931. doi: 10.1161/01.cir.97.9.916. [DOI] [PubMed] [Google Scholar]
- 10.Dobrin PB. Mechanical factors associated with the development of intimal and medial thickening in vein grafts subjected to arterial pressure: a model of arteries exposed to hypertension. Hypertension. 1995;26:38–43. doi: 10.1161/01.hyp.26.1.38. [DOI] [PubMed] [Google Scholar]
- 11.Pache G, Saueressig U, Frydrychowicz A, et al. Initial experience with 64-slice cardiac CT: non-invasive visualization of coronary artery bypass grafts. Eur Heart J. 2006;27:976–980. doi: 10.1093/eurheartj/ehi824. [DOI] [PubMed] [Google Scholar]
- 12.Moore RK, Sampson C, MacDonald S, Moynahan C, Groves D, Chester MR. Coronary artery bypass graft imaging using ECG-gated multislice CT: comparison with catheter angiography. Clin Radiol. 2005;60:990–998. doi: 10.1016/j.crad.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Salm LP, Jukema JW, Schuijf JD, et al. Comprehensive assessment of patients after coronary bypass grafting by 16 detector row CT. Am Heart J. 2005;150:775–781. doi: 10.1016/j.ahj.2004.11.029. [DOI] [PubMed] [Google Scholar]
- 14.Schlosser T, Konorza T, Hunold P, Kuhl H, Schmermund A, Barkhausen J. Non-invasive visualization of coronary bypass grafting using 16 detector row CT. J Am Coll Cardiol. 2004;44:1224–1229. doi: 10.1016/j.jacc.2003.09.075. [DOI] [PubMed] [Google Scholar]


