Abstract
Celiac disease (CD) is a common autoimmune disorder characterized by an immune response to ingested gluten and has a strong HLA association with HLA-DQ2 and HLA-DQ8 molecules, but human HLA-DQ risk factors do not explain the entire genetic susceptibility to gluten intolerance. CD is caused by the lack of immune tolerance (oral tolerance) to wheat gluten. In this sense, the expression of soluble HLA-G in CD is of special interest because the molecule plays an important role in the induction of immune tolerance. The enhanced expression of soluble HLA-G found in CD may be part of a mechanism to restore the gluten intolerance. In this editorial, we review recent progress in understanding CD in relation to its prevalence, diagnosis and possible mechanisms of pathogenesis.
Keywords: Celiac disease, Oral tolerance, IL-10, TGF-beta, Gluten intolerance
INTRODUCTION
Celiac disease (CD) is a chronic inflammatory disease which develops in genetically predisposed individuals. CD is a T cell-mediated inflammatory disorder with autoimmune features and it has environmental and immunologic components[1,2]. It is characterised by an immune response to ingested wheat gluten and related proteins of rye and barley that leads to inflammation, villous atrophy and crypt hyperplasia in the proximal part of the small intestine[2,3]. The common presentation symptoms and signs of CD include diarrhea, abdominal distention, abdominal pain, weight loss, fatigue, and malnutrition.
The clinical classification of CD is based on the presence or lack of gastrointestinal symptoms: “classical” or “symptomatic” CD refers to presentations with diarrhea and with malabsorption syndrome, whereas “atypical” or “asymptomatic” form has no gastrointestinal manifestations[4]. CD is defined as silent when the typical enteropathy is found in patients who apparently are healthy. Potential CD refers to a risk for developing a typical CD later in life; the patients have Endomysial antibody (EMA) and tissue transglutaminase (tTG) antibodies with HLA DQ2 or DQ8 predisposing genotype[6,7], and normal or minimal abnormal mucosa. Finally, a specific manifestation of CD is refractory sprue defined as symptomatic, severe villous atrophy with increased intraepithelial lymphocytes (IELs) despite maintenance of a strict gluten-free diet[5].
Although there have been major advances in our knowledge of the disease, there are few advances in the therapy. The only accepted treatment for CD is a nutritional therapy with a gluten-free diet for lifelong[8]. Here, we review recent advances in our understanding of CD with respect to its prevalence and diagnosis, and possible mechanisms underlying the gluten intolerance.
PREVALENCE
CD is the most common food-sensitive enteropathy in humans. The prevalence is estimated in the range of 1:100 to 1:300 in North America and Europe[9,10]. Recently, it has become clear that CD is much more prevalent than previously thought. We observed in our pediatric population (south-east of Spain) a 1:75 prevalence, which is in good agreement with the studies by Fasano et al [9] and Ciclitira et al[10] showing a prevalence of 1:133 in the United States and 1:100 in Europe, respectively.
At the present time, the form of clinical presentation of CD is changing. In our experience, CD is a very common disorder, and most affected individuals have the atypical and silent forms of the disease, which are also the prevalent forms of disease presentation in our population. Indeed, we observed a more elevated percentage of patients associated with HLA-DQ8 molecule in CD (around 20%-25%) than have been described previously by other studies, which estimated the percentage of HLA-DQ8 patients to be about 10%[11]. Furthermore, the HLA-DQ8 CD patients are commonly associated with extraintestinal symptoms presentations, and are frequently associated with others autoimmune diseases (unpublished results).
DIAGNOSIS
We believe that the current diagnostic criteria for CD need a revision. CD is often missed during diagnosis because many individuals do not present the disease with the classical gastrointestinal symptoms. In fact, the percentage of undiagnosed population has markedly increased, and significant risks and complications are associated with untreated CD (Table 1).
Table 1.
Clinical manifestations of untreated celiac disease
| Manifestations | Associated diseases | Genetic associated diseases |
| Classic symptoms: | Autoimmune diseases: | Down syndrome |
| Turner syndrome | ||
| Abdominal pain | Type 1 diabetes | William syndrome |
| Anorexia | Thyroiditis | IgA deficiency |
| Diarrhea | Sjogren’s syndrome | |
| Weight loss | IgA nephropathy | |
| Short stature | ||
| Irritability | Neurologic disturbances: | |
| Nonclassic symptoms: | Autism | |
| Depression | ||
| Dermatitis hepertiformis | Epilepsy | |
| Hepatitis | Cerebellar ataxia | |
| Anemia | ||
| Arthritis | Other diseases: | |
| Constipation | ||
| Alopecia | Osteopenia/osteoporosis | |
| Pubertal delay | Infertility | |
| Vomiting | Intestinal adenocarcinoma | |
| Inflammatory bowel disease | Non-Hodgkin lymphoma | |
| Migraine headaches |
As a multi-factorial disorder, CD may present highly diverse clinical manifestations[12]. CD patients typically display extraintestinal (non-classical) symptoms or lack classical gastrointestinal symptoms such as diarrhea, abdominal pain, distention, or weight loss. In our pediatric population, the non-classical symptoms are often the most common presentation in newly diagnosed CD cases. These include autoimmune alopecia, iron deficiency, or elevated levels of liver transaminases, and they often may be the only manifestation of CD in an affected individual (Table 1).
In our experience, small bowel biopsy is critical for diagnosing symptomatic patients with negative serology for CD and with HLA compatible with the disease. Although we consider intestinal biopsy as the gold standard for CD diagnosis, in many occasions the permission for intestinal biopsy is refused. Both serologic tests and genetic study are necessary to select subjects who need intestinal biopsy (Table 2).
Table 2.
Diagnosis in celiac disease
| Diagnostic criteria used in celiac disease | Diagnostic propose for celiac disease | Comments |
| Serological test: | With classical symptoms: | Positive serology supports a diagnosis of CD, but they are not |
| Tissue transglutaminase antibody (tTGA) | Serological test: | essential. Compatible with HLA-DQ2/D8 testing and identify |
| Endomysial antibody (EMA) | Tissue transglutaminase antibody (tTGA) | individuals for further biopsy evaluation. Small bowel biopsy |
| Gliadin antibodies (AGA) | Endomysial antibody (EMA) | is critical in symptomatic patients with negative serology for |
| Total IgA | Gliadin antibodies (AGA) | CD and with HLA compatible with the disease |
| Endoscopy | HLA-DQ2/DQ8 testing | Determination of HLA typing as a first step in diagnosis in CD family |
| Capsule endoscopy (with adequate pathological interpretation) | Adequate number of biopsies and well oriented. Estimate lymphocyte infiltration and partial or total villus atrophy | |
| Without classical symptoms HLA-DQ2/DQ8 testing | Primordial role of HLA-typing if serology is negative and with biopsy refused or equivocal to identify individuals | |
| Serologic test: | Adequate number of biopsies and well oriented. Estimate | |
| Tissue transglutaminase antibody (tTGA) | lymphocyte infiltration and partial or total villous atrophy | |
| Endomysial antibody (EMA) | ||
| Gliadin antibodies (AGA) | ||
| Capsule endoscopy (with adequate pathological interpretation) |
CD is more common in certain risk groups. Family members of known celiac patients represent the most important group of study patients. The determination of HLA typing as a first step is useful as it would exclude approximately one third of first degree relatives in a CD family. We found a high prevalence of CD between relatives, and the highest percentage was observed among daughters. The CD relatives are a population at high risk of developing gluten intolerance and we propose that an extensive study of such group should be undertaken. It is noteworthy that after the first diagnosis of CD, the family will become more self-aware in recognizing early symptoms related to the disease.
PATHOGENESIS
A defect in antigen processing by epithelial cells, together with the intrinsic properties of the gliadins, as well as the HLA-DQ haplotype of the individual are considered the principal factors involved in the pathogenesis of CD[3]. CD is strongly associated with HLA class II genes that map to the DQ locus. It has been shown that CD is associated with the expression of HLA-DQ2 and HLA-DQ8[6,7]. Several studies found that the majority of celiac patients carry DQ2 (DQA1*05/DQB1*02), with the remaining patients displaying an association with DQ8 (DQA1*0301/DQB1*0302). Collectively, these HLA genes confer up to 40% of the genetic risk for CD development.
Gliadin peptide presentation and T-cell activation are critical events in the pathogenesis of CD. Gluten peptides are not fully digested by the action of gastric, intestinal and pancreatic enzymes in CD patients. A 33-mer peptide was isolated and identified as the primary initiator of the inflammatory response to gluten in celiac patients[16]. This peptide reacted with tissue transglutaminase (tTG), the major autoantigen in CD that deamidates certain glutamine residues of gluten to glutamic acid. This in turn produces a negative charge that favours binding and presentation by HLA-DQ2 and DQ8 molecules, which are responsible for T-cell activation and subsequent production of cytokines, leading to tissue damage[17,18]. The inappropriate CD4+ T-cell activation in the lamina propia commonly observed in CD is triggered by specific gluten peptides bound to DQ2 and DQ8 heterodimers on the surface of antigen presentation cells[2,6]. The mucosal intestinal lesion is believed to be mainly induced by the production of IFN-gamma from these gluten specific T cells[1,2]. Moreover, changes in intestinal permeability, secondary to alterations in intercellular tight junctions or in the processing of the food antigen, have also been recently implicated in the loss of tolerance to gluten[19].
Immune (oral) tolerance
The gut immune system is exposed to a wide variety of antigens derived from foods, resident bacteria and invading microorganisms. Oral tolerance is a physiological condition characterized by induction of immune unresponsiveness toward intestinal alimentary and bacterial antigens of the intestinal flora. Multiple cellular and molecular mechanisms are involved in the regulation of this fundamental property of the gut immune system[20].
CD is the most common food-sensitive enteropathy in humans and is caused by the lack of immune tolerance (oral tolerance) to wheat gluten and the prolamin fractions of rye and barley. Many different gluten peptides recognized by intestinal T cells have been identified[21]. The activation of these gluten-reactive T cells represents a key event in the pathogenesis of CD[1,2]. The mucosa of CD patients is characterized by a high proportion of intraepithelial T cells bearing gamma-delta chain of the antigenic T cell receptors (γδ IEL)[22].
Ingested gliadin, the triggering agent of the disease, can cross the epithelial barrier and elicit a harmful T cell-mediated immune response. Dendritic cells are supposed to play a pivotal role in shaping the immune response[23]. Immature dendritic cells are characterised by low levels of MHC class II expression and co-stimulatory molecules and can mediate tolerance presumably by induction of T regulatory cells (Treg cells)[24]. Moreover, IL-10 released by Treg cells can modulate the function of immature dendritic cells and inhibit their differentiation, amplifying the local presence of ‘‘tolerizing dendritic cells’’[25]. IL-10-modulated dendritic cells induce anergy of effector T cells through still undefined mechanisms requiring cell-cell contact.
Therefore, the direction of the immune response toward immunity or tolerance depends on the stage of maturation and the functional properties of the dendritic cells. Gliadin peptides can contribute to overcoming the stage of unresponsiveness of immature dendritic cells by inducing phenotypic and functional dendritic cell maturation, resulting in more efficient processing and presentation of gliadin peptides to specific T lymphocytes[26].
HLA-G: molecule of immune tolerance
HLA-G is a non-classical major histocompatibility complex class I molecule selectively expressed at the maternal-foetal interface on cytotrophoblast cells, protecting the fetus from the maternal immune rejection, and creating a general state of tolerance[27]. HLA-G exhibit tolerogenic properties via interaction with inhibitory receptors presented in natural killer (NK) cells, T cells and antigen-presenting cells (APC)[28].
The presence of soluble HLA-G (sHLA-G) in the cerebrospinal fluid of multiple sclerosis[29] and allograft acceptance after transplantation[30] suggests a tolerogenic function for this molecule against innate and adaptive cellular immune responses. Interestingly, work from our lab and others have suggested that HLA-G antigens may play a protective role in inflammation[31,32]. Further analysis revealed that, sHLA-G molecules inhibit lytic activity of NK cells, induce apoptosis of CD8+ CTLs and affect CD4+ alloproliferation[33]. Thus, the immune modulatory properties of sHLA-G may suggest a potentia role in CD.
We have demonstrated an association of CD with sHLA-G expression (Figure 1A) and we found a correlation between increased levels of sHLA-G expression and CD associated with other autoimmune diseases, being dependent on a genetic link of these diseases through HLA genes[34].
Figure 1.
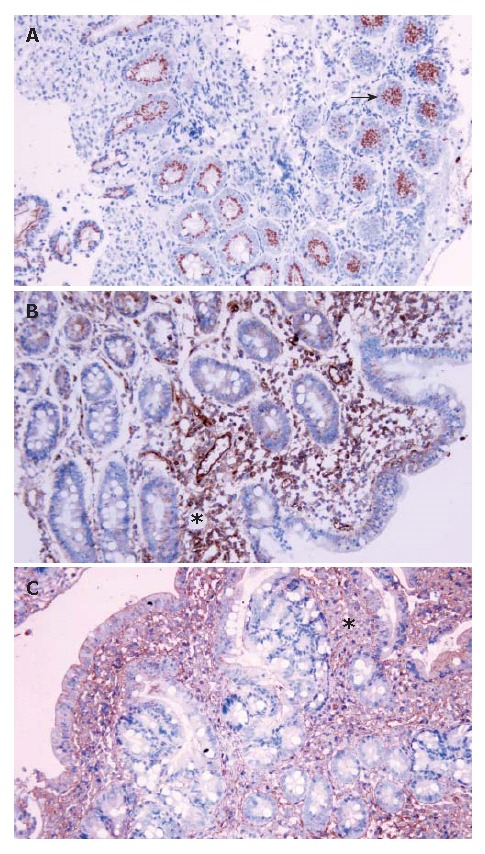
Immunohistochemistry analysis in celiac patients. A: Immunohisto-chemical staining for HLA-G in the Lieberkühn crypts; B: Immunohistochemical staining for IL-10 at the lamina propria level; C: Immunoreaction for TGF-beta in areas of infiltrated inflammatory cells. Arrows and asterisks: cells showing immunoreactivity (x 200).
The expression of soluble HLA-G in CD is of special interest because its molecule plays an important role in the induction of immune tolerance[35]. We propose that the enhanced expression of sHLA-G found in CD could be part of a mechanism to restore the gluten intolerance. HLA-G may act through inhibitory receptor (ILT) interactions that lead to development of tolerogenic dendritic cells with the induction of anergic and immunosuppressive T cells, and an arrest of maturation/activation of dendritic cells. The expression of these ILT receptors on dendritic cells is tightly controlled by inflammatory stimuli, and by cytokines[36].
Thus, a powerful anti-inflammatory response to gliadin might occur during the development of the disease with uncontrolled production of HLA-G and anti-inflammatory cytokines, such as IL-10 and TGF-beta, which counteract the inflammation and/or may cause recruitment of intra-epithelial lymphocytes, maintaining the intestinal lesions presented in CD[34].
Cytokines
The characteristics of an intestinal inflammatory res-ponse depend on the cytokines produced during this response. The production of cytokines from T cells and macrophages is of potential importance for the histological lesions that appear in CD. The CD lesions are associated with a marked infiltration of Th1 cells dominated by the synthesis of the pro-inflammatory cytokines, IFN-gamma and TNF-alpha[37]. IL-15 also has an important role in CD, because it orchestrates intraepithelial lymphocytes changes in the disease. Certain parts of gluten may stimulate the innate part of the immune system, and IL-15 is a central player in this immune response-induced by gluten, inducing the activation of IEL in CD[38]. Engineered IL-15 over-expression by epithelial cells in the intestine leads to a massive expansion of CD8+ intestinal T cells accompanied by a CD-like enteropathy[39]. Furthermore, IL-15 induces the expression of MICA, the epithelial ligand of NKG2D[40].
We found in the celiac patients increased levels of anti-inflammatory cytokines IL-10 and TGF-beta at the lamina propria level in biopsy samples of patients with villous atrophy and elevated lymphocyte infiltration (Figure 1B and C). IL-10 predominantly acts as a potent anti-inflammatory factor and a suppressive agent for Th1 responses[41]. TGF-beta is a major factor for the production of immunoglobulin A (IgA) and acts as a potent mediator of the tissue repair[42]. Interestingly, tTG, described as the major endomysial autoantigen in CD, is necessary for the activation of TGF-beta[43]. The elevated levels of IL-10 and TGF-beta are insufficient for the inhibition of the autoimmune reaction, and would modulate the immune response and induce the activation of B lymphocytes. These cytokines may play important roles in inducing HLA-G. In this regard, the possible role of IL-10 in inducing HLA-G protein expression has been already previously described in CD[34].
FUTURE DIRECTIONS
There are many unanswered questions about CD. What is responsible for the collapse of CD oral tolerance? Restoring immunological tolerance to gluten would represent the ideal way to treat or cure this disease. However, if gluten-specific T cells could be inactivated or deleted, tolerance to gluten should be restored. What is the significance of the vast number of currently undiagnosed people with the disease? What is the significance of the increased number of people with extraintestinal symptoms or without classical symptoms in CD? As we anticipate that the rate of the diagnosis will continue to increase, it will be important to further our understanding of the pathogenesis of CD and improve its diagnosis (Table 3). The diversity of the clinical presentation in CD can complicate the diagnosis and delay the treatment initiation. In our experience, the most important diagnostic test in CD is “the suspicion of the disease”. The screening of CD should start with a serologic test (for IgA and IgG anti-endomysial and anti-tTG antibodies), and HLA typing. If the patient is genetically compatible with the disease (even with negative serology), a confirmatory small biopsy by capsule endoscopy should be followed.
Table 3.
Future directions in celiac disease
| Unanswered questions | Future directions |
| Immunopathogenesis | |
| How is oral tolerance broken? | Restoring immunological tolerance to gluten would represent the ideal cure for CD |
| Gluten-specific T cells | Gluten-specific T cells could be inactivated or deleted, tolerance to gluten should be restored |
| Diagnosis | |
| What is the significance of the vast number of currently undiagnosed people with the disease? | The rate of the diagnosis will continue to increase with better diagnosis. |
| What is the significance of the increase number of people with extraintestinal symptoms or without classical symptoms in CD? | “the suspicion of the disease” |
| Genetics | |
| Identify the genetic risk factors that predispose to CD | Polymorphic genes located in the MHC region and CD |
| Genetic polymorphism of cytokine genes may influence the risk of CD | |
| Associated polymorphism with serological markers | |
| HLA-G polymorphism? |
Recently, many efforts have been made to identify the genetic risk factors that predispose to CD. The lack of immune tolerance in CD could occur due to genetic polymorphisms in any of the non-MHC molecules involved in the induction, regulation or expression of mucosal immune responses, such as IL-10, TGF-beta, IFN-gamma. Most of these polymorphisms affect gene transcription influencing the individual susceptibility to CD[44]. In addition, several associations between different polymorphic genes located in the MHC region and CD have been reported[45]. Furthermore, we found evidence that HLA-G is an interesting candidate as susceptibility gene in CD. These findings should open new perspectives for the identification of genetic susceptibility to CD.
Footnotes
S- Editor Liu Y L- Editor Tan SL E- Editor Ma WH
References
- 1.Sollid LM. Coeliac disease: dissecting a complex inflammatory disorder. Nat Rev Immunol. 2002;2:647–655. doi: 10.1038/nri885. [DOI] [PubMed] [Google Scholar]
- 2.Alaedini A, Green PH. Narrative review: celiac disease: understanding a complex autoimmune disorder. Ann Intern Med. 2005;142:289–298. doi: 10.7326/0003-4819-142-4-200502150-00011. [DOI] [PubMed] [Google Scholar]
- 3.Robins G, Howdle PD. Advances in celiac disease. Curr Opin Gastroenterol. 2005;21:152–161. doi: 10.1097/01.mog.0000153312.05457.8d. [DOI] [PubMed] [Google Scholar]
- 4.Fasano A. Clinical presentation of celiac disease in the pediatric population. Gastroenterology. 2005;128:S68–S73. doi: 10.1053/j.gastro.2005.02.015. [DOI] [PubMed] [Google Scholar]
- 5.Schuppan D, Dennis MD, Kelly CP. Celiac disease: epidemiology, pathogenesis, diagnosis, and nutritional management. Nutr Clin Care. 2005;8:54–69. [PubMed] [Google Scholar]
- 6.Kim CY, Quarsten H, Bergseng E, Khosla C, Sollid LM. Structural basis for HLA-DQ2-mediated presentation of gluten epitopes in celiac disease. Proc Natl Acad Sci USA. 2004;101:4175–4179. doi: 10.1073/pnas.0306885101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Louka AS, Sollid LM. HLA in coeliac disease: unravelling the complex genetics of a complex disorder. Tissue Antigens. 2003;61:105–117. doi: 10.1034/j.1399-0039.2003.00017.x. [DOI] [PubMed] [Google Scholar]
- 8.Fasano A, Catassi C. Current approaches to diagnosis and treatment of celiac disease: an evolving spectrum. Gastroenterology. 2001;120:636–651. doi: 10.1053/gast.2001.22123. [DOI] [PubMed] [Google Scholar]
- 9.Fasano A, Berti I, Gerarduzzi T, Not T, Colletti RB, Drago S, Elitsur Y, Green PH, Guandalini S, Hill ID, et al. Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: a large multicenter study. Arch Intern Med. 2003;163:286–292. doi: 10.1001/archinte.163.3.286. [DOI] [PubMed] [Google Scholar]
- 10.Ciclitira PJ, Johnson MW, Dewar DH, Ellis HJ. The pathogenesis of coeliac disease. Mol Aspects Med. 2005;26:421–458. doi: 10.1016/j.mam.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Tighe MR, Hall MA, Barbado M, Cardi E, Welsh KI, Ciclitira PJ. HLA class II alleles associated with celiac disease susceptibility in a southern European population. Tissue Antigens. 1992;40:90–97. doi: 10.1111/j.1399-0039.1992.tb01965.x. [DOI] [PubMed] [Google Scholar]
- 12.Meize-Grochowski R. Celiac disease: a multisystem autoimmune disorder. Gastroenterol Nurs. 2005;28:394–402; quiz 403-404. doi: 10.1097/00001610-200509000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Dewar D, Pereira SP, Ciclitira PJ. The pathogenesis of coeliac disease. Int J Biochem Cell Biol. 2004;36:17–24. doi: 10.1016/s1357-2725(03)00239-5. [DOI] [PubMed] [Google Scholar]
- 14.Kagnoff MF. Overview and pathogenesis of celiac disease. Gastroenterology. 2005;128:S10–S18. doi: 10.1053/j.gastro.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 15.Lundin KE, Scott H, Fausa O, Thorsby E, Sollid LM. T cells from the small intestinal mucosa of a DR4, DQ7/DR4, DQ8 celiac disease patient preferentially recognize gliadin when presented by DQ8. Hum Immunol. 1994;41:285–291. doi: 10.1016/0198-8859(94)90047-7. [DOI] [PubMed] [Google Scholar]
- 16.Shan L, Molberg Ø, Parrot I, Hausch F, Filiz F, Gray GM, Sollid LM, Khosla C. Structural basis for gluten intolerance in celiac sprue. Science. 2002;297:2275–2279. doi: 10.1126/science.1074129. [DOI] [PubMed] [Google Scholar]
- 17.Molberg O, Mcadam SN, Körner R, Quarsten H, Kristiansen C, Madsen L, Fugger L, Scott H, Norén O, Roepstorff P, et al. Tissue transglutaminase selectively modifies gliadin peptides that are recognized by gut-derived T cells in celiac disease. Nat Med. 1998;4:713–717. doi: 10.1038/nm0698-713. [DOI] [PubMed] [Google Scholar]
- 18.Reif S, Lerner A. Tissue transglutaminase--the key player in celiac disease: a review. Autoimmun Rev. 2004;3:40–45. doi: 10.1016/S1568-9972(03)00065-X. [DOI] [PubMed] [Google Scholar]
- 19.Fasano A. Intestinal zonulin: open sesame! Gut. 2001;49:159–162. doi: 10.1136/gut.49.2.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dubois B, Goubier A, Joubert G, Kaiserlian D. Oral tolerance and regulation of mucosal immunity. Cell Mol Life Sci. 2005;62:1322–1332. doi: 10.1007/s00018-005-5036-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arentz-Hansen H, McAdam SN, Molberg Ø, Fleckenstein B, Lundin KE, Jørgensen TJ, Jung G, Roepstorff P, Sollid LM. Celiac lesion T cells recognize epitopes that cluster in regions of gliadins rich in proline residues. Gastroenterology. 2002;123:803–809. doi: 10.1053/gast.2002.35381. [DOI] [PubMed] [Google Scholar]
- 22.Ebert EC. Intra-epithelial lymphocytes: interferon-gamma production and suppressor/cytotoxic activities. Clin Exp Immunol. 1990;82:81–85. doi: 10.1111/j.1365-2249.1990.tb05407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alpan O, Rudomen G, Matzinger P. The role of dendritic cells, B cells, and M cells in gut-oriented immune responses. J Immunol. 2001;166:4843–4852. doi: 10.4049/jimmunol.166.8.4843. [DOI] [PubMed] [Google Scholar]
- 24.Steinman RM, Turley S, Mellman I, Inaba K. The induction of tolerance by dendritic cells that have captured apoptotic cells. J Exp Med. 2000;191:411–416. doi: 10.1084/jem.191.3.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jonuleit H, Schmitt E, Schuler G, Knop J, Enk AH. Induction of interleukin 10-producing, nonproliferating CD4(+) T cells with regulatory properties by repetitive stimulation with allogeneic immature human dendritic cells. J Exp Med. 2000;192:1213–1222. doi: 10.1084/jem.192.9.1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Palová-Jelínková L, Rozková D, Pecharová B, Bártová J, Sedivá A, Tlaskalová-Hogenová H, Spísek R, Tucková L. Gliadin fragments induce phenotypic and functional maturation of human dendritic cells. J Immunol. 2005;175:7038–7045. doi: 10.4049/jimmunol.175.10.7038. [DOI] [PubMed] [Google Scholar]
- 27.McMaster MT, Librach CL, Zhou Y, Lim KH, Janatpour MJ, DeMars R, Kovats S, Damsky C, Fisher SJ. Human placental HLA-G expression is restricted to differentiated cytotrophoblasts. J Immunol. 1995;154:3771–3778. [PubMed] [Google Scholar]
- 28.Le Rond S, Gonzalez A, Gonzalez AS, Carosella ED, Rouas-Freiss N. Indoleamine 2,3 dioxygenase and human leucocyte antigen-G inhibit the T-cell alloproliferative response through two independent pathways. Immunology. 2005;116:297–307. doi: 10.1111/j.1365-2567.2005.02224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fainardi E, Rizzo R, Melchiorri L, Vaghi L, Castellazzi M, Marzola A, Govoni V, Paolino E, Tola MR, Granieri E, et al. Presence of detectable levels of soluble HLA-G molecules in CSF of relapsing-remitting multiple sclerosis: relationship with CSF soluble HLA-I and IL-10 concentrations and MRI findings. J Neuroimmunol. 2003;142:149–158. doi: 10.1016/s0165-5728(03)00266-2. [DOI] [PubMed] [Google Scholar]
- 30.Lila N, Rouas-Freiss N, Dausset J, Carpentier A, Carosella ED. Soluble HLA-G protein secreted by allo-specific CD4+ T cells suppresses the allo-proliferative response: a CD4+ T cell regulatory mechanism. Proc Natl Acad Sci USA. 2001;98:12150–12155. doi: 10.1073/pnas.201407398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carosella ED, Moreau P, Aractingi S, Rouas-Freiss N. HLA-G: a shield against inflammatory aggression. Trends Immunol. 2001;22:553–555. doi: 10.1016/s1471-4906(01)02007-5. [DOI] [PubMed] [Google Scholar]
- 32.Torres MI, Le Discorde M, Lorite P, Ríos A, Gassull MA, Gil A, Maldonado J, Dausset J, Carosella ED. Expression of HLA-G in inflammatory bowel disease provides a potential way to distinguish between ulcerative colitis and Crohn's disease. Int Immunol. 2004;16:579–583. doi: 10.1093/intimm/dxh061. [DOI] [PubMed] [Google Scholar]
- 33.Bainbridge DR, Ellis SA, Sargent IL. HLA-G suppresses proliferation of CD4(+) T-lymphocytes. J Reprod Immunol. 2000;48:17–26. doi: 10.1016/s0165-0378(00)00070-x. [DOI] [PubMed] [Google Scholar]
- 34.Torres MI, López-Casado MA, Luque J, Peña J, Ríos A. New advances in coeliac disease: serum and intestinal expression of HLA-G. Int Immunol. 2006;18:713–718. doi: 10.1093/intimm/dxl008. [DOI] [PubMed] [Google Scholar]
- 35.Rouas-Freiss N, Paul P, Dausset J, Carosella ED. HLA-G promotes immune tolerance. J Biol Regul Homeost Agents. 2000;14:93–98. [PubMed] [Google Scholar]
- 36.Ristich V, Liang S, Zhang W, Wu J, Horuzsko A. Tolerization of dendritic cells by HLA-G. Eur J Immunol. 2005;35:1133–1142. doi: 10.1002/eji.200425741. [DOI] [PubMed] [Google Scholar]
- 37.Nilsen EM, Lundin KE, Krajci P, Scott H, Sollid LM, Brandtzaeg P. Gluten specific, HLA-DQ restricted T cells from coeliac mucosa produce cytokines with Th1 or Th0 profile dominated by interferon gamma. Gut. 1995;37:766–776. doi: 10.1136/gut.37.6.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maiuri L, Ciacci C, Auricchio S, Brown V, Quaratino S, Londei M. Interleukin 15 mediates epithelial changes in celiac disease. Gastroenterology. 2000;119:996–1006. doi: 10.1053/gast.2000.18149. [DOI] [PubMed] [Google Scholar]
- 39.Meresse B, Chen Z, Ciszewski C, Tretiakova M, Bhagat G, Krausz TN, Raulet DH, Lanier LL, Groh V, Spies T, et al. Coordinated induction by IL15 of a TCR-independent NKG2D signaling pathway converts CTL into lymphokine-activated killer cells in celiac disease. Immunity. 2004;21:357–366. doi: 10.1016/j.immuni.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 40.Hüe S, Mention JJ, Monteiro RC, Zhang S, Cellier C, Schmitz J, Verkarre V, Fodil N, Bahram S, Cerf-Bensussan N, et al. A direct role for NKG2D/MICA interaction in villous atrophy during celiac disease. Immunity. 2004;21:367–377. doi: 10.1016/j.immuni.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 41.Li L, Elliott JF, Mosmann TR. IL-10 inhibits cytokine production, vascular leakage, and swelling during T helper 1 cell-induced delayed-type hypersensitivity. J Immunol. 1994;153:3967–3978. [PubMed] [Google Scholar]
- 42.Cataldo F, Lio D, Marino V, Scola L, Crivello A, Corazza GR. Plasma cytokine profiles in patients with celiac disease and selective IgA deficiency. Pediatr Allergy Immunol. 2003;14:320–324. doi: 10.1034/j.1399-3038.2003.00053.x. [DOI] [PubMed] [Google Scholar]
- 43.Hansson T, Ulfgren AK, Lindroos E, DannAEus A, Dahlbom I, Klareskog L. Transforming growth factor-beta (TGF-beta) and tissue transglutaminase expression in the small intestine in children with coeliac disease. Scand J Immunol. 2002;56:530–537. doi: 10.1046/j.1365-3083.2002.01157.x. [DOI] [PubMed] [Google Scholar]
- 44.Lio D, Scola L, Forte GI, Accomando S, Giacalone A, Crivello A, Cataldo F. TNFalpha, IFNgamma and IL-10 gene polymorphisms in a sample of Sicilian patients with coeliac disease. Dig Liver Dis. 2005;37:756–760. doi: 10.1016/j.dld.2005.04.027. [DOI] [PubMed] [Google Scholar]
- 45.Lie BA, Sollid LM, Ascher H, Ek J, Akselsen HE, Rønningen KS, Thorsby E, Undlien DE. A gene telomeric of the HLA class I region is involved in predisposition to both type 1 diabetes and coeliac disease. Tissue Antigens. 1999;54:162–168. doi: 10.1034/j.1399-0039.1999.540207.x. [DOI] [PubMed] [Google Scholar]


