Abstract
Background
Few nationally representative studies have examined racial/ethnic disparities in alcohol services utilization. Further, little is known about whether racial/ethnic disparities generalize across genders, and what factors account for these disparities. Thus, we aimed to describe the combined impact of race/ethnicity and gender on alcohol services utilization, and to explore roles for social influence factors in explaining racial/ethnic and gender disparities.
Methods
Data were pooled across the 2000, 2005, and 2010 National Alcohol Surveys. Outcomes included lifetime utilization of any services, specialty alcohol treatment, and Alcoholics Anonymous (AA). Social influence factors were assessed as lifetime social pressures (i.e., pressures from a partner, friends, and/or family), legal consequences, and work-related consequences. Core analyses included only those with a lifetime alcohol use disorder (AUD).
Results
Analyses revealed a pattern of lower services utilization among Latinos and Blacks (vs. Whites) and women (vs. men); further, race-by-gender interactions revealed that Black-White differences were limited to women, and provided some evidence of stronger Latino-White disparities among women (vs. men). Illustrating these patterns, among women, only 2.5% of Latinas and 3.4% of Blacks with a lifetime AUD accessed specialty treatment, vs. 6.7% of Whites; among men, corresponding figures were 6.8% for Latinos, 12.2% for Blacks, and 10.1% for Whites. Racial/ethnic differences were typically robust (or stronger) when controlling for demographics and AUD severity. Evidence did not support a role for measured social influence factors in racial/ethnic disparities, but did suggest that these factors contribute to gender disparities, particularly among Whites and Blacks.
Discussion
Findings for substantial Latino-White and Black-White disparities, especially among women, highlight the need for continuing research on explanatory factors and the development of appropriate interventions. Meanwhile, our evidence for persistent gender disparities and for social influence factors as drivers of these disparities tentatively suggests a need for intensified outreach to female heavy drinkers.
Keywords: Hispanic, African American, alcohol treatment, health disparities, social pressures, alcohol dependence
Introduction
The evidence base surrounding racial/ethnic disparities in alcohol consumption and problems is now well-developed, and provides some evidence that Black and Latino men are especially vulnerable to a range of alcohol-related problems, including alcohol-related injury and health problems (Caetano, 2003; Flores et al., 2008; Keyes et al., 2012). Overall, Latino men may also be at higher risk of high-volume drinking and alcohol dependence than White men (Caetano and Clark, 1998; Hasin and Grant, 2004; Kandel et al., 1997; Naimi et al., 2010; Neff, 1997; Zemore et al., 2013), though it bears emphasis that heterogeneity among Latino ethnic subgroups is substantial (Caetano et al., 1998; Vaeth et al., 2009). Both Latinos and Blacks also appear to be more likely than Whites to experience recurrent or persistent alcohol dependence (Dawson et al., 2005). By contrast, there are very few national studies examining racial/ethnic disparities in alcohol services utilization (Gomberg, 2003). Many studies fail to distinguish alcohol from drug treatment, and many have not had large enough samples to disaggregate by specific racial/ethnic groups. Thus, the current study aims to both describe and help explain racial/ethnic disparities in alcohol services utilization, acknowledging that gender disparities operate in concert with, and indeed may moderate, racial/ethnic disparities.
Racial/ethnic and Gender Disparities in Alcohol Services Utilization
To our knowledge, just three large, nationally representative studies have examined disparities across Whites, Latinos, and Blacks in alcohol services utilization since 1990. The first two analyzed multiple cross-sectional surveys: One combined the 1991-2 National Longitudinal Alcohol Epidemiologic Survey (NLAES) and the 2001-2 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; Chartier and Caetano, 2010), and the second combined the 1995 and 2000 National Alcohol Surveys (NAS; Schmidt et al., 2007); both compared lifetime services utilization among Whites, Latinos, and Blacks with a lifetime alcohol use disorder (AUD). The third (longitudinal) study sampled those who met criteria for at-risk drinking or alcohol abuse in the initial NESARC survey (2001-2) and examined alcohol services utilization across a 4-year period including the year preceding baseline (Mulia et al., 2014). All three studies reported significant Latino-White disparities that remained robust in multivariate analyses. Both cross-sectional studies reported substantially lower utilization of specialty alcohol/drug treatment programs1 among Latinos (vs. Whites), while Mulia et al. reported that Latinos had significantly lower odds than Whites of receiving an “alcohol intervention” (i.e., alcohol-related services provided by a physician/mental health clinician, or specialty treatment); disparities were strongest for foreign-born Latinos. Results were more mixed for utilization of other services, though both cross-sectional studies found that, at higher severity levels, Latinos and Blacks were less likely than Whites to have used any alcohol services. Consistent with the absence of strong Black-White differences above, Keyes et al. (2008), comparing Blacks and Whites alone in the 2001-2 NESARC, reported no racial/ethnic differences in alcohol services utilization in multivariate analyses of respondents with a lifetime AUD, though Blacks were slightly higher than Whites on services use in bivariate analyses. Notably, results from studies of substance abuse treatment (combining alcohol and drugs) diverge somewhat from the above results, suggesting that service utilization patterns for alcohol and drug treatment vary (Cook and Alegría, 2011; Mojtabai, 2005; Mojtabai and Crum, 2013).
Besides these studies, there are a handful of older studies and area studies that reveal mixed results. For example, a longitudinal study following a probabilistic national sample of U.S. adults first sampled in 1984 found that Latinos were more likely than Whites to report any alcohol services utilization at the 8-year follow-up, while Blacks and Whites were equivalent (Kaskutas et al., 1997). Another large, longitudinal study following problem drinkers in Northern California found that odds of receiving specialty treatment were conversely lower among Latinos than Whites at 3 years (but not at 1 year), while Blacks and Whites were again equivalent (Weisner et al., 2002).
Meanwhile, the evidence for gender disparities in alcohol services utilization is substantial, and consistent. In past research, female gender has been an extremely reliable and powerful predictor of lower alcohol services utilization (Chartier and Caetano, 2011; Dawson, 1996; Ilgen et al., 2011; Schmidt et al., 2007; Zemore et al., 2009). This effect has remained robust in analyses accounting for alcohol severity and other factors, suggesting that women’s lower severity cannot account for the disparity.
In sum, existing data suggest that both racial/ethnic minorities and women may be at particular risk for unmet treatment need. However, the evidence on racial/ethnic disparities is sparse (and mixed). Moreover, relevant national survey studies, while informative, are now as a whole somewhat dated, and may not be indicative of current disparities. Supporting this point, research has shown substantial changes in racial/ethnic disparities in services utilization over time (Chartier and Caetano, 2011). Additional studies are also needed to examine the combined impact of race/ethnicity and gender on services utilization. To our knowledge, no large-scale, existing studies have directly examined whether race/ethnicity and gender interact to predict alcohol services utilization.
Explanatory Factors—and the Role of Social Influence Specifically—in Race and Gender Disparities
At present, little is known about why Latinos, Blacks, and women may be less likely to obtain help than Whites and men. Existing research points to a range of potential barriers, including limitations in treatment access; lack of awareness of available options; low recognition of treatment need; concerns about treatment efficacy; logistical and cultural/linguistic barriers; and heightened alcoholism stigma (Perron et al., 2009; Rouse et al., 1995; Schmidt et al., 2007; Zemore et al., 2009). Many of these barriers have been hypothesized to especially affect Latina and Black women (Rouse et al., 1995)—which, notably, implies especially high unmet need in these groups. However, the research surrounding barriers has often not distinguished between alcohol, drug, and mental health treatment, and there have been no studies to our knowledge directly testing mediation of racial/ethnic and gender disparities. Thus, much work remains to be done.
Social pressures to cut down or seek help have received only minimal attention in the literature as factors that may explain disparities in alcohol services utilization. Nevertheless, research suggests that most problem drinkers experience social influences to change their drinking and/or seek help, and that this type of pressure is a major contributor to alcohol services utilization. Further, though these experiences are typically related to higher alcohol severity, they predict services utilization independently of severity (Korcha et al., 2013; Polcin et al., 2012; Weisner et al., 2002). Importantly, some (older) research also suggests that women are less likely than men to encounter social influences related to drinking (Room et al., 1991; Schober and Annis, 1996; Weisner, 1990), possibly as a result of a more covert drinking pattern and choice of venue (e.g., avoidance of public spaces). If this remains true, then diminished social influence may help explain the diminished alcohol services utilization among women. By contrast, there is no strong case for social factors as mediators of racial/ethnic disparities. While a few studies have examined social influence factors by race/ethnicity (Hasin, 1994; Polcin and Beattie, 2007; Polcin et al., 2012), results have been inconsistent and hard to interpret in relation to alcohol services utilization, largely because studies did not target drinkers in need of treatment. Further, Latinos and Blacks may, overall, experience elevated (vs. diminished) social influence to enter treatment because they are more likely to be coerced by employers and the criminal justice system (Polcin and Weisner, 1999). Still, there may be some role for social influence factors in explaining racial/ethnic disparities among women, such as they are.
The Current Paper
The current paper aims to extend existing research by offering a more recent examination of alcohol services utilization in a nationally representative sample. Our paper compares services utilization across Whites, Latinos, and Blacks, and tests whether effects for race/ethnicity are modified by gender. Although our sample is not sufficiently large to explore temporal changes in services utilization in interaction with race/ethnicity, we do describe the overall temporal trends. Outcomes include use of any services, a specialty alcohol/drug treatment program, and Alcoholics Anonymous (AA). Our focus on specialty treatment and AA is justified by the large literature linking use (vs. nonuse) of these services to better alcohol and drug outcomes (Emrick et al., 1993; McCrady and Miller, 1993; McLellan et al., 2000; Project MATCH Research Group, 1997; Tonigan et al., 1996), combined with the fact that, among individuals reporting seeking help for an alcohol problem, use of specialty programs and AA is common (Chartier and Caetano, 2011). An additional goal is to examine whether variation in social influences on services utilization—meaning pressures from family, friends, the law, and employers to cut down on drinking, abstain from drinking, and/or seek treatment—contributes to racial/ethnic and gender disparities in utilization.
Hypotheses
Based on the above, we hypothesized that Latinos with a lifetime AUD would report lower services utilization than Whites, and that women would report lower services utilization than men. We also expected that racial/ethnic differences would be strongest among women, and that such differences would maintain even accounting for lifetime alcohol dependence severity and other covariates. Finally, we expected that gender differences in services utilization would be at least partially mediated by lower levels of social influence to seek help among women. We expected only partial mediation because of the many other factors likely to be operative in relation to gender disparities, particularly for racial/ethnic minority women. While exploration of those other factors is beyond the scope of the current study, future studies are planned to address additional factors that may play explanatory roles.
Materials and Methods
Data Source and Sample
To yield adequate power, data were pooled from the three most recent waves of the National Alcohol Survey, or NAS (i.e., 2000, 2005, and 2010). The combined 2000-2010 NAS yield a total N=21,538 (13,471 Non-Hispanic Whites, 4,010 Non-Hispanic Blacks, and 4,057 Latinos). The NAS are independent, nationally representative surveys of adults aged 18 and over collected every 5 years by the Alcohol Research Group. Each of the 2000-2010 surveys were implemented as computer-assisted telephone surveys and included a large, probability sample of the U.S. population, selected via random-digit dialing, and oversamples of Blacks, Latinos, and sparsely populated states. The 2010 NAS also included a cell sample comprising about 14% (N=1,012) of the total sample. Respondents were interviewed in English and Spanish. Response rates were 58% in 2000, 56% in 2005, and 52% in 2010. These rates are typical of recent U.S. telephone surveys in a time of increasing barrier to RDD surveys (Midanik and Greenfield, 2003). Further, methodological studies conducted by the Alcohol Research Group investigating the impact of nonresponse in the 1995 and 2000 Surveys have, comparing independent national samples (or “replicates”) with differing response rates, yielded no consistent differences associated with nonresponse. This suggests that nonresponse is unlikely to have biased NAS prevalence rates. For detailed discussion of the NAS methodology, see Kerr et al. (2004).
Measures
Alcohol dependence symptoms
Dependence symptoms were measured using an 18-item scale that assesses symptoms in the 7 domains identified by the APA’s Diagnostic and Statistical Manual-4th Edition (DSM-IV, American Psychiatric Association, 1994) and that has been extensively validated (Caetano and Tam, 1995). Individuals indicating at least one symptom in 3+ domains over the past 12 months were coded as positive on current alcohol dependence, while those reporting symptoms in 3+ domains in their lifetime were coded as positive on lifetime alcohol dependence. Further, lifetime symptom count was used as a continuous measure of dependence severity in multivariate analyses.
Alcohol-related consequences
Symptoms of alcohol abuse (i.e., consequences) were measured using a 12-item scale assessing problems while or because of drinking across 4 domains: social (4 items), legal (3 items), workplace (3 items), and injuries and accidents (2 items). Participants reporting at least one consequence in the past 12 months were coded as positive on current alcohol abuse, while those experiencing at least one consequence in their lifetimes were coded as positive on lifetime alcohol abuse. Items were also used to create separate measures of lifetime legal and work-related consequences. Legal items assessed whether the respondent was ever “arrested for driving after drinking,” ever experienced “trouble with the law about drinking when driving was not involved,” and was ever “questioned or warned” by a police officer because of his or her drinking. Work-related items assessed whether the respondent ever “lost a job, or nearly lost one, because of drinking,” whether “people at work indicated that [he/she] should cut down on drinking,” and whether “Drinking may have hurt [his/her] chances for promotion, or raises, or better jobs.” All items were yes/no, and were used to create dichotomous measures indicating any vs. no consequences in each domain. In the current study, subscale alphas were .67 for legal consequences and .77 for work-related consequences; alpha for the total scale was .83.
Social pressures
Respondents were also asked to indicate which of 6 social relations “might have [ever] liked you to drink less or to act differently when you drank”, including a spouse/someone the respondent lived with, a parent, any other relative, a girlfriend or boyfriend, anyone else the respondent lived with, and any other friend. All questions were yes/no; responses were summed, so that higher scores indicated greater social pressures. This measure and slight variations of it have been used in several studies, where it has been associated with higher alcohol severity, treatment motivation, and services utilization (Hasin, 1994; Korcha et al., 2013; Room et al., 1991); 6-item alpha for the 2010 survey was .80.
Alcohol consumption variables
Current drinkers (vs. abstainers) were coded to include those who indicated drinking at least one alcoholic beverage in the prior 12 months. Heavy drinking was assessed as monthly 5+ and monthly 8+ drinking (vs. not). These variables were coded using our survey’s graduated quantity-frequency items (Greenfield, 1998), which include questions regarding the frequency of drinking 1-2, 3-4, 5-7, 8-11, and 12+ alcoholic beverages in a single day.
Alcohol services utilization variables
We assessed lifetime alcohol services utilization using two questions. Respondents were first asked, “Have you ever gone to anyone—a physician, AA, a treatment agency, anyone at all—for a problem related in any way to your drinking?” Respondents indicating “yes” were asked if they went to a) an alcoholism or drug treatment program, b) Alcoholics Anonymous (AA), and/or c) other institutions and professional people not relevant to the current paper. Respondents were also (subsequently) asked, “Did you ever receive treatment from a chemical dependency or substance abuse program for either alcohol or drugs?,” and if so, whether for alcohol, drugs, or both. Respondents indicating use of any services (in response to the first question) were coded as positive on any services, and respondents indicating use of AA (again in response to the first question) were coding as positive on AA. Respondents indicating use of an alcoholism or drug treatment program (for alcohol problems) in response to either question were coded as positive on specialty treatment. Outcomes were not mutually exclusive.
Demographic and other variables
Race/ethnicity was ascertained by asking participants which best described their family origin: White (not of Hispanic origin), White (of Hispanic origin), Black (not of Hispanic origin), Black (of Hispanic origin), Asian, American Indian/Alaskan Native, or Other. Categories were recoded as White (not of Hispanic origin), Latino (including both Whites and Blacks of Hispanic origin), Black (not of Hispanic origin), and Other (all other). We also coded respondent gender (female or male), age (continuous), education (less than high school, high school diploma, some college, or college graduate or more), employment status (employed full/part-time, unemployed, or out of the workforce), annual household income in 2005 dollars (<$20,000, $20,000-$39,999, $40,000-$59,999, $60,000 plus, or missing) and insurance status (none, private, and public). Survey year was coded categorically (2000, 2005, or 2010).
Analysis
All analyses excluding the descriptive analyses in Table 1 were restricted to respondents reporting a lifetime AUD. Preliminary, bivariate analyses were conducted to explore racial/ethnic and gender differences in key variables. We also conducted preliminary regressions to test whether gender interacted with race/ethnicity to affect services utilization, warranting disaggregation by subgroups. Planned follow-up analyses (assuming significant interactions) were hierarchical logistic regressions conducted among men and women separately modeling utilization of any alcohol services, specialty alcohol treatment, and AA as a function of 1) race/ethnicity when controlling for survey year alone, and with 2) demographics, 3) lifetime dependence severity, and 4) social influence variables. This sequence allowed us to assess whether racial/ethnic differences were robust to potential confounds (Models 2 and 3) and independent of or attributable to social influence variables (Model 4). (Controlling for survey alone had no notable effect on coefficients in any model.) Parallel regressions were employed among disaggregated samples of Whites, Latinos, and Blacks to test effects for gender within race/ethnicity. In short, we disaggregated first by gender, in order to examine effects for race/ethnicity, and then by race/ethnicity, to examine effects for gender. Analyses were then supplemented by path models offering more rigorous tests of whether gender disparities were mediated via social influence variables, and which. Data were weighted to account for nonresponse and to approximate the U.S. population at the time the survey was conducted, as indicated by the most recent U.S. Census or American Community Survey data. Core regressions were conducted in Stata (Stata Corp., 2009). Path modeling was conducted in Mplus; mediation tests were conducted within that framework using the available syntax for testing the significance of indirect pathways (MacKinnon et al., 2007; Muthén and Muthén, 2011).
Table 1.
Alcohol use and problems among Whites, Latinos, and Blacks (raw N’s and weighted percentages).
| Men | |||
|---|---|---|---|
|
| |||
| White (N=6113) |
Latino (N=1765) |
Black (N=1414) | |
| % current drinkers | 72.8 (4471) | 67.6 (1141)** | 57.7 (783)*** |
| % 5+ past month | 17.1 (970) | 21.5 (331)* | 12.2 (142)*** |
| % 8+ past month | 9.9 (531) | 12.9 (199)* | 6.5 (74)** |
| % lifetime abuse | 25.0 (1506) | 23.0 (344) | 16.6 (222)*** |
| % lifetime dependence | 15.3 (891) | 19.7 (327)** | 14.6 (209) |
| % current abuse | 6.3 (352) | 8.3 (153) | 6.1 (82) |
| % current dependence | 3.5 (183) | 6.7 (113)*** | 5.2 (51)† |
|
| |||
| Women | |||
|
| |||
| White (N=7358) |
Latina (N=2292) |
Black (N=2596) | |
|
| |||
| % current drinkers | 65.8 (4783) | 43.4 (929)*** | 46.5 (1159)*** |
| % 5+ past month | 5.8 (320) | 3.5 (71)*** | 3.2 (58)*** |
| % 8+ past month | 2.2 (114) | 1.5 (34)† | 0.8 (24)*** |
| % lifetime abuse | 13.3 (862) | 7.9 (157)*** | 9.1 (186)*** |
| % lifetime dependence | 7.9 (529) | 5.6 (121)** | 4.8 (121)*** |
| % current abuse | 3.3 (180) | 3.1 (50) | 3.1 (39) |
| % current dependence | 1.6 (92) | 1.6 (29) | 1.5 (28) |
Notes. p<.001,
p<.01,
p<.05,
p<.10 in pairwise tests with White as the comparison group.
Results
Main Results
Table 1 presents racial/ethnic differences in drinking patterns and problems in the total sample, by gender. This table shows that Latino men, while being less likely than White men to be current drinkers, nevertheless reported higher rates of heavy drinking and alcohol problems across outcomes, excepting lifetime abuse, which was nonsignificantly lower among Latinos than Whites. By contrast, Latina women (who were similarly less likely than White women to be current drinkers) reported lower levels of heavy drinking and alcohol problems across outcomes, excepting current abuse and dependence. Among both men and women, Blacks reported lower odds of any drinking, 5+ drinking, 8+ drinking, and lifetime abuse than Whites; Black women were also lower than White women on lifetime dependence. However, Black men were marginally higher than White men on current dependence.
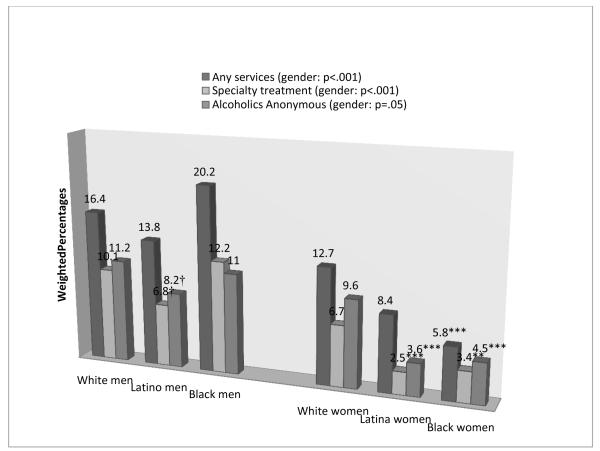
Figure 1 displays racial/ethnic and gender differences in services utilization, here including only those with a lifetime alcohol use disorder (AUD). This figure suggests substantial racial/ethnic disparities, particularly among women. Among men, Latinos were marginally less likely than Whites to report both specialty treatment and participation in Alcoholics Anonymous (AA). Among women, both Latinas and (unexpectedly) Blacks were significantly less likely than Whites to report use of all services, except that the Latina-White difference for any services was nonsignificant. Utilization of specialty treatment and AA among Latinas was just over a third that among White women; utilization among Black women was generally about half that among White women. Overall gender effects were also substantial, with women reporting significantly lower utilization (vs. men) of any services (11.1% vs. 16.3%, p<.001), specialty treatment (6.0% vs. 9.8%, p<.001), and AA (8.7% vs. 10.8%, p=.05).
Figure 1. Alcohol services utilization among Whites, Blacks, and Latinos with a lifetime alcohol use disorder.
Notes. P values for gender in the legend indicate gender comparisons for each of the three outcomes. P values above each bar reference a racial/ethnic comparison within gender for a given outcome using Whites as the referent group. * **p<.001, **p<.01, *p<.05, †p<.10.
Table 2 presents our preliminary, multivariate models of alcohol services utilization among those with a lifetime AUD. Consistent with our hypotheses, this table reveals significantly lower utilization among Latinos (vs. Whites) as well as Blacks (vs. Whites) across outcomes (except for the nonsignificant Latino vs. White effect for any services). Also as predicted, women were significantly lower than men on utilization of any services and specialty treatment. Last, significant race/ethnicity by gender interactions emerged across outcomes. Accordingly, subsequent analyses targeted disaggregated samples.
Table 2.
Overall, unadjusted models of alcohol services utilization among respondents with a lifetime alcohol use disorder.
| Any services |
Specialty alcohol
treatment |
Alcoholics
Anonymous |
||||
|---|---|---|---|---|---|---|
| Predictor | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Race/ethnicity (ref = White) | ||||||
| Latino | 0.63 | 0.33-1.20 | 0.36** | 0.17-0.78 | 0.35** | 0.17-0.72 |
| Black | 0.42*** | 0.25-0.70 | 0.48* | 0.26-0.91 | 0.44** | 0.24-0.81 |
| Male gender | 1.35* | 1.07-1.71 | 1.57** | 1.16-2.11 | 1.18 | 0.91-1.54 |
| Race × gender interactions | ||||||
| Male × Latino | 1.29 | 0.61-2.74 | 1.78 | 0.70-4.51 | 2.05† | 0.89-4.73 |
| Male × Black | 3.05*** | 1.61-5.79 | 2.56* | 1.19-5.48 | 2.23* | 1.07-4.62 |
Notes. p<.001,
p<.01,
p<.05,
p<.10.
Table 3 shows the results of our hierarchical multivariate models testing effects for race/ethnicity among men and women separately. Results indicate no effects for race/ethnicity on services utilization among men when controlling for survey year alone (i.e., Model 1). Nevertheless, Model 2 results show that Latino men were substantially and significantly less likely than White men to report use of specialty treatment and AA when adjusting for demographics. Latino-White disparities were if anything strengthened in subsequent models, including when adjusting for social influence factors, which suggests that social influence factors do not explain Latino-White disparities. Black men did not differ significantly from White men. Among women, Latinas and Blacks displayed substantially lower services utilization than Whites across outcomes in Model 1 (though again, the Latina vs. White effect for any services was not significant). Effects for race/ethnicity among women likewise tended to become stronger when adjusting for demographics and dependence severity, and were generally robust to inclusion of social influence factors, again largely (if not entirely) inconsistent with mediation of disparities via social influence factors. Dovetailing with these findings, exploratory analyses (not shown) revealed few, and mixed, associations between race/ethnicity and social influence factors. Both Latino and Black men reported significantly more work-related consequences than White men, and Black women reported significantly fewer legal consequences than White women. There were no other significant racial/ethnic differences in social influence factors for either gender. Survey effects were nonsignificant across models.
Table 3.
Multivariate models describing effects for race/ethnicity on alcohol services utilization among men and women (separately) with a lifetime alcohol use disorder.
| Men | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Any services |
Specialty alcohol
treatment |
Alcoholics
Anonymous |
||||
| Predictor | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Model 1: Adjusting for Survey Only | ||||||
| Latino (vs. White) | 0.81 | 0.55-1.21 | 0.64 | 0.38-1.09 | 0.71† | 0.47-1.07 |
| Black (vs. White) | 1.29 | 0.88-1.89 | 1.25 | 0.81-1.93 | 0.97 | 0.64-1.47 |
|
| ||||||
| Model 2: Adjusting for Survey and Demographics 1 | ||||||
| Latino (vs. White) | 0.71 | 0.69-1.53 | 0.55* | 0.32-0.94 | 0.59* | 0.36-0.94 |
| Black (vs. White) | 1.03 | 0.46-1.10 | 0.96 | 0.60-1.54 | 0.81 | 0.52-1.26 |
|
| ||||||
| Model 3: Adjusting for Survey, Demographics, and Dependence Severity 2 | ||||||
| Latino (vs. White) | 0.64 | 0.38-1.09 | 0.50* | 0.28-0.88 | 0.55* | 0.31-0.98 |
| Black (vs. White) | 1.15 | 0.68-1.96 | 1.07 | 0.63-1.82 | 0.69 | 0.40-1.19 |
|
| ||||||
| Model 4: Adjusting for Survey, Demographics, Dependence Severity, and Social Influence Variables 3 | ||||||
| Latino (vs. White) | 0.47** | 0.27-0.80 | 0.44** | 0.24-0.81 | 0.52† | 0.27-1.01 |
| Black (vs. White) | 0.95 | 0.60-1.52 | 1.02 | 0.61-1.70 | 0.85 | 0.47-1.53 |
|
| ||||||
| Women | ||||||
|
| ||||||
| Any services |
Specialty alcohol
treatment |
Alcoholics
Anonymous |
||||
| Predictor | OR | 95% CI | OR | 95% CI | OR | 95% CI |
|
| ||||||
| Model 1: Adjusting for Survey Only | ||||||
| Latino (vs. White) | 0.63 | 0.33-1.20 | 0.36** | 0.17-0.78 | 0.34** | 0.16-0.71 |
| Black (vs. White) | 0.42*** | 0.25-0.70 | 0.49* | 0.26-0.92 | 0.43** | 0.24-0.79 |
|
| ||||||
| Model 2: Adjusting for Survey and Demographics 1 | ||||||
| Latino (vs. White) | 0.70 | 0.35-1.40 | 0.36** | 0.17-0.77 | 0.38** | 0.18-0.79 |
| Black (vs. White) | 0.31*** | 0.17-0.56 | 0.38** | 0.19-0.79 | 0.37** | 0.19-0.70 |
|
| ||||||
| Model 3: Adjusting for Survey, Demographics, and Dependence Severity 2 | ||||||
| Latino (vs. White) | 0.68 | 0.29-1.56 | 0.31** | 0.13-0.71 | 0.30** | 0.13-0.71 |
| Black (vs. White) | 0.24** | 0.09-0.66 | 0.41† | 0.16-1.06 | 0.21** | 0.07-0.60 |
|
| ||||||
| Model 4: Adjusting for Survey, Demographics, Dependence Severity, and Social Influence Variables 3 | ||||||
| Latino (vs. White) | 0.36* | 0.16-0.85 | 0.24** | 0.10-0.62 | 0.22** | 0.09-0.57 |
| Black (vs. White) | 0.25** | 0.09-0.70 | 0.59 | 0.26-1.36 | 0.22** | 0.07-0.67 |
Notes. Demographic variables include age, age-squared, education, income, insurance status.
Dependence severity measured as total count of lifetime dependence symptoms.
Social influence variables include lifetime social pressures (sum of 6-item scale), lifetime legal consequences (any vs. none of 3), and lifetime work-related consequences (any vs. none of 3).
p<.001,
p<.01,
p<.05,
p<.10.
Table 4 displays the results of our hierarchical multivariate models testing gender effects among Whites, Latinos, and Blacks separately. Results show that women reported considerably lower services utilization than men across outcomes and across racial/ethnic groups, although gender differences were nonsignificant for AA among Whites and any services among Latinos. Gender effects were strongest among Blacks and weakest among Whites. Results from the final models show however that, when adjusting for all covariates, gender effects were reduced to nonsignificance (excepting one marginal effect) across race/ethnicity and across outcomes. Among Whites, social influence factors exclusively drove reductions in gender effects; gender effects were actually strengthened when accounting for demographics, and unaffected by controlling for dependence severity. Social influence factors likewise contributed to explaining gender effects on use of services among Latinos, though estimates from Models 2 and 3 show that demographic variables and dependence severity also contributed to gender disparities in this group. Among Blacks, social influence factors again made important contributions to explaining gender effects; similar to Whites, parameter estimates were strengthened when accounting for demographics and little affected by dependence severity. (Still, estimates representing gender effects among Latinos and Blacks remained large in the final models, if not significant.) Survey effects were again nonsignificant across models, except that among Whites, respondents reported significantly greater AA utilization in 2000 (OR=1.57, p<.05) and 2005 (OR=2.01, p<.01), compared to 2010.
Table 4.
Multivariate models describing effects for gender on alcohol services utilization among Whites, Latinos, and Blacks (separately) with a lifetime alcohol use disorder.
| Whites | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Any services |
Specialty alcohol
treatment |
Alcoholics
Anonymous |
||||
| Predictor | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Model 1: Adjusting for Survey Only | ||||||
| Male (vs. female) | 1.35* | 1.07-1.71 | 1.58** | 1.17-2.13 | 1.18 | 0.90-1.54 |
|
| ||||||
| Model 2: Adjusting for Survey and Demographics 1 | ||||||
| Male (vs. female) | 1.49*** | 1.17-1.91 | 1.80*** | 1.30-2.49 | 1.29† | 0.97-1.71 |
|
| ||||||
| Model 3: Adjusting for Survey, Demographics, and Dependence Severity 2 | ||||||
| Male (vs. female) | 1.47** | 1.11-1.95 | 1.78*** | 1.25-2.53 | 1.11 | 0.78-1.58 |
|
| ||||||
| Model 4: Adjusting for Survey, Demographics, Dependence Severity, and Social Influence Variables 3 | ||||||
| Male (vs. female) | 0.93 | 0.69-1.27 | 1.02 | 0.70-1.47 | 0.82 | 0.56-1.20 |
|
| ||||||
| Latinos | ||||||
|
| ||||||
| Any services |
Specialty alcohol
treatment |
Alcoholics
Anonymous |
||||
| Predictor | OR | 95% CI | OR | 95% CI | OR | 95% CI |
|
| ||||||
| Model 1: Adjusting for Survey Only | ||||||
| Male (vs. female) | 1.75 | 0.85-3.58 | 2.80* | 1.16-6.72 | 2.43* | 1.10-5.36 |
|
| ||||||
| Model 2: Adjusting for Survey and Demographics 1 | ||||||
|
| ||||||
| Male (vs. female) | 1.53 | 0.74-3.13 | 2.33† | 0.99-5.47 | 1.97† | 0.89-4.38 |
|
| ||||||
| Model 3: Adjusting for Survey, Demographics, and Dependence Severity 2 | ||||||
| Male (vs. female) | 1.51 | 0.72-3.19 | 2.49† | 0.97-6.36 | 1.76 | 0.73-4.28 |
|
| ||||||
| Model 4: Adjusting for Survey, Demographics, Dependence Severity, and Social Influence Variables 3 | ||||||
| Male (vs. female) | 1.07 | 0.47-2.44 | 2.24 | 0.66-7.60 | 1.74 | 0.66-4.58 |
|
| ||||||
| Blacks | ||||||
|
| ||||||
| Any services |
Specialty alcohol
treatment |
Alcoholics
Anonymous |
||||
| Predictor | OR | 95% CI | OR | 95% CI | OR | 95% CI |
|
| ||||||
| Model 1: Adjusting for Survey Only | ||||||
| Male (vs. female) | 4.29*** | 2.27-8.06 | 4.01*** | 1.93-8.37 | 2.78** | 1.37-5.66 |
|
| ||||||
| Model 2: Adjusting for Survey and Demographics 1 | ||||||
| Male (vs. female) | 5.24*** | 2.40-11.43 | 4.30*** | 1.80-10.23 | 3.16** | 1.37-7.27 |
|
| ||||||
| Model 3: Adjusting for Survey, Demographics, and Dependence Severity 2 | ||||||
| Male (vs. female) | 5.46*** | 2.32-12.85 | 4.23** | 1.55-11.54 | 2.78* | 1.08-7.14 |
|
| ||||||
| Model 4: Adjusting for Survey, Demographics, Dependence Severity, and Social Influence Variables 3 | ||||||
| Male (vs. female) | 2.29† | 0.94-5.55 | 1.53 | 0.62-3.74 | 2.02 | 0.61-6.80 |
Notes. Demographic variables include age, age-squared, education, income, insurance status.
Dependence severity measured as total count of lifetime dependence symptoms.
Social influence variables include lifetime social pressures (sum of 6-item scale), lifetime legal consequences (any vs. none of 3), and lifetime work-related consequences (any vs. none of 3).
p<.001,
p<.01,
p<.05,
p<.10.
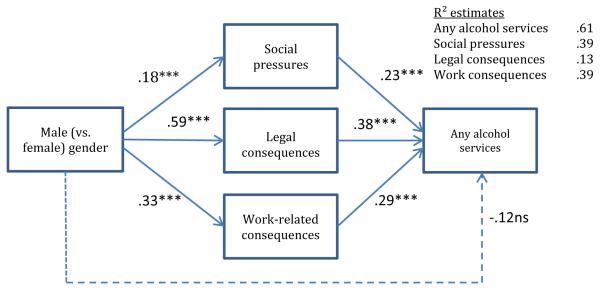
Given the above results tentatively suggesting mediation of gender disparities via social influence factors, a final set of analyses was conducted to more rigorously examine mediation. Specifically, we conducted sequential path models in Mplus examining indirect effects for gender via our proposed mediators (i.e., social pressures, legal consequences, and work-related consequences) for each of our three outcomes (i.e., any services, specialty treatment, and AA) separately among all three racial/ethnic groups, yielding nine models. Pathways from gender to each mediator controlled for lifetime AUD severity, while pathways from each mediator to the outcome controlled for all variables used in the final step of the multivariate analyses reported in Tables 3 and 4. Results supported the above findings. Among Whites, significant indirect pathways emerged linking gender to services utilization via all three mediators for all three outcomes (all p’s<.05); further, for both any services and specialty treatment, the direct pathway from gender to the dependent variable was nonsignificant, indicating full mediation (see Figure 2, depicting any services; additional results available upon request). Among both Latinos and Blacks, significant indirect pathways emerged linking gender to services utilization via legal consequences only, again for all three outcomes (all p’s<.05). In several cases, the direct effects for gender were again nonsignificant, though a conclusion of full mediation may not be justified given the relatively small samples of Latinos and Blacks.
Figure 2. Path model illustrating mediation of gender disparities via social influence factors among Whites.
Notes. All equations control for lifetime dependence severity. Model predicting any alcohol services also controls for age, age-squared, education, income, insurance status, and survey. X2 (42, 3601)=169.28, p<.001, RMSEA=.029 (.024, .033), CFI=.95, TLI=.92. ***p<.001, ns nonsignificant.
Discussion
Summary and Implications
Results from the current study partially confirm and extend prior findings of racial/ethnic disparities in alcohol services utilization among those with a lifetime alcohol use disorder (AUD). Findings from the most comparable studies—that is, national studies of alcohol services utilization—provide some evidence of lower utilization among Latinos than Whites, but mixed and generally weak results for Black-White comparisons (Chartier and Caetano, 2011; Keyes et al., 2008; Mulia et al., 2014; Schmidt et al., 2007). Our results suggest that these analyses mask important differences across genders. We found substantially and significantly lower services utilization among both Latina and Black (vs. White) women across outcomes (i.e., any services, specialty treatment, and Alcoholics Anonymous, or AA) and across bivariate and multivariate analyses, with only two exceptions, where parameter estimates were in a direction consistent with the other effects. Moreover, if anything, effects for Latina and Black (vs. White) race/ethnicity among women tended to become stronger in analyses controlling for demographics and dependence severity. By contrast, overall Latino-White disparities were weak and nonsignificant among men, and Black men reported nonsignificantly greater utilization of any services and specialty treatment than White men, which may reflect coercion. Still, multivariate analyses revealed significantly lower utilization among Latino (vs. White) men across outcomes when accounting for demographics and Latinos’ (greater) dependence severity.
Congruent with prior research, we also found that female gender was associated with much lower utilization across outcomes. Gender differences held across race/ethnicity, but were strongest among Blacks, followed by Latinos and then Whites. Latina women were thus at highest risk for unmet treatment need, followed by Black women, and then by White women and Latino men. Race and gender operated together to produce exceptionally large disparities. For example, only 2.5% of Latinas with a lifetime AUD accessed specialty treatment, compared to 3.4% of Black women, 6.7% of White women, 6.8% of Latino men, 10.1% of White men, and 12.2% of Black men. Our study is the first known national study to establish that gender may moderate racial/ethnic disparities in alcohol services utilization. Our effects argue for greater attention to gender in considering racial/ethnic disparities, and likewise to race/ethnicity in interpreting gender effects.
Multivariate analyses suggested that the racial/ethnic disparities above were not explained by measured social influence factors (or other potential confounds studied here). As noted in the introduction, a range of barriers may be elevated among Latinos and Blacks that were not addressed here (Perron et al., 2009; Rouse et al., 1995; Schmidt et al., 2007; Zemore et al., 2009). It may also be that unmeasured social influence factors, such as physician suggestions/referral to treatment, contribute to racial/ethnic disparities in service utilization.
Multivariate and path analyses relating to gender effects, on the other hand, suggested that diminished social influence of all three types (i.e., social pressures, legal consequences, and work-related consequences) strongly contribute to gender disparities in services utilization for Whites, while diminished legal consequences contribute to gender disparities among Blacks and Latinos. Effects held even controlling for demographics and dependence severity. These findings are consistent with studies suggesting that the social consequences of alcohol use are even more powerful predictors of services utilization than dependence severity (Kaskutas et al., 1997; Weisner et al., 1995). Results are highly meaningful in the context of existing theory on gender differences in services use, which has (relying heavily on treatment samples) emphasized low problem recognition, low treatment acceptability, childcare issues, and alcoholism stigma especially (Brienza and Stein, 2002; Schober and Annis, 1996; Thom, 1986). While these factors may indeed be important, particularly following treatment initiation, they may not be the primary or most proximal barriers to help seeking. Still, social influence factors may well relate to both stigma and problem recognition. Specifically, stigma may provoke the concealment of alcohol problems among women, encouraging social isolation and/or affiliation with other heavy drinkers, diminishing the likelihood of problem recognition and help seeking. Consistent with this reasoning, evidence does suggest that female dependent drinkers are more likely than males to hide their drinking, more likely to partner with other alcohol/drug abusers, and less likely to define drinking as their main problem (Jordan and Oei, 1989; Smith, 1992; Thom, 1986). These pathways should be explored in further research.
Limitations and Final Conclusions
One limitation is that the survey response rate was only moderate. However, as suggested in the Methods, methodological studies somewhat allay concerns regarding representivity. Second, our sample was not sufficiently large to allow for separate examination of NAS surveys, and necessitated collapsing across 2000-2010. Accordingly, our conclusions regarding racial/ethnic and gender disparities (and the mechanisms behind them) should ideally be verified in future research. Relatedly, our study was under-powered to examine differences in services utilization by Latino subgroup and acculturation. Additionally, the current study is based on self-report. Biases in reporting, particularly if associated with race/ethnicity, could thus affect the results. Finally, the cross-sectional design is not optimal for establishing the temporal ordering of associations between AUD development, exposure to social influence, and use of alcohol services.
Nevertheless, the present study is unique in that it uses recent, national data to simultaneously consider racial/ethnic and gender disparities, each in the context of the other. Findings for substantial racial/ethnic disparities among women highlight the need for continuing research on factors that may explain such disparities and constitute targets for intervention. Strong and historically persistent gender disparities, combined with the current results suggesting a role for social influence factors in perpetuating these disparities, suggest a need for outreach to female dependent drinkers and their social networks. Because female dependent drinkers do not generally elicit the same level of social consequences as male dependent drinkers, interventions may be necessary to increase problem recognition and perceived need for help in this population.
Acknowledgments
Funding: This work was funded by the National Institute on Alcohol Abuse and Alcoholism (P50AA005595, R01AA020474, and R01AA017197).
Footnotes
Conflict of interest: None.
The terms “specialty alcohol/drug treatment programs” and “specialty treatment” refer in this paper to inpatient or outpatient substance use rehabilitation programs; detoxification alone does not qualify as specialty treatment. Studies have measured utilization of specialty treatment using self-report questions similar to those used in the current study (Chartier and Caetano, 2011; Schmidt et al., 2007); see Measures.
References
- American Psychiatric Association . DSM-IV: Diagnostic & Statistical Manual of Mental Disorders. 4th ed American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Brienza RS, Stein MD. Alcohol use disorders in primary care: do gender-specific differences exist? J Gen Intern Med. 2002;17(5):387–397. doi: 10.1046/j.1525-1497.2002.10617.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caetano R. Alcohol-related health disparities and treatment-related epidemiological findings among whites, black, and Hispanics in the United States. Alcohol Clin Exp Res. 2003;27(8):1337–1339. doi: 10.1097/01.ALC.0000080342.05229.86. [DOI] [PubMed] [Google Scholar]
- Caetano R, Clark CL. Trends in alcohol-related problems among whites, blacks, and Hispanics: 1984-1995. Alcohol Clin Exp Res. 1998;22(2):534–538. [PubMed] [Google Scholar]
- Caetano R, Clark CL, Tam TW. Alcohol consumption among racial/ethnic minorities: theory and research. Alcohol Health Res World. 1998;22(4):233–241. [PMC free article] [PubMed] [Google Scholar]
- Caetano R, Tam TW. Prevalence and correlates of DSM-IV and ICD-10 alcohol dependence: 1990 U.S. National Alcohol Survey. Alcohol Alcohol. 1995;30(2):177–186. [PubMed] [Google Scholar]
- Chartier K, Caetano R. Ethnicity and health disparities in alcohol research. Alcohol Res Hlth. 2010;33(1-2):152–160. [PMC free article] [PubMed] [Google Scholar]
- Chartier KG, Caetano R. Trends in alcohol services utilization from 1991-1992 to 2001-2002: ethnic group differences in the U.S. population. Alcohol Clin Exp Res. 2011;35(8):1485–1497. doi: 10.1111/j.1530-0277.2011.01485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook BL, Alegría M. Racial-ethnic disparities in substance abuse treatment: the role of criminal history and socioeconomic status. Psychiatr Serv. 2011;62(11):1273–1281. doi: 10.1176/appi.ps.62.11.1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA. Gender differences in the probability of alcohol treatment. J Subst Abuse. 1996;2(8):211–225. doi: 10.1016/s0899-3289(96)90260-6. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100(3):281–292. doi: 10.1111/j.1360-0443.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- Emrick CD, Tonigan JS, Montgomery HA, Little L. Rutgers Center of Alcohol Studies. New Brunswick, NJ: 1993. Alcoholics Anonymous: what is currently known?, in Research on Alcoholics Anonymous: Opportunities and alternatives, McCrady BS, Miller WR eds, pp 41-78. [Google Scholar]
- Flores YN, Yee HF, Jr., Leng M, Escare JJ, Bastani R, Salmerón J, et al. Risk factors for chronic liver disease in blacks, Mexican Americans, and whites in the United States: results from NHANES IV, 1999-2004. American Journal of Gastroenterology. 2008;103(9):2231–2238. doi: 10.1111/j.1572-0241.2008.02022.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomberg ESL. In: Treatment for alcohol-related problems: special populations: research opportunities, in Recent Developments in Alcoholism. Galanter M, editor. Vol. 16. Plenum Press; New York: 2003. pp. 313–333. [DOI] [PubMed] [Google Scholar]
- Greenfield TK. Evaluating competing models of alcohol-related harm. Alcohol Clin Exp Res. 1998;22(Suppl. 2):52S–62S. doi: 10.1097/00000374-199802001-00008. [DOI] [PubMed] [Google Scholar]
- Hasin DS. Treatment/self-help for alcohol-related problems: relationship to social pressure and alcohol dependence. J Stud Alcohol. 1994;55(6):660–666. doi: 10.15288/jsa.1994.55.660. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Grant BF. The co-occurrence of DSM-IV alcohol abuse in DSM-IV alcohol dependence: results of the National Epidemiologic Survey on Alcohol and Related conditions on heterogeneity that differ by population subgroup. Arch Gen Psychiatry. 2004;61(9):891–896. doi: 10.1001/archpsyc.61.9.891. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Price AM, Burnett-Zeigler I, Perron B, Islam K, Bohnert ASB, et al. Longitudinal predictors of addictions treatment utilization in treatment-naïve adults with alcohol use disorders. Drug Alcohol Depend. 2011;113(2-3):215–221. doi: 10.1016/j.drugalcdep.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan CM, Oei TPS. Help-seeking behavior in problem drinkers: a review. Br J Addict. 1989;84:979–988. doi: 10.1111/j.1360-0443.1989.tb00778.x. [DOI] [PubMed] [Google Scholar]
- Kandel D, Chen K, Warner LA, Kessler RC, Grant B. Prevalence and demographic correlates of symptoms of last year dependence on alcohol, nicotine, marijuana and cocaine in the U.S. population. Drug Alcohol Depend. 1997;44(1):11–29. doi: 10.1016/s0376-8716(96)01315-4. [DOI] [PubMed] [Google Scholar]
- Kaskutas LA, Weisner C, Caetano R. Predictors of help seeking among a longitudinal sample of the general population, 1984-1992. J Stud Alcohol. 1997;58(2):155–161. doi: 10.15288/jsa.1997.58.155. [DOI] [PubMed] [Google Scholar]
- Kerr WC, Greenfield TK, Bond J, Ye Y, Rehm J. Age, period and cohort influences on beer, wine and spirits consumption trends in the US National Surveys. Addiction. 2004;99(9):1111–1120. doi: 10.1111/j.1360-0443.2004.00820.x. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Hatzenbuehler ML, Alberti P, Narrow WE, Grant BF, Hasin DS. Service utilization difference for axis I psychiatric and substance use disorders between white and black adults. Psychiatr Serv. 2008;59(8):893–901. doi: 10.1176/appi.ps.59.8.893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Liu XC, Cerda M. The role of race/ethnicity in alcohol-attributible injury in the United States. Epidemiol Rev. 2012;34(1):89–102. doi: 10.1093/epirev/mxr018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korcha RA, Polcin DL, Kerr WC, Greenfield TK, Bond J. Pressure and help seeking for alcohol problems: trends and correlates from 1984 to 2005. Addict Behav. 2013;38(3):1740–1746. doi: 10.1016/j.addbeh.2012.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Brown CH, Wang W, Hoffman JM. The intermediate endpoint effect in logistic and probit regression. Clinical Trials. 2007;4(5):499–513. doi: 10.1177/1740774507083434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrady BS, Miller WR, editors. Research on Alcoholics Anonymous: Opportunities and alternatives. Rutgers University Press; New Brunswick, NJ: 1993. [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. The Journal of the American Medical Association. 2000;284(13):1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- Midanik LT, Greenfield TK. Telephone versus in-person interviews for alcohol use: results of the 2000 National Alcohol Survey. Drug Alcohol Depend. 2003;72(3):209–214. doi: 10.1016/s0376-8716(03)00204-7. [DOI] [PubMed] [Google Scholar]
- Mojtabai R. Use of specialty substance abuse and mental health services in adults with substance use disorders in the community. Drug Alcohol Depend. 2005;78(3):345–354. doi: 10.1016/j.drugalcdep.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Mojtabai R, Crum RM. Perceived unmet need for alcohol and drug use treatments and future use of services: results from a longitudinal study. Drug Alcohol Depend. 2013;127(1-3):59–67. doi: 10.1016/j.drugalcdep.2012.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mplus. version 6.11 Muthén & Muthén; Los Angeles, CA: 2011. [Google Scholar]
- Mulia N, Tam TW, Schmidt LA. Disparities in the use and quality of alcohol treatment services and some proposed solutions to narrow the gap. Psychiatric Services. 2014 doi: 10.1176/appi.ps.201300188. doi: 10.1176/appi.ps.201300188 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naimi TS, Nelson DE, Brewer RD. The intensity of binge alcohol consumption among U.S. adults. Am J Prev Med. 2010;38(2):201–207. doi: 10.1016/j.amepre.2009.09.039. [DOI] [PubMed] [Google Scholar]
- Neff JA. Solitary drinking, social isolation, and escape drinking motivates as predictors of high quantity drinking, among anglo, African American and Mexican American males. Alcohol Alcohol. 1997;32(1):33–41. doi: 10.1093/oxfordjournals.alcalc.a008232. [DOI] [PubMed] [Google Scholar]
- Perron BE, Mowbray OP, Glass JE, Delva J, Vaughn MG, Howard MO. Differences in service utilization and barriers among blacks, Hispanics, and whites with drug use disorders. Substance Abuse Treatment, Prevention, and Policy. 2009;4(3) doi: 10.1186/1747-597X-4-3. online journal. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL, Beattie M. Relationship and institutional pressure to enter treatment: differences by demographics, problem severity, and motivation. J Stud Alcohol Drugs. 2007;68(3):428–436. doi: 10.15288/jsad.2007.68.428. [DOI] [PubMed] [Google Scholar]
- Polcin DL, Korcha R, Greenfield TK, Kerr WC, Bond JC. Twenty-one year trends and correlates of pressure to change drinking Alcohol Clin Exp Res. 2012;36(4):705–715. doi: 10.1111/j.1530-0277.2011.01638.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL, Weisner C. Factors associated with coercion in entering treatment for alcohol problems. Drug Alcohol Depend. 1999;54(1):63–68. doi: 10.1016/s0376-8716(98)00143-4. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group Matching alcoholism treatment to client heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997;58(1):7–29. [PubMed] [Google Scholar]
- Room R, Greenfield TK, Weisner C. People who might have liked you to drink less: changing responses to drinking by U.S. family members and friends, 1979-1990. Contemp Drug Prob. 1991;18(4):573–595. [Google Scholar]
- Rouse BA, Carter JH, Rodriquez-Andrew S. In: Race/ethnicity and other sociocultural influences on alcholism treatment for women, in Recent developments in alcoholism. Galanter M, editor. Plenum; New York: 1995. pp. 343–367. [DOI] [PubMed] [Google Scholar]
- Schmidt LA, Ye Y, Greenfield TK, Bond J. Ethnic disparities in clinical severity and services for alcohol problems: results from the National Alcohol Survey. Alcohol Clin Exp Res. 2007;31(1):48–56. doi: 10.1111/j.1530-0277.2006.00263.x. [DOI] [PubMed] [Google Scholar]
- Schober R, Annis HM. Barriers to help-seeking for change in drinking: a gender-focused review of the literature. Addict Behav. 1996;21(1):81–92. doi: 10.1016/0306-4603(95)00041-0. [DOI] [PubMed] [Google Scholar]
- Smith L. Help seeking in alcohol-dependent females. Alcohol Alcohol. 1992;27(1):3–9. [PubMed] [Google Scholar]
- Stata Statistical Software: Release 11.0. Stata Corporation; College Station, TX: 2009. [Google Scholar]
- Thom B. Sex differences in help-seeking for alcohol problems: 1. the barriers to help-seeking. Br J Addict. 1986;81:777–788. doi: 10.1111/j.1360-0443.1986.tb00405.x. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Toscova R, Miller WR. Meta-analysis of the literature on Alcoholics Anonymous: sample and study characteristics moderate findings. J Stud Alcohol. 1996;57(1):65–72. doi: 10.15288/jsa.1996.57.65. [DOI] [PubMed] [Google Scholar]
- Vaeth PAC, Caetano R, Ramisetty-Mikler S, Rodriguez LA. Hispanic Americans Baseline Alcohol Survey (HABLAS): alcohol-related problems across Hispanic national groups. J Stud Alcohol Drugs. 2009;70(6):991–999. doi: 10.15288/jsad.2009.70.991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisner C. The alcohol treatment-seeking process from a problems perspective: responses to events. Br J Addict. 1990;85(4):561–569. doi: 10.1111/j.1360-0443.1990.tb01677.x. [DOI] [PubMed] [Google Scholar]
- Weisner C, Greenfield TK, Room R. Trends in the treatment of alcohol problems in the U.S. general population, 1979 through 1990. Am J Public Health. 1995;85(1):55–60. doi: 10.2105/ajph.85.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisner C, Matzger H, Tam TW, Schmidt L. Who goes to alcohol and drug treatment? Understanding utilization within the context of insurance. J Stud Alcohol. 2002;63(6):673–682. doi: 10.15288/jsa.2002.63.673. [DOI] [PubMed] [Google Scholar]
- Zemore SE, Karriker-Jaffe KJ, Mulia N. Temporal trends and changing racial/ethnic disparities in alcohol problems: results from the 2000 to 2010 National Alcohol Surveys. Journal of Addiction Research and Therapy. 2013;4(4):160. doi: 10.4172/2155-6105.1000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore SE, Mulia N, Ye Y, Borges G, Greenfield TK. Gender, acculturation, and other barriers to alcohol treatment utilization among Latinos in three National Alcohol Surveys. J Subst Abuse Treat. 2009;36(4):446–456. doi: 10.1016/j.jsat.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]