Abstract
Splenic abscess is a rare entity normally associated with underlying diseases. We report a case of splenic abscess with large gas formation in a non-diabetic and non-immunosuppressed patient after surgery for colon perforation. The most frequent cause of splenic abscess is septic embolism arising from bacterial endocarditis. Splenic abscess has a high rate of mortality when it is diagnosed late. Computed tomography resolved any diagnostic doubt, and subsequent surgery confirmed the diagnosis.
Keywords: Splenic abscess, Colon perforation
INTRODUCTION
The incidence of septic complications, such as abscess formation, in fecal peritonitis due to colon perforation has been reported in various organs[1,2]. The spleen is one of the least involved organs especially in non-diabetic and non-immunosuppressed patients[3,4]. In a recent review[5], out of 67 cases of splenic abscess, only one was due to colon perforation. We present a patient with persistent high fever two weeks after surgery due to colon perforation despite optimal treatment. An occult splenic abscess was found during diagnostic work up.
CASE REPORT
An 84-year-old Caucasian non-diabetic and non-immunosuppressed woman presented with abdominal tenderness and peritoneal irritation. Chest radiography revealed free air at the left subdiaphragmatic area confirming a hollow visceral perforation. An exploratory laparotomy revealed traumatic perforation of the sigmoid due to chicken bone with diffuse fecal peritonitis. The postoperative period was uneventful with complete recovery and the patient was discharged on the 8th postoperative day. Two weeks later the patient complained of high fever (40°C) and vague left upper quadrant pain. The chest X-ray documented left pleural effusion associated with a left subdiaphragmatic abscess by ultrasound. The white cell count was 13 000 cells/mL with neutrophil predominance (85%). Computed tomography with contrast enhancement revealed a large splenic abscess associated with a vast amount of gas formation (Figure 1). The patient underwent exploratory laparotomy with splenectomy and recovered completely on the 7th postoperative day. Culture of the purulent material showed Enterococcus sensitive to vancomycin.
Figure 1.
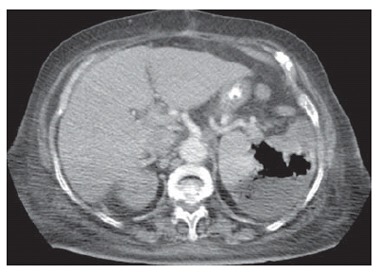
Computed tomography with contrast enhancement revealed a large splenic abscess associated with a vast amount of gas formation.
DISCUSSION
Splenic abscess is a very rare manifestation of fecal peritonitis especially in non-diabetic and non-immunocompromised patients[3,4]. Successful management requires a combination of early diagnosis and early surgery or imaging-guided intervention[6,7].
Splenic abscess can be identified by ultrasonography. However, ultrasonography can not discriminate between abscess and infarct in some cases, while large gas formation within the abscess may lead to technical difficulties. Gas formation when noted within splenic abscesses is associated mainly with gram negative bacillus infection. In a recent review[5], gas formation in splenic abscess was found in 11.9% of patients.
Computed tomography is the examination of choice. Splenic abscesses appear as focal areas of low attenuation. Usually there is no inflammatory rim. Gas collections are very rarely seen. Many abscesses remain uniformly hypoattenuating after contrast administration and do not show peripheral enhancement. In atypical cases, clinical presentation must be considered in order to make an accurate diagnosis.
In conclusion, after fecal peritonitis although an intra-abdominal abscess in the proximity of the primary lesion is rather common, an unexpected splenic abscess formation, despite the patient immune status, could also be a rare but possible complication.
Footnotes
S- Editor Liu Y L- Editor Ma JY E- Editor Lu W
References
- 1.Alonso Cohen MA, Galera MJ, Ruiz M, Puig la Calle J, Ruis X, Artigas V, Puig la Calle J. Splenic abscess. World J Surg. 1990;14:513–516; discussion 516-517. doi: 10.1007/BF01658678. [DOI] [PubMed] [Google Scholar]
- 2.Gadacz TR. Splenic abscess. World J Surg. 1985;9:410–415. doi: 10.1007/BF01655275. [DOI] [PubMed] [Google Scholar]
- 3.Nelken N, Ignatius J, Skinner M, Christensen N. Changing clinical spectrum of splenic abscess. A multicenter study and review of the literature. Am J Surg. 1987;154:27–34. doi: 10.1016/0002-9610(87)90285-6. [DOI] [PubMed] [Google Scholar]
- 4.Pomerantz RA, Eckhauser FE, Thornton JW, Strodel WE, Knol JA, Zuidema GD. Covert splenic abscess: a continuing challenge. Am Surg. 1986;52:386–390. [PubMed] [Google Scholar]
- 5.Chang KC, Chuah SK, Changchien CS, Tsai TL, Lu SN, Chiu YC, Chen YS, Wang CC, Lin JW, Lee CM, et al. Clinical characteristics and prognostic factors of splenic abscess: a review of 67 cases in a single medical center of Taiwan. World J Gastroenterol. 2006;12:460–464. doi: 10.3748/wjg.v12.i3.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smyrniotis V, Kehagias D, Voros D, Fotopoulos A, Lambrou A, Kostopanagiotou G, Kostopanagiotou E, Papadimitriou J. Splenic abscess. An old disease with new interest. Dig Surg. 2000;17:354–357. doi: 10.1159/000018878. [DOI] [PubMed] [Google Scholar]
- 7.Tikkakoski T, Siniluoto T, Päivänsalo M, Taavitsainen M, Leppänen M, Dean K, Koivisto M, Suramo I. Splenic abscess. Imaging and intervention. Acta Radiol. 1992;33:561–565. [PubMed] [Google Scholar]


