Abstract
Background
Physical activity is recommended to mitigate functional limitations associated with knee osteoarthritis (OA). However, it is unclear whether walking on its own protects against the development of functional limitation.
Methods
Walking over 7 days was objectively measured as steps/day within a cohort of people with or at risk of knee OA from the Multicenter Osteoarthritis Study. Incident functional limitation over two years was defined by performance-based (gait speed ≤ 1.0 m/s) and self-report (WOMAC physical function ≥ 28/68) measures. We evaluated the association of steps/day at baseline with developing functional limitation two years later by calculating risk ratios adjusted for potential confounders. The number of steps/day that best distinguished risk for developing functional limitation was estimated from the maximum distance from chance on Receiver Operator Characteristic curves.
Results
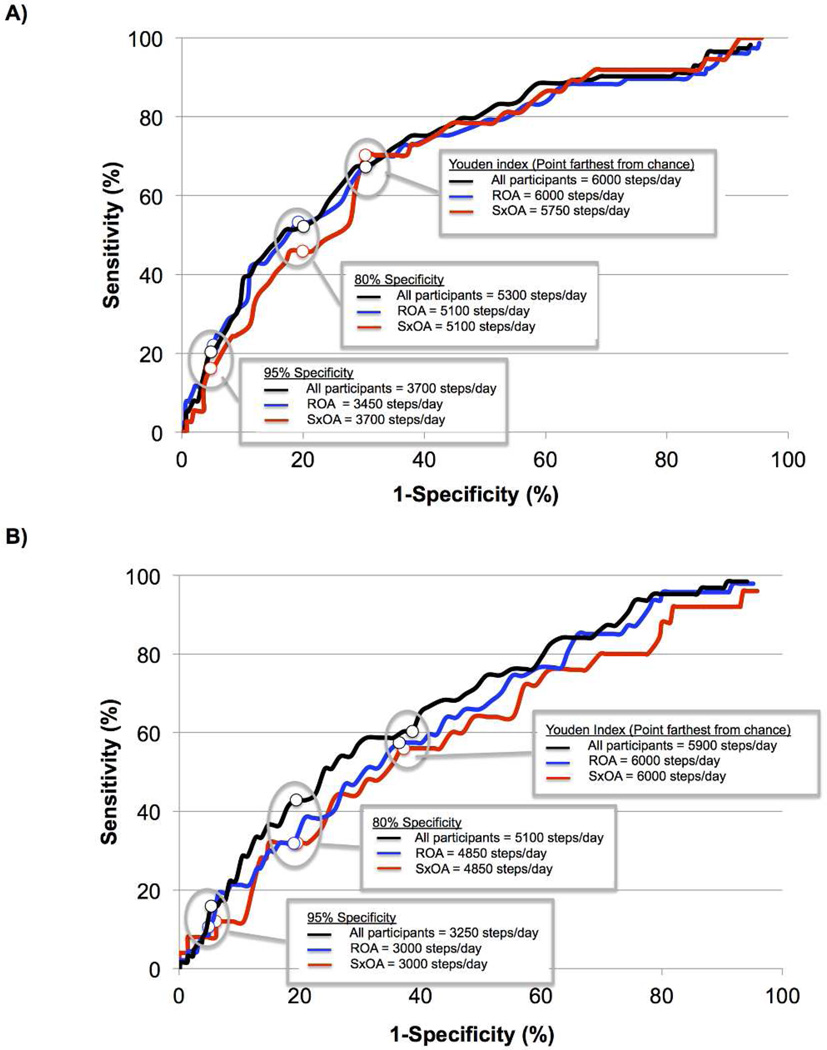
Among 1788 participants (mean age 67, mean BMI 31 kg/m2, female 60%), each additional 1000 steps/day was associated with a 16% and 18% reduction in incident functional limitation by performance-based and self-report measures, respectively. Walking < 6000 and < 5900 steps/day were the best thresholds to distinguish incident functional limitation by performance-based (67.3%/71.8% [sensitivity/specificity]) and self-report (58.7%/68.9%) measures, respectively.
Conclusions
More walking was associated with less risk of functional limitation over two years. Walking ≥ 6000 steps/day provides a preliminary estimate of the level of walking activity to protect against developing functional limitation in people with or at risk of knee OA.
Keywords: Physical Activity, Arthritis, Physical Function
INTRODUCTION
Knee osteoarthritis (OA) is the leading cause of functional limitation, such as difficulty walking and climbing stairs, among older adults. (1, 2) As such, there is a critical need to improve intervention strategies to address decline in physical functioning in knee OA. The 2014 OA Research Society International (OARSI) guidelines recommend non-pharmacological modalities, e.g., exercise, for knee OA. (3) Unfortunately, less than one-third of primary-care physicians recommend exercise to their patients with OA. (4) Further, for those who do exercise, most abandon training following the conclusion of their structured program effectively negating any exercise-related health gains. (5)
Adopting a physically active lifestyle in addition to exercising may offer additional therapeutic opportunities to people with knee OA. Exercise is a subset of physical activity (PA) and both refer to energy expenditure above a basal level. (6) However, exercise is planned, structured, and recurring, such as weight-lifting or aerobic exercise, typically performed at a particular intensity for a set duration of time, whereas PA incudes unstructured activities, such as energy expenditure from with getting to work, preparing meals, and raking leaves. (6) While there is support that strength training and aerobic exercise improve physical function in knee OA, (3, 7) it is not known whether there are added benefits from unstructured PA.
Walking is one of the most common types of unstructured PA older adults with knee OA employ on a daily basis, (8) but two-thirds of US adults with arthritis report walking less than 90 minutes/week, (9) and whether walking has an effect on function is not known. If unstructured PA through walking, regardless of continuous duration or intensity, reduces the risk of functional limitation in knee OA, it would be necessary to additionally study how much daily walking is needed to achieve this risk reduction. Such an understanding would enable development of recommendations regarding daily walking and its benefits. Specifically, whether there are any minimum values of walking activity to initially recommend or to target as an ultimate goal for walking on an ongoing basis to best protect against the development of functional limitation is presently not known. This is an important gap given that the ability to measure daily walking and progress towards step goals has greatly improved in recent years. Currently, accelerometer-enable devices worn on the wrist or waist are widely available, as are smart phone apps that record daily walking. To optimally take advantage of such off-the-shelf technology to promote walking activity as a therapeutic strategy, general guidance regarding daily step goals for people with knee OA is needed.
Therefore, the purpose of this study was to examine the association of step-defined daily walking with incident functional limitation two years later in people with or at risk of knee OA. We investigated preliminary estimates of a starting level and an ideal amount of ongoing daily walking to protect against the development of functional limitation.
METHODS
Study Sample: The Multicenter Osteoarthritis (MOST) Study
A detailed description of the MOST Study has been published in detail elsewhere. (10) In brief, MOST is a large multi-center longitudinal cohort study of community-dwelling participants who have or are at high risk of knee OA. (10) The MOST study cohort at baseline included adults aged 50 – 79 years who were recruited from communities in and surrounding Birmingham, Alabama and Iowa City, Iowa starting in 2003. Study criteria, focused on risk for knee OA, included the presence of known risk factors, such as being ≥ 50 years of age, female, reporting a previous knee injury or operation, and having a body weight in excess of the median weight for each age- and sex-specific group based on data from the Framingham OA Study. (11) The MOST Study protocol was approved by the institutional review boards at the University of Iowa in Iowa City, University of California in San Francisco, University of Alabama in Birmingham, and Boston University Medical Center. All participants in the MOST Study provided informed consent.
This particular study focused on a subset of the MOST cohort. We included data from the 60-month follow-up exam conducted between May of 2009 and January of 2011 and the 84-month follow-up exam conducted between September of 2011 and January of 2013. The 60-month visit was the first study visit in which objectively measured PA was collected. For purposes of the present analysis of these data, the 60-month visit was considered ‘baseline’ and the 84-month visit was the ‘two-year follow-up’.
Incident functional limitation
Our primary outcome was incident functional limitation at the two-year follow-up. We defined functional limitation using both performance-based and self-report measures since both provide distinct information about the underlying construct of physical function. (12)
The performance-based measure of functional limitation was defined as walking with a gait speed < 1.0 m/s since walking slower than this threshold is a risk factor for persistent limitations in physical functioning, hospitalization, and mortality in older adults. (13, 14) Gait speed was determined from the average of two trials of walking along a marked 20-meter course in an unobstructed corridor. Timing started when the first foot crossed the start line and ended after the last foot crossed the finish line. Participants were allowed to use walking aids during the test if needed, such as a cane.
The self-reported measure of functional limitation was defined as scores of ≥ 28 out of 68 on the Western Ontario and McMasters University Osteoarthritis Index (WOMAC) physical function subscale (0–68; higher scores are worse). (15) This is consistent with a previous definition of poor functional outcome for persons with knee OA (16), and within a range of scores reported for persons awaiting total knee replacement (17). Persons with a score of 28/68 report having at least slight to moderate difficulty in all 17 tasks from the WOMAC physical function scale, or severe to extreme difficulty in 7 to 9 tasks.
Both gait speed and WOMAC physical function have high test-retest reliability in people with knee OA (Gait speed ICC= 0.94 and WOMAC ICC=0.68) (15, 18) and older adults (Gait speed ICC=0.90). (19)
Daily walking
Daily walking was assessed at baseline as steps/day using a StepWatch Activity Monitor (Orthocare Innovations, Mountlake Terrace, WA). This is a small (70 × 50 × 20 mm; 38 g), waterproof, self-contained accelerometer-based device that attaches to the ankle and records the number of strides taken every minute without providing any feedback to the user. To calculate the number of steps, the stride output is doubled. The StepWatch has high concurrent validity in comparison with a visual count of step frequency in older adults (20) and high convergent validity in comparison with SF-36 scores among participants with OA. (21)
Each study participant was fitted with the StepWatch and given written and verbal instructions for attaching the monitor each morning and removing it at bedtime for up to 7 consecutive days. To determine whether participants wore the monitor long enough to be considered a valid day, we adopted a published method for processing accelerometer data (22) and defined 10 hours of monitoring as the minimum amount of wearing time. The 10-hour requirement represents more than 66% of waking hours and has been utilized as a threshold in studies of PA in the general adult population (23) and people with knee OA. (22) Time worn was determined from the first step recorded in the morning to the last step recorded in the evening. To exclude times that participants may have taken the StepWatch off during the day, we omitted minutes when the monitor registered no steps for 180 consecutive minutes during the day. (24) Finally, we restricted our sample to those participants who wore the instrument for at least 3 valid days, considered a minimum standard to establish a reliable estimate of PA. (25)
We calculated average steps/day by totaling the number of steps taken each valid day of monitoring divided by the number of valid days. Waist-mounted pedometers are known to count fewer steps when compared with an ankle-mounted StepWatch activity monitor. (26) Since pedometers are inexpensive, readily accessible, and likely to be used in clinical and public health applications, we converted steps/day from Stepwatch data to what would be expected from a waist-mounted piezoelectric pedometer using previously reported methods. (27) Specifically, we reduced the number of steps/day from Stepwatch data by 25%.
Radiographic knee OA
Radiographic knee OA (ROA) at baseline was defined from weight-bearing posteroanterior and lateral fixed flexion radiographic evaluations of both knees. (28) Three expert readers (two rheumatologists and a musculoskeletal radiologist) blinded to clinical data graded joint space narrowing (JSN) and osteophytes using the OARSI atlas (29) in both tibiofemoral (TF) and patellofemoral (PF) joints (both graded 0–3). The presence of JSN and osteophytes in the TF joint was also graded according to Kellgren and Lawrence (K/L) criteria (0–4). Any disagreements between readers were adjudicated by 3 readers to reach consensus. We defined ROA based on radiographic findings in either TF or PF joints. Participants were classified as having ROA with the presence of ROA in one or both knees. For the TF joint this was a KL grade ≥ 2, and for the PF joint an osteophyte score ≥ 2, or any joint space narrowing score ≥ 2 with any osteophyte, sclerosis, or cyst score of ≥ 1 on a lateral plain view film. (30, 31) The inter-rater reliability weighted kappa for the KL grade at baseline was 0.80.
Symptomatic knee OA
Symptomatic knee OA was defined by the presence of ROA and consistent frequent knee pain in the same knee. Frequent knee pain was assessed at two time points by the following the knee-specific question “During the past 30 days, have you had pain, aching, or stiffness on most days?” Participants were asked this question at a telephone screen approximately 30-days before the 60-month clinic visit, and again during the clinic visit. Positive responses to this question at both time points indicated the presence of consistent frequent knee pain. We classified participants as having symptomatic knee OA based on the status of his/her worst knee. For example, a person with symptomatic knee OA in one knee and frequent pain only in the contralateral knee was classified as having symptomatic knee OA, whereas a person with radiographic OA only in one knee and frequent knee pain only in the contralateral knee was classified as not having symptomatic knee OA.
Potential Confounders
The following factors were considered as potential confounders (based on their association with function and PA in previous studies (16, 32, 33)) and ascertained by interview, questionnaire, and/or direct measurement as appropriate, at baseline: age, sex, race (Non-White vs. White), education (<some college vs. ≥college), body mass index (BMI) computed from standardized weight and height assessments classified into World Health Organization categories (34), ROA, knee pain (0–100) from a Visual Analogue Scale (VAS) of the average knee pain in the past 30 days, self-reported comorbidities based on the modified Charlson comorbidity index (35) (≥1 vs. none), depressive symptoms measured with the Center for Epidemiologic Studies Depression Scale (CES-D)(36) (≥ 16 vs. < 16), and widespread pain (present vs. absent), as pain above and below the waist, pain on the right and left sides of the body, and axial pain based upon a standard homunculus. (37)
Statistical Analysis
We computed means and standard deviations for continuous variables and proportions for categorical variables to describe the study sample. To examine the association of steps/day with the incidence of functional limitation at the two-year follow-up, we used regression methods with a log-link function and robust standard errors to obtain risk ratios adjusted for potential confounders including ROA and knee pain. (38) We included study participants without functional limitation at baseline. For the performance-based measure of functional limitation we included study participants with a gait speed > 1.0 m/s at baseline, and for the self-reported measure of functional limitation we included those with WOMAC physical function < 28 (out of 68) at baseline. We did not adjust for baseline levels of gait speed or WOMAC function since the bias introduced by such an adjustment may exceed the bias eliminated. (39) Converted steps/day were used for all analyses.
Analyses were conducted separately for steps/day as a continuous measure with incident function limitation, and as steps/day as a categorical measure based on Tudor-Locke and Bassett’s 2004 pedometer-determined PA cut-points for healthy adults: < 5000 (sedentary), 5000 to 7499 (low active), and ≥ 7500 steps/day (somewhat to highly active). (40) We did not include the ≥ 10,000 steps/day category as only 14% of our study participants had this level of PA.
Next, we used separate logistic regression models to identify steps/day values protective against the development of functional limitation. To identify a recommended amount of ongoing daily walking, we used the Youden index to calculate the number of steps/day that best distinguishes between subjects with and without incident functional limitation. (41) This is the point on a Receiver Operating Characteristic (ROC) curve that is the maximum distance from the chance line, or positive diagonal, i.e., is the farthest from chance. (41) Sensitivity was calculated as the proportion of study participants whose steps/day count was less than an identified threshold and who had incident functional limitation divided by all who had incident functional limitation. Specificity refers to the proportion of study participants whose steps/day was greater than an identified threshold and who did not develop functional limitation divided by all who did not have incident functional limitation.
Next, to identify a minimum steps/day value that may be a reasonable first goal of PA, we identified steps/day values on the ROC curve that corresponded to 80% and 95% specificity, i.e., the proportion of people who walk above a given threshold of steps/day and did not develop functional limitation. We calculated the area under the curve (AUC) in separate models to assess the overall ability of steps/day to discriminate those with and without incident functional limitation defined by performance and self-report measures, respectively. (42) To specifically examine the effects of daily walking on incident functional limitation among people with knee OA, we repeated all analyses by restricting our sample to those with ROA (i.e., regardless of symptoms) followed by further restricting to those with symptomatic knee OA to assess whether the effects differed by OA status.
RESULTS
The 2,330 MOST study participants attending the 60-month follow-up visit have been described previously. (43) In brief, 16% (377) did not agree to wear the StepWatch monitor, and 2% (58) had monitor malfunctions. Of the remaining 1,895 participants, 94% (1,788) wore the monitor for necessary duration and therefore comprise the present study’s sample. The average (sd) age of the study sample was 67.2 (7.7) years and the average BMI was 30.7 (6.0) kg/m2. A majority of the participants were women (60%) and white (90%). Table 1.
Table 1.
Characteristics of study participants
| All Study Participants (N = 1788) |
ROA* (n=1003) |
Symptomatic OA† (n=390) |
|
|---|---|---|---|
| Age [Mean (sd)] | 67.2 (7.7) | 67.8 (7.8) | 66.9 (7.9) |
| Women [%] | 59.8 | 59.3 | 63.6 |
| BMI [kg/m] [Mean (sd)] | 30.7 (6.0) | 31.4 (6.2) | 32.1 (6.7) |
| Education [% ≥ college] | 46.9 | 44.4 | 41.5 |
| Race [% white] | 90.3 | 88.4 | 87.2 |
| Knee pain (VAS: 0–100) [Mean (sd)] | 18.8 (20.9) | 22.8 (22.2) | 36.9 (23.0) |
| Comorbidity [%] | 40.8 | 43.0 | 45.9 |
| Study Site [% Alabama] | 38.0 | 38.1 | 39.0 |
| Depressive Symptoms [% CES-D ≥16] | 9.0 | 9.7 | 13.1 |
| Gait speed at baseline [meters/second] [Mean (sd)] | 1.22 (0.21) | 1.19 (0.21) | 1.16 (0.21) |
| WOMAC Physical Function at baseline [Mean (sd)] | 11.8 (11.1) | 14.2 (11.4) | 21.9 (11.0) |
| Steps/day [Mean (sd)] | 7073 (2912) | 6823 (2868) | 6476 (2613) |
Abbreviations: MOST=Multicenter Osteoarthritis Study; BMI = Body Mass Index; VAS=Visual Analogue Scale; OA= Osteoarthritis; CES-D= Center for Epidemiologic Studies Depression Scale; WOMAC = Western Ontario and McMasters Universities Osteoarthritis Index
Of those with ROA, 6% had patellofemoral OA, 61% had tibiofemoral OA, and the remainder had both patellofemoral and tibiofemoral OA.
Of those with symptomatic OA, 5% had patellofemoral OA, 54% had tibiofemoral OA, and the remainder had both patellofemoral and tibiofemoral OA.
Of those without functional limitation at baseline, 8% (113/1381) and 4% (63/1422) developed functional limitation defined by performance and self-report, respectively, at the two-year follow-up. Higher steps/day were associated with lower risk of incident functional limitation. Table 2 Specifically, those who walked 5000 – 7499 steps/day had 0.50 and 0.51 times the adjusted risk by the performance-based and self-report measures, respectively, compared with those walking < 5000 steps/day. Those who walked ≥ 7500 steps/day, had 0.31 and 0.41 times the risk by performance-based and self-report measures, respectively, compared with those walking < 5000 steps/day. Each additional 1000 steps/day was associated with a 16% and 18% reduction in incident functional limitation by the performance-based and self-report measures, respectively.
Table 2.
Risk Ratio (RR) of incident functional limitation at the two-year follow-up as measured by gait speed during the 20-meter walk and WOMAC physical function among all study participants (n=1788).
| Steps/day | Baseline [Mean (sd)] |
Incident functional limitation‡/Total |
% | Adj RR§ [95% CI] |
|---|---|---|---|---|
| Gait Speed (m/s) | ||||
| < 5000 | 1.19 (0.13) | 55/257 | 21.4 | 1.00 [Reference] |
| 5000 – 7499 | 1.26 (0.16) | 39/495 | 7.9 | 0.50 [0.33, 0.76] |
| ≥ 7500 | 1.32 (0.17) | 19/631 | 3.0 | 0.31 [0.18, 0.56] |
| Increase by 1000 steps/day | 0.84 [0.76, 0.93] | |||
| WOMAC Physical Function (0–68) | ||||
| < 5000 | 10.9 (8.6) | 27/293 | 9.2 | 1.0 [Reference] |
| 5000 – 7499 | 9.1 (7.9) | 20/500 | 4.0 | 0.51 [0.29, 0.92] |
| ≥ 7500 | 7.9 (7.6) | 16/629 | 2.5 | 0.41 [0.20, 0.86] |
| Increase by 1000 steps/day | 0.82 [0.72, 0.94] |
Incident functional limitation defined as gait speed < 1.0 m/s or WOMAC Physical Function > 28
Adjusted for age, sex, race, education, Body Mass Index, comorbidity, depressive symptoms, widespread pain, knee pain severity, radiographic knee OA, and study site
The PA cut-point with the best balance of sensitivity and specificity for functional limitation defined by performance was 6000 steps/day; for self-report it was 5900 steps/day. Figure 1 The sensitivity / specificity was 67.3% / 71.8% for performance, and 58.7% / 68.9% for self-report. The PA cut-point for 80% specificity for functional limitation defined by performance was 5300 steps/day. Among study participants who did not develop slow walking at the two-year follow-up (< 1.0 m/s), 80% walked at least 5300 steps/day. The PA cut-point for 80% specificity for functional limitation defined by self-report was 5100 steps/day. For 95% specificity, the PA cut-point was 3700 for performance and 3250 for self-report defined functional limitation. The AUC for steps/day associated with functional limitation by performance and self-report was fair with values of 0.73 and 0.67, respectively.
Figure 1. Receiver operating characteristic curves of steps/day with incident functional limitation by A) performance (slow gait speed) and B) self report (WOMAC physical function).
The Youden index represents the best combination of sensitivity and specificity by being the point farthest away from chance. The area under the curve was 0.73 and 0.67 for performance and self-report, respectively.
ROA and Symptomatic knee OA
To determine whether the effects of daily walking on the incident functional limitation may differ based upon the presence of ROA or symptomatic knee OA, we restricted our sample to study participants with ROA (n=1003) followed by those with symptomatic knee OA (n=390) to perform additional analyses. Subject characteristics of these samples are described in Table 1. In general, those with ROA and those with symptomatic knee OA had a higher BMI, less education, more knee pain, more comorbidity and depressive symptoms, poorer physical function and fewer steps/day as compared with the entire study sample of those with or at risk of knee OA. Functional limitation by performance-based and self-report measures developed in a higher proportion of those with ROA (10% and 6%, respectively) and symptomatic knee OA (13% and 10%, respectively) compared with the entire study sample (8% and 4%, respectively).
In general, the protective effects of more steps/day were similar for those with ROA and symptomatic knee OA as for the entire study sample, although the precision was somewhat limited with functional limitation as measured by self-report for those with ROA and symptomatic knee OA. Table 3. We also found similar PA cut-points and AUC values for those with ROA and symptomatic knee OA as the entire study sample by both outcome measures (performance-based and self-reported). Figure 1
Table 3.
Risk ratios (RR) of incident functional limitation among study participants with A) ROA (n=1003) and B) Symptomatic ROA (n=390).
| A | |||
|---|---|---|---|
| Steps/day | Incident functional limitation**/Total |
% | Adj RR†† [95% CI] |
| Functional Limitation measured by Performance (Slow Gait Speed) | |||
| < 5000 | 39/163 | 23.9 | 1.00 [Reference] |
| 5000 – 7499 | 25/291 | 8.6 | 0.52 [0.32, 0.84] |
| ≥ 7500 | 13/315 | 4.1 | 0.34 [0.18, 0.65] |
| Increase by 1000 steps/day | 0.84 [0.75, 0.95] | ||
| Functional Limitation measured by Self-Report (WOMAC Physical Function) | |||
| < 5000 | 18/179 | 10.0 | 1.00 [Reference] |
| 5000 – 7499 | 17/282 | 6.0 | 0.70 [0.37, 1.34] |
| ≥ 7500 | 12/307 | 3.9 | 0.54 [0.22, 1.31] |
| Increase by 1000 steps/day | 0.87 [0.75, 1.00] | ||
| B | |||
|---|---|---|---|
| Steps/day | Incident functional limitation1/Total |
% | Adj RR2 [95% CI] |
| Functional Limitation measured by Performance (Slow Gait Speed) | |||
| < 5000 | 17/62 | 27.4 | 1.00 [Reference] |
| 5000 – 7499 | 15/119 | 12.6 | 0.57 [0.30, 1.09] |
| ≥ 7500 | 5/107 | 4.7 | 0.26 [0.10, 0.70] |
| Increase by 1000 steps/day | 0.80 [0.67, 0.95] | ||
| Functional Limitation measured by Self-Report (WOMAC Physical Function) | |||
| < 5000 | 8/52 | 15.4 | 1.00 [Reference] |
| 5000 – 7499 | 10/97 | 10.3 | 0.95 [0.35, 2.59] |
| ≥ 7500 | 7/91 | 7.7 | 0.80 [0.24, 2.71] |
| Increase by 1000 steps/day | 0.97 [0.80, 1.18] | ||
Incident functional limitation defined as gait speed < 1.0 m/s or WOMAC Physical Function > 28
Adjusted for age, sex, race, education, Body Mass Index, comorbidity, depressive symptoms, widespread pain, knee pain severity, radiographic knee OA, and study site
DISCUSSION
In this large prospective cohort study of people with or at risk of knee OA, those who walked more on a daily basis were less likely to develop functional limitation two years later. Based on our data, we discerned preliminary values of PA associated with maintaining physical functioning that may be considered as preliminary clinical recommendations for therapeutic PA targets for people with or at risk of knee OA. Specifically, walking ≥ 3000 steps/day may be an initial minimum daily walking goal to recommend as few people meeting this benchmark developed functional limitation two years later. Increasing this amount to walking ≥ 6000 steps/day may be an ideal amount on an ongoing basis as this threshold best discriminated those who developed functional limitation from those who did not. Further, we found that each additional 1000 steps/day study participants walked at baseline was associated with 16% to 18% less risk of developing functional limitation two years later. Lastly, the effects of walking on incidence of functional limitations were similar regardless of presence of ROA or symptomatic knee OA, suggesting that all older adults with or at risk of knee OA can be similarly counseled regarding targets for their daily walking activity. In addition, the magnitudes of effect were similar between performance-based and self-reported ascertainment of function, indicating that both metrics were assessing similar constructs.
The threshold of ≥ 3000 steps/day as a minimum initial goal is consistent with previous studies. Walking < 2500 steps/day fits within a ‘sedentary’ or ‘basal’ pedometer-determined PA category for healthy adults between 18 and 65 years of age. (45) Further, Fisher et al. reported walking < 2000 steps/day to be a strong predictor of 30-day readmission for older adults hospitalized with an acute medical illness. (46) Our findings extend these previous studies by providing empirical evidence that few people with or at risk of knee OA who walked ≥ 3000 steps/day developed poor functioning two years later. Moreover, walking ≥ 6000 steps/day as an ideal level of daily walking to ultimately adopt is also consistent with previous studies. Healthy older adults typically walk 6000 – 8500 steps/day, which is in contrast to people with a broad range of disabilities and chronic diseases, who walk 3500 – 5000 steps/day. (47) Additionally, walking ≥ 6000 steps/day fits within the ‘low active’ pedometer-determined PA category for healthy adults between 18 and 65 years of age, (40, 45) and is associated with a lower prevalence of adverse cardiometabolic health indicators. (48) Thus, the thresholds for functional limitation noted in our study are consistent with the findings for other clinical outcomes. Additionally, the benchmark of ≥ 6000 steps/day is a more attainable goal for people with knee OA compared to the popular recommendation to walk 10,000 steps/day. (40, 49) Walking 10,000 steps/day may be unrealistic for many people with knee OA; <14% of our study sample met this threshold. Rather than promoting potentially difficult-to-achieve walking activity goals that could further discourage people with knee OA, our study results suggest that lower targets may still provide therapeutic benefits.
In contrast to prior intervention studies assessing the effect of structured aerobic walking on function, (7) our current study largely provides data on unstructured daily walking, i.e., non-exercise steps that are not necessarily performed for a particular continuous duration, or at a particular intensity. We have previously reported that around two-thirds of MOST study participants did not have any sustained bouts of walking at moderate intensity for ≥ 10 minutes, (50) which would be expected if they were walking for exercise. Hence, our current study adds to the existing exercise literature by demonstrating that non-exercise-related PA through walking is associated with less risk of functional limitation two years later in knee OA.
Our findings of a dose-response relationship between PA and functional limitation is consistent with the 2008 Physical Activity Guidelines for American’s message that “some is good; more is better”. (44) This relationship has been shown in people with other musculoskeletal conditions, such as low back pain. (51) However, the dose-response relationship has not been widely studied in arthritis, except for one study with people with radiographic knee OA. (52)
There are limitations to our study that should be acknowledged. First, our thresholds should ideally be tested in clinical trials to truly determine effectiveness in reducing the risk of functional limitation. However, the incidence of functional limitation was low in our sample, between 4–13%, and studies of older men and women ≥ 70 years of age have reported incidence rates of 7.1/100 person-years and 10.6/100 person-years, respectively. (53) Thus, the necessary sample size and follow-up duration for a clinical trial may make it impractical to properly test the effectiveness of these thresholds. Nonetheless, until such trials are done (or in lieu of such trial data in the interim), these data at least provide guidance regarding reasonable thresholds that are likely to have benefits on physical function. Second, our findings should be interpreted carefully since different monitors and methods of estimating pedometer steps have been previously employed across studies. We believe our pedometer-step counts were a reasonable estimate since our average steps/day values were similar to previously published pedometer-determined steps/day in comparable samples. (54) Third, we did not examine the association of moderate intensity steps with our study outcomes, but instead focused on total steps/day as a simple indicator of PA. Given the well-known health benefits of moderate intensity PA with health outcomes, (44) it is possible that more time walking at a higher intensity is associated with less functional limitation. However, an approach focusing on total step counts is more clinically and practically relevant, particularly to engage older adults in increasing their walking activity for health benefits. Fourth, physical function can fluctuate over time dependent on underlying impairment, such as knee pain. A limitation is that our outcome of incident functional limitation does not discriminate between those who truly have a first instance of functional limitation at two years from those who have fluctuating physical function over time. This is an inherent challenge in any observational cohort study with fixed time-point visits; we have followed the standard approach used to assess this type of outcome. Fifth, it is possible that participants engaged in physical activity with no steps, such as cycling or swimming, or minimal steps, such as gardening. However, MOST study participants were unlikely to participate in these non-stepping activities with any regularity based upon data collected about other physical activities. Study participants completed the Physical Activities Scale of the Elderly at the MOST baseline visit five years earlier and only 9% of men and 7% of women reported engaging in strenuous non-ambulatory activities ‘often’. Given that time spent participating in physical activities decreases with age, (55) the prevalence of non-ambulatory activities is likely to continue to be low at the 60-month visit.
Our study also has several strengths. First, we used a longitudinal study design to investigate the association of steps/day with the development of functional limitation two years later, which is an advance over previous cross-sectional studies. (56, 57) Second, our study provides preliminary pedometer-equivalent step thresholds associated with the development of functional limitation in people with or at risk of knee OA; a paucity of studies currently exist for what number of steps/day to recommend for this patient population.
CONCLUSIONS
In summary, we found a greater number of steps/day was increasingly protective against the development of functional limitation, both measured by self-report and performance, in people with or at high risk of knee OA. A starting goal may be to walk > 3000 steps/day, as few study participants meeting this level of PA developed functional limitation. Ultimately, walking ≥ 6000 steps/day may be the ideal goal, as this threshold best discriminating ability to identify those who developed functional limitation. Clinicians and policy makers can consider these goals as preliminary levels of physical activity to recommend to people with or at high risk of knee OA. These steps/day thresholds merit further evaluation as improving daily walking may be an inexpensive means of minimizing functional limitations in knee OA.
SIGNIFICANCE AND INNOVATION.
While physical activity through structured exercise may improve function, it is not known whether daily walking is associated with lower risk of developing functional limitation among people with or at risk of knee osteoarthritis (OA).
Walking 1000 more steps/day was associated with 16% to 18% less risk of developing functional limitation two years later.
A starting goal for physical activity may be to walk ≥ 3000 steps/day and progress to ultimately walking ≥ 6000 steps/day on an ongoing basis to reduce the risk of developing functional limitation. These thresholds require testing in clinical trials.
ACKNOWLEDGEMENTS
The authors acknowledge MOST study participants for their time and effort to provide data for this study. The authors also thank the physical therapists at the University of Delaware Physical Therapy Clinics for conversation related to pedometer use in their patients, which led to conceptualization of this manuscript.
FUNDING
NIH AG18820, AG 18832, AG 18947, AG 19069, AR007598, NIH AR47785, NIAMS R01AR062506, ACR/RRF Rheumatology Investigator Award, the Boston Rehabilitation Outcomes Center (Boston ROC) R24HD0065688, the Boston Claude D. Pepper Older Americans Independence Center 1P30AG031679 and the Foundation for Physical Therapy Geriatric Research Grant. This material is based upon work supported by the U.S. Department of Agriculture, under agreement No. 58-1950-0-014. Any opinions, findings, conclusion, or recommendations expressed in this publication are those of the authors and do not necessarily reflect the view of the U.S. Department of Agriculture.
REFERENCES
- 1.Guccione AA, Felson DT, Anderson JJ, Anthony JM, Zhang Y, Wilson PW, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. American journal of public health. 1994;84(3):351–358. doi: 10.2105/ajph.84.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray CJ, Richards MA, Newton JN, Fenton KA, Anderson HR, Atkinson C, et al. UK health performance: findings of the Global Burden of Disease Study 2010. Lancet. 2013;381(9871):997–1020. doi: 10.1016/S0140-6736(13)60355-4. [DOI] [PubMed] [Google Scholar]
- 3.McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma-Zeinstra SM, et al. OARSI Guidelines for the Non-Surgical Management of Knee Osteoarthritis. Osteoarthritis and Cartilage. 2014;(0) doi: 10.1016/j.joca.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 4.Maserejian NN, Fischer MA, Trachtenberg FL, Yu J, Marceau LD, McKinlay JB, et al. Variations among primary care physicians in exercise advice, imaging, and analgesics for musculoskeletal pain: results from a factorial experiment. Arthritis Care Res (Hoboken) 2014;66(1):147–156. doi: 10.1002/acr.22143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Focht BC. Effectiveness of exercise interventions in reducing pain symptoms among older adults with knee osteoarthritis: a review. J Aging Phys Act. 2006;14(2):212–235. doi: 10.1123/japa.14.2.212. [DOI] [PubMed] [Google Scholar]
- 6.Fisher G, Hunter GR, Allison DB. Commentary: Physical activity does influence obesity risk when it actually occurs in sufficient amount. Int J Epidemiol. 2013;42(6):1845–1848. doi: 10.1093/ije/dyt163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loew L, Brosseau L, Wells GA, Tugwell P, Kenny GP, Reid R, et al. Ottawa panel evidence-based clinical practice guidelines for aerobic walking programs in the management of osteoarthritis. Arch Phys Med Rehabil. 2012;93(7):1269–1285. doi: 10.1016/j.apmr.2012.01.024. [DOI] [PubMed] [Google Scholar]
- 8.Barbour KE, Hootman JM, Helmick CG, Murphy LB, Theis KA, Schwartz TA, et al. Meeting physical activity guidelines and the risk of incident knee osteoarthritis: a population-based prospective cohort study. Arthritis Care Res (Hoboken) 2014;66(1):139–146. doi: 10.1002/acr.22120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.State-specific prevalence of walking among adults with arthritis--United States, 2011. Mmwr. 2013;62(17):331–334. [PMC free article] [PubMed] [Google Scholar]
- 10.Felson DT, Niu J, Guermazi A, Roemer F, Aliabadi P, Clancy M, et al. Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis and rheumatism. 2007;56(9):2986–2992. doi: 10.1002/art.22851. [DOI] [PubMed] [Google Scholar]
- 11.Felson DT, Anderson JJ, Naimark A, Walker AM, Meenan RF. Obesity and knee osteoarthritis. The Framingham Study. Ann Intern Med. 1988;109(1):18–24. doi: 10.7326/0003-4819-109-1-18. [DOI] [PubMed] [Google Scholar]
- 12.Latham NK, Mehta V, Nguyen AM, Jette AM, Olarsch S, Papanicolaou D, et al. Performance-based or self-report measures of physical function: which should be used in clinical trials of hip fracture patients? Arch Phys Med Rehabil. 2008;89(11):2146–2155. doi: 10.1016/j.apmr.2008.04.016. [DOI] [PubMed] [Google Scholar]
- 13.Cesari M, Kritchevsky SB, Penninx BW, Nicklas BJ, Simonsick EM, Newman AB, et al. Prognostic value of usual gait speed in well-functioning older people--results from the Health, Aging and Body Composition Study. Journal of the American Geriatrics Society. 2005;53(10):1675–1680. doi: 10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- 14.Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. The Journal of rheumatology. 1988;15(12):1833–1840. [PubMed] [Google Scholar]
- 16.Sharma L, Cahue S, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis and rheumatism. 2003;48(12):3359–3370. doi: 10.1002/art.11420. [DOI] [PubMed] [Google Scholar]
- 17.McHugh GA, Luker KA, Campbell M, Kay PR, Silman AJ. Pain, physical functioning and quality of life of individuals awaiting total joint replacement: a longitudinal study. J Eval Clin Pract. 2008;14(1):19–26. doi: 10.1111/j.1365-2753.2007.00777.x. [DOI] [PubMed] [Google Scholar]
- 18.Fransen M, Crosbie J, Edmonds J. Reliability of gait measurements in people with osteoarthritis of the knee. Physical therapy. 1997;77(9):944–953. doi: 10.1093/ptj/77.9.944. [DOI] [PubMed] [Google Scholar]
- 19.Curb JD, Ceria-Ulep CD, Rodriguez BL, Grove J, Guralnik J, Willcox BJ, et al. Performance-based measures of physical function for high-function populations. Journal of the American Geriatrics Society. 2006;54(5):737–742. doi: 10.1111/j.1532-5415.2006.00700.x. [DOI] [PubMed] [Google Scholar]
- 20.Resnick B, Nahm ES, Orwig D, Zimmerman SS, Magaziner J. Measurement of activity in older adults: reliability and validity of the Step Activity Monitor. Journal of nursing measurement. 2001;9(3):275–290. [PubMed] [Google Scholar]
- 21.Brandes M, Schomaker R, Mollenhoff G, Rosenbaum D. Quantity versus quality of gait and quality of life in patients with osteoarthritis. Gait Posture. 2008;28(1):74–79. doi: 10.1016/j.gaitpost.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 22.Song J, Semanik P, Sharma L, Chang RW, Hochberg MC, Mysiw WJ, et al. Assessing physical activity in persons with knee osteoarthritis using accelerometers: data from the osteoarthritis initiative. Arthritis Care Res (Hoboken) 2010;62(12):1724–1732. doi: 10.1002/acr.20305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 24.King WC, Li J, Leishear K, Mitchell JE, Belle SH. Determining activity monitor wear time: an influential decision rule. J Phys Act Health. 8(4):566–580. doi: 10.1123/jpah.8.4.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mudge S, Taylor D, Chang O, Wong R. Test-retest reliability of the Step Watch Activity Monitor outputs in healthy adults. J Phys Act Health. 7(5):671–676. doi: 10.1123/jpah.7.5.671. [DOI] [PubMed] [Google Scholar]
- 26.Tyo BM, Fitzhugh EC, Bassett DR, Jr, John D, Feito Y, Thompson DL. Effects of body mass index and step rate on pedometer error in a free-living environment. Medicine and science in sports and exercise. 2011;43(2):350–356. doi: 10.1249/MSS.0b013e3181e9b133. [DOI] [PubMed] [Google Scholar]
- 27.Feito Y, Bassett DR, Thompson DL. Evaluation of activity monitors in controlled and free-living environments. Medicine and science in sports and exercise. 2012;44(4):733–741. doi: 10.1249/MSS.0b013e3182351913. [DOI] [PubMed] [Google Scholar]
- 28.Peterfy C, Li J, Zaim S, Duryea J, Lynch J, Miaux Y, et al. Comparison of fixed flexion positioning with fluoroscopic semi-flexed positioning for quantifying radiographic joint-space width in the knee: test-retest reproducibility. Skeletal Radiol. 2003;32(3):128–132. doi: 10.1007/s00256-002-0603-z. [DOI] [PubMed] [Google Scholar]
- 29.Altman RD, Hochberg M, Murphy WA, Jr, Wolfe F, Lequesne M. Atlas of individual radiographic features in osteoarthritis. Osteoarthritis Cartilage. 1995;3(Suppl A):3–70. [PubMed] [Google Scholar]
- 30.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Annals of the rheumatic diseases. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Felson DT, McAlindon TE, Anderson JJ, Naimark A, Weissman BW, Aliabadi P, et al. Defining radiographic osteoarthritis for the whole knee. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 1997;5(4):241–250. doi: 10.1016/s1063-4584(97)80020-9. [DOI] [PubMed] [Google Scholar]
- 32.Guccione AA, Felson DT, Anderson JJ. Defining arthritis and measuring functional status in elders: methodological issues in the study of disease and physical disability. Am J Public Health. 1990;80(8):945–949. doi: 10.2105/ajph.80.8.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jordan J, Luta G, Renner J, Dragomir A, Hochberg M, Fryer J. Knee pain and knee osteoarthritis severity in self-reported task specific disability: the Johnston County Osteoarthritis Project. The Journal of rheumatology. 1997;24(7):1344–1349. [PubMed] [Google Scholar]
- 34.WHO. WHO Technical Report Series 894. Geneva: World Health Organization; 2000. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation. [PubMed] [Google Scholar]
- 35.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Medical care. 1996;34(1):73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 36.Radloff L. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 37.Leveille SG, Ling S, Hochberg MC, Resnick HE, Bandeen-Roche KJ, Won A, et al. Wide spread musculoskeletal pain and the progression of disability in older disabled women. Ann Intern Med. 2001;135(12):1038–1046. doi: 10.7326/0003-4819-135-12-200112180-00007. [DOI] [PubMed] [Google Scholar]
- 38.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 39.Glymour MM, Weuve J, Berkman LF, Kawachi I, Robins JM. When is baseline adjustment useful in analyses of change? An example with education and cognitive change. American journal of epidemiology. 2005;162(3):267–278. doi: 10.1093/aje/kwi187. [DOI] [PubMed] [Google Scholar]
- 40.Tudor-Locke C, Hatano Y, Pangrazi RP, Kang M. Revisiting "how many steps are enough?". Medicine and science in sports and exercise. 2008;40(7 Suppl):S537–S543. doi: 10.1249/MSS.0b013e31817c7133. [DOI] [PubMed] [Google Scholar]
- 41.Perkins NJ, Schisterman EF. The inconsistency of "optimal" cut points obtained using two criteria based on the receiver operating characteristic curve. American journal of epidemiology. 2006;163(7):670–675. doi: 10.1093/aje/kwj063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Akobeng AK. Understanding diagnostic tests 3: Receiver operating characteristic curves. Acta Paediatr. 2007;96(5):644–647. doi: 10.1111/j.1651-2227.2006.00178.x. [DOI] [PubMed] [Google Scholar]
- 43.White D, Tudor-Locke C, Felson D, Gross K, Nevitt M, Lewis C, et al. Do radiographic diease and pain account for why people with or at high risk of knee osteoarthritis do not meet Physical Activity Guidelines? Arthritis & Rheumatism. 2012 doi: 10.1002/art.37748. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.US Department of Health and Human Services. 2008 physical activity guidelines for Americans 2008. :1–10. http://www.health.gov/paguidelines/.
- 45.Tudor-Locke C, Bassett DR., Jr How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med. 2004;34(1):1–8. doi: 10.2165/00007256-200434010-00001. [DOI] [PubMed] [Google Scholar]
- 46.Fisher SR, Kuo YF, Sharma G, Raji MA, Kumar A, Goodwin JS, et al. Mobility After Hospital Discharge as a Marker for 30-Day Readmission. The journals of gerontology. 2012 doi: 10.1093/gerona/gls252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tudor-Locke CE, Myers AM. Methodological considerations for researchers and practitioners using pedometers to measure physical (ambulatory) activity. Res Q Exerc Sport. 2001;72(1):1–12. doi: 10.1080/02701367.2001.10608926. [DOI] [PubMed] [Google Scholar]
- 48.Schmidt MD, Cleland VJ, Shaw K, Dwyer T, Venn AJ. Cardiometabolic risk in younger and older adults across an index of ambulatory activity. Am J Prev Med. 2009;37(4):278–284. doi: 10.1016/j.amepre.2009.05.020. [DOI] [PubMed] [Google Scholar]
- 49.Wilde BE, Sidman CL, Corbin CB. A 10,000-step count as a physical activity target for sedentary women. Res Q Exerc Sport. 2001;72(4):411–414. doi: 10.1080/02701367.2001.10608977. [DOI] [PubMed] [Google Scholar]
- 50.White DK, Niu J, Zhang Y. Is symptomatic knee osteoarthritis a risk factor for a trajectory of fast decline in gait speed? Results from a longitudinal cohort study. Arthritis Care Res (Hoboken) 2013;65(2):187–194. doi: 10.1002/acr.21816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hartvigsen J, Christensen K. Active lifestyle protects against incident low back pain in seniors: a population-based 2-year prospective study of 1387 Danish twins aged 70–100 years. Spine (Phila Pa 1976) 2007;32(1):76–81. doi: 10.1097/01.brs.0000250292.18121.ce. [DOI] [PubMed] [Google Scholar]
- 52.Dunlop DD, Song J, Semanik PA, Sharma L, Chang RW. Physical activity levels and functional performance in the osteoarthritis initiative: a graded relationship. Arthritis and rheumatism. 2011;63(1):127–136. doi: 10.1002/art.27760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Leveille SG, Penninx BW, Melzer D, Izmirlian G, Guralnik JM. Sex differences in the prevalence of mobility disability in old age: the dynamics of incidence, recovery, and mortality. J Gerontol B Psychol Sci Soc Sci. 2000;55(1):S41–S50. doi: 10.1093/geronb/55.1.s41. [DOI] [PubMed] [Google Scholar]
- 54.Tudor-Locke C, Johnson WD, Katzmarzyk PT. Accelerometer-determined steps per day in US adults. Medicine and science in sports and exercise. 2009;41(7):1384–1391. doi: 10.1249/MSS.0b013e318199885c. [DOI] [PubMed] [Google Scholar]
- 55.Siegel PZ, Brackbill RM, Heath GW. The epidemiology of walking for exercise: implications for promoting activity among sedentary groups. American journal of public health. 1995;85(5):706–710. doi: 10.2105/ajph.85.5.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dunlop DD, Song J, Semanik PA, Chang RW, Sharma L, Bathon JM, et al. Objective physical activity measurement in the osteoarthritis initiative: Are guidelines being met? Arthritis and rheumatism. 2011;63(11):3372–3382. doi: 10.1002/art.30562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.White DK, Tudor-Locke C, Felson DT, Gross KD, Niu J, Nevitt M, et al. Walking to meet physical activity guidelines in knee osteoarthritis: Is 10,000 steps enough? Arch Phys Med Rehabil. 2012 doi: 10.1016/j.apmr.2012.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]