Abstract
Background and Purpose
Mexican Americans (MAs) were previously found to have lower mortality following ischemic stroke than non Hispanic Whites (NHWs). We studied mortality trends in a population-based design.
Methods
Active and passive surveillance were used to find all ischemic stroke cases from January, 2000–December, 2011 in Nueces County, Texas. Deaths were ascertained from the Texas Department of Health through December 31 2012. Cumulative 30-day and 1 year mortality adjusted for covariates was estimated using log-binomial models with a linear term for year of stroke onset used to model time trends. Models used data from the entire study period to estimate adjusted mortality among stroke cases in 2000 and 2011, and to calculate projected ethnic differences.
Results
There were 1,974 ischemic strokes among NHWs and 2,439 among MAs. Between 2000 and 2011, model estimated mortality declined among NHWs at 30 days (7.6% to 5.6%, p=0.24) and 1 year (20.8% to 15.5%, p=0.02). Among MAs, 30-day model estimated mortality remained stagnant at 5.1% to 5.2% (p=0.92), and a slight decline from 17.4% to 15.3% was observed for 1 year mortality (p=0.26). While ethnic differences in 30-day (p=0.01) and 1 year (p=0.06) mortality were apparent in 2000, they were not so in 2011 (30-day, p=0.63; 1 year p=0.92).
Conclusions
Overall, mortality following ischemic stroke has declined in the last decade, although significant declines were only observed for NHWs and not MAs at 1 year. The survival advantage previously documented among MAs vanished by 2011. Renewed stroke prevention and treatment efforts for MAs are needed.
Keywords: Hispanic, Mortality, trends
Hispanic Americans are the largest minority population in the US, and Mexican Americans (MAs) are the largest sub-group comprising 63% of Hispanic Americans1. In 2010, 50.5 million Hispanics comprised 16% of the US population, an increase of 35 million since 2000, with MAs making up 75% of the growth2. Hispanic Americans are projected to comprise one-third of the US population in 2060. In 2010, just 7% of the Hispanic American population was ≥65 years; this is expected to rise to 20% by 20503 indicating the potential for a large increase in stroke among Hispanic Americans in the coming decades.
The “Hispanic Paradox” is the observation that despite increased risk factors, comorbidities and worse access to care, Hispanic Americans have lower case fatality compared with non Hispanic whites (NHWs) for a number of diseases including stroke4. We previously reported a 42% lower 28-day ischemic stroke case fatality rate and a 21% lower all-cause mortality rate following ischemic stroke in Mexican Americans (MAs) compared with NHWs in a population-based study4.
While many have tried to explain the Hispanic Paradox with everything from genetics to increased social support5, we wondered if the effect was changing over time. Using an urban, non-immigrant community of MAs and NHWs we examined population-based trends in mortality following stroke.
METHODS
This was a primary pre-specified analysis of the Brain Attack Surveillance in Corpus Christi (BASIC) project. The methods were previously published6 and are summarized here. The University of Michigan and Corpus Christi hospitals’ IRBs approved this project.
Setting and Subjects
BASIC takes place in Nueces County, on the Texas Gulf Coast, and 89% of residents reside in the city of Corpus Christi7. The population is stable, non-immigrant and composed of US citizens. There are few undocumented residents making return to Mexico following stroke for long-term care or other reasons unlikely. There are 6 acute care hospitals, all with advanced neuroimaging and neurology consultation. Ethnicity (MA and NHW) is obtained from the medical record. We previously reported 96% agreement between self-report and chart abstracted ethnicity in this community8. Over the years, surveillance techniques including out of hospital and coroner inquiries have supplemented the rigorous active and passive surveillance used to capture all acute strokes in the population6. Cases are validated by stroke physicians based on source documentation blinded to ethnicity and age.
Mortality Determination
Deaths from all causes were identified from: 1) routine active and passive surveillance of all hospital and Emergency Department deaths, and 2) Texas Department of Health (TDH) death certificate database for the state of Texas. First name, last name, date of birth and permanent address, were crossed-referenced with the TDH database. At least three of the five items had to be identical for the BASIC stroke case to be considered a match with the TDH death data. Cases were ascertained between January 1, 2000 and December 31, 2011 and mortality data were completed through December 2012, such that there was no censoring for either 30 day or 1 year mortality.
Statistical Analysis
Descriptive statistics for all patient characteristics were computed overall and by ethnicity, and ethnic comparisons were derived using chi-squared or Kolmogorov-Smirnov two sample tests for categorical or continuous variables, respectively. Descriptive statistics were also calculated yearly, and we examined trends in risk factors over the study period using linear or log-binomial regression models using time since 2000 as a continuous variable. We examined if risk factor trends differed by ethnicity by including an interaction term between a binary ethnicity indicator and years since 2000 in these models.
Since 30 day or 1 year mortality was fully observed (no censoring), and mortality was high among some subgroups, log-Binomial regression models (versus Cox or logistic regression models) were used to examine trends in cumulative 30-day and 1-year mortality9. Log binomial models have the benefit of directly estimating risk ratios, instead of approximating risk ratios with odds ratios. A linear term of year since 2000 was included in the model to capture the overall trend in mortality, and its interaction with a binary ethnicity indicator was used to test if the trend differed by ethnicity. Models were estimated adjusting for: sex, quartiles of the age distribution (45–60, 61–72, 73–81 and >81), diabetes, coronary artery disease, high cholesterol, history of stroke/TIA, atrial fibrillation, hypertension, smoking status, insurance status, and stroke severity (NIHSS, categories 0–1, 2–3, 4–7, 8–11, 12–42). Age (quartiles) and NIHSS (five groups) were treated as categorical variables since they demonstrated non-linear associations with mortality in crude models. Further, since confounding of the ethnicity by time interaction coefficient is possible (i.e., confounding on the effect modification scale), we also empirically selected additional terms to be added into the model out of a list of interaction terms of the above risk factors and time, or the risk factors and ethnicity. Specifically, for the 30 day model, the interaction terms between year since 2000 and atrial fibrillation, NIHSS, age, insurance status were included; as well as the interaction terms of ethnicity and atrial fibrillation, coronary artery disease, hypertension, and smoking status. For the 1 year model the interactions of year since 2000 and atrial fibrillation and hypertension were included; and the interactions between ethnicity and coronary artery disease, hypertension and smoking status. For interpretation, we estimated adjusted mortality trends by ethnicity for individuals with average age and otherwise average population characteristics. We used the coefficients from models fitted to data from the entire study period to estimate: mortality risk in 2000 and 2011 by ethnicity; mortality risk ratios for ethnicity in 2000 or 2011; mortality trends by ethnicity; and ethnic differences in the mortality trends. Therefore, rather than using the individual rates for each year, we used the model which incorporates rates from all years to calculate the estimated rates for each year based on the trend lines.
In the fully adjusted models, the mortality-age association did not deviate significantly from linearity, and a linear term for age was thus used in the sensitivity analysis. We also conducted sensitivity analyses modeling age and NIHSS continuously using splines to examine if results could be attributed to residual confounding within age or severity categories. Finally, model coefficients for ethnicity, time since 2000, and ethnicity by time since 2000 were used to extrapolate mortality trend lines beyond our study period to enable us to calculate the year when the ethnicity risk ratios estimated for the year 2000 would be reversed.
RESULTS
There were 4,413 ischemic stroke cases, 1,974 (44.7%) in NHWs and 2,439 (55.2%) in MAs. Of these, there was missing covariate data on 99 (2.2%) and they were excluded from the model calculations. In aggregate, over the study period MAs were younger, and had more diabetes and hypertension; while NHWs had a higher prevalence of atrial fibrillation and smoking, and were more likely to be insured (Table 1). The Supplementary Figure I provides data on trends in demographics and risk factors among stroke cases over the study period. The trends in risk factors did not differ by ethnicity (p>0.05 for all time by ethnicity interactions). Across the observation period, the total 30 day case fatality was 12.9% (95% CI: 11.9%, 13.9%) among NHWs and 8.2% (95% CI: 7.4%, 9%) among MAs. Total one year mortality was 27.0% (95% CI: 25.7%, 28.3%) among NHWs and 20.7% (95% CI: 19.5%, 21.9%) among MAs. Supplementary Table I provides the raw NIHSS, 30 day and one year mortality data by age category and ethnicity.
Table 1.
Descriptive statistics of study population aggregated throughout the study.
| All (N=4,413) | MA (N=2,439) | NHW (N=1,974) | p* | |
|---|---|---|---|---|
| Age in years, median (Q1, Q3) | 72 (61,81) | 69 (58,78) | 76 (65,83) | <0.001 |
| Age, % | ||||
| 45–60 | 24.8 | 30.8 | 17.3 | <0.001 |
| 61–72 | 26.2 | 28.7 | 23.1 | |
| 73–81 | 25.4 | 22.9 | 28.5 | |
| >81 | 23.6 | 17.6 | 31.1 | |
| Atrial Fibrillation, % | 15.0 | 10.5 | 20.5 | <0.001 |
| Coronary Artery Disease, % | 32.9 | 32.5 | 33.4 | 0.52 |
| Diabetes Mellitus, % | 41.4 | 54.2 | 25.4 | <0.001 |
| Excessive ETOH, % | 5.7 | 6.1 | 5.3 | 0.27 |
| Sex, % female | 51.3 | 50.7 | 52.1 | 0.37 |
| High Cholesterol, % | 33.5 | 34.3 | 32.5 | 0.19 |
| Hypertension, % | 76.8 | 78.8 | 74.4 | <0.001 |
| NHISS, median (Q1, Q3) | 4 (2,8) | 4 (2,8) | 4 (2,8) | 0.05 |
| NIHSS, % | 0.09 | |||
| 0–1 | 20.4 | 20.3 | 20.5 | |
| 2–3 | 24.7 | 25.0 | 24.4 | |
| 4–7 | 27.9 | 29.1 | 26.4 | |
| 8–11 | 12.6 | 12.4 | 12.8 | |
| 12–42 | 14.4 | 13.3 | 15.8 | |
| Smoking status, % | <0.001 | |||
| Current | 19.4 | 18.7 | 20.3 | |
| Former | 13.0 | 10.7 | 15.9 | |
| Never | 67.6 | 70.6 | 63.8 | |
| Any insurance, % | 89.7 | 86.9 | 93.2 | <0.001 |
| History of stroke or TIA, % | 29.8 | 29.4 | 30.3 | 0.52 |
| Cumulative 30 day mortality | 10.3 | 8.2 | 12.9 | <0.001 |
| Cumulative 1 year mortality | 23.5 | 20.7 | 27.0 | <0.001 |
Chi-square test or KM test for equality of distribution (continuous age, continuous NIHSS)
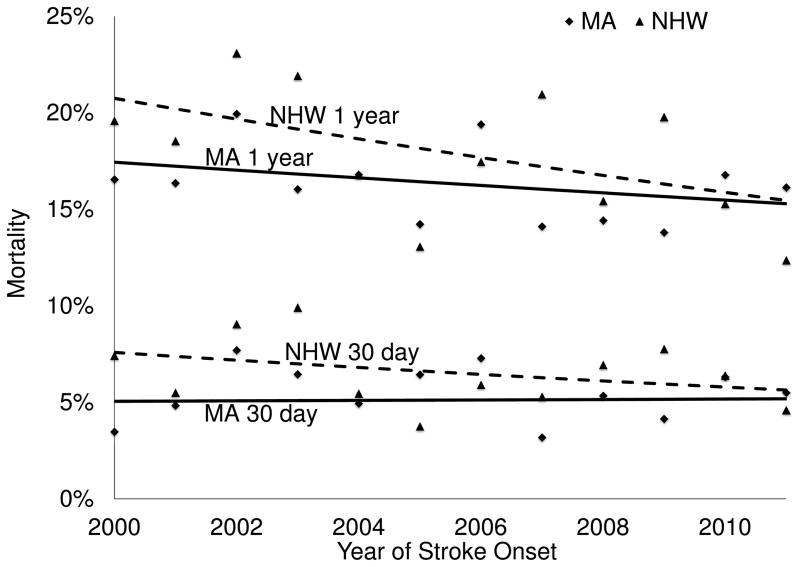
Between 2000 and 2011, the model predicted mortality for an average patient declined among NHWs at 30 days (7.6% to 5.6%, p=0.24) and 1 year (20.8% to 15.5%, p=0.02). Among MAs, 30-day model predicted mortality remained stagnant at 5.1% to 5.2% (p=0.92), and a slight decline from 17.4% to 15.3% was observed for 1 year mortality (p=0.26) (Table 2). While ethnic differences in 30-day (p=0.014) and 1 year (p=0.06) mortality were apparent in 2000, they were not so in 2011 (30-day, p=0.63; 1 year p=0.92). Figure 1 demonstrates the loss of the MA survival advantage during the study period.
Table 2.
Model estimated ethnic-specific mortality, mortality trends* 2000–2011, and ethnic comparisons in mortality.
| Timing of mortality | Year | Mortality | MA vs NHW RR (95%CI) |
|
|---|---|---|---|---|
| MA | NHW | |||
| 30 days | 2000 | 5.1% | 7.6% | 0.67 (0.48, 0.92)† |
| 2011 | 5.2% | 5.6% | 0.92 (0.65, 1.29) | |
| % change 2000 to 2011 | 2.7% (−40.2%, 76.2%) | −27.7% (−57.9%, 24.3%) | ||
| 1 year | 2000 | 17.4% | 20.8% | 0.84 (0.70, 1.01)‡ |
| 2011 | 15.3% | 15.5% | 0.99 (0.81, 1.21) | |
| % change 2000 to 2011 | −13.3% (−32.5%, 11.4%) | −27.5% (−44.1%, −5.9%) | ||
P for time trend by MA interaction: 30 day, p=0.22; 1 year, p=0.30
p=0.014;
p=0.06
Figure 1.
2000–2011 adjusted trend lines for 30-day and 1 year mortality by ethnicity
Sensitivity analysis using splines to model age and NIHSS continuously did not change the results suggesting that residual confounding by age was not responsible for the ethnic differences over time. Using the models to project future trends of ethnic differences in stroke mortality, the 1 year stroke mortality advantage seen for MAs versus NHWs would be reversed by 2023, and the advantage seen for MAs versus NHWs in 30 day case-fatality would be reversed by 2028.
DISCUSSION
The post-stroke survival advantage for MAs compared with NHWs diminished over the past decade. This is an important finding considering the rapid growth and aging of the MA population. A recent American Heart Association/American Stroke Association Scientific Statement attributed the widespread decline in stroke mortality to risk factor control10. It also stated that stroke mortality was declining in all race/ethnic groups. Stroke mortality may be declining in MAs due to declines in stroke incidence6, but post-stroke case fatality and one-year post-stroke mortality are not significantly declining as illustrated by the current work. In addition to higher incidence6 MAs have more stroke recurrence11 compared with NHWs. The new data presented in this paper coupled with a recent report of worse neurologic, functional and cognitive outcomes in MA stroke survivors compared with NHWs12 suggests that the relative stroke burden in MAs continues to be high. The projections provided by the current work suggest that MA will soon have higher stroke case-fatality and one-year stroke mortality rates compared with NHWs. It appears that the “Hispanic Paradox” is no longer relevant for MA stroke since the previously identified post-stroke survival advantage is no longer apparent.
There are limitations to this work. The overall unadjusted case fatality and 1 year mortality rates are somewhat lower compared with other recently reported Western population-based studies13, 14. While this may reflect geographical variation, or good medical care in this community and better tools to improve stroke outcome, it may also reflect missed mortality assessment despite the rigorous methods employed. It could also reflect better ascertainment of cases less likely to die than other studies. Comparing population-based studies with different methods in different communities is always perilous. Further, using sensitivity analysis we examined whether changes in the ethnic-specific age distributions over time explained the results but found no such effect. Our projections for the reversal of the mortality advantage must be taken with extreme caution since they are based on the current trend lines and do not consider the many possible influences on health care over the next two decades15. However, these influences would need to have a differential impact on MAs and NHWs to alter these projections.
Since stroke incidence and outcome are worse in MAs compared with NHWs, and 1 year mortality is not significantly declining in MAs but is declining in NHWs, efforts to remedy the increased stroke burden in MAs must involve primary and secondary prevention as well as acute treatment and recovery efforts. While this appears to be a daunting task, it is important to note incidence has declined in MAs over the past decade6. This indicates that positive change is possible.
Supplementary Material
Acknowledgments
SOURCE OF FUNDING
National Institutes of Health R01NS38916 and K23 AG038731
Footnotes
DISCLOSURES
None
References
- 1.2010 census shows nation’s Hispanic population grew four times faster than the total US Population. United States Census Bureau; 2011. [Accessed June 17, 2014]. http://www.census.gov/newsroom/releases/archives/2010_census/cb11-cn146.html. [Google Scholar]
- 2.Ennis S, Ríos-Vargas M, Albert NG. The Hispanic population: 2010. 2010 Census Briefs. United States Census Bureau; [Accessed June 17, 2014]. http://www.census.gov/prod/cen2010/briefs/c2010br-04.pdf. [Google Scholar]
- 3.Vincent GK, Velkoff VA. The Next Four Decades. The Older Population in the United States: 2010 to 2050. United States Census Bureau; [Accessed June 17, 2014]. http://www.census.gov/prod/2010pubs/p25-1138.pdf. [Google Scholar]
- 4.Lisabeth LD, Risser JM, Brown DL, Al-Senani F, Uchino K, Smith MA, et al. Stroke burden in Mexican Americans: The impact of mortality following stroke. Ann Epidemiol. 2006;16:33–40. doi: 10.1016/j.annepidem.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 5.Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethn Dis. 2001;11:496–518. [PubMed] [Google Scholar]
- 6.Morgenstern LB, Smith MA, Sanchez BN, Brown DL, Zahuranec DB, Garcia N, et al. Persistent ischemic stroke disparities despite declining incidence in Mexican Americans. Ann Neurol. 2013;74:778–785. doi: 10.1002/ana.23972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. [Accessed March 7, 2014];State and County Quick Facts: Nueces County, Texas. United States’ Census Bureau web site. Http://quickfacts.Census.Gov/qfd/states/48/48355.html.
- 8.Caveney AF, Smith MA, Morgenstern LB, Lisabeth LD. Use of death certificates to study ethnic-specific mortality. Public Health Rep. 2006;121:275–281. doi: 10.1177/003335490612100309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 10.Lackland DT, Roccella EJ, Deutsch AF, Fornage M, George MG, Howard G, et al. Factors influencing the decline in stroke mortality: A statement from the American Heart Association/American Stroke Association. Stroke. 2014;45:315–353. doi: 10.1161/01.str.0000437068.30550.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lisabeth LD, Smith MA, Brown DL, Moye LA, Risser JM, Morgenstern LB. Ethnic differences in stroke recurrence. Ann Neurol. 2006;60:469–475. doi: 10.1002/ana.20943. [DOI] [PubMed] [Google Scholar]
- 12.Lisabeth LD, Sánchez BN, Baek J, Skolarus LE, Smith MA, Garcia N, et al. Neurologic, functional and cognitive stroke outcomes in Mexican Americans. Stroke. 2014;45:1096–1010. doi: 10.1161/STROKEAHA.113.003912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmidt M, Jacobsen JB, Johnsen SP, Botker HE, Sorensen HT. Eighteen-year trends in stroke mortality and the prognostic influence of comorbidity. Neurology. 2014;82:340–350. doi: 10.1212/WNL.0000000000000062. [DOI] [PubMed] [Google Scholar]
- 14.Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of stroke during 1990–2010: Findings from the global burden of disease study 2010. Lancet. 2014;383:245–254. doi: 10.1016/s0140-6736(13)61953-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Howard G, Goff DC. Population shifts and the future of stroke: Forecasts of the future burden of stroke. Annals of the New York Academy of Sciences. 2012;1268:14–20. doi: 10.1111/j.1749-6632.2012.06665.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.