Abstract
Purpose
To determine whether young adults are interested in a Facebook intervention for smoking cessation and to inform the design of such an intervention.
Design
Mixed-methods.
Setting
Participants throughout the United States were recruited through Facebook.
Participants
Young adults age 18 to 25 who had smoked at least once in the past month.
Method
Participants (N=570) completed an online survey of tobacco and social media use. A subset of 30 survey completers, stratified by motivation to quit smoking, agreed to participate in a structured interview over online chat. Themes were identified using grounded theory.
Results
About a third of the full sample (31%) reported they would want to get help to quit smoking using Facebook. Interest in using Facebook to quit was greater among those more motivated to quit (χ2=75.2, p<.001), who had made a quit attempt in the past year (χ2=16.0, p<.001), and had previously used the Internet for assistance with a quit attempt (χ2=6.2, p=.013). In qualitative interviews, social support and convenience were identified as strengths of a Facebook intervention; while privacy was the main issue of concern.
Conclusion
Nearly one in three young adult smokers on Facebook expressed interest in using Facebook for quitting smoking. Social media approaches that respect privacy and tailor to readiness to quit are likely to maximize participation.
Keywords: smoking cessation, young adults, social media, Facebook
Purpose
Although the prevalence of cigarette smoking has been slowly declining since the 1970s, the smoking prevalence among young adults aged 18–25 years has remained stable and higher than other age groups, with past month cigarette use at 32% in 2012.1 Compared to other age groups, young adults are less likely to use behavioral or pharmacotherapy interventions for smoking cessation,2 and studies of tobacco use have reported great challenges in recruiting young adults.3, 4 Reaching the US public health goals of cutting the smoking rate to no higher than 12% by 20205 will require novel approaches to reach and intervene with young adult smokers.
For reaching young adult smokers, the Internet is a particularly promising strategy. Almost all (94%) young adults in the US use the Internet, and young adults are the age group most likely to go online.6 Online smoking-cessation strategies have reached large samples of smokers.7 However, as online interventions have been associated with large drop-offs in engagement of smokers,8, 9 strategies are needed to increase demand for and sustained engagement in online interventions for young adults.
Online social networks may serve as a solution to the problems of reach and engagement in smoking cessation interventions for young adults. Social networks, including those developed through online social media, play a well-established role in onset and perpetuation of smoking behavior.10-12 Social network science has helped to explain how diffusion of information among members of a social network can also influence a broad range of behavioral and emotional changes including smoking cessation.13-15 Social networks in the form of peer email support have been successful at influencing engagement in online smoking cessation intervention that could lead to quitting.16, 17 Further, patterns of social interactions through online smoking cessation forums have characterized ways that social networks can influence smoking cessation through social support, including by offering encouragement and emotional support, stories, congratulations, “thank” you messages, giving practical advice and tips, and discussing nicotine replacement therapy.18, 19 With wide reach and engagement among users, social media websites (e.g., Facebook, GooglePlus) offer phenomenal opportunity to use social interactions to engage young people in behavior change interventions and to foster socially supportive communities that can help each other quit smoking and maintain abstinence.
The reach of social media among young adults is vast. Over three-quarters (83%) of online 18-29 year olds use social-networking websites, with 70% doing so on a typical day.20, 21 Facebook is the 2nd most popular website in the US,22 with over 1.15 billion monthly active users and 699 million daily users as of June 2013.23 Facebook has been the source of numerous wide-reaching public health campaigns targeting smoking among young people. For example the American Legacy Foundation’s national truth® campaign had over 2 million “Likes” on its Facebook page as of October 2013, and according to Facebook data, was most often mentioned directly in any type of communication on Facebook by 18-24 year olds compared to other age groups.24 Further marketing campaigns on social media offer the opportunity to target only those who have identified within a certain age range (e.g., 18-25 years old) and/or have indicated interest in behaviors such as smoking, making Facebook a promising mechanism to target young adult smokers for cessation programs.25 However, the use of social media including Facebook to intervene with young adult smokers has yet to be evaluated.
The US Senate Appropriations Committee has called for the NIH to support research using social media,26 and the technology industry has recognized the potential of Facebook to change health behaviors.27 Some work has examined the feasibility, engagement, and efficacy of using Facebook to deliver health behavior change interventions in areas other than smoking. A randomized controlled trial testing the efficacy of a physical activity intervention combining education, a self-monitoring tool, and a Facebook group versus education alone found that participants were satisfied with their use of a Facebook group and participation was higher compared to other online support mechanisms.28 A study of adolescents and young adults (ages 15-24) who accessed a Facebook site that disseminated sexually transmitted disease education reported a 23% increase in condom utilization.29 In a randomized controlled evaluation of Facebook for disseminating information on condom adoption, Bull et al.30 enrolled 1578 adolescents and young adults in the U.S. (ages 16-25) and reported their Facebook page had 43 unique visitors per week during the intervention period and approximately 10% of the intervention’s 942 participants regularly posted to the Facebook page. Three quarters of the sample completed at least one follow-up assessment, and participants in the intervention group more consistently used condoms than controls at 2 months follow-up (68% vs. 54%). Napolitano et al.31 found that an 8-week intervention for college students that included a Facebook page, text messaging, and personalized feedback resulted in greater weight loss than a Facebook-only or wait-list control group.
It is unknown whether young adult smokers will be receptive to a Facebook intervention targeting tobacco cessation. Given the strong addictive potential of nicotine32 that often necessitates both behavioral and pharmacologic intervention,33 and less likelihood among young adults to identify as “smokers” 34 or seek treatment for smoking cessation,2 there may be some unique challenges to engaging young adults in a smoking cessation intervention using Facebook.
We have had good success with recruiting young adult smokers through social networking websites and other online resources for participation in one-time survey studies.25, 35 In 9 months time, we recruited and surveyed 1987 young adult smokers; about half of whom wanted to quit smoking in the next 6 months. Among smokers who were motivated to quit, one in four expressed interest in a cessation intervention administered through the Internet. Thus, there appears to be some interest in online interventions targeting young adult smokers. The specific format, process and content of online interactions for smoking cessation, however, are largely unshaped; and efforts to increase the perceived attractiveness and utility are needed. In particular, ideas are needed on how best to leverage and optimize young adults’ experiences with and use of social media for health behavior change efforts such as quitting smoking.
Mixed-methods study designs, combining quantitative and qualitative data, provide unique benefits over single-method designs36, 37 and may yield a fuller understanding of complex phenomena such as receptivity to intervention through social media.38 Quantitative data can reveal patterns of health behavior and Internet use, while qualitative data are beneficial for identifying the lived experience of the target audience and their receptivity to specific aspects of an intervention.
The present study combined qualitative and quantitative methods to answer the following three research questions: 1) Are young adults interested in a smoking cessation intervention through Facebook?; 2) Should a Facebook intervention be targeted to a particular type of smoker?; and 3) How exactly can/should Facebook be used to help young adults quit smoking?
Design
This mixed-methods research was conducted in two phases. In Phase I, quantitative data were gathered from young adults who completed an online survey. In Phase II, qualitative interviews were conducted online with a subsample of survey respondents.
Setting
The study (Phases I and II) was conducted entirely online.
Participants
Participants were young adults between the ages of 18 and 25, who were English literate, and reported smoking at least one cigarette in the past 30 days. Advertisements on Facebook invited young adults to participate in a 20-minute online survey with a chance to win a prize in a drawing (worth $100). Advertisement text and images were targeted to tobacco smokers (e.g., picture of a pack of cigarettes or person smoking; text that read “Ever smoke?”). The campaign ran for two 5-month periods, from 9/27/10 to 2/8/11 and again 4/28/11 to 9/26/11, with the break due to a two-month lapse in recruitment funds. Advertisements contained a hyperlink that directed potential participants to: 1) the study’s University of California, San Francisco IRB-approved consent form that included verification questions to determine understanding of the consent process; and 2) a screener for determining eligibility including English literacy, age (18 to 25), and past month cigarette smoking (y/n).
Method
Data Collection: Quantitative
Participants who consented and were deemed eligible were asked to complete a demographic questionnaire and measures of tobacco and Internet use and receptivity to using social networking websites for smoking cessation. The survey was anonymous, and data were encrypted for added security protection. Participants were required to answer all questions before they could continue to the next page of the survey, but could quit and return to the survey at any time. Computer IP addresses were tracked and only one entry was allowed from a single computer to prevent duplicate entries from the same person; however, multiple entries were allowed from the same Internet connection (dormitories, apartment buildings). Eligibility checks excluded respondents who: 1) had discrepant data on similar demographic questions (e.g., date of birth and age indicating they were either too young or too old to participate); 2) reported the same email address across multiple survey entries; 3) had clearly invalid data (e.g., every entry was the same across the entire survey).
The demographic and tobacco use measures in the current study were previously analyzed with young adult smokers using anonymous online survey methods and demonstrated good reliability and validity.39, 40
Sociodemographics
Gender, age, race/ethnicity, student status, employment status, annual personal and family income, and highest parental level of education were assessed. Residential zip codes were used to categorize participants as residing in: 1) one of four U.S. Census Regions: Northeast, Midwest, South, and West;41 and 2) an urban or rural area, using zip code approximations of rural-urban communing area data from the 2000 census in a coding system made public by the University of Washington Rural Health Research Center.42
Cigarette smoking behavior
We assessed participants’ average number of cigarettes smoked per day, days smoking per week on average (from which we computed percent smoking 7 days per week as “daily”), age of initiation of smoking, years of smoking, prior quit attempts (lifetime and past year), and strategies used to aid a prior quit attempt including Internet-based strategies.43 Time to first cigarette upon waking (<30 min or >30 min), with good psychometric properties, was used as a measure of dependence.44 One item assessed self-identified social smoking, “Are you a social smoker?” (y/n). The 3-item Tobacco Smoking Stages of Change Questionnaire assessed motivation to quit,45 categorizing smokers into one of three pre-action stages of change (Precontemplation: no intention to quit within the next 6 months; Contemplation: intention to quit within the next 6 months but no 24-hr quit attempt in the past year; Preparation: intention to quit within the next month and a 24-hr quit attempt in the past year).
Social networking use
The frequency of social media use, sites visited most often, and ways in which individuals use social media were assessed using questions from a recent survey conducted for the Pew Internet and American Life Project.46, 47 Some questions were adapted to specifically address Facebook usage and trends, including assessing for usage frequency, modes of communication, and use of Facebook applications (“apps”). This measure is available upon request from the first author.
Likelihood of using social media for smoking cessation
A measure was developed for the present study to assess participants’ likelihood of using social media for smoking cessation and likelihood that they would take advantage of specific features of such an intervention (e.g., chat rooms, links to others who are also trying to quit smoking, links to other resources).
Analysis Strategies: Quantitative
Descriptive statistics were used to examine sample characteristics and patterns of tobacco, Internet, and social media use. To evaluate whether young adults were interested in using Facebook to quit smoking, we looked at frequencies of reports of intentions to use Facebook and intentions to use specific Facebook communication strategies. To evaluate whether a Facebook intervention should be targeted to a particular type of smoker, ANOVA and chi-square analyses examined relationships between Internet use variables (frequency of Internet use, frequency of Facebook use, previous quit attempts using the Internet, and intention to use FB to quit smoking) and smoking variables (average cigarettes per day, average days smoking per week, daily smoking status, smoking within 30 minutes of waking [y/n], age of first cigarette, total years smoked, past year quit attempt [y/n], stage of change [precontemplation, contemplation, preparation], and self-identification as a social smoker [y/n].
Data Collection: Qualitative
Upon completing the online survey, all participants were asked if they were interested in completing a one-hour online interview about their smoking and Internet behaviors at a later time. Those who agreed were screened for stage of change and then contacted by email to schedule an interview through meebo.com, an online instant messaging service. To obtain representation from each stage of change (precontemplation, contemplation, preparation), participants were contacted for scheduling in order of survey completion until 10 participants completed interviews from each stage (N=30 interviews). Scheduled participants were provided with a username and a unique password for their interviews.
A semi-structured interview guide was developed for the current study that asked participants more detailed questions about their smoking behavior, identity, and quitting (e.g., “Do you see yourself as a smoker or something else?,” “What do you think would need to be different for you to quit forever?”), general thoughts about a smoking cessation program administered through Facebook (e.g, “How would your Facebook friends react if they knew you were trying to stop smoking?”), and their willingness to perform specific activities on Facebook that support smoking cessation and how they might benefit from those activities (e.g., “Would you download a Facebook app that would help you quit smoking? What do you think you would get out of that?”). After half of the interviews had been completed, data were loosely examined and based on recurring themes of quit attempts and online privacy, questions were added to the interview guide to assess detailed experiences with quit attempts and views on online privacy. Recruitment continued until information was saturated as determined by the first author.
Analysis Strategies: Qualitative
Two research staff members independently coded the interview transcripts using two major types of coding. For specific types of communication on Facebook, responses were initially open-coded and valence was coded for each type of communication participants were asked about (positive, negative, or ambivalent). Next, using a Grounded Theory approach,48 major themes on any topic were identified from the interviews and grouped into concepts around using Facebook to quit smoking. This process was facilitated by using ATLAS.ti, a qualitative data analysis software for organizing open coding.49 A tentative list of codes was developed by one of the coders and the first author based on the semi-structured interview. The coders began coding the interviews with this list and added new codes as more themes became apparent. Once complete, the coded interviews were compared and discussed with the first author and discrepant codes were resolved.
Results
Survey
Sample characteristics
The online survey received more than 3483 hits and 975 people gave online consent to determine eligibility to complete the survey. Of those, 718 (74%) met criteria and 39 (5%) were deemed invalid, leaving 679 (70%) eligible and valid cases. Of those, 646 (95%) completed the demographic items, 594 (87%) completed the smoking items, and 570 (84%) completed the entire survey. Compared to those who only completed demographic items (n=76), survey completers were more likely to be female (29.8% vs. 17.1%, χ2 = 5.34, p = .021) but did not differ on any other demographic characteristic. Compared to those who only completed the smoking items (n=24), survey completers were less likely to be daily smokers (70% vs. 88%, χ2 = 4.48, p = .043), smoked fewer cigarettes per day on average (6.0 vs. 6.8, t = -2.86, p = .004), and were less likely to smoke their first cigarette within the first 30 minutes of waking (42% vs. 56%, χ2 = 10.57, p = .014). Data analyses were restricted to those who completed the entire survey (N = 570). Sociodemographic and smoking characteristics of the sample are summarized in Table 1.
Table 1.
Sociodemographic characteristics of young adults smokers who completed the online survey (N = 570) compared to the subset that also completed the online interview (n = 30)
| Variable | Full sample (N = 570) | Interviewees (n = 30) | χ2 / t | p-value |
|---|---|---|---|---|
| Age (M [SD]) | 19.9 (1.8) | 20.3 (1.7) | -1.40 | .163 |
| Gender (% female)a | 29.8 | 40.0 | 1.54 | .223 |
| Ethnicity | 13.47 | .019 | ||
| African-American | 2.6 | 0.0 | ||
| Asian-American/Pacific Islander | 3.7 | 13.3 | ||
| Caucasian-American | 68.6 | 66.7 | ||
| Hispanic/Latino | 9.8 | 0.0 | ||
| Multi-Ethnic | 13.2 | 20.0 | ||
| Other | 1.9 | 0.0 | ||
| Annual personal income | 2.95 | .400 | ||
| Less than $10,000 | 84.9 | 90.0 | ||
| $10,000 - $30,000 | 13.9 | 6.7 | ||
| $30,000 - $50,000 | 1.1 | 3.3 | ||
| Over $50,000 | 0.2 | 0.0 | ||
| Annual household income | 2.86 | .414 | ||
| Less than $20,000 | 27.4 | 36.7 | ||
| $20,000 - $60,000 | 37.4 | 23.3 | ||
| $60,000 - $100,000 | 21.1 | 23.3 | ||
| Over $100,000 | 14.2 | 16.7 | ||
| Years of education (M [SD]) | 12.5 (1.5) | 13.0 (1.3) | -1.73 | .084 |
| Employment status | 1.15 | .562 | ||
| Employed (>= 20 hours per week) | 27.9 | 33.3 | ||
| Employed part-time (<20 hours per week) | 25.8 | 30.0 | ||
| Unemployed/Homemaker | 46.3 | 36.7 | ||
| Currently enrolled in school a | 0.23 | .709 | ||
| Full-time/part-time | 52.5 | 56.7 | ||
| Not enrolled | 47.5 | 43.3 | ||
| Highest level of parental education | 4.74 | .315 | ||
| Some high school or less | 5.2 | 0.0 | ||
| Completed high school/GED | 21.1 | 31.0 | ||
| Some college | 16.4 | 6.9 | ||
| Completed college | 35.7 | 37.9 | ||
| Some graduate work/A graduate degree | 21.6 | 24.1 | ||
| Region | 2.20 | .532 | ||
| Northeast | 19.8 | 30.0 | ||
| Midwest | 26.7 | 23.3 | ||
| South | 25.8 | 23.3 | ||
| West | 27.7 | 23.3 | ||
| Area type a | 3.33 | .107 | ||
| Urban | 84.9 | 96.7 | ||
| Rural | 15.1 | 3.3 | ||
| Daily smoker | 70.0 | 79.3 | 1.03 | .403 |
| Cigarettes per day (M [SD]) | 10.3 (8.2) | 1.4 (.57) | ||
| Smoke first cigarette within 30 minutes of waking | 41.6 | 34.5 | 9.11 | .028 |
| Smoking stage of change | 8.01 | .018 | ||
| Precontemplation | 57.5 | 34.5 | ||
| Contemplation | 28.1 | 37.9 | ||
| Preparation | 14.4 | 27.6 |
Note. All values are percentages unless otherwise indicated.
Fisher’s exact test.
Cigarette smoking behavior
On average, the sample smoked 10.3 cigarettes per day (SD = 8.2), first tried smoking at age 14.5 (SD = 3.0), smoked for 3.7 years (SD = 2.8), 42% smoked within 30 minutes of waking, 70% were daily smokers, and 65% identified as a social smoker. A little over half the sample (57%) made a quit attempt in the past year, 2% had previously used the Internet to quit smoking, and 43% indicated they were intending to quit smoking in the next six months (Contemplation or Preparation).
Internet/Social media use
Internet use and social media use behaviors of young adults recruited through Facebook are reported in Figure 1. A large proportion of the sample (85%) used the Internet multiple times a day, and an equally large proportion (87%) visited Facebook daily. More than half of the sample (57%) used their cell phones to browse or update their Facebook profile. Participants reported how they communicated using Facebook with the three most common communication strategies being: posting comments on their friends’ walls/pages (70%), adding comments to their friends’ pictures (64%), and sending private messages through Facebook (63%). About a quarter of the sample (27%) downloaded one or more Facebook applications (“apps”) in the past month and a similar proportion (27%) used one or more Facebook apps regularly. More than half the sample (65%) had profiles on two or more social networking websites.
Figure 1.
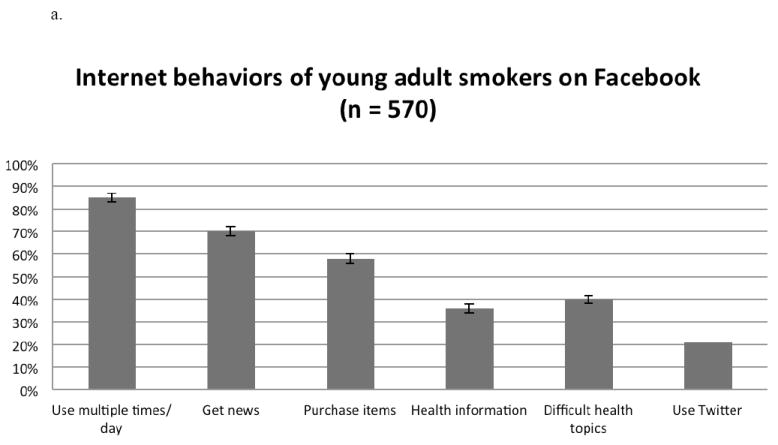
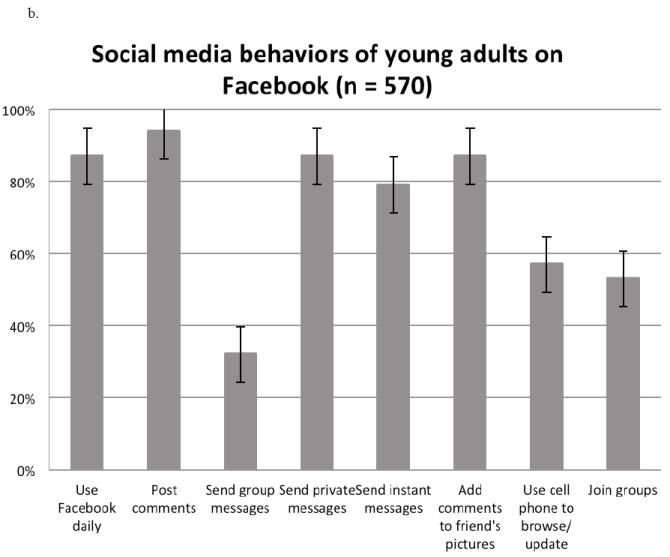
a. Internet behaviors of young adult smokers. Error bars represent standard errors.
b. Social media behaviors of young adult smokers. Error bars represent standard errors.
Intention and strategies to cut down/quit smoking using social media
About a third of all participants (31%) reported they would like help to cut down or quit smoking using social media, and 56% of those ready to quit indicated they would use social media to quit. Specific strategies and proportions reporting likely use included: general resource about smoking/quitting (30%), personalized messages (28%), downloading an app for quitting (26%), making new FB friends with similar issues around smoking (26%), status updates (19%), downloading an app for information about smoking and health (17%), wall postings (15%), and other (26%).
Relationships between motivation to quit, smoking characteristics and interest in Facebook for quitting smoking
Interest in using Facebook to quit smoking in the future was greater among those with greater motivation to quit smoking (17.1% precontemplation < 48.1% contemplation < 56.1% preparation; χ2 = 75.2, p < .001), those who had made a quit attempt in the past year (38.2% vs. 22.4%, χ2 = 16.0, p < .001), and those who had previously used the Internet for assistance with a quit attempt (66.7% vs. 28.6%, χ2 = 6.2, p = .013). No other smoking variables were associated with intention to quit smoking by using Facebook.
Qualitative Interviews
Of the 570 respondents who completed the survey, 395 indicated they would be interested in completing a follow-up interview, 219 were contacted for scheduling, 59 responded, and 30 of those were interviewed (10 in each stage of change). Sample characteristics are presented in Table 1. Compared to the full sample (N = 570), the qualitative interview respondents were more likely to identify as Asian or multi-ethnic and less likely to be African-American or Hispanic (χ2 = 13.5, p = .019). They were also less likely to smoke their first cigarette of the day within 30 minutes of waking (χ2 = 9.11, p = .028) and were more ready to quit smoking (65.5% ready to quit in the next 6 months vs. 42.5%; χ2 = 8.01, p = .018). No other demographic or smoking variables differed.
First, specific quotes were organized by General reactions to a Facebook intervention and six specific ways of communicating on Facebook, quotes were coded for valence, and frequencies were counted for each communication type (Table 2). Valence reflected positive, negative, and ambivalent/neutral responses. More detailed descriptions and sample quotes are presented below, with all quotes followed by interviewee sex, age, and stage of change (precontemplation, contemplation, or preparation) and in Table 2.
Table 2.
Types of communication, valence, and sample quotes around using Facebook for smoking cessation
| Facebook communications | Count/respondents | Valence (counts/respondents) | Sample Quote |
|---|---|---|---|
| General reactions to Facebook intervention | 52/30 |
|
Facebook is always better about everything. I am already there so I wouldn’t have to go other places to see it. (Positive) |
| Facebook page that actively helps quitting | 60/28 |
|
yes, if the page posted quitting smoking facts or facts about how bad ciggerettes are. reading the posts on my community wall would be helpful. (Positive) |
| Facebook application that actively helps quitting | 41/24 |
|
Well my biggest thing every time I actually quit was trying to break my normal routine. So if you had something that would ask you to challenge that or modify your routine, that would work (Positive) |
| Personalized messages | 23/21 |
|
everyone is different so everyone goes through different withdrawl symptoms. While I may be irritable and gain a buncha weight, my friend could be coughing up a storm and having other symptoms. So personalized messages would def. be a good idea. (Positive) |
| Status updates about quitting | 20/19 |
|
there is plenty of interaction with those online…. Even just “liking” the status shows support. But friends also have the chance to show their opinion with comments. (Positive) |
| Wall posts | 31/22 |
|
…[wall posts] would provide an opportunity for your friends and loved ones to see how you’re doing and maybe give you some words of encouragement. (Positive) |
| Using Facebook instead of other websites for quitting smoking | 39/29 |
|
I feel like if I was going to try and find a support group online for smoking, I would just use facebook… I feel like Facebok is really casual, and I don’t want to mix casual circles with serious ones, usually. (Positive) |
Note. Sample quotes were chosen to reflect the most common subthemes for each theme. All quotes are reproduced exactly as written by respondents.
General reactions to using a Facebook intervention were more positive than negative and ambivalent. Some thought Facebook could be supportive yet less invasive than the real world, with one participant noting “It’d be great for people who just need to know that they aren’t the only one quitting, or that people support their decision without feeling pressured to quit (since family can be pretty pushy and it sucks to hide things from your family)…” (female, age 22, preparation).
We asked participants their opinions about various types of Facebook interactions. There were far more positive than negative quotes about a page that actively helps with quitting (77% positive quotes), receiving personalized messages to help them quit smoking (78% positive quotes), and being asked to update their Facebook status about quitting smoking (70% positive quotes). One participant suggested “one article a day max and not very long but ‘rich’” (male, age 20, contemplation). Concerns about these strategies reflected ambivalence about quitting in general such as “I don’t like being nagged, and even though it would be well intentioned, I would feel pressured, and I tend to push against being pressured…” (male, 22, precontemplation).
There was also general enthusiasm for an intervention through a Facebook application (“app”) that would have to be downloaded to participants’ Facebook pages (63% positive quotes). Positive comments reflected the convenience of an application such as “..I think it’d be a helpful reminder to stay on track” (female, 20, precontemplation). Negative comments reflected concerns about applications and privacy. One participant noted “I’m a little reluctant on the app because some of them can be intrusive and post things without your permission” (male, 20, precontemplation). Participants were generally ambivalent about receiving posts on their Facebook walls about smoking (52% positive quotes, 35% negative, and 13 neutral), with specific concerns about repetition. For example, one participant noted “I’d ignore it if it was repetitive, the same info, the same picture, the same plot, but I guess there could be something different every time so you’re curious and want to click on it and read more” (female, 19, contemplation).
Participants were asked whether they would be interested in using other websites than Facebook to quit smoking. Comments tended to support Facebook as a more interesting and/or convenient approach to smoking cessation (51% of quotes supported using Facebook over other websites, 33% were partial to other websites, and 15% of quotes were ambivalent). For example, one participant noted, “If I did want to quit, I would go to other websites. They probably would not be as effective though, because they are not social networking sites where you can get immediate support from others” (male, 18, precontemplation). Another participant who was hesitant about using other websites said “I think that a website would be more impersonal than using FB. Using FB as a means to quit would be more beneficial since the social aspect is there” (male, 24, precontemplation).
In addition to valence codes for types of communication on Facebook, four unique themes were identified around using Facebook to quit smoking including social support, privacy, convenience of Facebook, and inconvenience of other websites (see Table 3 for theme counts, subthemes, and sample quotes).
Table 3.
Themes and sample quotes around using Facebook for smoking cessation
| Themes | Count/respondents | Subthemes (counts/respondents) | Sample Quote |
|---|---|---|---|
| Social support | 75/25 |
|
yes [I would be interested in a page that brought people together who are dealing with similar issues with smoking], then there would be a group of people in the same situation and that can sometimes help things (Positive) |
|
| |||
| Privacy | 48/20 |
|
are they degrees of privacy settings available?? not sure if i’d want everyone seeing that. some of my younger family doesnt kno i smoke and theyre parents are a little over protective. other ppl using the app might be ashamed as well (Concerned) |
| hm, not really [concerned about privacy]. You are all trying to achieve the same goal so you aren’t complete strangers (Not concerned) | |||
|
| |||
| Convenience of Facebook | 28/17 | if something was available on facebook and well designed, i would stick to just the facebook one, since i’m already on facebook, it’s one less thing to check and keep track off | |
|
| |||
| Inconvenience of other websites | 10/9 | Probably not [go to another website to get information about smoking], I would never get around to it. | |
Note. All quotes are reproduced exactly as written by respondents.
Social support was identified as a strength of a Facebook intervention. The shared experience of quitting was an important aspect of the support, with one participant noting “I enjoy the whole working as a team type environment. If there’s victory (quitting) in the end, we’re all satisfied” (male, 20, precontemplation). Negative comments about social support related to smoking being the focus of the social support. One participant noted, “I feel like forming a group centered solely around smoking would be a little uncomfortable” (male, 22, precontemplation).
Two major themes arose about the uniqueness of Facebook as a medium to deliver health behavior change intervention: convenience and privacy. Facebook was generally viewed as convenient. The ease of access to an intervention in addition to other social material was identified as a strength of Facebook. One participant noted “FB is just convenient because I’m there so often and updates to the page would be on my home page feed, so I could keep track of that as well as creep on my friends” (female, 22, preparation). Another participant referred to a Facebook intervention as “one stop shopping” because “they can socialize with friends, and work on quitting” (20, female, contemplation.” Many saw privacy as a concern, especially as it related to smoking behavior reported on Facebook. One participant with concerns said “One of the things that’s always hardest for me with quitting smoking is the outside pressure to quit, and I don’t want something spreading the information around about my cigarettes. I’d like to keep it a little more controlled and private” (male, 22, precontemplation). In contrast, those who did not have concerns were comfortable with the social nature of Facebook. One participant, though not currently motivated to quit smoking, stated “If I were quitting smoking, I wouldn’t care if it was the most public thing of my life. That’s not something worth keeping private. It’s something to be proud of” (male, 20, precontemplation).
Conclusion
Applying a mixed-methods approach, this study evaluated young adults’ receptivity to using Facebook for smoking cessation. Our findings indicated that a Facebook intervention could reach and appeal to young adult smokers across all smoking severities who use Facebook, though interest was greater among those more interested in quitting and with recent evidence of attempts to change or quit their smoking. The findings suggest the value of tailoring to readiness to quit in designing a Facebook intervention to appeal to the widest group of young adult smokers. Incentives for participation also may be useful to spur engagement and retention, as well as gaming activities and those that emphasize socializing.
Survey results and qualitative interviews yielded suggestions as to the most successful strategies for intervening with young adults using Facebook. An intervention designed directly through Facebook may reach more young adults than an application that would have to be installed due to privacy concerns. Some participants reflected concern about sharing information with a third party application. Further, apps are much less popular than Facebook itself, with the most popular app on Facebook used by about 2% of daily active users in February 2013,23, 50, and only a quarter of the sample in the present study being recent Facebook app users. An intervention through Facebook also was largely favored over using another website as it is already so well integrated into young adults’ lives. Specific strategies that were particularly appealing were personalized messages sent to participants and updating their Facebook status as a way to get support for quitting smoking. Participants emphasized that the intervention not be boring or repetitive. Thus, an intervention that varies the content and maximizes the supportive environment that social media can provide while giving participants opportunities to keep their disclosures private if they would like would be ideal. Private groups on Facebook made up of participants with similar smoking characteristics (e.g., severity, motivation to quit) could both support social interaction and respect privacy concerns. Although not mentioned often in qualitative interviews, survey data indicated that over half of participants used their cell phones to browse the Internet or update their Facebook social media status, indicating that a Facebook intervention should be fully accessible using mobile technology.
Consistent with previous findings that young adults can be engaged in online health behavior change interventions that are not delivered through social media,16, 17 our qualitative data showed some enthusiasm for using other websites than Facebook to quit smoking. However, very few (2%) respondents in our online survey had ever used the Internet to quit smoking. This is consistent with recent data that less than 1% of adult smokers in England had used the Internet to aid a quit attempt in the past year despite 47% reporting an interest in doing so.51 Consistent with our findings, adults who were more motivated to quit were also more likely to report an interest in using the Internet to quit smoking. Findings by Brown et al. and in the present study underscore the importance of using tailored outreach approaches to engage motivated smokers to participate in Internet interventions and to engage unmotivated smokers to quit. Bringing health promotion interventions to social media that is so well integrated into the daily lives of many young adults could be engaging.
There were some differences in the online behavior reported here compared to US data. Post-hoc comparisons were made between prevalence of various Internet and social media behaviors in our sample (smokers recruited through Facebook) to teen and adult surveys conducted by the Pew Internet and American Life Project using phone sampling.52, 53 Our sample showed higher prevalence than teens and lower prevalence than adults for using the Internet to get news, make online purchases, and look up health information, likely reflecting developmental differences in financial independence and health concerns. Our sample was more likely to use Twitter than the Pew samples of either teens or adults, and exhibited a greater range of social media behaviors than teens, suggesting that intervention strategies that incorporate multiple forms of social media and interaction tools may be particularly successful with young adult smokers. However, given that our survey used Facebook for recruitment, we are not able to generalize to the entire population of young adults in the United States.
This work on the literature suggests guidelines for developing successful online health promotion activities. A meta-analysis of 85 online interventions found those most successful were strongly based in theory and provided tailored messaging to individual audiences.54 Similarly, Fry and Neff found positive results through tailoring prompts through regular contacts with a counselor.55 Social media offers additional opportunity over traditional Internet platforms to interact over multiple channels, share messages with many different types of social networks, and is extremely engaging to users. Our work suggests that a Facebook intervention that tailors to motivation to quit while attending to protection of privacy is likely to maximize engagement.
Study limitations include the use of self-reported data that could be subject to recall bias. In addition, social media (and Facebook in particular) is changing rapidly such that new features of Facebook communication (e.g., posting on an individual’s timeline, increased ease of using video) and thus intervention have become available since the data were collected. We were not able to assess receptivity to some of these newer features of Facebook. Further, we acknowledge that although a sizable minority of young adults indicated an interest in using Facebook to change smoking behavior, formal study is needed to confirm to what extent young people would use and engage in a smoking cessation intervention through Facebook. Nonetheless, it is clear that there is interest in an intervention that uses Facebook for smoking cessation.
The present study demonstrates an interest in and provides a framework from which to develop a social media intervention for smoking cessation targeted to young adults. Social media intervention, methods to track its engagement and efficacy, and costs and benefits of this method as a health promotion tool are in their infancy.56 As such, this formative work is fundamental to broaden our understanding of what might work for whom. Then theory-based interventions can be most effectively adapted for delivery over the powerful tool that social media represents.
SO WHAT?
What is already known on this topic?
Young adults use social media more than any other age group. Social media websites such as Facebook have shown promise in changing health behavior. Yet little is know about how to engage young adults in a smoking cessation intervention using Facebook.
What does this article add?
In a mixed-methods design, we found young adults would be interested in a smoking cessation intervention using Facebook with recommendations that it be tailored to motivation to quit and provide options for keeping interactions private.
What are the implications for health promotion practice or research?
Social media presents a generally untapped strategy to help young adults quit smoking. Because young adults are less likely than other groups to take advantage of traditional smoking cessation aids, social media, including Facebook could be a means of reducing tobacco use among young people.
Acknowledgments
This study was supported by the National Institute on Drug Abuse (NIDA T32 DA007250, and the California Tobacco-Related Disease Research Program (TRDRP; 18FT-0055). The preparation of this manuscript was supported in part by NIDA (P50 DA009253, K23 DA032578), the National Institute of Mental Health (R01 MH083684), and the CA TRDRP (13-KT-0152).
We thank Christina Wa for coding the interviews.
References
- 1.Substance Abuse and Mental Health Services Administration. NSDUH Series H-46 HHS Publication No (SMA) 13-4795. Rockville, MD: Substance Abuse Mental Health Services Administration; 2013. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. [Google Scholar]
- 2.Curry SJ, Sporer AK, Pugach O, Campbell RT, Emery S. Use of tobacco cessation treatments among young adult smokers: 2005 National Health Interview Survey. American Journal of Public Health. 2007 Aug;97(8):1464–1469. doi: 10.2105/AJPH.2006.103788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bost ML. A descriptive study of barriers to enrollment in a collegiate health assessment program. Journal of Community Health Nursing. 2005;22(1):15–22. doi: 10.1207/s15327655jchn2201_2. [DOI] [PubMed] [Google Scholar]
- 4.Davies J, McCrae BP, Frank J, et al. Identifying male college students’ perceived health needs, barriers to seeking help, and recommendations to help men adopt healthier lifestyles. Journal of American College Health. 2000 May;48(6):259–267. doi: 10.1080/07448480009596267. [DOI] [PubMed] [Google Scholar]
- 5.Office of Disease Prevention and Health Promotion. Healthy People 2020 Objective Topic Areas and Page Numbers. Department of Health and Human Services; Rockville, MD: 2011. [Google Scholar]
- 6.Pew Internet & American Life Project. [April 30, 2013];Who’s Online: Internet User Demographics. Available at: http://www.pewinternet.org/Static-Pages/Trend-Data-(Adults)/Whos-Online.aspx.
- 7.Kramer JJ, Willemsen MC, Conijn B, van Emst AJ, Brunsting S, Riper H. Effectiveness of a web-based self-help smoking cessation intervention: protocol of a randomised controlled trial. BMC Public Health. 2009;9:32. doi: 10.1186/1471-2458-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eysenbach G. Issues in evaluating health websites in an Internet-based randomized controlled trial. Journal of Medical Internet Research. 2002;4(3):e17. doi: 10.2196/jmir.4.3.e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feil EG, Noell J, Lichtenstein E, Boles SM, McKay HG. Evaluation of an Internet-based smoking cessation program: Lessons learned from a pilot study. Nicotine & Tobacco Research. 2003;5(2):189–194. doi: 10.1080/1462220031000073694. [DOI] [PubMed] [Google Scholar]
- 10.Westmaas JL, Bontemps-Jones J, Bauer JE. Social support in smoking cessation: reconciling theory and evidence. Nicotine Tob Res. 2010 Jul;12(7):695–707. doi: 10.1093/ntr/ntq077. [DOI] [PubMed] [Google Scholar]
- 11.Cohen S, Lemay EP. Why would social networks be linked to affect and health practices? Health Psychol. 2007 Jul;26(4):410–417. doi: 10.1037/0278-6133.26.4.410. [DOI] [PubMed] [Google Scholar]
- 12.Huang GC, Unger JB, Soto D, et al. Peer Influences: The Impact of Online and Offline Friendship Networks on Adolescent Smoking and Alcohol Use. J Adolesc Health. 2013 Aug 28; doi: 10.1016/j.jadohealth.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Christakis NA. Health care in a web. British Medical Journal. 2008 Jun 28;336(7659):1468. doi: 10.1136/bmj.a452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cobb NK, Graham AL, Abrams DB. Social network structure of a large online community for smoking cessation. Am J Public Health. 2010 Jul;100(7):1282–1289. doi: 10.2105/AJPH.2009.165449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Simoni JM, Nelson KM, Franks JC, Yard SS, Lehavot K. Are peer interventions for HIV efficacious? A systematic review. AIDS Behav. 2011 Nov;15(8):1589–1595. doi: 10.1007/s10461-011-9963-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Klatt C, Berg CJ, Thomas JL, Ehlinger E, Ahluwalia JS, An LC. The role of peer e-mail support as part of a college smoking-cessation website. American Journal of Preventive Medicine. 2008 Dec;35(6 Suppl):S471–478. doi: 10.1016/j.amepre.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 17.An LC, Perry CL, Lein EB, et al. Strategies for increasing adherence to an online smoking cessation intervention for college students. Nicotine Tob Res. 2006 Dec;8(Suppl 1):S7–12. doi: 10.1080/14622200601039881. [DOI] [PubMed] [Google Scholar]
- 18.Burri M, Baujard V, Etter JF. A qualitative analysis of an internet discussion forum for recent ex-smokers. Nicotine Tob Res. 2006 Dec;8(Suppl 1):S13–19. doi: 10.1080/14622200601042513. [DOI] [PubMed] [Google Scholar]
- 19.van Mierlo T, Voci S, Lee S, Fournier R, Selby P. Superusers in social networks for smoking cessation: analysis of demographic characteristics and posting behavior from the Canadian Cancer Society’s smokers’ helpline online and StopSmokingCenter.net. J Med Internet Res. 2012;14(3):e66. doi: 10.2196/jmir.1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duggan M, Brenner J. The Demographics of Social Media Users - 2012. Washington, DC: Pew Internet & American Life Project; Dec, 2013. [Google Scholar]
- 21.Zickuhr K, Madden M. Older adults and internet use. Pew Internet & American Life Project; 2012. [Google Scholar]
- 22.Alexa. [February 21, 2013];Top sites in United States. Available at: http://www.alexa.com/topsites/countries/US.
- 23.Facebook. [September 30, 2013];Key Facts. Available at: http://newsroom.fb.com/Key-Facts.
- 24.Facebook. [February 13, 2013];truth. Available at: https://http://www.facebook.com/truthorange/likes.
- 25.Ramo DE, Prochaska JJ. Broad reach and targeted recruitment using Facebook for an online survey of young adult substance use. Journal of Medical Internet Research. 2012;14(1):e28. doi: 10.2196/jmir.1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pollick A. APS Observer. Vol. 23. American Psychological Society; 2010. Senate supports behavioral science in 2011. [Google Scholar]
- 27.Morris ME, Consolvo S, Munson SA, Kramer ADI, Patrick K, Tsai J. Facebook for health: Opportunities and challenges for driving behavior change. Paper presented at: 29th ACM Conference on Human Factors in Computing Systems; May, 2011; Vancouver BC, Canada. [Google Scholar]
- 28.Cavallo DN, Tate DF, Ries AV, Brown JD, Devllis RF, Ammerman AS. A social media-based physical activity intervention: A randomized controlled trial. American Journal of Preventive Medicine. 2012;43(5):527–532. doi: 10.1016/j.amepre.2012.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jones K, Baldwin KA, Lewis PR. The potential influence of a social media intervention on risky sexual behavior and Chlamydia incidence. Journal of Community Health Nursing. 2012;29:106–120. doi: 10.1080/07370016.2012.670579. [DOI] [PubMed] [Google Scholar]
- 30.Bull SS, Levine DK, Black SR, Schmiege SJ, Santelli J. Social media delivered sexual health intervention: A cluster randomized controlled trial. American Journal of Preventive Medicine. 2012;43(5):467–474. doi: 10.1016/j.amepre.2012.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Napolitano MA, Hayes S, Bennett GG, Ives AK, Foster GD. Using facebook and text messaging to deliver a weight loss program to college students. Obesity. 2013 Jan;21(1):25–31. doi: 10.1002/oby.20232. [DOI] [PubMed] [Google Scholar]
- 32.Benowitz NL. Pharmacology of nicotine: addiction, smoking-induced disease, and therapeutics. Annu Rev Pharmacol Toxicol. 2009;49:57–71. doi: 10.1146/annurev.pharmtox.48.113006.094742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.U. S. Public Health Service. A clinical practice guideline for treating tobacco use and dependence: A US Public Health Service report. The Tobacco Use and Dependence Clinical Practice Guideline Panel, Staff, and Consortium Representatives. JAMA. 2000;283(24):3244–3254. [PubMed] [Google Scholar]
- 34.Berg CJ, Lust KA, Sanem JR, et al. Smoker self-identification versus recent smoking among college students. Am J Prev Med. 2009 Apr;36(4):333–336. doi: 10.1016/j.amepre.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 35.Ramo DE, Hall SM, Prochaska JJ. Reaching young adult smokers through the Internet: Comparison of three recruitment mechanisms. Nicotine & Tobacco Research. 2010;12(7):768–775. doi: 10.1093/ntr/ntq086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O’Cathain A, Murphy E, Nicholl J. Integration and publications as indicators of “yield” from mixed methods studies. Journal of Mixed Methods Research. 2007;1(2):147–163. [Google Scholar]
- 37.Teddlie C, Tashakkori A. Major issues and controversies in the use of mixed methods in the social and behavioral sciences. In: Tashakkori A, Teddlie C, editors. Handbook of mixed methods in social & behavioral research. Thousand Oaks, CA: SAGE; 2003. pp. 3–50. [Google Scholar]
- 38.Mertens DM. Mixed methods and the politics of human research: The transformative-emancipatory perspective. In: Tashakkori A, Teddlie C, editors. Handbook of mixed methods in social & behavioral research. Thousand Oaks, CA: SAGE; 2003. pp. 135–166. [Google Scholar]
- 39.Ramo DE, Hall SM, Prochaska JJ. Reliability and validity of self-reported smoking in an anonymous online survey with young adults. Health Psychology. 2011 May 16;30(6):693–701. doi: 10.1037/a0023443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ramo DE, Liu H, Prochaska JJ. Reliability and validity of young adults’ anonymous online reports of marijuana use and thoughts about use. Psychology of Addictive Behaviors. 2011 doi: 10.1037/a0026201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.U. S. Census Bureau. [February 4, 2010];Census Regions and Division of the United States. Available at: http://www.census.gov/geo/www/us_regdiv.pdf.
- 42.Rural Health Research Center. Rural Urban Commuting Area Codes Data. [July 25, 2011];WWAMI Rural Health Research Center, Department of Family Medicine, University of Washington. Available at: http://depts.washington.edu/uwruca/ruca-data.php.
- 43.Hall SM, Tsoh JY, Prochaska JJ, et al. Treatment for cigarette smoking among depressed mental health outpatients: A randomized clinical trial. American Journal of Public Health. 2006 Oct;96(10):1808–1814. doi: 10.2105/AJPH.2005.080382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baker TB, Piper ME, McCarthy DE, et al. Time to first cigarette in the morning as an index of ability to quit smoking: implications for nicotine dependence. Nicotine and Tobacco Research. 2007 Nov;9(Suppl 4):S555–570. doi: 10.1080/14622200701673480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Prochaska JO, DiClemente CC. Stages and processes of self-change for smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology. 1983;51(3):390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 46.Lenhart A, Purcell K, Smith A, Zickuhr K. Social media and young adults. Washington, DC: Pew Research Center; Feb, 2010. [Google Scholar]
- 47.Pew Internet & American Life Project. Parent Teen Cell Phone Survey 2009. 2009 [Google Scholar]
- 48.Grbich C. Qualitative Data Analysis: An Introduction. Thousand Oaks, CA: SAGE; 2007. [Google Scholar]
- 49.ATLAS.ti Version 4.2 [computer program] Berlin: Scientific Software Development; 2008. Version. [Google Scholar]
- 50.AppData. Facebook Apps Leaderboard. [February 21, 2013]; Available at: http://appdata.com/leaderboard/apps?metric_select=dau_estimate&style=classic.
- 51.Brown J, Michie S, Raupach T, West R. Prevalence and characteristics of smokers interested in Internet-based smoking cessation interventions: Cross-sectional findings from a national household survey. J Med Internet Res. 2013;15(3):e50. doi: 10.2196/jmir.2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Princeton Survey Research Associates International. 2009 Parent-Teen Cell Phone Survey Topline. Pew Internet & American Life Project; Oct 1, 2009. [Google Scholar]
- 53.Princeton Survey Research Associates International. Spring Change Assessment Survey 2010 Topline. Pew Internet & American Life Project; Jun 4, 2010. [Google Scholar]
- 54.Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res. 2010;12(1):e4. doi: 10.2196/jmir.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fry JP, Neff RA. Periodic prompts and reminders in health promotion and health behavior interventions: systematic review. J Med Internet Res. 2009;11(2):e16. doi: 10.2196/jmir.1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Korda H, Itani Z. Harnessing social media for health promotion and behavior change. Health Promot Pract. 2013 Jan;14(1):15–23. doi: 10.1177/1524839911405850. [DOI] [PubMed] [Google Scholar]


