Abstract
AIM: To determine the rates of success and complications of precut biliary sphincterotomy (PBS) based on prior experience and to compare the complication rates between PBS and standard endoscopic sphincterotomy (ES).
METHODS: A retrospective evaluation of prospectively collected non-randomized data at an academic tertiary referral center. The study included all patients in an eight-year period who underwent PBS and ES by a single endoscopist who had no formal training in PBS. The main outcome measures of the study were success and complications of PBS with a comparison to complications of ES.
RESULTS: A total of 2939 endoscopic retrograde cholangiopancreatographies (ERCPs) were performed during the study period, including 818 (28%) ES and 150 (5%) PBS procedures. Selective biliary cannulation via PBS was successful at the first attempt in 75% of the patients. Cannulation was achieved in an additional 13% of the patients at a subsequent attempt (total 87%). Complication rate from PBS was 45% higher than ES, but did not differ significantly [7% (10/50) vs 5% (38/818), P = 0.29]. None of the complications from PBS was severe. A significant trend towards increasing success existed with regard to the endoscopist’s first attempt at precut (P = 0.0393, Cochran-Armitage exact test for trend, Z = -1.7588).
CONCLUSION: Despite the lack of specific training in this technique, PBS was performed with a high success rate and a complication rate similar to or less than reports from other experienced centers. These results suggest that endoscopic experience and perhaps innate endoscopic skill may play an important role in the outcome of this procedure.
Keywords: Biliary sphincterotomy, Precut sphincterotomy, Complication rate, Endoscopic skill
INTRODUCTION
Although endoscopic retrograde cholangiopancreatography (ERCP) was initially used only diagnostically, currently most ERCPs are performed for therapy and therefore, require selective ductal cannulation. Since the first endoscopic sphincterotomy was performed in 1974 by Kawai and Claussen, it has become the primary means of accessing the pancreaticobiliary system for treatment[1]. Standard cannulation techniques, however, fail between 5% and 10% of the time[2-4]. When cannulation cannot be achieved after several attempts with standard methods, precut biliary sphincterotomy (PBS) can be employed as an alternative means of gaining access to the duct. Precut sphincterotomies are used in 3.8%-19.2% of ERCP procedures with reported success rates ranging from 75% to 99% and complication rates from 1.9% to 30%[1,3,5-10]. One of the largest studies on precut sphincterotomies reported a success rate of 85.2% and a complication rate of 7.3%[11]. PBS is thought to carry a higher risk of complications such as pancreatitis, bleeding, infection, and perforation than standard endoscopic sphincterotomy (ES). Many of the concerns about PBS among experts, however, were based on findings from early studies[12-14]. Although multiple studies have shown that PBS carries a higher risk when performed by a less experienced endoscopist, reported complication rates from PBS are not significantly different than from standard sphincterotomy in most tertiary care centers[4,7,9,15]. Given the varied success and complication rates, we sought to evaluate these outcomes of PBS based on prior training and experience, and also to compare the complication rates of PBS to ES.
MATERIALS AND METHODS
This retrospective study evaluated the success and complication rate of ES and PBS by a single endoscopist (CMW) from September 1, 1998-April 27, 2006. The data were abstracted from data collected prospectively, and the study was approved by our Institutional Review Board. Previous experience included approximately 100 ERCPs during fellowship training from 1988-1989, approximately 68 ERCPs from 1990-1995 (over half therapeutic), and 45 ERCPs from 1995-September 1998. The endoscopist had performed no PBS procedures before 1998. Prior to performing PBS, the technique was reviewed in published articles and textbooks as well as from videotapes available at postgraduate courses. Data were collected prospectively, including patient history, indications for the procedure, and ERCP findings at the time of the procedure. Post-procedure follow-up was conducted by a nurse coordinator both at 24 h and then within the first month to evaluate the complications. If a first attempt of PBS was unsuccessful, a second attempt was made at a later time in some, but not all of the patients.
A standard catheter or sphincterotome was used to attempt cannulation of the common bile duct (CBD). If this method failed, a glidewire was next used in combination with a sphincterotome to attempt selective biliary cannulation (Boston Scientific, Natick, MA). If selective cannulation was still unsuccessful, precut sphincterotomy was then attempted using a standard needle-knife with pure cutting current with or without prior placement of a pancreatic duct stent[4,15].
The precut method used was similar to the technique described by Mavrogiannis for the removal of CBD stones[16]. The PBS incision began between the 11:00 and 1:00 positions in the middle to upper part of the intraduodenal portion of the CBD. The incision was extended downward in the direction of the papillary orifice. Additional incisions were made until gentle probing with the needle knife catheter entered the bile duct. If necessary, the sphincterotomy was further extended using a standard sphincterotome and blended current[11,16]. The decision to use a pancreatic stent was based upon the size of the papilla (small) and the perceived risk of pancreatitis. For example, if the major papilla was bulbous and precut sphincterotomy felt simpler, then a pancreatic duct stent was not placed. When a stent was used, either a 5-French single pigtail or a 3-French single pigtail stent was placed prior to precut sphincterotomy. ES was performed using a braided wire sphincterotome (Cook Endoscopy Inc., Winston Salem, N.C.). Most of these were performed using pure cutting current. Over the last year, the procedures were performed using an ERBE device. Success of PBS was defined as the ability to deeply cannulate the common bile duct. Complications were classified using the criteria previously published by Cotton et al[17]. All patients gave written informed consent for the procedure and the study was approved by the institutional review board of our institution. Variables were compared using Chi-square or Fisher’s exact test and t-tests as appropriate. The Cochran-Armitage exact test for trend (1-tailed) was used to determine if there was an increasing trend for success over time. P < 0.05 was considered statistically significant.
RESULTS
A total of 2939 ERCPs were performed by a single endoscopist (CMW) during the study period, including 818 (28%) ES and 150 (5%) PBS procedures. Some overlap occurred between these two groups in patients who had both procedures performed during the study period. The average age in the total group of 150 patients was 58.5 years (range, 11-92 years), and 67% (n = 101) of these patients were female (data not shown). The indications for sphincterotomy were similar between those undergoing ES and PBS. The most frequent indications for PBS were, in order of prevalence: stones, malignancy, biliary dilatation, and stricture (Table 1). Sphincter of Oddi dysfunction (SOD) was the indication in only one of the 150 patients who underwent PBS. The percentage of PBS, both of the total number of ERCPs and ES, ranged from 4% to 8% and from 14% to 30% respectively, but did not trend up or down during the study period (data not shown).
Table 1.
Indications for precut and standard biliary sphincterotomy
| Indication | PBS (%) | ES (%) | 1P |
| n = 150 | n = 818 | ||
| Stones | 27 | 35 | 0.04a |
| Malignancy | 15 | 3 | < 0.001c |
| Biliary dilatation | 15 | 10 | 0.07 |
| Stricture | 11 | 2 | < 0.001c |
| Bile leak | 9 | 4 | 0.006b |
| Pancreatitis | 8 | 15 | 0.017a |
| Jaundice | 5 | 3 | 0.36 |
| Stent | 1 | 6 | 0.19 |
| Elevated LFTs | 2 | 2 | 0.74 |
| Cholangitis | 1 | 1 | 1.00 |
| r/o SOD | 1 | 8 | 0.002b |
P < 0.5,
P < 0.01,
P < 0.001 expressed as PBS vs ES using Chi-square (or Fisher’s exact test where appropriate). PBS: precut biliary sphincterotomy; ES: endoscopic sphincterotomy.
Based on selective ductal cannulation, PBS was successful with the first attempt in 75% of the patients. Cannulation was achieved in an additional 13% of the patients during a subsequent attempt usually performed within 1 wk, yielding a cumulative PBS success rate of 87% (95% CI, 81%-92%).
Overall, the total complication rate of all 2939 ERCPs performed during the study period was 4%, while the complication rate of the 150 PBS procedures was 7% (95% CI, 4%-12%). This complication rate resulting from PBS was 45% higher than that (5%) resulting from the 818 ES procedures (95% CI, 3%-6%). However, the difference was not significant (P = 0.29) (Table 2). Of the ten PBS-related complications (7%), six were pancreatitis and four were bleeding. Of these six patients, pancreatitis was classified as mild in four and moderate in two patients with pancreatic duct stents placed before PBS. Bleeding complication was classified as mild in one patient and as moderate in the other three patients. None of the ten complications was classified as severe and there were no infections or perforations.
Table 2.
Complications: ES vs PBS
| ES (%) | PBS (%) | P | |
| Pancreatitis | 2.7 | 4 | 0.38 |
| Bleeding | 1.3 | 2.7 | 0.23 |
| Infection | 0.5 | 0 | 0.39 |
| Perforation | 0.1 | 0 | 0.67 |
| Total | 4.6 | 6.7 | 0.29 |
PBS: precut biliary sphincterotomy; ES: endoscopic sphincterotomy.
In order to gauge success over time, the 150 PBS procedures performed in the study were divided arbitrarily in chronological order into six groups, 25 patients in each group (Table 3). None of the six groups varied significantly from the total number of patients who underwent PBS with regard to age, gender, or diagnosis (data not shown). A pancreatic duct stent was placed in 41 cases (27%) of the 150 patients undergoing PBS. Stenting was increasingly used in group 5 (48% of the cases in the group) compared with 16%-28% of the cases in the other five groups. The total success rate of PBS increased over the study period from 84% in group 1 compared to 92% in group 6 (P = 0.67) (Table 3). Success during the first attempt at PBS also increased from 64% in group 1 to 84% in group 6 (P = 0.11). Similarly, the complication rate decreased over time from 8% in group 1 to 0% in group 5 and 4% in group 6 (P = 0.49, P = 1.00, respectively). The small number of patients may explain the lack of statistical significance between the groups. There was a significant trend towards increasing success for primary PBS over the time period (P = 0.0393, Cochran-Armitage exact test for trend, Z = -1.7588) (Figure 1).
Table 3.
One hundred and fifty precuts performed in the 6 groups during the study period
| Group 1 (%) | Group 2 (%) | Group 3 (%) | Group 4 (%) | Group 5 (%) | Group 6 (%) | Total(%) | |
| 1º success | 64 | 68 | 76 | 80 | 76 | 84 | 74.7 |
| 2º success | 20 | 16 | 12 | 8 | 12 | 8 | 12.7 |
| Total success | 84 | 84 | 88 | 88 | 88 | 921 | 87.3 |
| Complications | 8 | 8 | 16 | 4 | 0 | 4 | 6.7 |
| PD stent | 20 | 28 | 24 | 28 | 48 | 16 | 27.3 |
Indicates the success rates compared in the discussion. 1o success: successful cannulation of the duct at the first attempt; 2o success: successful cannulation of the duct at a subsequent attempt. PD: pancreatic duct.
Figure 1.
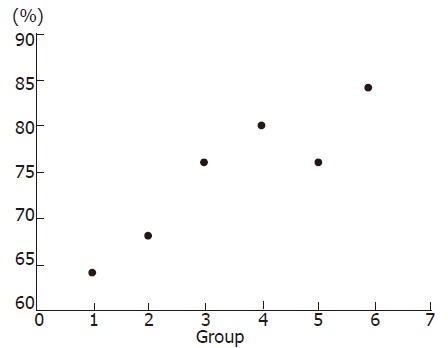
Trend analysis of primary success of PBS. The success rate of the first attempt at PBS in six chronological groups of 25 patients demonstrates an overall trend towards success over time (P = 0.0393, Cochran-Armitage exact test for trend, Z = -1.7588). Success rate in the six groups respectively is 64%, 68%, 76%, 80%, 76%, and 84%.
DISCUSSION
Our findings are consistent with other large trials showing that PBS is a safe and effective alternative to standard techniques when deep cannulation is required and when the procedure is performed by a skilled endoscopist. Although our study reports a higher complication rate for PBS than for ES (7% vs 5%), these rates are not significantly different. Lack of significance could possibly be explained by the relatively small number of patients. Although comparing results from multiple endoscopists would provide more information, we had ES and PBS data from only one endoscopist over a prolonged period of time.
Our results suggest that the PBS success rate is directly proportional and the complication rate is inversely proportional to the volume of procedures performed. Total success in PBS increased from 84% in group 1 to 92% in group 6. The greatest proportion of improvement was in the first attempt at precut with a significant trend towards increasing success rates in this area over time (P = 0.0393). Ten procedures out of 150 PBS resulted in complications: 6 pancreatitis (4 mild, 2 moderate) and 4 bleeding (1 mild, 3 moderate). Eight of these ten complications occurred early in the study period (groups 1-3). Therefore, the number of complications decreased throughout the study, with only one mild and one moderate bleeding complication in the latter half of the study. This decline in complications differs from the results reported in a similar study showing that while precut success increases as the endoscopist gains more experience, the complication rate generally reaches a plateau after an initial decline[11].
One possible explanation for a decline in complications over time is the increased use of a pancreatic stent in the latter part of the study period. Placement of a pancreatic stent prior to a precut or pancreatic sphincterotomy is often used to help prevent post-ERCP pancreatitis, especially in the setting of suspected SOD[11,18]. A study by Harewood and Baron reporting a precut complication rate of 15% (out of 253 PBS procedures) attributes their higher number of complications in part to a lack of PD stent placement[11]. Sherman et al[15] reported a complication rate of 14% in their unstented controls compared with a 2% rate of pancreatitis in patients with a PD stent placed. In our study, a PD stent was used in 48% of the procedures in group 5, compared with an average of 23% of the time in the other five groups. Group 5 had a 0% complication rate compared with 4%-16% in the other groups. Therefore, our results are consistent with other findings showing that the rate of pancreatitis is higher in the absence of a pancreatic stent.
Our low number of complications from PBS may also be directly related to the indications for the procedure. Several studies have identified SOD as a risk factor for pancreatitis following both ES and PBS[5,15,19]. The small number of SOD patients requiring PBS in our study (1/150) is one explanation for the low complication rate. However, we also hypothesize that endoscopist expertise may play a significant role in determining complication rate since our rate is lower than a 12% PBS complication rate reported by a series that excluded any patient with suspicion of SOD[3].
A problem with evaluation of the safety of PBS is the lack of an equal alternative procedure for comparison. Although we did not directly evaluate the success rate of ES in this study, the rate nears 100%. Our series evaluates the complication rates of PBS vs ES performed by one endoscopist with a high volume of ERCPs per year. Although precut is often evaluated against standard sphincterotomy, we recognize that the two procedures are not equal for comparison since the clinical indications are often very different[12,20]. A duct that is easily cannulated differs from a duct that cannot be entered using standard methods. Failed cannulation itself creates a new scenario that carries a higher risk of complications. For example, higher rates of pancreatitis from PBS can partly be explained by the additional manipulation of the duct during several unsuccessful attempts at cannulation[1,2,5,21]. Therefore, trauma to the duct while trying to gain access to it may be the direct cause of pancreatitis in many cases, rather than the actual precut.
The issue of who should perform PBS remains controversial. While formalized post-fellowship training is strongly recommended and more likely today as programs are moving to the third tier endoscopic training, our results suggest that the procedure can be performed with a high level of success and safety by an endoscopist skilled in ERCP. However, we must emphasize that a baseline competence in therapeutic ERCP is mandatory before performing the procedure given the risks as well as medicolegal implications[22]. Our results confirm the notion that endoscopic skills are variable even among those with similar training, suggesting that innate endoscopic skills may be important. For example, specialized training in PBS may not necessarily confer high success and low complication rates subsequently.
In summary, both success and complication rates of PBS may improve with increased endoscopist experience. Our findings justify the conclusions of other studies that PBS is an effective alternative to gain access to the common bile duct when performed in appropriate circumstances by an experienced endoscopist. Not only does success rate of PBS increase with experience, the complication rate may concurrently decline over time. Given the lack of post-fellowship training in PBS by the endoscopist in our study, extensive ERCP experience coupled with innate endoscopist expertise and appropriate use of PBS may determine the successful performance and low complication rate of this procedure. Future studies examining the use of PBS in a community setting with explicit information regarding prior training, success, and complications would be helpful in putting this procedure in proper perspective regarding who should be employing this technique.
Footnotes
S- Editor Liu Y L- Editor Wang XL E- Editor Wang HF
References
- 1.Maydeo A, Borkar D. Techniques of selective cannulation and sphincterotomy. Endoscopy. 2003;35:S19–S23. doi: 10.1055/s-2003-41532. [DOI] [PubMed] [Google Scholar]
- 2.Sriram PV, Rao GV, Nageshwar Reddy D. The precut--when, where and how A review. Endoscopy. 2003;35:S24–S30. doi: 10.1055/s-2003-41528. [DOI] [PubMed] [Google Scholar]
- 3.Kahaleh M, Tokar J, Mullick T, Bickston SJ, Yeaton P. Prospective evaluation of pancreatic sphincterotomy as a precut technique for biliary cannulation. Clin Gastroenterol Hepatol. 2004;2:971–977. doi: 10.1016/s1542-3565(04)00484-7. [DOI] [PubMed] [Google Scholar]
- 4.Huibregtse K, Katon RM, Tytgat GN. Precut papillotomy via fine-needle knife papillotome: a safe and effective technique. Gastrointest Endosc. 1986;32:403–405. doi: 10.1016/s0016-5107(86)71921-4. [DOI] [PubMed] [Google Scholar]
- 5.Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909–918. doi: 10.1056/NEJM199609263351301. [DOI] [PubMed] [Google Scholar]
- 6.Sherman S, Ruffolo TA, Hawes RH, Lehman GA. Complications of endoscopic sphincterotomy. A prospective series with emphasis on the increased risk associated with sphincter of Oddi dysfunction and nondilated bile ducts. Gastroenterology. 1991;101:1068–1075. [PubMed] [Google Scholar]
- 7.Freeman ML. Precut (access) sphincterotomy. Tech Gastrointest Endosc. 1999;1:40–48. [Google Scholar]
- 8.Shakoor T, Geenen JE. Pre-cut papillotomy. Gastrointest Endosc. 1992;38:623–627. doi: 10.1016/s0016-5107(92)70537-9. [DOI] [PubMed] [Google Scholar]
- 9.Freeman ML. Adverse outcomes of ERCP. Gastrointest Endosc. 2002;56:S273–S282. doi: 10.1067/mge.2002.129028. [DOI] [PubMed] [Google Scholar]
- 10.Foutch PG. A prospective assessment of results for needle-knife papillotomy and standard endoscopic sphincterotomy. Gastrointest Endosc. 1995;41:25–32. doi: 10.1016/s0016-5107(95)70272-5. [DOI] [PubMed] [Google Scholar]
- 11.Harewood GC, Baron TH. An assessment of the learning curve for precut biliary sphincterotomy. Am J Gastroenterol. 2002;97:1708–1712. doi: 10.1111/j.1572-0241.2002.05829.x. [DOI] [PubMed] [Google Scholar]
- 12.Rollhauser C, Johnson M, Al-Kawas FH. Needle-knife papillotomy: a helpful and safe adjunct to endoscopic retrograde cholangiopancreatography in a selected population. Endoscopy. 1998;30:691–696. doi: 10.1055/s-2007-1001390. [DOI] [PubMed] [Google Scholar]
- 13.Cotton PB. Precut papillotomy--a risky technique for experts only. Gastrointest Endosc. 1989;35:578–579. doi: 10.1016/s0016-5107(89)72921-7. [DOI] [PubMed] [Google Scholar]
- 14.Baillie J. Needle knife sphincterotomy. Gastrointest Endosc. 1991;37:650. doi: 10.1016/s0016-5107(91)70880-8. [DOI] [PubMed] [Google Scholar]
- 15.Sherman S, Hawes R, Earle D, Baute P, Buckshot L, Lehman G. Does leaving a main pancreatic duct stent in place reduce the incidence of precut biliary sphincterotomy (ES)-induced pancreatitis? A final analysis of a randomized prospective study. Gastrointest Endosc. 1996;3:413A (abstract). doi: 10.1016/j.gie.2012.08.022. [DOI] [PubMed] [Google Scholar]
- 16.Mavrogiannis C, Liatsos C, Romanos A, Petoumenos C, Nakos A, Karvountzis G. Needle-knife fistulotomy versus needle-knife precut papillotomy for the treatment of common bile duct stones. Gastrointest Endosc. 1999;50:334–339. doi: 10.1053/ge.1999.v50.98593. [DOI] [PubMed] [Google Scholar]
- 17.Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383–393. doi: 10.1016/s0016-5107(91)70740-2. [DOI] [PubMed] [Google Scholar]
- 18.Tarnasky PR, Palesch YY, Cunningham JT, Mauldin PD, Cotton PB, Hawes RH. Pancreatic stenting prevents pancreatitis after biliary sphincterotomy in patients with sphincter of Oddi dysfunction. Gastroenterology. 1998;115:1518–1524. doi: 10.1016/s0016-5085(98)70031-9. [DOI] [PubMed] [Google Scholar]
- 19.Freeman ML, Guda NM. Prevention of post-ERCP pancreatitis: a comprehensive review. Gastrointest Endosc. 2004;59:845–864. doi: 10.1016/s0016-5107(04)00353-0. [DOI] [PubMed] [Google Scholar]
- 20.Baron TH. Complications of endoscopic biliary sphincterotomy: the first cut is the deepest. Clin Gastroenterol Hepatol. 2004;2:968–970. doi: 10.1016/s1542-3565(04)00439-2. [DOI] [PubMed] [Google Scholar]
- 21.Freeman ML, Nelson DB, Sherman S. Pancreatitis from endoscopic sphincterotomy (ES): a prospective multi-centre, 30-day study (abstract). Gastrointest Endosc. 1994;40:108. [Google Scholar]
- 22.Cotton PB. Analysis of 59 ERCP lawsuits; mainly about indications. Gastrointest Endosc. 2006;63:378–382; quiz 464. doi: 10.1016/j.gie.2005.06.046. [DOI] [PubMed] [Google Scholar]


