Abstract
Pancreatic tumors are primary in most of the cases. Pancreatic metastases associated with other primary malignancies, especially pancreatic metastasis of leiomyosarcoma, are uncommon. A 66-year-old woman underwent surgical resection of malignant mesenchymoma (70% osteosarcoma and 30% leiomyosarcoma) in the right thigh. In the postoperative period, a pancreatic mass was identified radiologically by abdominal computed tomography. Pylorus-preserving pancreaticoduodenectomy was performed. The surgical specimen revealed leiomyosarcoma metastasized to the pancreas. A metastatic nodule on the remnant pancreatic tail was discovered 9 mo after the first pancreatic resection, and distal pancreatectomy was performed. Cases of pancreatic metastasis from leiomyosarcoma are extremely rare, especially when the tumor was resectable. We report here a unique case of pancreatic metastasis from a leiomyosarcoma in the right thigh that had been treated surgically.
Keywords: Pancreatic tumor, Leiomyosarcoma, Meta-stasis
INTRODUCTION
The occurrence of metastatic lesions in the pancreas is very uncommon. The incidence of metastatic pancreatic tumors is 1.6%-11% at autopsy[1,2]. The majority of patients with pancreatic metastasis have widespread diseases. Isolated, potentially resectable pancreatic metastasis is detected infrequently. Therefore, resection of metastatic tumors of the pancreas has been occasionally reported, and its role in improving the survival or quality of life is not clearly defined[3,4]. However, some recent studies have reported that surgical resection can be performed in selected patients with isolated pancreatic metastases, achieving long-term survival and good palliation[1,5]. We report here a case of pancreatic metastatic from leiomyosarcoma of the right anterior thigh, which was treated by surgical resection, and review the literature about pancreatic metastasis.
CASE REPORT
A 66-year-old woman was referred to our hospital with a mass in the right thigh (Figure 1). In September 2005, she had undergone surgical resection for this mass. Malignant mesenchymoma (70% osteosarcoma and 30% leiomyosarcoma) was diagnosed histologically. In the postoperative period, abdominal computed tomography (CT) identified a pancreatic mass. The patient complained of non-specific abdominal discomfort. Laboratory findings were all within normal limits. The levels of the tumor markers including carcinoembryonic agent and carbohydrate antigen 19-9, were within the normal ranges. Abdominal CT revealed a mass at the head of the pancreas. Magnetic resonance imaging of the abdomen showed a low-intensity mass on T1-weighted images and a non-homogeneous high-intensity mass on T2-weighted images. No evidence of other distant metastases was seen (Figure 1). At laparotomy, a fixed mass of 4 cm or so in length was palpated at the head of the pancreas, displacing the surrounding duodenum. Therefore, pylorus-preserving pancreaticoduodenectomy was performed. Macroscopic examination of the operative specimen showed a 4 cm × 3 cm lobulated solid mass with a thin wall. Microscopic examination revealed a malignant neoplasm with predominance of spindle cells. The tumor cells were immunoreactive for desmin. Metastatic leiomyosarcoma was diagnosed histologically (Figure 2). The postoperative course was uneventful. We recommended systemic chemotherapy to the patient, but she declined. Nine months after the first pancreatic resection, a follow-up abdominal CT showed development of a new 1-cm mass in the remnant tail of the pancreas (Figure 1). Distal pancreatectomy was performed. The tumor showed the same microscopic findings, and leiomyosarcoma was also diagnosed histologically.
Figure 1.
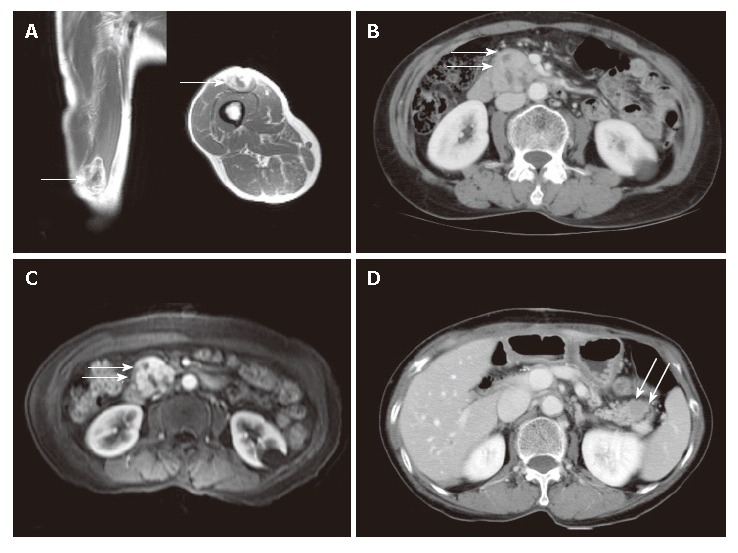
Radiological findings. A: Gadolinium-enhanced T1 weighted image showing a soft tissue tumor in the muscle of the anterior thigh; B: Contrast-enhanced abdominal CT scan showing a heterogeneously enhanced mass at the head of the pancreas; C: Gadolinium-enhanced T1 weighted image showing a well-enhanced mass with necrotic foci at the head of the pancreas; D: Follow-up CT obtained after 10 mo showing a low attenuated mass in the tail of the pancreas.
Figure 2.
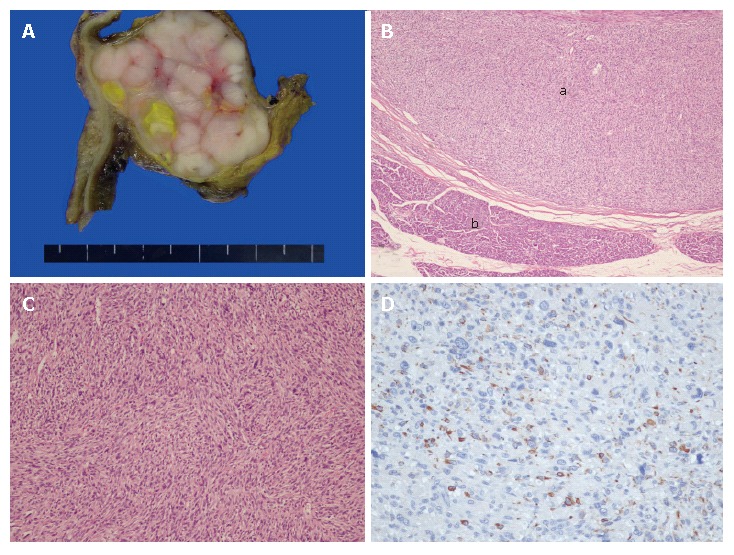
Gross and microscopic findings for metastatic leiomyo-sarcoma. A: The section reveals a whitish solid tumor with a lobulated pattern and a yellowish necrotic portion, abutting duodenal wall on the left side, and compressed pancreatic head tissue on the right side; B: Low-power view displaying eosinophilic intersecting fascicles circumscribed by a fibrous capsule (a) and adjacent normal pancreatic tissue (b) (hematoxylin and eosin stain ×40); C: Cellular proliferation of atypical spindle tumor cells is accompanied by nuclear atypia and hyperchromasia (hematoxylin and eosin stain × 200); D: Tumor cells show immunoreactivity for desmin.
DISCUSSION
Metastatic lesions in the pancreas are uncommon. Adsay et al[1] reviewed pathological specimens from 4955 adult autopsy cases in an attempt to identify tumors that had metastasized to the pancreas. There were only 81 (1.6%) cases of metastatic tumors, the majority of which were of epithelial origin, and the most common sites of the primary lesions were the lung, kidney, and gastrointestinal tract. However, a few cases of leiomyosarcoma with metastases to the pancreas have been reported. Primary sites of leiomyosarcomas included the uterus[6,7], ovary[8], veins[9], spermatic cord[10], intestine[3,10], retroperitoneum[2,11], and soft tissue[11,12]. To the best of our knowledge, including the present case, only 16 cases of pancreatic metastasis from leiomyosarcoma have been reported to date in the English language literature[7,8,12].
The differential diagnosis between a solitary metastatic tumor and primary pancreatic carcinoma may be very difficult as signs and symptoms are similar for both primary and secondary tumors, and radiological imaging is unable to differentiate primary from secondary pancreatic lesions[13]. In our case, non-specific abdominal pain appeared to be the most common symptom. The symptoms of pancreatic metastases often include pain, weight loss, obstructive jaundice, and duodenal obstruction, which are very similar to the symptoms of primary pancreatic cancer[1,3,9]. Therefore, pre-operative diagnosis is challenging, and considerable caution is needed for patients with a previous history of non-pancreatic neoplastic disease. The pre-operative diagnosis of our case was primarily a non-functioning islet cell tumor of pancreas, although the patient had previously undergone surgical treatment for mesenchymoma of the left leg. Various diagnostic tools have been used to assess tumors. In recent years, 18-FDG-PET has proven to be useful for the accurate staging of tumors[3]. Percutaneous fine-needle aspiration (FNA) is found helpful in establishing the correct preoperative diagnosis, especially in patients who are not amenable to surgery, and in assisting in decisions related to the possibility and type of chemotherapy[3]. However, with the exception of postoperative histology, there is no definitive method for unambiguous diagnosis.
Metastatic tumors of the pancreas are usually diagnosed at an advanced stage, and solitary resectable metastasis occurs less frequently. Therefore, metastatic tumors of the pancreas are rarely treated surgically. Sperti et al[3] reported that 8/259 (3%) pancreatic resections were performed for pancreatic metastases. Therefore, our patient represents a very unusual case.
Only a few cases of pancreatic metastasis from sarcomas have been reported. Experience is limited, and the effectiveness of surgery for these types of lesions has not been clearly established. However, long-term survival may be conferred by ‘‘curative’’ resection for pancreatic metastasis from visceral or soft tissue sarcoma[3,7,9,14]. It is clear that surgical excision has the potential to improve prognosis if the primary site and other metastases are well-controlled. In the present unique case, pancreatic metastasis from leiomyosarcoma was diagnosed, and the patient underwent pancreatectomy twice in 10 mo. An attempt at complete tumor resection can offer patients the best hope of prolonged survival.
Footnotes
S- Editor Liu Y L- Editor Ma JY E- Editor Ma WH
References
- 1.Crippa S, Angelini C, Mussi C, Bonardi C, Romano F, Sartori P, Uggeri F, Bovo G. Surgical treatment of metastatic tumors to the pancreas: a single center experience and review of the literature. World J Surg. 2006;30:1536–1542. doi: 10.1007/s00268-005-0464-4. [DOI] [PubMed] [Google Scholar]
- 2.Adsay NV, Andea A, Basturk O, Kilinc N, Nassar H, Cheng JD. Secondary tumors of the pancreas: an analysis of a surgical and autopsy database and review of the literature. Virchows Arch. 2004;444:527–535. doi: 10.1007/s00428-004-0987-3. [DOI] [PubMed] [Google Scholar]
- 3.Sperti C, Pasquali C, Liessi G, Pinciroli L, Decet G, Pedrazzoli S. Pancreatic resection for metastatic tumors to the pancreas. J Surg Oncol. 2003;83:161–166; discussion 166. doi: 10.1002/jso.10262. [DOI] [PubMed] [Google Scholar]
- 4.Roland CF, van Heerden JA. Nonpancreatic primary tumors with metastasis to the pancreas. Surg Gynecol Obstet. 1989;168:345–347. [PubMed] [Google Scholar]
- 5.Hiotis SP, Klimstra DS, Conlon KC, Brennan MF. Results after pancreatic resection for metastatic lesions. Ann Surg Oncol. 2002;9:675–679. doi: 10.1007/BF02574484. [DOI] [PubMed] [Google Scholar]
- 6.Iwamoto I, Fujino T, Higashi Y, Tsuji T, Nakamura N, Komokata T, Douchi T. Metastasis of uterine leiomyosarcoma to the pancreas. J Obstet Gynaecol Res. 2005;31:531–534. doi: 10.1111/j.1447-0756.2005.00344.x. [DOI] [PubMed] [Google Scholar]
- 7.Falconi M, Crippa S, Sargenti M, Capelli P, Pederzoli P. Pancreatic metastasis from leiomyosarcoma of the broad ligament of the uterus. Lancet Oncol. 2006;7:94–95. doi: 10.1016/S1470-2045(05)70543-X. [DOI] [PubMed] [Google Scholar]
- 8.Nasu M, Inoue J, Matsui M, Minoura S, Matsubara O. Ovarian leiomyosarcoma: an autopsy case report. Pathol Int. 2000;50:162–165. doi: 10.1046/j.1440-1827.2000.01020.x. [DOI] [PubMed] [Google Scholar]
- 9.Le Borgne J, Partensky C, Glemain P, Dupas B, de Kerviller B. Pancreaticoduodenectomy for metastatic ampullary and pancreatic tumors. Hepatogastroenterology. 2000;47:540–544. [PubMed] [Google Scholar]
- 10.Wernecke K, Peters PE, Galanski M. Pancreatic metastases: US evaluation. Radiology. 1986;160:399–402. doi: 10.1148/radiology.160.2.3523591. [DOI] [PubMed] [Google Scholar]
- 11.Nakamura E, Shimizu M, Itoh T, Manabe T. Secondary tumors of the pancreas: clinicopathological study of 103 autopsy cases of Japanese patients. Pathol Int. 2001;51:686–690. doi: 10.1046/j.1440-1827.2001.01258.x. [DOI] [PubMed] [Google Scholar]
- 12.Boudghène FP, Deslandes PM, LeBlanche AF, Bigot JM. US and CT imaging features of intrapancreatic metastases. J Comput Assist Tomogr. 1994;18:905–910. doi: 10.1097/00004728-199411000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Ishigure K, Kaneko T, Takeda S, Inoue S, Kawase Y, Nakao A. Pancreatic metastasis from leiomyosarcoma in the back. Hepatogastroenterology. 2003;50:1675–1677. [PubMed] [Google Scholar]
- 14.Nakajima Y, Kakizaki S, Kanda D, Shimada Y, Sohara N, Sato K, Takagi H, Mori M, Watanabe H. Pancreatic and gastric metastases of leiomyosarcoma arising in the left leg. Int J Clin Oncol. 2005;10:342–347. doi: 10.1007/s10147-005-0487-8. [DOI] [PubMed] [Google Scholar]


