Abstract
Background
Anxiety disorders and major depressive disorder (MDD) often co-occur and share a broad range of risk factors. The goal of this study was to examine whether the co-occurrence of anxiety disorders and MDD could be explained by an underlying latent factor and whether the risk factors exert their effect exclusively through this factor, directly on each disorder, or through a combination of effects at both levels.
Methods
Data were drawn from a large, nationally representative sample. Confirmatory factor analysis was used to identify the latent structure of anxiety disorders. A multiple indicators multiple causes (MIMIC) approach was used to assess the common and specific effects of risk factors for anxiety disorders.
Results
A one-factor model provided a good fit to the co-occurrence of anxiety disorders. Low self-esteem, family history of depression, female sex, childhood sexual abuse, White race, years of education, number of traumatic experiences, and disturbed family environment increased the risk of anxiety disorders and MDD through their effect on the latent factor. There were also several direct effects of the covariates on the disorders, indicating that the effect of the covariates differed across disorders.
Conclusions
Risk for anxiety disorders and MDD appears to be mediated partially by a latent variable underlying anxiety disorders and MDD, and partially by disorder-specific effects. These findings may contribute to account for the high rates of comorbidity among disorders, identify commonalities in the etiologies of these disorders, and provide clues for the development of unified preventive interventions.
Keywords: risk factors, anxiety disorders, common effects, specific effects, conceptual model
Anxiety disorders and major depressive disorder (MDD) are among the most common mental disorders in the United States,[1] with high individual and societal burden derived from their considerable associated work and social impairment.[2,3] Decreasing the burden of anxiety disorders and MDD is an important public health priority. Anxiety disorders often co-occur with each other and with MDD[4,5] suggesting the existence of a latent structure that may parsimoniously explain these patterns of comorbidity[6–9]. Several studies have examined the genetic liability of anxiety disorders and MDD, and consistently concluded that most of this genetic liability is exerted at the level of the latent variable,[8, 10–13] rather than at the disorder-specific level. Because anxiety disorders and MDD share a broad range of other risk factors,[14–24] an essential step in the development of more effective treatment and prevention interventions is to determine whether those factors exert their effect through the common latent variable, directly on each disorder, or through a combination of effects at both levels.[14, 16, 25]
We sought tsreo address this gap in knowledge by drawing on data from a large, nationally representative survey to compare the common and the specific contribution of a set of observable risk factors to risk of anxiety disorders and MDD. We followed a conceptual model of risk factors, which was initially developed by Kendler and colleagues to examine the prevalence of MDD,[26, 27] but seems to be applicable to other internalizing disorders.[28] Because anxiety disorders often co-occur with each other and with MDD and seem to have a partially shared liability,[8, 13, 14] prior to our analyses, we hypothesized that the comorbidity structure of anxiety disorders and MDD would be well described by a single latent variable and that the risk factors postulated in Kendler’s model would exert part of their effect through this latent variable. However, because the prevalence and course of the different anxiety disorder and MDD does not fully overlap[29–31] and they also have nonshared variance, we also hypothesized that the risk factors would also partially exert their effect directly on the individual disorders.
METHODS
SAMPLE
The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) sample is a nationally representative sample of the adult population of the United States. The NESARC target population was the civilian noninstitutionalized population consisting of 18 years and older residing in households and group living quarters, including residents of the continental United States, Columbia, Alaska, and Hawaii. The 2004–2005 Wave 2 NESARC is the second wave longitudinal follow-up of the Wave 1 NESARC, conducted in 2001–2002. The first wave included face-to-face interviews with 43,093 respondents, yielding an overall response rate of 81.0%.[32,33] The Wave 2 interview was conducted approximately 3 years later. Excluding individuals who were ineligible (e.g., deceased), the response rate in Wave 2 was 86.7% (n = 34,653).[32] Wave 2 NESARC data were adjusted for nonresponse based on sociodemographic characteristics and presence of any lifetime Wave 1 NESARC psychiatric disorder. The adjusted data are representative of the civilian population of the United States based on the 2000 Decennial Census.[34] The research protocol, including informed consent procedures, received full human subjects review and approval from the U.S. Census Bureau and the U.S. Office of Management and Budget. Because several of the risk factors included in our conceptual model were only measured in Wave 2, the sample for this study was composed of all individuals who participated in both waves (n = 34,653).
MEASURES
DSM-IV Anxiety Disorders and MDD
All psychiatric diagnoses were made according to DSM-IV-TR criteria[35] using the Alcohol Use Disorder and Associated Disabilities Interview Schedule—DSM-IV Version (AUDADIS-IV), Wave 2 version.[36,37] The lifetime DSM-IV anxiety disorders included panic disorder, social anxiety disorder (SAD), specific phobia, PTSD and generalized anxiety disorder (GAD). Obsessive-compulsive disorder was not assessed in the NE-SARC, and thus was not included in this study. By contrast, based on its high comorbidity with anxiety disorders and to be consistent with and build on Kendler’s original model, we included MDD in our study. AUDADIS-IV has shown fair to good test–retest reliability in the general population for anxiety disorders and MDD.[33,38]
Conceptual Model
In accord with prior genetic and epidemiologic research, we conceptualized the individual anxiety disorders as indicators of an underlying latent variable and sought to examine whether the risk factors exerted their effect through this latent variable or through direct effects on the disorders. Also consistent with previous research,[26–28] we selected our risk factors based on a conceptual model for risk factors, which addresses the etiologic complexity of internalizing disorders.[14–24] The risk factors included were family history of depression,[33,38] low parental warmth (assessed with the neglect items of the Child Trauma Questionnaire[39]), parental loss before age 18, disturbed family environment (operationalized, as in previous studies, as parental absence or separation from a biological parent before age 18),[40,41] childhood sex abuse (also measured with items from the Child Trauma Questionnaire), history of conduct disorder (assessed with the AUDADIS),[15] low self-esteem (a binary variable considered present if probands believed they were not as good, smart, or attractive as most other people), number of traumatic experiences prior to age 21, history of substance use disorder (SUD) prior to age 21 (assessed with the AUDADIS, using methods previously reported by our group),[42,43] and years of education (measured by self-report). The model also controlled for race/ethnicity and sex.
To minimize the risk that the results were due to reverse causality that could arise if the onset of the disorders preceded the occurrence of the risk factors, we repeated our analyses restricting our sample to individuals whose onset of anxiety disorders was after age 21, to ensure that all risk factors were present before the onset of any anxiety disorder. Because the results of both analyses are very similar, we present the results of the full sample and indicate differences with the results of the restricted sample. Full results of the restricted sample are available upon request.
STATISTICAL ANALYSIS
To assess the association between all risk factors and the five anxiety disorders and MDD, separate logistic regressions were run for each disorder including all risk factors simultaneously, and odds ratios (ORs) and 95% confidence intervals are presented. Given previous results indicating the five anxiety disorders and MDD load on a single factor, we then performed a confirmatory factor analysis (CFA) to assess the fit of a one-factor model. Goodness-of-fit measures including the comparative fit index (CFI), Tucker–Lewis index (TLI), and root mean squared error of approximation (RMSEA) were used to assess fit. Hu and Bentler recommended CFI and TLI values above .95, and RMSEA values below .06, as representing good model fit.[44] We also examined the eigenvalues of the tetrachoric correlation matrix to quantify what percentage of the variability in the anxiety disorders was explained by a single common factor.
We used a multiple indicators multiple causes (MIMIC) approach[45] to assess the common and specific effects of the different risk factors. The MIMIC model is a special case of structural equation modeling (SEM) that includes three sets of relationships: (1) the measurement model, which describes the relationships between the indicators (in this case, the five anxiety disorders and MDD) and the latent factors; (2) the structural model, which describes the relationships between the latent factors and the covariates (in this case, the risk factors); and (3) the relationships between the indicators and the covariates (i.e., risk factors), called the direct effects, because they indicate effects of the covariates on the indicators that are not mediated through the factors (i.e., are still present after adjusting for the effect of the covariates on the latent factors).[46] In this approach, the structural model represents the effect of the covariates (i.e., risk factors) on the latent factor (i.e., the effect of the risk factors on the shared latent liability), whereas the direct effects represent the disorder-specific effects of the risk factors. For example, if the coefficient of a predictor (e.g., family history of MDD) on the latent factor is positive, but the coefficient of the direct effect on a disorder is negative (e.g., specific phobia), the interpretation would be that predictor increases the overall risk of disorders represented by the latent factor, but this increase in risk is smaller for the specific disorder with the negative direct effect (in this case, specific phobia) than for the other disorders in the factor. By contrast, if the coefficient of the direct effect is also positive (e.g., in the case of MDD), this would mean that family history of MDD increases the risk of MDD even more than for the other disorders in the factor.
Modification indices were used to identify whether direct (i.e., specific) effects from risk factors to specific disorders were warranted using a conservative cutoff for determining statistical significance following previously established procedures.[47] Specifically, we used a modification index cutoff of 10 corresponding to a chi-square test with 1 degree of freedom and a critical value of .001 to identify predictors with significant direct effects.
All analyses were conducted in Mplus Version 6.1,[46] which takes into account the NESARC sampling weights and design effects in all analyses, including parameter as well as standard error estimation and model fit calculations. The default estimator for the analysis was the variance-adjusted weighted least squares (WLSMV), a robust estimator that does not assume normally distributed variables and provides the best option for modeling categorical or ordered data.
RESULTS
BIVARIATE ASSOCIATIONS BETWEEN RISK FACTORS AND ANXIETY DISORDERS
In the bivariate analyses, female gender, family history of MDD, disturbed family environment, childhood sexual abuse, low self-esteem, and lower educational attainment all increased the risk of all anxiety disorders and MDD. White race increased the risk of all disorders except PTSD, conduct disorder increased the risk of SAD and specific phobia, and the number of traumas before age 21 increased the risk of panic disorder, PTSD, and GAD. Early parental loss increased the risk of PTSD, but decreased the risk of panic disorder, whereas SUD before age 21 decreased the risk of SAD, specific phobia, and PTSD (Table 1).
TABLE 1.
Lifetime anxiety disorders by risk factors. NESARC Wave 2 (n = 34,653)
| Panic | Social anxiety | Specific phobia | PTSD | GAD | MDD | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| White race | 1.4 | (1.2−1.5) | 1.4 | (1.2−1.5) | 1.1 | (1.0−1.2) | 0.9 | (0.8−1.1) | 1.4 | (1.2−1.5) | 1.4 | (1.3−1.5) |
| Family history MDD | 3.1 | (2.8−3.4) | 3.2 | (2.9−3.5) | 2.2 | (2.0−2.4) | 2.3 | (2.0−2.5) | 3.5 | (3.1−3.9) | 3.3 | (3.0−3.5) |
| Female | 2.1 | (1.9−2.3) | 1.4 | (1.3−1.5) | 2.1 | (2.0−2.3) | 2.2 | (2.0−2.4) | 2.1 | (1.9−2.4) | 2.1 | (2.0−2.3) |
| Disturbed family environment | 1.1 | (1.1−1.1) | 1.1 | (1.1−1.1) | 1.0 | (1.0−1.0) | 1.1 | (1.1−1.1) | 1.1 | (1.1−1.1) | 1.1 | (1.1−1.1) |
| Early parental loss | 0.9 | (0.7−1.0) | 1.0 | (0.9−1.2) | 1.1 | (1.0−1.2) | 1.2 | (1.0−1.4) | 1.1 | (0.9−1.3) | 1.0 | (0.9−1.1) |
| Childhood sexual abuse | 3.4 | (3.0−3.8) | 2.9 | (2.6−3.3) | 2.5 | (2.2−2.7) | 3.9 | (3.5−4.4) | 3.4 | (3.0−3.9) | 2.6 | (2.3−2.8) |
| Conduct disorder | 1.3 | (0.9−2.0) | 1.6 | (1.1−2.4) | 1.5 | (1.1−2.0) | 1.3 | (0.9−2.1) | 1.3 | (0.8−2.0) | 1.5 | (1.1−2.1) |
| SUD before 21 | 1.1 | (1.0−1.3) | 0.5 | (0.4−0.6) | 0.6 | (0.5−0.6) | 0.7 | (0.6−0.8) | 1.0 | (0.8−1.1) | 1.2 | (1.1−1.3) |
| Number of traumas before 21 | 1.2 | (1.2−1.2) | 1.0 | (1.0−1.1) | 1.0 | (1.0−1.0) | 1.3 | (1.3−1.3) | 1.2 | (1.2−1.2) | 1.1 | (1.1−1.2) |
| Years of education before 21 | 0.9 | (0.9−0.9) | 0.8 | (0.8−0.8) | 0.8 | (0.8−0.8) | 0.9 | (0.9−0.9) | 0.9 | (0.9−0.9) | 0.9 | (0.9−1.0) |
| Low self-esteem | 3.6 | (3.2−4.1) | 6.3 | (5.6−7.0) | 2.9 | (2.6−3.2) | 2.7 | (2.4−3.1) | 4.2 | (3.7−4.7) | 2.4 | (2.2−2.6) |
PTSD, posttraumatic stress disorder; GAD, generalized anxiety disorder; MDD, major depressive disorder. Significance at P < .05. Significant odds ratios (ORs) are bolded.
FACTOR ANALYSIS
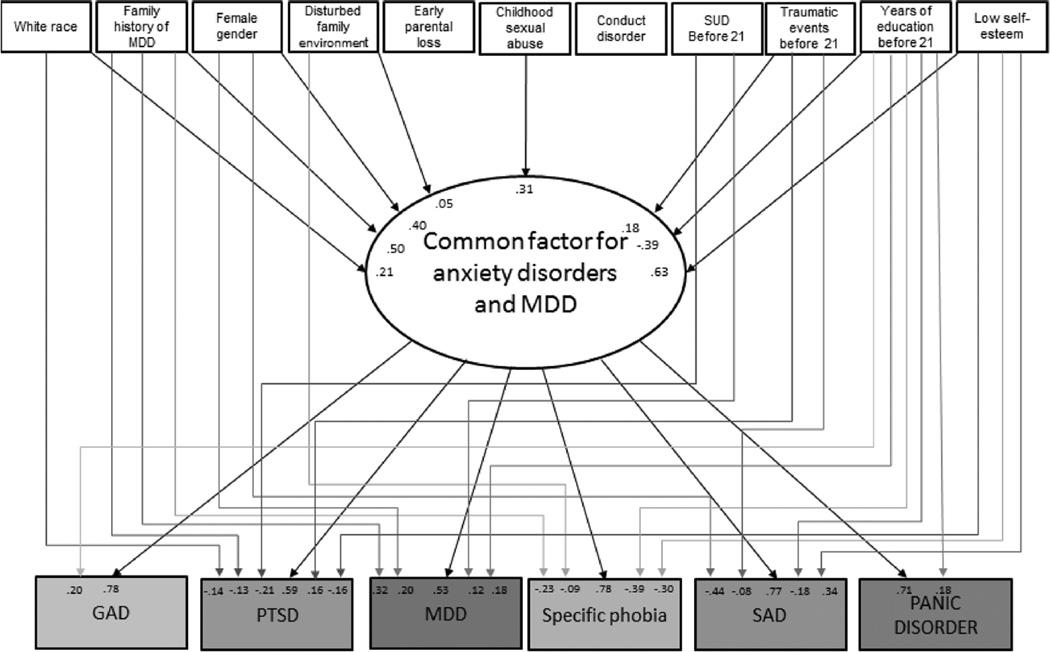
Fit indices for the CFA model with one factor were χ2 = 130.11, df = 9, P < .001; CFI = .99; RMSEA = .02; standardized root mean square residual (SRMR) = .03, indicating an excellent fit. All loadings were at least 0.60, further indicating the adequacy of a single-factor solution. Eigenvalues (3.1, 0.8, 0.6, 0.6, 0.5, 0.4) indicated the presence of one common factor that explained 3.1/6 = 52% of the shared variance in the anxiety disorders and MDD. GAD had the largest loading (0.78), followed by panic disorder (0.70), SAD (0.69), specific phobia (0.63), PTSD (0.57), and MDD (0.51; Fig. 1).
Figure 1.
Model including significant effects of the risk factors on the common factor and direct effects on the disorders.
COMMON AND SPECIFIC EFFECTS OF INDICATORS ON ANXIETY DISORDERS
Overall, the risk factors explained 46% of the variance in the common factor for anxiety disorders and MDD. After adjusting for other covariates, risk factors that had a statistically significant independent effect on the latent variable included low self-esteem, family history of MDD, female sex, childhood sexual abuse, White race, years of education, number of traumatic experiences by age 21, and disturbed family environment (Fig. 1).
Consistent with the varying magnitudes of the ORs of the risk factors with different anxiety disorders, there were several significant direct effects, indicating that the effect of the risk factors was not completely mediated through the latent variable (Table 2 and Fig. 1). The total effects of the covariates on each disorder, which are calculated by combining the indirect (i.e., mediated through the factor) and direct (i.e., without mediation through the factor) effects, are presented in Table 2. For example, the total effect of female gender on SAD (−0.14) was the result of adding the indirect effect (0.31) to the direct effect (–0.44), whereas the effect of low self-esteem on SAD was 0.82, resulted from combining the indirect (0.48) and direct (0.34) effects. In most cases, after adjusting for the effect of the other covariates in the model, the total effects were positive, indicating that the presence of the risk factor increased the likelihood of having the disorder.
TABLE 2.
Direct, indirect and total effects of risk factors on the anxiety disorders
| Panic disorder | SAD | Specific phobia | PTSD | GAD | MDD | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Indirect | Direct | Total | Indirect | Direct | Total | Indirect | Direct | Total | Indirect | Direct | Total | Indirect | Direct | Total | Indirect | Direct | Total | |
| White race | 0.15 | 0.15 | 0.16 | 0.16 | 0.16 | 0.16 | 0.12 | −0.14 | −0.02 | 0.16 | 0.16 | 0.11 | 0.11 | |||||
| Family history MDD |
0.35 | 0.35 | 0.39 | 0.39 | 0.39 | −0.23 | 0.16 | 0.30 | −0.13 | 0.16 | 0.39 | 0.39 | 0.27 | 0.32 | 0.59 | |||
| Female | 0.28 | 0.28 | 0.31 | −0.44 | −0.14 | 0.31 | 0.31 | 0.24 | 0.24 | 0.31 | 0.31 | 0.21 | 0.20 | 0.42 | ||||
| Disturbed family environment |
0.04 | 0.04 | 0.04 | 0.04 | 0.04 | −0.09 | −0.05 | 0.03 | 0.03 | 0.04 | 0.04 | 0.03 | 0.03 | |||||
| Early parental loss | ||||||||||||||||||
| Childhood sexual abuse |
0.22 | 0.22 | 0.24 | 0.24 | 0.24 | 0.24 | 0.18 | 0.18 | 0.24 | 0.24 | 0.17 | 0.17 | ||||||
| Conduct disordera | ||||||||||||||||||
| SUD before 21 | −0.21 | −0.21 | 0.12 | 0.12 | ||||||||||||||
| Number of traumas before 21 |
0.13 | 0.13 | 0.14 | −0.08 | 0.06 | 0.14 | 0.14 | 0.11 | 0.16 | 0.27 | 0.14 | 0.14 | 0.10 | 0.10 | ||||
| Years of education before 21 |
−0.28 | 0.18 | −0.10 | −0.30 | −0.18 | −0.48 | −0.31 | −0.39 | −0.69 | −0.23 | −0.23 | −0.30 | 0.20 | −0.11 | −0.21 | 0.18 | −0.03 | |
| Low self-esteem | 0.44 | 0.44 | 0.48 | 0.34 | 0.82 | 0.49 | −0.30 | 0.19 | 0.37 | −0.16 | 0.21 | 0.49 | 0.49 | 0.33 | 0.33 | |||
SAD, social anxiety disorder; PTSD, posttraumatic stress disorder; GAD, generalized anxiety disorder. Only significant values (P < .05) are shown. Indirect effects represent the effect of the predictor on the disorder occurring through the factor. It is obtained by multiplying the loading of the disorder on the factor by the effect of the covariate on the factor. Direct effects represent the effect of the predictor on the disorder above and beyond the effect of the covariate on the factor. Total effects are the sum of the direct and the indirect effects.
Conduct disorder did not have any significant direct or indirect effect on any anxiety disorder. For that reason, all cells are left empty.
ADDITIONAL ANALYSES
The CFA of the subsample with onset of the first anxiety disorder after age 21 also indicated that a one-factor model had excellent fit χ2 = 119.22, df = 9, P < .001; CFI=.98; RMSEA=.02;SRMR=.05 with all loadings over 0.53.
After adjusting for other covariates, all of the risk factors that had a significant effect on the latent factor in the whole sample remained significant in the subsample with onset of the first anxiety disorder after age 21. However, modification indices for this model indicated that only 8 of the 19 direct effects that were significant in the whole sample remained significant in this subsample: after adjusting for the effects of the covariates on the common factor, female gender decreased the probability of SAD but increased the probability of specific phobia and MDD, White race decreased the probability of PTSD, family history of MDD decreased the probability of SAD and specific phobia but increased the probability of MDD, and low self-esteem increased the probability of SAD (data available upon request).
DISCUSSION
In a large, nationally representative sample, we examined whether (1) the comorbidity structure of anxiety disorders and MDD was well explained by a single latent variable; (2) a comprehensive model initially developed to explain the etiology of MDD could also contribute to explain the risk of anxiety disorders; and (3) the risk factors of that model exerted their effect through a common latent variable or through disorder-specific effects. We found that a single factor described well the comorbidity structure of anxiety disorders and MDD, and that both common and disorder-specific effects explained the relationship between risk factors and anxiety disorders and MDD.
In accord with previous research,[8, 10–13] a single factor described the latent structure of five anxiety disorders and MDD well,[48] supporting the existence of a latent shared risk for these disorders. Previous studies have shown that part of this shared risk is due to shared genetic and environmental liability.[8, 13, 14] Our study extends these prior findings by identifying some of the risk factors that may underlie those shared liabilities. The risk factors examined in this study were based on a conceptual model for risk of MDD, and had previously shown promising results in also predicting the risk of GAD.[28] Our study suggests that the model may have broader applicability than previously thought and may help understand the etiology of a wider range of internalizing disorders and their high rates of co-occurrence. Furthermore, the finding that the disorders differed in their loadings on the latent factor indicates that the disorders have shared but also specific risk factors. In particular, MDD had the lowest loading, suggesting that MDD may stand a bit apart from the anxiety disorders, as previously suggested.
In accord with previous studies,[15, 28, 49] when examined separately in the bivariate analyses, most risk factors increased the odds of all the anxiety disorders and MDD, suggesting that they might be common risk factors for these disorders. Consistent with this view, the results of the MIMIC model indicated that most of the effects of the risk factors were exerted through the latent variable representing the shared liability for all the disorders. In fact, in some cases, such as childhood sexual abuse, the effect was exclusively through the latent variable, in line with prior findings on the effect of child maltreatment on the structure of psychiatric disorders.[50] For example, through its effect on the latent factor, a history of childhood sexual abuse increased by 0.24 standard deviations the risk of having SAD, GAD, or specific phobia, by 0.22 standard deviations the risk of having panic disorder, 0.18 standard deviations the risk of PSTD, and 0.17 standard deviations the risk of MDD. There is a need to better understand the psychological and biological mechanisms underlying the generalized effects of these risk factors.[51–54]
At the same time, as could be expected from the different magnitudes of the association between the risk factors and the different disorders observed in the bivariate analyses, not all the effects of the risk factors occurred through the latent variable. Nineteen of the possible 66 disorder-specific effects were significant, and for each disorder, there was at least one significant direct effect. Our results indicate that, in addition to the shared etiology that pulls them together, all anxiety disorders and MDD have specific effects of risk factors that contribute to their individuality. For example, family history of MDD had a substantial specific effect on MDD in addition to its effect on the latent variable, indicating that this risk factor may contribute to the risk of MDD beyond the risk it confers to anxiety disorders. Similarly, we found that low self-esteem, which has been previously documented among individuals with SAD[55] but also associated with a broad range of mental disorders,[56] has a stronger association with SAD than with other anxiety disorders or MDD. The anxiety about one’s performance and fear of negative evaluation by others may lead individuals to internalize some of those perceptions leading to low self-esteem. Alternatively, low self-esteem might make individuals more reliant on the opinions of others, which may lead to anxiety about their evaluation.[57]
Traumatic experiences had a large specific effect on PTSD above and beyond their effect on the latent factor, whereas being White constituted a specific protective factor (i.e., after adjusting for the effect of race on the latent factor), probably as a result of lower exposure to trauma of White individuals.[58] A surprising finding was that history of SUD before age 21 decreased the risk of PTSD. It is possible that substance use may mask or decrease the intensity of some anxiety symptoms. Alternatively, early-onset SUD may indicate a greater propensity for externalizing disorders than for some internalizing disorders. Despite these isolated findings, overall, the specific effects that were significant in our analyses are consistent with specific risk factors identified in previous studies,[56–60] and are informative about how risk factors may shape individual disorders by involving mechanisms that may be less salient for other disorders.
Our findings have etiological, treatment, and preventive implications. From the etiological point of view, our findings suggest that risk factors may exert their effects, at least in part, through broad dimensions of psychopathology, consistent with the views of the Research Domain Criteria (RDoC) project,[61, 62] and that those effects may differ across disorders. Future research should seek to uncover the genetic, cellular, and circuit-level underpinnings of those psychopathological dimensions and their overlapping and distinct contribution to anxiety disorders and MDD. Furthermore, the large effects of risk factors on the latent variable underlying anxiety disorders and MDD suggest that their shared liability[63] may contribute to explain the high comorbidity among them.[13, 14, 64] From the interventions perspective, the large impact of the risk factors on the latent structure of anxiety disorders and MDD suggests that preventive interventions on a single risk factor with large effect on the latent structure could simultaneously decrease the risk for all the disorders. At the same time, since several risk factors affect the latent structure jointly, interventions that address several risk factors simultaneously are likely to be the most effective. The presence of disorder-specific effects suggests that supplementary modules may be necessary to provide intervention flexibility, promote personalized medicine, and optimize the outcome of all individuals.
Several limitations should be considered in the interpretation of these results. First, because of the cross-sectional nature of the study, although associations identified in this study could be informative regarding the etiology of anxiety disorders and MDD, causality cannot be inferred. However, because our results remain almost unchanged when we restricted the analyses to individuals 21 and older, reverse causality is unlikely to explain our results. Second, although our model is comprehensive, it is not exhaustive. In order to be parsimonious, in accord with established recommendations for model[65] development, we limited the number of variables based on a priori conceptual model.[26, 28] Future investigations could examine the common and specific effects of other potential risk factors. Third, our sample was composed of individuals 18 and older. The model may not be applicable to younger individuals or individuals of other cohorts. Fourth, some variables, such as childhood sexual abuse, were assessed retrospectively and may be subject to recall bias, whereas others, such as low self-esteem, were assessed with a single item. This may have increased error variance and underestimated the strength of association of the risk factors with the outcomes. Therefore, our estimates are likely to be conservative. Fifth, some variables of potential interest, such as family history of anxiety disorders, were not assessed in the NESARC and could not be included in the model.
In conclusion, risk for anxiety disorders and MDD appears to be mediated partially by a latent variable underlying these disorders, and partially by disorder-specific effects. The shared risk may contribute to the large rates of comorbidity among disorders, help to identify commonalities in the etiologies of these disorders, and provide clues for the development of unified treatment protocols or integrated preventive interventions.[66] The disorder-specific effects may contribute toward the distinct aspects of the etiology of each disorder and suggest the need for intervention flexibility. These findings may help inform dimensional models of classification of psychiatric disorders.
Supplementary Material
Acknowledgments
This study was supported by NIH grants DA019606, DA023200, MH076051, and MH082773 (CB) and the New York State Psychiatric Institute (CB and MW).
REFERENCES
- 1.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 2.Wittchen HU. Generalized anxiety disorder: prevalence, burden, and cost to society. Depress Anxiety. 2002;16:162–171. doi: 10.1002/da.10065. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization, editor. Geneva, Switzerland: WHO; 2001. World Health Report 2001: Mental Health: New Understanding, New Hope. [Google Scholar]
- 4.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 5.Rodriguez BF, Bruce SE, Pagano ME, Keller MB. Relationships among psychosocial functioning, diagnostic comorbidity, and the recurrence of generalized anxiety disorder, panic disorder, and major depression. J Anxiety Disord. 2005;19:752–766. doi: 10.1016/j.janxdis.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 6.Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- 7.Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychol Med. 2006;36:1593–1600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- 8.Tambs K, Czajkowsky N, Roysamb E, et al. Structure of genetic and environmental risk factors for dimensional representations of DSM-IV anxiety disorders. Brit J Psychiat. 2009;195:301–307. doi: 10.1192/bjp.bp.108.059485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vollebergh WAM, Iedema J, Bijl RV, et al. The structure and stability of common mental disorders: the NEMESIS study. Arch Gen Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- 10.Kendler KS, Heath AC, Martin NG, Eaves LJ. Symptoms of anxiety and symptoms of depression: same genes, different environments? Arch Gen Psychiatry. 1987;44:451–457. doi: 10.1001/archpsyc.1987.01800170073010. [DOI] [PubMed] [Google Scholar]
- 11.Andrews G, Stewart G, Allen R, Henderson A. The genetics of six neurotic disorders: a twin study. J Affect Disord. 1990;19:23–29. doi: 10.1016/0165-0327(90)90005-s. [DOI] [PubMed] [Google Scholar]
- 12.Scherrer JF, True WR, Xian H, et al. Evidence for genetic influences common and specific to symptoms of generalized anxiety and panic. J Affect Disord. 2000;57:25–35. doi: 10.1016/s0165-0327(99)00031-2. [DOI] [PubMed] [Google Scholar]
- 13.Hettema JM, Prescott CA, Myers JM, et al. The structure of genetic and environmental risk factors for anxiety disorders in men and women. Arch Gen Psychiatry. 2005;62:182–189. doi: 10.1001/archpsyc.62.2.182. [DOI] [PubMed] [Google Scholar]
- 14.Hettema JM, Neale MC, Kendler KS. A review and meta-analysis of the genetic epidemiology of anxiety disorders. Am J Psychiatry. 2001;158:1568–1578. doi: 10.1176/appi.ajp.158.10.1568. [DOI] [PubMed] [Google Scholar]
- 15.Morcillo C, Duarte CS, Sala R, et al. Conduct disorder and adult psychiatric diagnoses: associations and gender differences in the US adult population. J Psychiatr Res. 2012;46:323–330. doi: 10.1016/j.jpsychires.2011.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kessler RC, McLaughlin KA, Green JG, et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Brit J Psychiat. 2010;197:378–385. doi: 10.1192/bjp.bp.110.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Magee WJ, Eaton WW, Wittchen HU, et al. Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Arch Gen Psychiatry. 1996;53:159–168. doi: 10.1001/archpsyc.1996.01830020077009. [DOI] [PubMed] [Google Scholar]
- 18.Marmorstein NR. Anxiety disorders and substance use disorders: different associations by anxiety disorder. J Anxiety Disord. 2012;26:88–94. doi: 10.1016/j.janxdis.2011.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McEvoy PM, Grove R, Slade T. Epidemiology of anxiety disorders in the Australian general population: findings of the 2007 Australian National Survey of Mental Health and Wellbeing. Aust NZ J Psychiat. 2011;45:957–967. doi: 10.3109/00048674.2011.624083. [DOI] [PubMed] [Google Scholar]
- 20.Merikangas KR, Zhang H, Avenevoli S, et al. Longitudinal trajectories of depression and anxiety in a prospective community study: the Zurich Cohort Study. Arch Gen Psychiatry. 2003;60:993–1000. doi: 10.1001/archpsyc.60.9.993. [DOI] [PubMed] [Google Scholar]
- 21.Mulhare ES, Ghesquiere A, Shear AK. Attachment, separation and anxiety disorders. In: Simpson HB, Neria Y, Lewis-Fernandez R, Schneier F, editors. Anxiety Disorders: Theory, Research and Clinical Perspectives. New York, NY: Cambridge University Press; 2010. pp. 227–238. [Google Scholar]
- 22.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Anxiety Disord. 2010;25:456–465. doi: 10.1016/j.janxdis.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Richards M, Hardy R, Wadsworth M. The effects of divorce and separation on mental health in a national UK birth cohort. Psychol Med. 1997;27:1121–1128. doi: 10.1017/s003329179700559x. [DOI] [PubMed] [Google Scholar]
- 24.Zoccolillo M. Co-occurrence of conduct disorder and its adult outcomes with depressive and anxiety disorders: a review. J Am Acad Child Adolesc Psychiatry. 1992;31:547–556. doi: 10.1097/00004583-199205000-00024. [DOI] [PubMed] [Google Scholar]
- 25.Brandes M, Bienvenu OJ. Personality and anxiety disorders. Curr Psychiatry Rep. 2006;8:263–269. doi: 10.1007/s11920-006-0061-8. [DOI] [PubMed] [Google Scholar]
- 26.Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in women. Am J Psychiatry. 2002;159:1133–1145. doi: 10.1176/appi.ajp.159.7.1133. [DOI] [PubMed] [Google Scholar]
- 27.Kendler KS, Prescott CA. Genes, Environment and Psychopathology: Understanding the Causes of Psychiatric and Substance Use Disorders. New York: The Guilford Press; 2006. [Google Scholar]
- 28.Alegria AA, Hasin DS, Nunes EV, et al. Comorbidity of generalized anxiety disorder and substance use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2010;71:1187–1195. doi: 10.4088/JCP.09m05328gry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Noyes R, Holt CS, Woodman CL. Natural course of anxiety disorders. In: Mavissakalian M, Prien R, editors. Long-Term Treatments of Anxiety Disorders. Washington, DC: American Psychiatric Press; pp. 1–48. [Google Scholar]
- 30.Blanco C, Xu Y, Schneier FR, et al. Predictors of persistence of social anxiety disorder: a national study. J Psychiatr Res. 2011;45:1557–1563. doi: 10.1016/j.jpsychires.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 31.Yonkers KA, Bruce SE, Dyck IR, Keller MB. Chronicity, relapse, and illness—course of panic disorder, social phobia, and generalized anxiety disorder: findings in men and women from 8 years of follow-up. Depress Anxiety. 2003;17:173–179. doi: 10.1002/da.10106. [DOI] [PubMed] [Google Scholar]
- 32.Grant B, Moore TC, Shepard J, Kaplan K. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. Source and Accuracy Statement: Wave 1. National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) [Google Scholar]
- 33.Grant BF, Dawson DA, Stinson FS, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 34.Grant B, Moore TC, Shepard J, Kaplan K. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2005. Source and Accuracy Statement: Wave 2. National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) [Google Scholar]
- 35.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 36.Grant BF, Dawson DA, Hasin DS, editors. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2004. The Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions Alcohol Use Disorder and Associated Disabilities Interview Schedule—DSM-IV Version. [Google Scholar]
- 37.Grant B, Dawson D, Hasin D. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. [Google Scholar]
- 38.Ruan W, Goldstein RB, Chou SP, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. J Am Acad Child Adolesc Psychiatry. 1997;36:340–348. doi: 10.1097/00004583-199703000-00012. [DOI] [PubMed] [Google Scholar]
- 40.Vesga-Lopez O, Schneier FR, Wang S, et al. Gender differences in generalized anxiety disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) J Clin Psychiatry. 2008;69:1606–1616. [PMC free article] [PubMed] [Google Scholar]
- 41.Blanco C, Vesga-Lopez O, Stewart JW, et al. Epidemiology of major depression with atypical features: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) J Clin Psychiatry. 2012;73:224–232. doi: 10.4088/JCP.10m06227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lopez-Quintero C, Hasin DS, De Los Cobos JP, et al. Probability and predictors of remission from life-time nicotine, alcohol, cannabis or cocaine dependence: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addiction. 2011;106:657–669. doi: 10.1111/j.1360-0443.2010.03194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lopez-Quintero C, Cobos JP, Hasin DS, et al. Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Drug Alcohol Depend. 2011;115:120–130. doi: 10.1016/j.drugalcdep.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hu LT, Bentler PM, Kano Y. Can test statistics in covariance structure analysis be trusted? Psychol Bull. 1992;112:351–362. doi: 10.1037/0033-2909.112.2.351. [DOI] [PubMed] [Google Scholar]
- 45.Kim ES, Yoon M, Lee T. Testing measurement invariance using MIMIC: likelihood ratio test with a critical value adjustment. Educ Psychol Meas. 2011;72:469–492. [Google Scholar]
- 46.Muthen LK, Muthen BO. Mplus User’s Guide. Los Angeles, CA: Muthen & Muthen; 1998–2006. [Google Scholar]
- 47.Stark S, Chernyshenko OS, Drasgow F. Detecting differential item functioning with confirmatory factor analysis and item response theory: toward a unified strategy. J Appl Psychol. 2006;91:1292–1306. doi: 10.1037/0021-9010.91.6.1292. [DOI] [PubMed] [Google Scholar]
- 48.Blanco C, Rubio JM, Wall MM, et al. The latent structure and comorbidity patterns of generalized anxiety disorder and major depressive disorder: a national study. Depress Anxiety. 2013 doi: 10.1002/da.22139. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pérez-Fuentes GOM, Villegas L, Morcillo C, Wang S, Blanco C. Prevalence and correlates of child sexual abuse: a national study. Compr Psychiat. 2013;54:16–27. doi: 10.1016/j.comppsych.2012.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Keyes KM, Eaton NR, Krueger RF, et al. Childhood maltreatment and the structure of common psychiatric disorders. Br J Psychiatry. 2012;200:107–115. doi: 10.1192/bjp.bp.111.093062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Heim C, Nemeroff CB. The impact of early adverse experiences on brain systems involved in the pathophysiology of anxiety and affective disorders. Biol Psychiatry. 1999;46:1509–1522. doi: 10.1016/s0006-3223(99)00224-3. [DOI] [PubMed] [Google Scholar]
- 52.Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biol Psychiatry. 2001;49:1023–1039. doi: 10.1016/s0006-3223(01)01157-x. [DOI] [PubMed] [Google Scholar]
- 53.Blanco C, Hasin DS, Liu SM, et al. Mapping common psychiatric disorders: structure and predictive validity in the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2013;70:199–208. doi: 10.1001/jamapsychiatry.2013.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- 55.Acarturk C, Smit F, De Graaf R, et al. Incidence of social phobia and identification of its risk indicators: a model for prevention. Acta Psychiat Scand. 2009;119:62–70. doi: 10.1111/j.1600-0447.2008.01275.x. [DOI] [PubMed] [Google Scholar]
- 56.Silverstone PH. Low self-esteem in different psychiatric conditions. Brit J Clin Psychol. 1991;30:185–188. doi: 10.1111/j.2044-8260.1991.tb00936.x. [DOI] [PubMed] [Google Scholar]
- 57.Silverstone PH, Salsali M. Low self-esteem and psychiatric patients: part I—the relationship between low self-esteem and psychiatric diagnosis. Ann Gen Psychiatry. 2003;2:2. doi: 10.1186/1475-2832-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Breslau N, Kessler RC, Chilcoat HD, et al. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- 59.Cosci F, Schruers KRJ, Abrams K, Griez EJL. Alcohol use disorders and panic disorder: a review of the evidence of a direct relationship. J Clin Psychiatry. 2007;68:874–880. doi: 10.4088/jcp.v68n0608. [DOI] [PubMed] [Google Scholar]
- 60.Kendler KS, Neale MC, Kessler RC, et al. Major depression and generalized anxiety disorder: same genes, (partly) different environments? Arch Gen Psychiatry. 1992;49:716–722. doi: 10.1001/archpsyc.1992.01820090044008. [DOI] [PubMed] [Google Scholar]
- 61.Insel TR, Cuthbert BN, Garvey MA, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 62.National Institute of Mental Health. NIMH Research Domain Criteria (RDoC) 2011. doi: 10.1037/abn0000768. Available at: http://www.nimh.nih.gov/research-funding/rdoc/nimh-research-domain-criteria-rdoc.shtml. [DOI] [PubMed]
- 63.Neale MC, Kendler KS. Models of comorbidity for multifactorial disorders. Am J Hum Genet. 1995;57:935–953. [PMC free article] [PubMed] [Google Scholar]
- 64.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kline RB. Principles and Practice of Structural Equation Modeling. 2nd ed. New York: Guilford Press; 2005. [Google Scholar]
- 66.Barlow D, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behav Ther. 2004;35:205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.