Abstract
AIM: To study the role of retrograde terminal ileoscopy in patients suspected to have ileocolonic tuberculosis.
METHODS: A retrospective analysis was performed for patients undergoing colonoscopy for suspected ileocolonic tuberculosis between January 2000 and June 2004, in whom retrograde ileoscopy had been performed. Only patients diagnosed with tuberculosis on the basis of histological findings of either a caseating granuloma or those having non-caseating granuloma or a collection of epithelioid cells at a minimum of one endoscopic lesion (either in the colon or the terminal ileum) on histology with good responses to conventional anti-tuberculous drugs were enrolled for the study.
RESULTS: Fifty-three patients were included. The terminal ileum was involved in only 11 patients. Eight of these patients had involvement of the cecum too. Two patients had ileal lesions without cecal involvement; however, lesions were noted in the ascending colon. In one patient the whole colon was normal and only the terminal ileum showed nodularity and ulceration. Histological examination of the ileal biopsies obtained from the ileal lesions showed noncaseating granulomas in five, collection of epithelioid cells in four and nonspecific histology in two patients. Mucosal biopsies obtained from the lesion in the terminal ileum, in the patient in whom mucosal abnormality was observed to be confined to the ileum, showed noncaseating granulomas. In two other patients the ileal biopsies alone showed histological evidence of tuberculosis with biopsies from the colonic lesions showing non-specific inflammatory changes only.
CONCLUSION: Retrograde ileoscopy should be performed in all patients undergoing colonoscopy for suspected ileocolonic tuberculosis. In some patients only the terminal ileum may be involved and histological examination may reveal evidence of tuberculosis only from the lesions in the terminal ileum. This approach would lead to additional lesions being picked up and increasing the chances of well-timed diagnosis of tuberculosis.
Keywords: Tuberculosis, Ileoscopy, Colonoscopy
INTRODUCTION
Even now, colonic tuberculosis is common in the developing countries[1-8]. More importantly, in the recent past it has been observed that the disease has been staging resurgence even in the developed world, with more and more cases being reported especially in Hispanics, African Americans, immigrants and refugees and in patients having acquired immunodeficiency virus infections[9-16].
In clinical practice the diagnosis of colonic tuberculosis is made mostly by the colonoscopic appearance of the lesions and the histological findings[1-7]. The colonoscopic appearance of the lesions includes transverse or linear ulcers, nodules, deformed ileocecal valve and cecal mucosa, strictures and polypoid lesions mimicking malignancy[1-7]. More recently, haphazardly arranged fibrous bands forming irregular pockets have also been described[3,4]. A few cases of colonic tuberculosis presenting like chronic ulcerative colitis have also been reported[17-19]. Additionally, a rare presentation of colonic tuberculosis where colonoscopy revealed only aphthous ulceration of the colonic mucosa has been reported recently[20].
Terminal ileoscopy is an integral part of complete colonoscopy. Retrograde terminal ileoscopy has been noted to be useful in patients with inflammatory bowel disease, diarrhea, lymphoma, cytomegalovirus induced ileitis, tuberculosis, portal hypertension and a host of other conditions involving the terminal ileum[21-34]. In a recent study, it has been noted that obtaining blind biopsies from even a normal-appearing terminal ileum is useful in patients suspected to have ileocaecal tuberculosis[35]. Retrograde ileoscopy has also been reported to be useful in patients with hematochezia in whom colonoscopic examination did not detect any lesions. Interestingly, ileal tuberculosis was noted to be the cause of bleeding in one of the patients[36]. However, despite being recommended by several authors[21-36] terminal ileoscopy is not routinely performed on all patients undergoing colonoscopy[37,38]. However; routine retrograde ileoscopy is very useful and easy to perform after imparting proper training[38].
Although, there are several studies dealing with the role of colonoscopy in patients with colonic tuberculosis, the role of retrograde ileoscopy has not been evaluated in this condition and, apart from a few stray reports dealing with ileoscopy in patients with ileocolonic tuberculosis[30,36], there has been no systematic approach to study this facet. In this study we attempt to evaluate whether or not performing retograde ileoscopy in patients with ileocolonic tuberculosis increases the diagnostic yield in patients with ileocolonic tuberculosis.
MATERIALS AND METHODS
A retrospective analysis was performed for patients undergoing colonoscopy for suspected ileocolonic tuberculosis between January 2000 and June 2004, in whom retrograde ileoscopy had been performed. Only patients diagnosed to have tuberculosis on the basis of histological findings of either a caseating granuloma or those having non-caseating granuloma or a collection of epithelioid cells at a minimum of one endoscopic lesion (either in the colon or the terminal ileum) on histology with good response to conventional anti-tuberculous drugs were enrolled in the study. Those having non-specific histology were not enrolled, even though they responded well to anti-tuberculous therapy. After colonoscopy and retrograde ileoscopy, those patients who did not show any lesions were also excluded.
The clinical details of the patients were noted along with the colonscopic and ileoscopic findings. Colonoscopy was performed with an Olympus colonoscope (CF 130 L, Olympus Optical Co., Tokyo). Colonic preparation was done using one liter 10% mannitol solution, given 6-8 h before colonoscopic examination, followed by World Health Organization oral rehydration solution or a polyethylene glycol-electrolyte-based solution (Peglec, Tablets India Ltd, Chennai). The procedure was performed under conscious sedation with intravenous diazepam (5-10 mg) and pentazocine (25-50 mg). During colonoscopy a careful search was made for the presence of ulcers, nodularity, strictures, mass lesions, fibrous bands and any other abnormality. If any abnormality was present then multiple biopsies were obtained from the lesion and the margins for histopathological examination. After reaching the cecum, the ileocaecal opening was located and the terminal ileum intubated. Once in the terminal ileum all attempts were made to go as far as possible in the ileum. Any abnormality in the mucosa of the terminal ileum was carefully recorded and biopsies were obtained from suspicious-looking lesions.
All patients underwent an X-ray of the chest and ultrasound/CT scan of the abdomen. Sputum examination for acid-fast bacilli and ascitic/pleural fluid examinations for acid-fast bacilli and PCR for TB were performed where indicated.
Patients who were diagnosed to have ileocolonic tuberculosis were provided anti-tuberculous treatment (rifampicin, isoniazide, pyrazinamide and ethambutol for two months followed by rifampicin and isoniazid for a further period of ten months). Monthly follow-up examinations were performed in the outpatient department.
RESULTS
A total of 55 patients were selected. Two patients were removed from the final analyses since, although retrograde ileoscopy had been performed and documented, no specific mention about the terminal ileum being normal or abnormal was found. Therefore the final analysis is of 53 patients.
The mean (SD) age of the patients was 39.98 (8.85) years(range 23-60 years). There were 40 male. X-ray evidence of tuberculosis was noted in 12 patients. In two patients, sputum examination showed evidence of acid-fast bacilli. Ascites was observed in two patients and pleural effusion was noted in one patient and the fluid was positive by PCR for TB in all of them. One patient had significant cervical lympadenopathy and histology of the lymph nodes showed caseating Langhans granulomas with acid-fast bacilli. Two patients had been diagnosed to have pulmonary tuberculosis in the recent past but had not taken proper treatment as advised by their physicians.
At colonoscopy, the rectum and the descending colon were not involved in any patient. The transverse colon was noted to be affected in 9 patients, the ascending colon in 20 and the cecum in 34 patients. The terminal ileum was noted to be involved in 11 patients. The overlap is due to the fact that in some patients, more than one site was involved. Of the 11 patients in whom endoscopic lesions were noted in the terminal ileum, eight had involvement of the cecum too. Two patients had ileal tuberculosis without cecal involvement. However, in these two patients, lesions were noted in the ascending colon during colonoscopy. In one patient the whole colon including the cecum was normal and only the terminal ileum showed nodularity and ulceration.
The colonoscopic findings noted were nodules, ulceration, polypoid lesion, strictures, and deformed cecum and ileocaecal valve. The findings in the terminal ileum included ulceration (Figure 1) with or without nodularity (Figure 2). Strictures, fibrous bands and polypoid lesions were not observed in the terminal ileum of any patient. Upon histology of the target lesions, caseating granulomas were seen in four patients, noncaseating granulomas in 22, and a collection of epithelioid cells in 27 patients.
Figure 1.
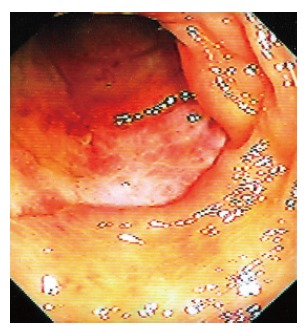
Retrograde ileoscopy showing an ulcer in the terminal ileum.
Figure 2.
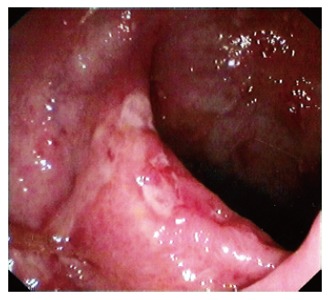
Ulcers and nodularity of the terminal ileal mucosa. The endoscopic lesions were confined only to the terminal ileum and colonoscopy till the cecum did not reveal any abnormality.
Histological examination of the ileal biopsies obtained from the lesions showed noncaseating granulomas in five (Figure 3), collection of epithelioid cells in four and nonspecific histology in two patients. Mucosal biopsies obtained from the lesion in the terminal ileum, in the patient in whom mucosal abnormality was observed to be confined to the ileum, showed noncaseating granulomas (Figure 4). In two other patients the ileal biopsies alone showed histological evidence of tuberculosis (noncaseating grauloma in one and collection of epithelioid cells in another patient). In these patients, although lesions were noted in the colon, the histological examination of the colonic target biopsies showed non-specific inflammatory changes only. Therefore in 3 cases, ileoscopy was useful in making a positive diagnosis of tuberculosis.
Figure 3.
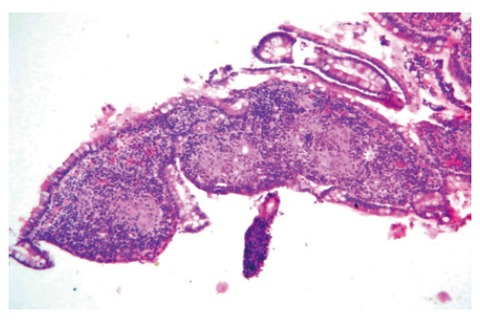
Histological appearance of the mucosal biopsies obtained from the lesion shown in Figure 1. Note the presence of noncaseating granulomas (HE × 40).
Figure 4.
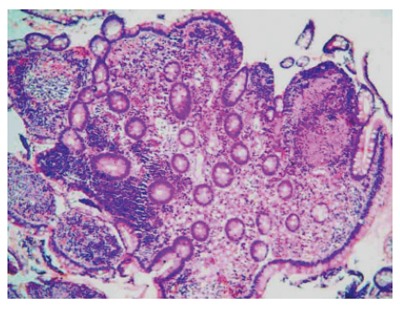
Noncaseating granulomas seen upon histological examination of the mucosal biopsies obtained from the lesion shown in Figure 2 (HE × 80).
Upon follow-up, two patients developed drug-induced hepatitis. Rifampicin, pyrazinamide and isoniazid were stopped and the patients given ethambutol, streptomycin and sparfloxacin for a period of three months. Thereafter, rifampicin and isoniazid were reintroduced. There was no recurrence of hepatitis in either of the patients.
DISCUSSION
The procedure to diagnose colonic tuberculosis is colonoscopy and targeted biopsies of the lesion seen during the procedure. Although ileoscopy is considered as an integral part of colonoscopy, it is not performed in all patients undergoing colonoscopy[37,38]. This is despite the fact that a number of studies have demonstrated the utility of retrograde ileoscopy during colonoscopic examination of the large bowel[21-36]. A recent study speculated that perceived difficulty of ileal intubation, time constraints, and the expectation of a low diagnostic yield were the likely reasons for the resistance on the part of the endoscopists in attempting retrograde ileoscopy[38].
The results of this study show that retrograde ileoscopy is of additional benefit in patients suspected to have ileocolonic tuberculosis. In two patients, had retrograde ileoscopy not been performed, the diagnosis of tuberculosis would have been conjectural and would have to been relied upon a positive response to anti-tuberculous medication. In one patient, the diagnosis would have not been possible as full-length colonoscopy till the cecum did not reveal any abnormality and the lesions were confined to the terminal ileum. Lueng et al[31] had reported two similar cases earlier.
Another interesting aspect of this study was that the terminal ileum was more commonly involved if the cecal area was affected too. Of the 11 cases in which the terminal ileum was affected, eight had cecal involvement too. In two other patients, the cecum was normal but the ascending colon was involved. It is known that the ileocaecal region is the most common site for involvement of gastrointestinal tuberculosis. The predilection for the ileocaecal area is attributed to the relative stasis in this area, the abundance of lymphoid tissue and the higher rate of absorption in this area. However, histologically, three of the patients showed evidence of tuberculosis only in the terminal ileum and, although lesions were noted in the colon in two of these patients, the histology did not show clear-cut evidence of tuberculosis.
Caseating granulomas are considered a hallmark for the diagnosis of tuberculosis. However, as seen in our earlier studies[4,34-36], these were rare and were observed in only four patients and that too from the colonic lesions. None of the patients showed caseating granulomas upon histiological examination of biopsies obtained from the terminal ileal lesions. It is our opinion that this is due to the fact that with the relative availability of endoscopic facilities coupled with a high clinical suspicion of ileocolonic tuberculosis, in our patients, and a low threshold for performing colonoscopy in these patients, colonoscopic examinations are being performed earlier in these patients.
We recruited only patients in whom histology of target biopsies from at least one site showed presence of either caseating granuloma or noncaseating granuloma or collection of epithelioid cells with a good clinical response to antituberculous drugs and patients in whom histological examination of the biopsies showed only non-specific inflammatory changes were excluded. In most other studies, nonspecific inflammatory changes on histology coupled with a good response to antituberculous agents has been taken to be evidence of colonic tuberculosis[1-5,7,39,40]. We deliberately did not include these cases, as that would have led to some speculation about the diagnosis. In such cases a close monitoring of the patients is of utmost importance and the approach may be clinically very relevant if on a close follow-up these patients show a good response to the drugs[1-5,7,39-40]. The poor sensitivity of the colonic biopsies is due the fact that most lesions are located in the submucosa and are not sampled by the biopsy.
The colonoscopic appearance of lesions noted in this study were similar to that reported earlier. Lesions of the terminal ileum have not been described in detail. Although, the colonoscopic lesions described include transverse or linear ulcers, nodules, deformed ileocecal valve and cecal mucosa, strictures, polypoid lesions mimicking malignancy[1-7], haphazardly arranged fibrous bands[3,4] and rarely a chronic ulcerative colitis like endoscopic appearance[17-19]; ulceration with or without nodularity were the only lesions observed in the terminal ileum. Other lesions such as polypoid masses, fibrous bands and strictures were not noted in the terminal ileum of patients in the present study. However, nothing prevents a stricture from forming in the terminal ileum. What was interesting, however, was the fact that of the 11 lesions in the terminal ileum, five showed formation of noncaseous granulomas and collection of epithelioid cells were observed in four patients. In only two patients did the histology of the targeted biopsies show non-specific inflammatory changes. Although, this is a highly selected cohort of patients, the high percentage of patients with a positive histology from lesions in the ileum makes retrograde ileoscopy and histological examination of ileal biopsies very interesting. If terminal ileoscopy is performed in all patients undergoing colonoscopy for suspected ileocolonic tuberculosis, additional lesions would be picked up and the chances of making a diagnosis of tuberculosis would increase considerably.
Footnotes
S- Editor Wang J L- Editor Li M E- Editor Chin GJ
References
- 1.Bhargava DK, Tandon HD, Chawla TC, Shriniwas BN, Kapur BM. Diagnosis of ileocecal and colonic tuberculosis by colonoscopy. Gastrointest Endosc. 1985;31:68–70. doi: 10.1016/s0016-5107(85)71995-5. [DOI] [PubMed] [Google Scholar]
- 2.Shah S, Thomas V, Mathan M, Chacko A, Chandy G, Ramakrishna BS, Rolston DD. Colonoscopic study of 50 patients with colonic tuberculosis. Gut. 1992;33:347–351. doi: 10.1136/gut.33.3.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh V, Kumar P, Kamal J, Prakash V, Vaiphei K, Singh K. Clinicocolonoscopic profile of colonic tuberculosis. Am J Gastroenterol. 1996;91:565–568. [PubMed] [Google Scholar]
- 4.Misra SP, Misra V, Dwivedi M, Gupta SC. Colonic tuberculosis: clinical features, endoscopic appearance and management. J Gastroenterol Hepatol. 1999;14:723–729. doi: 10.1046/j.1440-1746.1999.01940.x. [DOI] [PubMed] [Google Scholar]
- 5.Villanueva Sáenz E, Martínez Hernández Magro P, Fernando Alvarez-Tostado Fernández J, Valdés Ovalle M. Colonic tuberculosis. Dig Dis Sci. 2002;47:2045–2048. doi: 10.1023/a:1019624913037. [DOI] [PubMed] [Google Scholar]
- 6.Naga MI, Okasha HH, Ismail Z, El-Fatatry M, Hassan S, Monir BE. Endoscopic diagnosis of colonic tuberculosis. Gastrointest Endosc. 2001;53:789–793. doi: 10.1067/mge.2001.114965. [DOI] [PubMed] [Google Scholar]
- 7.Uygur-Bayramicli O, Dabak G, Dabak R. A clinical dilemma: abdominal tuberculosis. World J Gastroenterol. 2003;9:1098–1101. doi: 10.3748/wjg.v9.i5.1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Snider DE, Roper WL. The new tuberculosis. N Engl J Med. 1992;326:703–705. doi: 10.1056/NEJM199203053261011. [DOI] [PubMed] [Google Scholar]
- 9.Guth AA, Kim U. The reappearance of abdominal tuberculosis. Surg Gynecol Obstet. 1991;172:432–436. [PubMed] [Google Scholar]
- 10.Bloch AB, Rieder HL, Kelly GD, Cauthen GM, Hayden CH, Snider DE. The epidemiology of tuberculosis in the United States. Implications for diagnosis and treatment. Clin Chest Med. 1989;10:297–313. [PubMed] [Google Scholar]
- 11.Watson JM, Gill ON. HIV infection and tuberculosis. BMJ. 1990;300:63–65. doi: 10.1136/bmj.300.6717.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Soriano V, Tor J, Doménech E, Gabarre E, Muga R, Inaraja L, Casas D, Olazábal J, Clotet B. Abdominal tuberculosis in patients with acquired immunodeficiency syndrome. Med Clin (Barc) 1991;97:121–124. [PubMed] [Google Scholar]
- 13.Corbett EL, Watt CJ, Walker N, Maher D, Williams BG, Raviglione MC, Dye C. The growing burden of tuberculosis: global trends and interactions with the HIV epidemic. Arch Intern Med. 2003;163:1009–1021. doi: 10.1001/archinte.163.9.1009. [DOI] [PubMed] [Google Scholar]
- 14.Dye C, Scheele S, Dolin P, Pathania V, Raviglione MC. Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. JAMA. 1999;282:677–686. doi: 10.1001/jama.282.7.677. [DOI] [PubMed] [Google Scholar]
- 15.Trends in tuberculosis--United States, 1998-2003. MMWR Morb Mortal Wkly Rep. 2004;53:209–214. [PubMed] [Google Scholar]
- 16.Ruddy MC, Davies AP, Yates MD, Yates S, Balasegaram S, Drabu Y, Patel B, Lozewicz S, Sen S, Bahl M, et al. Outbreak of isoniazid resistant tuberculosis in north London. Thorax. 2004;59:279–285. doi: 10.1136/thx.2003.010405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Misra SP, Misra V, Dwivedi M, Singh PA. Colonic tuberculosis mimicking ulcerative colitis. J Assoc Physicians India. 1998;46:309–310. [PubMed] [Google Scholar]
- 18.Misra A, Khanduri A, Jain M, Gupta RK, Choudhuri G. Colonic tuberculosis presenting as diffuse pancolitis. Indian J Gastroenterol. 1996;15:105. [PubMed] [Google Scholar]
- 19.Ahuja SK, Gaiha M, Sachdev S, Maheshwari HB. Tubercular colitis simulating ulcerative colitis. J Assoc Physicians India. 1976;24:617–619. [PubMed] [Google Scholar]
- 20.Tarumi K, Koga H, Iida M, Kobori Y, Matsumoto H, Fujita M, Takeda M, Hoshika K, Mikami Y. Colonic aphthoid erosions as the only manifestation of tuberculosis: case report. Gastrointest Endosc. 2002;55:743–745. doi: 10.1067/mge.2002.122797. [DOI] [PubMed] [Google Scholar]
- 21.Coremans G, Rutgeerts P, Geboes K, Van den Oord J, Ponette E, Vantrappen G. The value of ileoscopy with biopsy in the diagnosis of intestinal Crohn's disease. Gastrointest Endosc. 1984;30:167–172. doi: 10.1016/s0016-5107(84)72358-3. [DOI] [PubMed] [Google Scholar]
- 22.Börsch G, Schmidt G. Endoscopy of the terminal ileum. Diagnostic yield in 400 consecutive examinations. Dis Colon Rectum. 1985;28:499–501. doi: 10.1007/BF02554095. [DOI] [PubMed] [Google Scholar]
- 23.Kundrotas LW, Clement DJ, Kubik CM, Robinson AB, Wolfe PA. A prospective evaluation of successful terminal ileum intubation during routine colonoscopy. Gastrointest Endosc. 1994;40:544–546. doi: 10.1016/s0016-5107(94)70249-7. [DOI] [PubMed] [Google Scholar]
- 24.Zwas FR, Bonheim NA, Berken CA, Gray S. Diagnostic yield of routine ileoscopy. Am J Gastroenterol. 1995;90:1441–1443. [PubMed] [Google Scholar]
- 25.Geboes K, Ectors N, D'Haens G, Rutgeerts P. Is ileoscopy with biopsy worthwhile in patients presenting with symptoms of inflammatory bowel disease? Am J Gastroenterol. 1998;93:201–206. doi: 10.1111/j.1572-0241.1998.00201.x. [DOI] [PubMed] [Google Scholar]
- 26.Halligan S, Saunders B, Williams C, Bartram C. Adult Crohn disease: can ileoscopy replace small bowel radiology? Abdom Imaging. 1998;23:117–121. doi: 10.1007/s002619900301. [DOI] [PubMed] [Google Scholar]
- 27.Tribl B, Turetschek K, Mostbeck G, Schneider B, Stain C, Pötzi R, Gangl A, Vogelsang H. Conflicting results of ileoscopy and small bowel double-contrast barium examination in patients with Crohn's disease. Endoscopy. 1998;30:339–344. doi: 10.1055/s-2007-1001279. [DOI] [PubMed] [Google Scholar]
- 28.Marshall JK, Hewak J, Farrow R, Wright C, Riddell RH, Somers S, Irvine EJ. Terminal ileal imaging with ileoscopy versus small-bowel meal with pneumocolon. J Clin Gastroenterol. 1998;27:217–222. doi: 10.1097/00004836-199810000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Lewis BS. Ileoscopy should be part of standard colonoscopy: a comparison of radiographic and endoscopic evaluation of the ileum. J Clin Gastroenterol. 2000;31:103–104. doi: 10.1097/00004836-200009000-00002. [DOI] [PubMed] [Google Scholar]
- 30.Bhasin DK, Goenka MK, Dhavan S, Dass K, Singh K. Diagnostic value of ileoscopy: a report from India. J Clin Gastroenterol. 2000;31:144–146. doi: 10.1097/00004836-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Leung VK, Tang WL, Cheung CH, Lai MS. Importance of ileoscopy during colonoscopy for the early diagnosis of ileal tuberculosis: report of two cases. Gastrointest Endosc. 2001;53:813–815. doi: 10.1067/mge.2001.114954. [DOI] [PubMed] [Google Scholar]
- 32.Yusoff IF, Ormonde DG, Hoffman NE. Routine colonic mucosal biopsy and ileoscopy increases diagnostic yield in patients undergoing colonoscopy for diarrhea. J Gastroenterol Hepatol. 2002;17:276–280. doi: 10.1046/j.1440-1746.2002.02686.x. [DOI] [PubMed] [Google Scholar]
- 33.Morini S, Lorenzetti R, Stella F, Martini MT, Hassan C, Zullo A. Retrograde ileoscopy in chronic nonbloody diarrhea: a prospective, case-control study. Am J Gastroenterol. 2003;98:1512–1515. doi: 10.1111/j.1572-0241.2003.07523.x. [DOI] [PubMed] [Google Scholar]
- 34.Misra SP, Dwivedi M, Misra V, Gupta M. Ileal varices and portal hypertensive ileopathy in patients with cirrhosis and portal hypertension. Gastrointest Endosc. 2004;60:778–783. doi: 10.1016/s0016-5107(04)02049-8. [DOI] [PubMed] [Google Scholar]
- 35.Misra SP, Dwivedi M, Misra V, Gupta M, Kunwar BK. Endoscopic biopsies from normal-appearing terminal ileum and cecum in patients with suspected colonic tuberculosis. Endoscopy. 2004;36:612–616. doi: 10.1055/s-2004-814518. [DOI] [PubMed] [Google Scholar]
- 36.Misra SP, Dwivedi M, Misra V. Ileoscopy in 39 hematochezia patients with normal colonoscopy. World J Gastroenterol. 2006;12:3101–3104. doi: 10.3748/wjg.v12.i19.3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Joint Advisory Group on Gastrointestinal Endoscopy. Guidelines for the training and assessment of trainees in gastrointestinal endoscopy. 2001. Available from: http://www.BSG.org.uk/sections/endoscopy.htm.
- 38.Cherian S, Singh P. Is routine ileoscopy useful? An observational study of procedure times, diagnostic yield, and learning curve. Am J Gastroenterol. 2004;99:2324–2329. doi: 10.1111/j.1572-0241.2004.40730.x. [DOI] [PubMed] [Google Scholar]
- 39.Misra SP, Misra V, Dwivedi M, Arora JS, Kunwar BK. Tuberculous colonic strictures: impact of dilation on diagnosis. Endoscopy. 2004;36:1099–1103. doi: 10.1055/s-2004-826046. [DOI] [PubMed] [Google Scholar]
- 40.Lee YJ, Yang SK, Byeon JS, Myung SJ, Chang HS, Hong SS, Kim KJ, Lee GH, Jung HY, Hong WS, et al. Analysis of colonoscopic findings in the differential diagnosis between intestinal tuberculosis and Crohn's disease. Endoscopy. 2006;38:592–597. doi: 10.1055/s-2006-924996. [DOI] [PubMed] [Google Scholar]


