Abstract
Objective
To calculate the effect of Reiki therapy for pain and anxiety in randomized clinical trials.
Data Sources
A systematic search of PubMed, ProQuest, Cochrane, PsychInfo, CINAHL, Web of Science, Global Health, and Medline databases was conducted using the search terms pain, anxiety, and Reiki. The Center for Reiki Research was also examined for articles.
Study Selection
Studies that used randomization and a control or usual care group, used Reiki therapy in one arm of the study, published in 2000 or later in peer-reviewed journals in English, and measured pain or anxiety were included.
Results
After removing duplicates, 49 articles were examined and 12 articles received full review. Seven studies met the inclusion criteria: four articles studied cancer patients; one examined post-surgical patients; and two analyzed community dwelling older adults. Effect sizes were calculated for all studies using Cohen’s d statistic. Effect sizes for within group differences ranged from d=0.24 for decrease in anxiety in women undergoing breast biopsy to d=2.08 for decreased pain in community dwelling adults. The between group differences ranged from d=0.32 for decrease of pain in a Reiki versus rest intervention for cancer patients to d=4.5 for decrease in pain in community dwelling adults.
Conclusions
While the number of studies is limited, based on the size Cohen’s d statistics calculated in this review, there is evidence to suggest that Reiki therapy may be effective for pain and anxiety. Continued research using Reiki therapy with larger sample sizes, consistently randomized groups, and standardized treatment protocols is recommended.
Introduction
The use of complementary and alternative medicine (CAM) techniques is growing in popularity with the public. CAM modalities are often either lauded or debunked in the popular press and the scientific community based on the evidence of one study. Reiki therapy, a form of biofield energy has been examined with community dwelling older adults, specific disease conditions such as cancer, chronic fatigue, diabetic neuropathy, surgical patients, and others. The objective of this review is to determine if Reiki therapy is effective for pain and anxiety in adults and to calculate the effect sizes for Reiki therapy in randomized clinical trials. Moreover, this review considers the use of Reiki therapy for pain and anxiety in adults and seeks to discover if Reiki therapy is effective for these conditions based on current evidence.
There is a lot of confusion around what Reiki therapy is. From a practical standpoint, Reiki therapy is a way for the practitioner to guide energy to the recipient, to assist the innate healing energy of the recipient and facilitate self-healing (National Center for Complementary and Alternative Medicine, 2012a). The practitioner does not cause the healing, nor are they the source of the energy. The practitioner is a channel for the energy, much like a garden hose is a channel for water. Many call this energy universal, but some say it is from God, Buddha, or a sacred source. A common interpretation for the word Reiki is spiritually guided life force energy (Rand, 2005).
There are several versions regarding the origins of Reiki therapy. It is generally accepted that Reiki therapy began with Dr. Mikau Usui, a spiritual seeker who undertook a 21 day penance and fast on Mount Kurama in Japan (Miles, 2008). Usui experienced the Reiki energy on the 21st day and was healed. He brought the technique to his family and subsequently opened a clinic in order to treat the public. Usui taught Reiki therapy level one to many people and taught several students the master/teacher level (Rand, 2005). Usui taught Reiki therapy as part of a spiritual practice, but not as a religion (Miles, 2008). As Reiki therapy evolved and came to the West, the hands-on healing practices came to the fore and the spirituality piece of the practice faded. There are three degrees or levels of Reiki practice. First degree practitioners are able to treat themselves or others through light touch (Miles & True, 2003). This level of Reiki is suitable for anyone from school aged children to the very old. Second degree Reiki expands practice to the use of distance healing: the practitioner may send Reiki energy to the next room or around the world (Rand, 2005). Third degree or master level Reiki expands Reiki practice to teaching and initiating others into Reiki and involves extensive practice.
A typical Reiki therapy session may last from 30 to 90 minutes. Ideally, the recipient lies comfortably on a massage table fully clothed and the practitioner places their hands lightly on the body in a set sequence of hand positions. Most people leave a Reiki therapy session feeling very relaxed. A qualitative study found that during a Reiki treatment participants felt “dreamy,” “safe,” “secure,” and “more grounded” (Ring, 2009, p. 255). A study of nurses who use Reiki therapy for self-care found that the nurses used Reiki therapy during their workday to feel more calm, centered, and more able to care for others (Vitale, 2009).
The National Center for Complementary and Alternative Medicine (NCCAM) places Reiki therapy in the in the category of biofield energy. Biofield energy is any electrical or magnetic field produced by a biological organism, e.g. a human. The human body produces measurable electrical and magnetic fields. The heart produces an electrical field to regulate its beat: This electrical signal is measured through an electrocardiogram (ECG or EKG), a common medical test. The brain also produces an electrical field but at a much lower level than the heart. In fact, every cell in the human body produces minute amounts of electricity, a magnetic field, has a positive charge on the outer cell wall, and a negative charge on the inner cell wall (Dale, 2009). Electrical fields produce magnetic fields with a stronger electrical field producing a stronger magnetic field (Rae, 2005; Thomas, 2012). A magnetic resonance imaging (MRI) scan uses the body’s own magnetic field (along with a strong magnet and radio waves that are emitted from the machine) to produce sharp images of soft tissue within the body (Berger, 2002). Classic Newtonian physics experiments have shown how waves interact with each other: Depending on the pattern, some waves are enhanced and some are cancelled (Figure 1). The interference pattern between two human magnetic fields may explain some of the results that any touch therapy creates.
Figure 1.
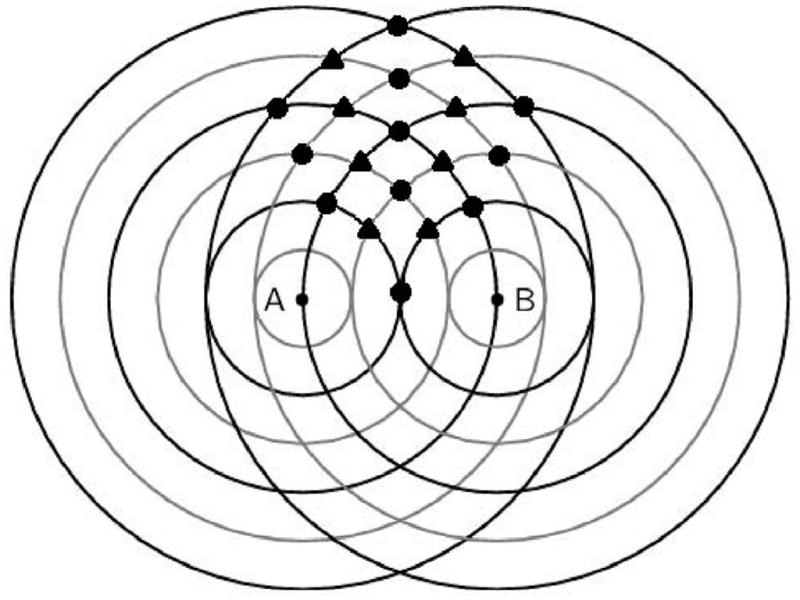
Wave interference pattern. “A” and “B” are two people standing near each other. The black lines are peaks and the grey lines are troughs. The circles indicate areas where the two waves enhance one another (either higher peak or lower trough). The diamonds indicate areas where the two waves cancel each other.
The theory of quantum physics may hold promise in the future explanation of the mechanisms of Reiki. Although no verified theory exists that explains how Reiki therapy (or any biofield energy therapy) works, there may be a scientific explanation for Reiki therapy to be found in quantum physics, a branch of physics that was first discovered in the 1800’s and studies extremely small particles (electrons, photons, and the like) that do not behave in a predictable way. Quantum physics studies these particles and attempts to describe the interactions of energy and matter. Physicists have found that very tiny particles have some very curious properties: Not only can these tiny particles be in more than one place at once, some theorists say they have to be in more than one place at the same time (Rosenblum & Kuttner, 2006). The Nobel Prize in Physics for 2012 was won by two scientists who were each able to detect a particle being in two places at the same time (Nobelprize.org, 2012). Biofield energy may be gathered and directed by the practitioner to the recipient as explained by quantum physics, e.g., thought produces change in how the particles work (Rosenblum & Kuttner, 2006). Distance healing may be explained by energy particles being simultaneously present at the location and time of the Reiki practitioner and the location and time of the recipient through the intention of the Reiki practitioner.
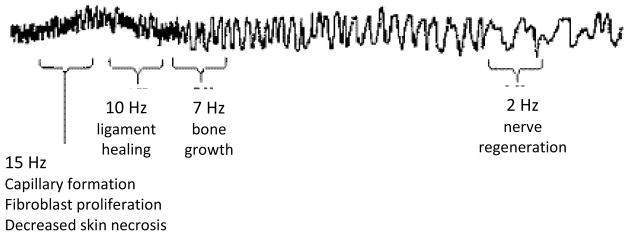
These particles by definition are difficult to measure but beginning in the 1960’s scientists began measuring the biomagnetic field coming from the human heart that is believed to extend beyond the body (see Figure 2). In the 1990’s Dr. John Zimmerman was able to measure a biomagnetic field coming from a healing practitioner’s hands (see Figure 3) with a device called a superconducting quantum interference device (SQUID). A few years later a Japanese team measured a biomagnetic field emanating from the hands of practitioners of yoga, meditation, Qigong and similar modalities (Oschman, 2000). These electromagnetic signal pulses varied from 0.3 to 30 Hertz (cycles per second). Device-generated pulsed electromagnetic fields (PEMF) have been effective for bone stimulation, stroke rehabilitation, decreased postoperative pain, and other applications (Abo et al., 2012; Heden & Pilla, 2008; Kondo et al., 2013). Transcutaneous electrical nerve stimulation (TENS) units are a well-known example of an adjustable pulsed electromagnetic field that is used to decrease chronic pain. Although it may be difficult to imagine tiny particles that react to human thought, scientific experiments have shown this phenomenon to be true for some time now (Rae, 2005). The similarities between human-generated biomagnetic energy such as Reiki therapy and device-generated electromagnetic fields for healing seem clear. The measurement of human biofield energy demonstrates the existence of human-generated biomagnetic energy. The similarities in the behavior of quantum particles and Reiki energy require more study, however repeated physics experiments with thought-driven particles united with the measurement of human biofield energy suggests that Reiki energy may consist of quantum particles that may lead to a validated theory of Reiki therapy.
Figure 2.
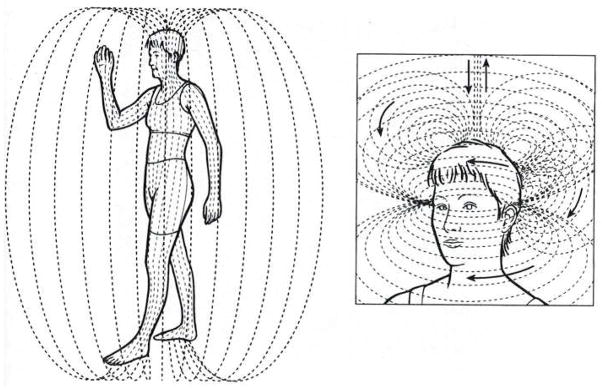
Human biofield as it extends outside the body. Reprinted from Energy Medicine: The Scientific Basis, Oschman, J. L Polarity, therapeutic touch, magnet therapy, and related methods, p. 77, Copyright Elsevier Limited (2000), with permission from Elsevier
Figure 3.
Signal recorded from the hands of a therapeutic touch practitioner on the SQUID device. Reprinted from Energy Medicine: The Scientific Basis, Oschman, J. L. Polarity, therapeutic touch, magnet therapy, and related methods, p. 87, Copyright Elsevier Limited (2000), with permission from Elsevier
Significance
Pain is a very common symptom. Approximately 100 million Americans suffer from chronic pain (Institute of Medicine, 2011). Additionally, millions of people suffer from acute pain (pain that lasts for 6 months or less) such as people with cancer, trauma or surgical patients, and other everyday events such as a sprained ankle or a stubbed toe. Anxiety is a state that may accompany many of the conditions that cause pain such the diagnosis of a serious illness like cancer or heart disease.
Very few high-quality studies have been done exploring Reiki therapy for pain and anxiety. Despite the lack of evidence, articles are published in peer reviewed journals giving anecdotal evidence for the effectiveness of Reiki therapy citing the few studies that have been published (Hurvitz, Leonard, Ayyangar, & Nelson, 2003; Rand, 2011). While there have been a total of four review articles published examining Reiki therapy in clinical trials (Jain & Mills, 2010; Lee, Pittler, & Ernst, 2008; vanderVaart, Gijsen, de Wildt, & Koren, 2009; Vitale, 2007), none have focused exclusively on pain and anxiety and none report effect sizes for study variables.
Search Strategy and Inclusion Criteria
A systematic search was conducted using PubMed, ProQuest, Cochrane, PsychInfo, CINAHL, Web of Science, Global Health, and Medline databases in addition to the Center for Reiki Research (The International Center for Reiki Training, 2012). The following keywords were used: pain, anxiety, and Reiki. The last search was run on April 4, 2012. After removing duplicates there were 49 articles: 17 review articles, 6 informational articles, 1 study that reported on the prevalence of CAM use that included Reiki, 6 qualitative studies, 1 dissertation, and 18 studies of any type, any year.
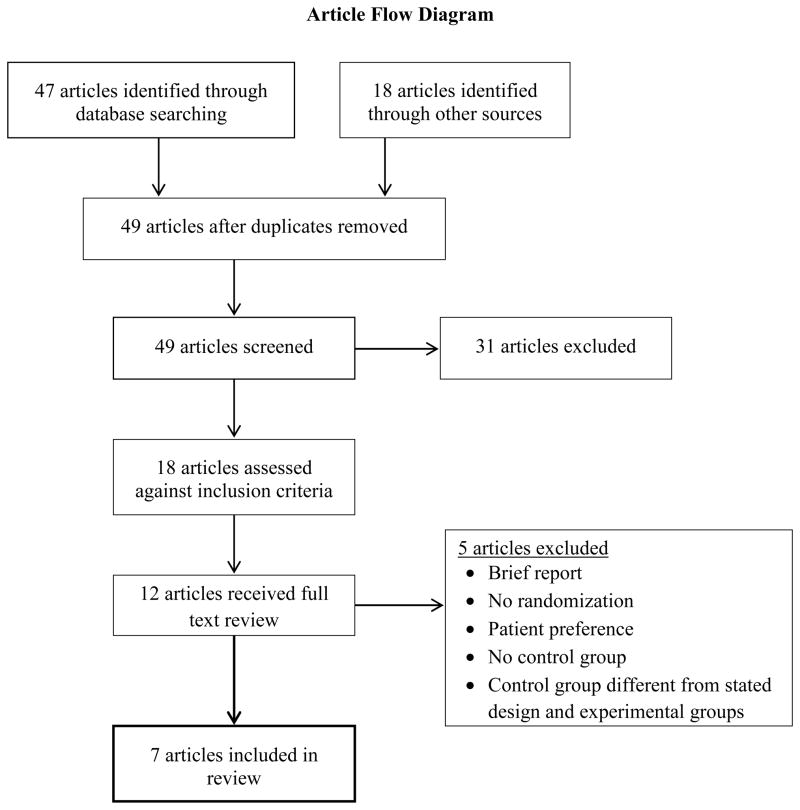
Studies that include Reiki therapy as an intervention are scarce. To present the best evidence, articles were included in the review if they (a) used Reiki therapy as one arm of the study, (b) used randomization with a control or usual care group, (c) were published in peer-reviewed journals, (d) measured either pain or anxiety, (e) published in 2000 or later, and (e) were published in English. After evaluating the 18 studies against inclusion criteria, 12 studies remained for full review (see Figure 4).
Figure 4.
Article flow diagram.
Method of Review and Data Extraction
Each of the 12 studies selected for full text review was carefully evaluated by both authors against the inclusion criteria. Five of the 12 did not fully meet the inclusion criteria. One article was a one-page preliminary report (Miles, 2003), a second used a convenience sample with no randomization or control (Birocco et al., 2011), a third used a semi-randomized patient preference design (Hulse, Stuart-Shor, & Russo, 2010), a fourth used a four-group design with a combination of Reiki and sham Reiki and no control (Assefi, Bogart, Goldberg, & Buchwald, 2008) and the fifth included a control group that was different from the stated design and the two experimental groups (Park, McCaffrey, Dunn, & Goodman, 2011). The remaining seven studies met the inclusion criteria for review as determined by both authors (Beard et al., 2011; Gillespie, Gillespie, & Stevens, 2007; Olson, Hanson, & Michaud, 2003; Potter, 2007; Richeson, Spross, Lutz, & Peng, 2010; Tsang, Carlson, & Olson, 2007; Vitale & O’Connor, 2006) (see Table 1).
Table 1.
Summary of Reiki studies
| Authors/Journal/Year | Purpose of Study | Outcomes Measured/Length of Intervention | Study Design | Population/Sample | Significant Results (Within& Between#) | Effect Sizes: Within& Between# |
|---|---|---|---|---|---|---|
|
| ||||||
| Beard, C. Stason, W. B. Wang, Q. Manola, J. Dean-Clower, E. et al. Cancer, 2011 | Examine the clinical effects of RRT and Reiki v. control |
Anxiety Reiki: twice per week for 8 weeks for 50 minutes |
3 group RCT
|
Prostate Cancer: 54 adult males, mean age 64 years (range 46–91), 91% white |
↓ Anxiety for RRT (p=.02) | d=.55& |
|
| ||||||
| ↓ Anxiety for Reiki (p=.10) | d=.39& | |||||
|
| ||||||
| RRT: Reiki (p=.02) | d=.57# | |||||
|
| ||||||
| RRT: Control (p=.01) | d=.62# | |||||
|
| ||||||
| Olson, K. Hanson, J. Michaud, M. Journal of Pain and Symptom Management, 2003 | Determine whether Reiki + standard opioids resulted in better pain control, less analgesic use and improved QOL when compared to opioid + rest |
Pain Reiki treatments on days 1 and 4 of a 7 day trial for 90 minutes |
Randomized to either Reiki or rest group | Cancer, primarily solid tumor: 24 adults, mean age 59.5 years, 63% female |
Reiki: Rest Day 1: ↓ Pain (p=.035) |
d=.64# |
|
| ||||||
| Day 4: ↓ Pain (p=.002) |
d=.93# |
|||||
|
| ||||||
| Tsang, K. L., Carlson, L. E., Olson, K. Integrative Cancer Therapies, 2007 | Examine the effects of Reiki on fatigue, pain, anxiety, and overall quality of life in cancer patients who had recently completed chemotherapy treatment |
Pain, Anxiety Reiki tx for 5 consecutive days followed by a 1 week washout then 2 Reiki tx the following week (3 weeks total) for 45 minutes |
Random crossover | Cancer: 16 adults ages 33 to 84 (mean 59, SD=15.23) 81% female, 75% white, 13% Asian, 12% other with a diagnosis of colorectal (63%), breast (13%), gastric (12%), or lung (12%) cancer |
Pre first Reiki session to post last Reiki session: ↓ Pain (p<.05) |
d=.76& |
|
| ||||||
| ↓ Anxiety (p<.005) | d=.83& | |||||
|
| ||||||
| Reiki: Rest (Day 1 → Day5) Pain |
d=.32# |
|||||
|
| ||||||
| Anxiety (no p values given) |
d=.64# | |||||
|
| ||||||
| Potter, P. J. Journal of Holistic Nursing, 2007 | Determine feasibility of testing Reiki for women undergoing a breast biopsy |
Anxiety 1 Reiki tx within 7 days prior to biopsy, 1 Reiki tx within 7 days after biopsy for 50 minutes |
Randomized to either Reiki or usual care | Possible breast cancer: 32 women, ages 37 to 75 years |
Reiki: HADS (Anxiety) | d=.24& |
|
| ||||||
| STAI | d=.27& | |||||
|
| ||||||
| Usual: HADS (Anxiety) | d=.24& | |||||
|
| ||||||
| STAI No significant differences in between group means. |
d=.49& | |||||
|
| ||||||
| Vitale, A. T., O’Connor, P. C. Holist Nursing Practice, 2006 | Compare levels of pain and state anxiety in women after abdominal hysterectomy |
Pain, Anxiety Reiki txs immediately pre-op, 24 hours and 48 hours post-op for 30 minutes |
Randomized to either Reiki or usual care group | Post-hysterectomy: 22 women ages 40 to 73 years (mean=47, SD=6.5) |
Reiki: Usual Care ↓ Pain at 24 hours (p=.04) |
d=.79# |
|
| ||||||
| ↓ Anxiety (p=.005) | d=1.36# | |||||
|
| ||||||
| ↓ Pain medication ↓ Dilaudid T2 (p=.001) |
d=1.82# |
|||||
|
| ||||||
| ↓ Dilaudid T3 (p=.007) | d=1.29# | |||||
|
| ||||||
| ↓ Toradol T6 (p=.04) | d=.81# | |||||
|
| ||||||
| Gillespie, E. A. Gillespie, B. W. Stevens, M. J. Diabetes Care, 2007 | Assess the effectiveness of Reiki therapy to alleviate pain and improve mobility in subjects with Type 2 diabetes and PDN |
Pain 12 week intervention—2 tx first week than once weekly for 25 minutes |
3 group RCT
|
Type 2 Diabetes 160 adults, mean age 65, 61% male |
Reiki group ↓ total pain (p=.002) |
Pre/post d=.36& |
|
| ||||||
| Sham Reiki ↓ total pain (p=.039) |
d=.26& |
|||||
|
| ||||||
| Usual care ↓ total pain (p=.622) No significant differences between groups for total pain. |
d=.17& |
|||||
|
| ||||||
| Richeson, M. E., Spross, J. A. Lutz, K. Research in Gerontological Nursing, 2010 | Evaluate the effect of Reiki as an alternative and complementary approach to treating community- dwelling adults who experience pain, depression, and/or anxiety |
Pain, Anxiety Reiki tx once per week for 8 weeks for 45 minutes |
Randomized to either experiment or wait list control group | Community-dwelling: 20 Adults ages 57 to 76 (mean age 63.8 (SD=4.9), 60% female |
Reiki group ↓ Pain (p=.0078) |
d=2.08& |
|
| ||||||
| ↓ Anxiety (p=.0005) | d=.51& | |||||
|
| ||||||
| Control group ↑ Pain (p=.0156) |
d= −2.08& |
|||||
|
| ||||||
| ↑ Anxiety (p=.0313) | d= −.55& | |||||
|
| ||||||
| Reiki: Control Pain |
d= 4.5# |
|||||
|
| ||||||
| Anxiety | d= .75# | |||||
Data were extracted from each study including: (a) sample population (disease process, gender, mean age, and race if available), (b) study design, (c) outcome measures for anxiety or pain or both and (d) statistical significance for within group and between group differences including p values, means, standard deviations, and z values for calculating Cohen’s d statistic for effect sizes.
Findings
Sample sizes for the seven studies included in this review ranged from 16 to 160 participants (median = 24) for a total of 328 participants. There were 48% women and the mean age for the overall sample was 63 years old. Only two studies mentioned race. Beard et al. (2011) had 91% white participants but did not say how the remaining 9% of the participants identified themselves. Tsang et al. (2007) reported 75% white, 13% Asian, and 12% other participants.
The seven studies (see Table 1) included in the review examined a variety of populations: three studied cancer patients (Beard et al., 2011; Olson et al., 2003; Tsang et al., 2007), two tested Reiki therapy in a surgical setting (Potter, 2007; Vitale & O’Connor, 2006), and two looked at Reiki therapy in adults living in the community (Gillespie et al., 2007; Richeson et al., 2010). The results from each individual study may be found in Table 2.
Table 2.
Summary of Results: Reiki therapy and control groups
| Author (year) | Reiki therapy N | Mean (SD) | Sham Reiki, Usual Care, Waitlist Control, or Other | Mean (SD) |
|---|---|---|---|---|
|
Beard (2011) Mean diff, no SD |
N=16 | −4, | RRT: N=16 | RRT: −8 |
| Anxiety | Control: N=16 | Control: −1 | ||
|
| ||||
|
Olson (2003) Mean diff, no SD |
N=11 | −1.5 (Day 4) | Usual: N=13 | −0.1 (Day 4) |
| Pain | ||||
|
| ||||
|
Tsang (2007) Crossover study |
N=16 | Day 1 to Day 5 | N=16 | Day 1 to Day 5 |
| Pain | −1.33(1.54) | Pain | −0.53(3.14) | |
| Anxiety | −1.86(2.68) | Anxiety | −0.43(1.65) | |
|
| ||||
| Potter (2007) | N=17 | T1=7.29(4.80) | N=15 | T1=8.27(5.16) |
| Anxiety | T3=6.18(4.60) | Anxiety | T2=5.73(5.15) | |
|
| ||||
| Vitale (2006) | N=10 | 24h post-surgery | N=12 | 24h post-surgery |
| Pain | 3.8(2.4) | Pain | 5.4(1.4) | |
| Anxiety | At discharge 27(7.05) | Anxiety | At discharge 38(9.64) | |
|
| ||||
|
Gillespie (2007) Mean diff (0–78) |
N=76 | Sham, N=66 | 2.3(8.8) | |
| Pain | 2.9(7.9) | Usual Care N=18 | 1.8(15) | |
|
| ||||
| Richeson (2010) | N=12 | N=8 | ||
| Pain | Pre=4.8(1.3) Post=2.2(1.2) |
Pain | Pre=5.0(1.3) Post=7.6(1.2) |
|
| Anxiety | Pre=25.2(14.4) Post=17.5(15.5) |
Anxiety | Pre=21.2(12.9) Post=28.5(13.5) |
|
Study Design and Comparison Groups
All studies in this review used randomization as specified in the inclusion criteria. Three studies used a two group design with the control group utilizing either usual care (Potter, 2007; Vitale & O’Connor, 2006) or wait list control (Richeson et al., 2010). Olson et al. (2003) used a rest period equal to the Reiki therapy intervention as the control group and Tsang et al. (2007) used a random crossover design. Two studies used a three group design. Beard et al. (2011) explored Reiki therapy as compared to Relaxation Response Therapy (RRT) and a wait list control while Gillespie, et al. (2007) explored Reiki and sham Reiki compared to usual care. In sham Reiki, an actor performs the same treatment sequence as the real Reiki practitioner, but with no Reiki energy.
Variables and Measures
Three of the studies examined both pain and anxiety (Richeson et al., 2010; Tsang et al., 2007; Vitale & O’Connor, 2006). Two studies considered just pain (Gillespie et al., 2007; Olson et al., 2003) and two only evaluated anxiety (Beard et al., 2011; Potter, 2007). There were a variety of validated measures used.
Anxiety
Three studies chose the Spielberger State Anxiety Inventory (STAI) (Spielberger, Gorsch, Lushene, Vagg, & Jacobs, 1983) to measure anxiety (Beard et al., 2011; Potter, 2007; Vitale & O’Connor, 2006). The STAI scale was originally created to measure anxiety in adolescents with cancer but has been well validated in adults. Tsang et al. (2007) used the Edmonton Symptom Assessment System (ESAS) questionnaire (Chang, Hwang, & Feuerman, 2000) a validated nine symptom visual analog scale to measure anxiety. Potter also used the Hospital Anxiety and Depression Scale (HADS) (Zigmund & Snaith, 1983), because it recognizes anxiety in populations suffering from physical symptoms as a result of their disease. Richeson et al. (2010) used the HAM-A rating scale which exhibits high reliability and internal consistency (Cronbach’s alpha = .85, r=.23, p<.05) (Diefenbach et al., 2001).
Pain
Two studies used an 11-point Visual Analog Scale (VAS) (Olson et al., 2003; Vitale & O’Connor, 2006) to measure pain. Olson also used an unspecified “Likert” scale to measure pain. Tsang et al. also employed the ESAS questionnaire mentioned above to evaluate pain. Gillespie et al. (2007) used The McGill Pain Questionnaire (Melzack, 1975) to evaluate pain in patients with painful diabetic neuropathy. Richeson et al. utilized the faces pain scale originally developed for children but has been shown to be effective in older adults as well (A. G. S. Panel on Persistent Pain in Older Persons, 2002).
Outcomes and Effect Sizes
All but one study included in this review achieved at least one statistically significant result on the outcome variables of interest for the Reiki therapy intervention. Effect sizes were calculated using standard equations and were measured using the Cohen’s d statistic. Effect sizes for the Reiki therapy intervention ranged from small (d=.28) to very large (1.82).
Anxiety
While investigating Reiki therapy and relaxation response therapy compared to wait-list control for men with prostate cancer receiving radiation therapy, Beard et al. (2011) found a within group decrease in anxiety for relaxation response therapy (RRT) with a medium effect size (p=.02, d=.55) and non-significant within group decrease in anxiety for Reiki therapy with a small effect size (d=.39). The between group differences of RRT compared to Reiki therapy resulted in a significant difference between RRT and Reiki therapy (p=.02, d=.57) and between RRT and control (p=.01, d=.62) both in favor of the RRT intervention. Working with cancer patients who had recently completed chemotherapy treatment, Tsang et al. (2007) found within group differences for a decrease in anxiety (p<.005) and a large effect size (d=.83) for subjects in the Reiki therapy treatment arm when measured prior to the first Reiki therapy treatment, compared with following the last Reiki therapy treatment in a group of cancer patients on standard opioid therapy. When comparing Reiki therapy versus rest for between group differences, there was a medium effect size (d=.64) when calculated using means and standard deviations. Potter (2007) found a non-significant within group decrease in anxiety with a small effect size for the HADS anxiety subscale for both the Reiki therapy intervention (d=.24) and the usual care group (d=.24) and for the STAI measure for the Reiki intervention (d=.27) and the usual care group (d=.49) when exploring the use of Reiki therapy for women undergoing a breast biopsy. There were no between group differences when comparing the Reiki therapy intervention to usual care. In an investigation of women undergoing hysterectomy, Vitale et al. (2006) found a significant between group decrease in anxiety (p=.005) and a large effect size (d=1.36) just before discharge from the hospital. Richeson et al. (2010) found a significant decrease in anxiety (p=.0005) and a large effect size (d=2.08) within the Reiki therapy intervention and a significant increase in anxiety (p=.0313) and a large effect size (d= −.208) within the control group while investigating the use of Reiki therapy with community-dwelling older adults. When calculating between group differences post Reiki therapy intervention, there was a very large between group difference when comparing the Reiki therapy group to the control group (d= −4.5).
Pain
A Reiki therapy intervention used with cancer patients found a significant between group decrease in pain (p=.035) and a medium effect size (d=.64) on day one of the intervention and a significant between group decrease in pain (p=.002) and a large effect size (d=.93) for opioids plus Reiki therapy when compared to opioids plus rest on day four of the intervention (Olson et al., 2003). Cancer patients in the Tsang et al. study who had recently completed chemotherapy realized a significant decrease in pain (p<.05) and a medium effect size (d=.76) for within group measures when comparing scores from before the first Reiki treatment to after the final Reiki treatment. When comparing between group scores for Reiki therapy versus rest, the Reiki therapy group realized a small effect size (d=.32) when calculated using means and standard deviations (Tsang et al., 2007). When Vitale and O’Conner (2006) investigated the effect of Reiki therapy on pain in women post hysterectomy, the study found a significant between group decrease in pain at 24 hours post-surgery (p=.04) and a borderline large effect size (d=.79). Of equal interest, comparing the Reiki therapy and usual care groups, the women in the Reiki therapy intervention took less pain medication at T2 (p=.001, d=1.82), T3 (p=.007, d=1.29), and T6 (p=.04, d=.81) with large to very large between group effect sizes. In a study to explore the effect of Reiki and sham Reiki compared to usual care for painful diabetic neuropathy, Gillespie et al. (2007) found that Reiki and sham Reiki resulted in a within group decrease in pain (p=.002 and p=.039 respectively) and a small effect size (d=.36 and d=.26 respectively) while the usual care group had a non-significant within group decrease in pain and a very small effect size (p=.622, d=.17). There were no between group differences in total pain. Comparing a Reiki therapy intervention with a wait list control group of community dwelling older adults, there was a significant within group decrease in pain (p=.0078) and a large effect size (d=2.08) and a significant within group increase in pain (p=.0156) and a large effect size (d= −2.08) for the wait list control group (Richeson et al., 2010). Because of the decrease in pain for the Reiki therapy group and corresponding increase in pain for the control group, the calculated effect size for the between group difference was very large (d=4.5).
Discussion
Reiki therapy has been explored in a variety of populations including cancer patients, community dwelling adults, surgical patients and more.. The studies included in this review exhibit design flaws common to research involving complementary therapies. The most obvious difficulty is sample size. The median number of study participants was 24 (range of 16 to 160 participants). It is difficult to make generalizations to a population, even a limited one such as adults with cancer utilizing such small sample sizes. Moreover, acquiring these samples may take months to years. For example, Beard et al. took 22 months to recruit 54 subjects and Potter required 15 months to recruit 32 subjects. The length of recruitment time creates difficulties if a longitudinal design would be more appropriate. Olson et al. and another that did not meet the inclusion criteria had difficulty recruiting subjects and in fact took two years to recruit 24 adults because the subjects stated they would not participate unless they could be in the Reiki therapy group. Gillespie et al. also had to limit the control group due to high attrition.
Length of intervention may have been problematic for some study outcomes. Although Olsen et al. was able to show a significant reduction in pain and a medium effect size for the Reiki treatment group (p=.035, d=.64) on day one and significant reduction in pain and a large effect size on day four (p=.002, d=.93), the intervention consisted of only two Reiki treatments four days apart. It seems possible that if the study had lasted several weeks they may have seen the decrease in medication usage that they were looking for. Another study that may have benefitted from a longer intervention time was Gillespie et al. when they examined Reiki therapy for reduction in pain in diabetic subjects with painful diabetic neuropathy (PDN). Although this was one of the longer interventions (12 weeks total), PDN is not an easy condition to treat and does not respond well to medications. While the intervention did achieve a statistically significant decrease in pain for the Reiki group (p=.002, d=.36), the effect sizes were not very different for the sham Reiki group (p=.039, d=.26) leading the authors to question the clinical significance. Possibly if the intervention had run 26 weeks or longer, the authors may have been able to detect a difference between the Reiki group and the sham Reiki group.
Timing of interventions can also be important to success. For example in the Reiki therapy intervention for breast biopsy, the pre-biopsy intervention was given within seven days prior to the biopsy and the post-biopsy intervention was given within seven days post biopsy. The study author admitted that the timing was for subject convenience and that an intervention “within the clinical setting might more effectively mitigate a crisis response” (Potter, 2007, p. 246). In contrast, Vitale et al. timed the Reiki therapy intervention around abdominal hysterectomy in a way that makes more sense: just prior to surgery, then 24 and 48 hours post-surgery. This timing resulted in a significant decrease in both pain and medication usage.
Most studies included in this review used a standardized protocol of timing and hand positions. However, these protocols differed significantly from study to study. Reiki treatment times varied from 25 minutes in the diabetic neuropathy study (Gillespie et al., 2007) to 90 minutes in the Reiki therapy plus opioid use in cancer patients study (Olson et al., 2003). The average treatment length was 48 minutes. All but one study used a set protocol for treatment hand positions. Richeson et al. allowed the treatments to be patient specific rather than follow a particular hand placement and timing protocol, making it difficult to compare subjects to each other much less compare between studies.
Suggestions for Future Research
Based on the findings of this review it may be helpful if future Reiki therapy studies consider the following design strategies. First, in order to be able to conform to scientific research standards, a three arm design which includes a Reiki intervention, a sham Reiki intervention (placebo), and a non-intervention control group seems most effective. Having a sham Reiki group allows for investigators to take into account and control for the therapeutic effect of attention and potential effect of human interaction. It has been shown that any touch therapy, even a sham intervention produces an effect on subjects as demonstrated by several of the studies in this review. Reiki interventions need to show significantly better results than the sham group in order to overcome the “placebo effect.” It is suggested that effect sizes be calculated and reported in articles so that readers may understand and compare the effect of the interventions. Second, in order to combat the reluctance of subjects to participate in complementary research, a crossover design is suggested. In this way, control subjects know that they will receive the intervention either now, or in the near future. Studies that use a crossover design seem to have fewer issues with control groups (Post-White et al., 2009; Tsang et al., 2007). Third, a standardized protocol of intervention length and hand positions seems essential. It is difficult to compare subjects who have not utilized the same treatment protocol. Fourth, researchers need to consider whether Reiki therapy is appropriate for a particular condition, and what the optimal timing of the intervention may be. For example, the timing of the Reiki treatments used in the abdominal hysterectomy study (Vitale & O’Connor, 2006) consisting of immediately before surgery then 24 and 48 hours after surgery was well considered and makes sense.
Another possible avenue of research would be to teach first degree Reiki to subjects and have them practice Reiki therapy as a self-healing strategy. This could be combined with weekly or periodic Reiki treatments by a Reiki therapy professional. The reasons for this suggestion are two-fold. First, a preliminary report using this method with an HIV population showed a decrease in pain and anxiety using self-Reiki (Miles, 2003). Second, when considering the study using Reiki versus RRT for men with prostate cancer, the RRT arm showed a larger decrease in anxiety (Beard et al., 2011). This may be because the men using RRT were encouraged to practice daily while the Reiki therapy intervention was only twice per week. It would be interesting to discover whether daily Reiki self-treatment would produce a larger decrease in pain or anxiety than a once or twice weekly session given by a Reiki therapy professional.
Limitations
Every effort was made to limit bias in study selection. Inclusion criteria were tight and strictly adhered to. Small sample sizes may contribute to some inflation of effect sizes. Only studies that used a reliable randomization scheme were included. There was no requirement on study use of validated measures although most studies included in this review did use validated measures. Only studies published in English were included and no gray literature such as dissertations or conference abstracts were included. Publication bias may of course account for some inflation of results.
Conclusion
There are very few high quality studies that explore the use of Reiki therapy for pain or anxiety. Because the number of studies is small, the interventions are dissimilar from each other, and the populations presented are so different, it is difficult to make generalizations or recommendations from these studies. Some of the dissimilarities included length of individual treatments which ranged from 30 to 90 minutes and populations varied from cancer to surgical to community dwelling adults. Design issues included small sample sizes, the timing of interventions in relation to the complaint, and the length of the intervention in relation to the issue being addressed such as painful diabetic neuropathy which is known to be difficult to treat. While it is often difficult to recruit subjects into non-drug related studies, more than one study specifically mentioned the difficulty of recruiting or keeping subjects in the non-Reiki control groups.
On the other hand, the majority of studies in this review did achieve statistical significance or near significance on the variable of interest; either pain or anxiety or both. Effect size calculations were performed using Cohen’s d which allows comparison of studies in a standardized way. Effect sizes for most of the studies in this review went from small to very large. Based on statistical significance, the strength of the effect sizes (see Table 1), and public interest in Reiki therapy as a non-invasive even comforting intervention, there is enough evidence to suggest continued research using Reiki therapy. Suggestions for study design and standardization of treatment protocol were proposed in order to increase the potential for positive outcomes in future research.
Implications for Nursing Education, Practice, and Research
Reiki therapy is a non-invasive, often comforting and relaxing intervention that is within nursing scope of practice in most states. Nurses may easily learn Reiki therapy and use this intervention with patients in day-to-day practice (Whelan & Wishnia, 2003). Additionally, Reiki therapy may be a good self-care tool as suggested by more than one study (Cuneo et al., 2011; Diaz-Rodriguez et al., 2011; Vitale, 2009). Based on this review, there is enough evidence to continue researching Reiki therapy as an intervention for pain and anxiety. Certainly more research is required in order to definitively recommend Reiki therapy as an intervention for decreased pain or anxiety.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Susan Thrane, Email: sut11@pitt.edu, University of Pittsburgh School of Nursing, Research in Cancer Survivorship, Supported by NINR (TNR011972A), 3500 Victoria Street, Victoria Building, Pittsburgh, PA 15261.
Susan M. Cohen, Email: cohensu@pitt.edu, University of Pittsburgh School of Nursing, 3500 Victoria Street, Victoria Building, Pittsburgh, PA 15261.
References
- A. G. S. Panel on Persistent Pain in Older Persons. The management of persistent pain in older persons. J Am Geriatr Soc. 2002;50(6 Suppl):S205–224. doi: 10.1046/j.1532-5415.50.6s.1.x. [DOI] [PubMed] [Google Scholar]
- Abo M, Kakuda W, Watanabe M, Morooka A, Kawakami K, Senoo A. Effectiveness of low-frequency rTMS and intensive speech therapy in poststroke patients with aphasia: a pilot study based on evaluation by fMRI in relation to type of aphasia. Eur Neurol. 2012;68(4):199–208. doi: 10.1159/000338773. [DOI] [PubMed] [Google Scholar]
- Assefi N, Bogart A, Goldberg J, Buchwald D. Reiki for the treatment of fibromyalgia: a randomized controlled trial. J Altern Complement Med. 2008;14(9):1115–1122. doi: 10.1089/acm.2008.0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard C, Stason WB, Wang Q, Manola J, Dean-Clower E, Dusek JA, Benson H. Effects of complementary therapies on clinical outcomes in patients being treated with radiation therapy for prostate cancer. Cancer. 2011;117(1):96–102. doi: 10.1002/cncr.25291. [DOI] [PubMed] [Google Scholar]
- Berger A. Magnetic resonance imaging. British Medical Journal. 2002;324:35. [Google Scholar]
- Birocco N, Guillame C, Storto S, Ritorto G, Catino C, Gir N, Ciuffreda L. The effects of Reiki therapy on pain and anxiety in patients attending a day oncology and infusion services unit. Am J Hosp Palliat Care. 2011 doi: 10.1177/1049909111420859. [DOI] [PubMed] [Google Scholar]
- Chang VT, Hwang SS, Feuerman M. Validation of the Edmonton Symptom Assessment Scale. Cancer. 2000;88(9):2164–2171. doi: 10.1002/(sici)1097-0142(20000501)88:9<2164::aid-cncr24>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- Cuneo CL, Curtis Cooper MR, Drew CS, Naoum-Heffernan C, Sherman T, Walz K, Weinberg J. The effect of Reiki on work-related stress of the registered nurse. J Holist Nurs. 2011;29(1):33–43. doi: 10.1177/0898010110377294. [DOI] [PubMed] [Google Scholar]
- Dale C. The Subtle body: An encyclopedia of your energetic anatomy. Boulder, CO: Sounds True, Inc; 2009. [Google Scholar]
- Diaz-Rodriguez L, Arroyo-Morales M, Cantarero-Villanueva I, Fernandez-Lao C, Polley M, Fernandez-de-las-Penas C. The application of Reiki in nurses diagnosed with Burnout Syndrome has beneficial effects on concentration of salivary IgA and blood pressure. Rev Lat Am Enfermagem. 2011;19(5):1132–1138. doi: 10.1590/s0104-11692011000500010. [DOI] [PubMed] [Google Scholar]
- Diefenbach GJ, Stanley MA, Beck JG, Novy DM, Verill P, Swann AC. Examination of the Hamilton Scales in assessment of anxious adults: A replication and extension. Journal of Psychopathology and Behavioral Assessment. 2001;23:117–127. [Google Scholar]
- Gillespie E, Gillespie BW, Stevens MJ. Painful diabetic neuropathy: Impact of an alternative approach. Diabetes Care. 2007;30(4):999–1001. doi: 10.2337/dc06-1475. [DOI] [PubMed] [Google Scholar]
- Heden P, Pilla AA. Effects of pulsed electromagnetic fields on postoperative pain: a double-blind randomized pilot study in breast augmentation patients. Aesthetic Plast Surg. 2008;32(4):660–666. doi: 10.1007/s00266-008-9169-z. [DOI] [PubMed] [Google Scholar]
- Hulse RS, Stuart-Shor EM, Russo J. Endoscopic procedure with a modified Reiki intervention: a pilot study. Gastroenterol Nurs. 2010;33(1):20–26. doi: 10.1097/SGA.0b013e3181ca03b9. [DOI] [PubMed] [Google Scholar]
- Hurvitz EA, Leonard C, Ayyangar R, Nelson VS. Complementary and alternative medicine use in families of children with cerebral palsy. Dev Med Child Neurol. 2003;45(6):364–370. doi: 10.1017/s0012162203000707. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Relieving pain in America: A blueprint for transforming prevention, care education, and research. 2011 from http://books.nap.edu/openbook.php?record_id=13172&page=1. [PubMed]
- Jain S, Mills PJ. Biofield therapies: helpful or full of hype? A best evidence synthesis. Int J Behav Med. 2010;17(1):1–16. doi: 10.1007/s12529-009-9062-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo T, Kakuda W, Yamada N, Shimizu M, Hagino H, Abo M. Effect of low-frequency rTMS on motor neuron excitability after stroke. Acta Neurol Scand. 2013;127(1):26–30. doi: 10.1111/j.1600-0404.2012.01669.x. [DOI] [PubMed] [Google Scholar]
- Lee MS, Pittler MH, Ernst E. Effects of reiki in clinical practice: a systematic review of randomised clinical trials. Int J Clin Pract. 2008;62(6):947–954. doi: 10.1111/j.1742-1241.2008.01729.x. [DOI] [PubMed] [Google Scholar]
- Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975;1(3):277–299. doi: 10.1016/0304-3959(75)90044-5. [DOI] [PubMed] [Google Scholar]
- Miles P. Preliminary report on the use of Reiki HIV-related pain and anxiety. [Evaluation Studies] Altern Ther Health Med. 2003;9(2):36. [PubMed] [Google Scholar]
- Miles P. Reiki: A comprehensive guide. New York: Tarcher/Penguin; 2008. [Google Scholar]
- Miles P, True G. Reiki--review of a biofield therapy history, theory, practice, and research. Altern Ther Health Med. 2003;9(2):62–72. [PubMed] [Google Scholar]
- National Center for Complementary and Alternative Medicine. Reiki: An introduction. 2012a Jul; 2009. from http://nccam.nih.gov/health/reiki/introduction.htm.
- National Center for Complementary and Alternative Medicine. What is complementary and alternative medicine? 2012b from http://nccam.nih.gov/health/whatiscam/
- Nobelprize.org. The nobel prize in physics 2012. 2012 from http://www.nobelprize.org/nobel_prizes/physics/laureates/2012/wineland.html.
- Olson K, Hanson J, Michaud M. A phase II trial of Reiki for the management of pain in advanced cancer patients. J Pain Symptom Manage. 2003;26(5):990–997. doi: 10.1016/S0885-3924(03)00334-8. [DOI] [PubMed] [Google Scholar]
- Oschman JL. Energy medicine: The scientific basis. New York: Churchill Livingstone; 2000. [Google Scholar]
- Park J, McCaffrey R, Dunn D, Goodman R. Managing osteoarthritis: comparisons of chair yoga, Reiki, and education (pilot study) Holist Nurs Pract. 2011;25(6):316–326. doi: 10.1097/HNP.0b013e318232c5f9. [DOI] [PubMed] [Google Scholar]
- Post-White J, Fitzgerald M, Savik K, Hooke MC, Hannahan AB, Sencer SF. Massage therapy for children with cancer. J Pediatr Oncol Nurs. 2009;26(1):16–28. doi: 10.1177/1043454208323295. [DOI] [PubMed] [Google Scholar]
- Potter PJ. Breast biopsy and distress: feasibility of testing a Reiki intervention. J Holist Nurs. 2007;25(4):238–248. doi: 10.1177/0898010107301618. discussion 249–251. [DOI] [PubMed] [Google Scholar]
- Rae AIM. Quantum Physics: A beginner’s guide. 2005. [Google Scholar]
- Rand WL. Reiki: The healing touch. Southfield, MI: Vision Publications; 2005. [Google Scholar]
- Rand WL. Reiki at University Medical Center, Tucson, Arizona, a magnet hospital. Holistic Nursing Practice. 2011;25(5):233–237. doi: 10.1097/HNP.0b013e31822a0291. [DOI] [PubMed] [Google Scholar]
- Richeson NE, Spross JA, Lutz K, Peng C. Effects of Reiki on anxiety, depression, pain, and physiological factors in community-dwelling older adults. Res Gerontol Nurs. 2010;3(3):187–199. doi: 10.3928/19404921-20100601-01. [DOI] [PubMed] [Google Scholar]
- Ring ME. Reiki and changes in pattern manifestations. Nurs Sci Q. 2009;22(3):250–258. doi: 10.1177/0894318409337014. [DOI] [PubMed] [Google Scholar]
- Rosenblum B, Kuttner F. Quantum enigma: Physics encounters consciousness. New York: Oxford University Press; 2006. [Google Scholar]
- Spielberger CD, Gorsch RL, Lushene RE, Vagg PR, Jacobs GA. State-Trait Anxiety Inventory for Adults. Menlo Park, CA: Mindgarden; 1983. [Google Scholar]
- The International Center for Reiki Training. The Center for Reiki Research. 2012 from http://www.centerforreikiresearch.org/
- Thomas ADH. Hidden in plain sight: The simple link between relativity and quantum mechanics. 2012. [Google Scholar]
- Tsang KL, Carlson LE, Olson K. Pilot crossover trial of Reiki versus rest for treating cancer-related fatigue. Integr Cancer Ther. 2007;6(1):25–35. doi: 10.1177/1534735406298986. [DOI] [PubMed] [Google Scholar]
- vanderVaart S, Gijsen VM, de Wildt SN, Koren G. A systematic review of the therapeutic effects of Reiki. J Altern Complement Med. 2009;15(11):1157–1169. doi: 10.1089/acm.2009.0036. [DOI] [PubMed] [Google Scholar]
- Vitale AT. An integrative review of Reiki touch therapy research. Holist Nurs Pract. 2007;21(4):167–179. doi: 10.1097/01.HNP.0000280927.83506.f6. quiz 180-161. [DOI] [PubMed] [Google Scholar]
- Vitale AT. Nurses’ lived experience of Reiki for self-care. Holist Nurs Pract. 2009;23(3):129–141. 142–125. doi: 10.1097/01.HNP.0000351369.99166.75. quiz 146-127. [DOI] [PubMed] [Google Scholar]
- Vitale AT, O’Connor PC. The effect of Reiki on pain and anxiety in women with abdominal hysterectomies: a quasi-experimental pilot study. Holist Nurs Pract. 2006;20(6):263–272. [PubMed] [Google Scholar]
- Whelan KM, Wishnia GS. Reiki therapy: the benefits to a nurse/Reiki practitioner. Holist Nurs Pract. 2003;17(4):209–217. doi: 10.1097/00004650-200307000-00008. [DOI] [PubMed] [Google Scholar]
- Zigmund A, Snaith R. The hospital anxiety and depression scale. Acta Psychiatricia Scandinavica. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]