Abstract
Because of the higher yield over traditional chromosomal analysis, chromosomal microarray analysis (CMA) is being used increasingly in prenatal diagnosis. Unfortunately, the clinical implication of many copy number variants found on prenatal CMA is uncertain, complicating genetic counseling. Recognizing that uncertain results will be encountered frequently as more of the genome is assayed prenatally, we set out to understand the experiences and needs of genetic counselors when counseling patients about uncertain prenatal microarray results, their comfort with various aspects of prenatal genetic counseling, and their interest in additional education and training about prenatal microarray testing. We first interviewed 10 genetic counselors about their experiences of providing pre- and post-test genetic counseling about prenatal CMA. Based on the findings from the counselor interviews, we developed items for a survey to assess the prevalence of genetic counselors’ attitudes towards, experience and comfort with, and educational needs regarding prenatal CMA. Based on surveys completed by 193 prenatal genetic counselors, we found that when there is an uncertain CMA result, only 59% would be comfortable providing genetic counseling and only 43% would be comfortable helping a patient make a decision about pregnancy termination. Being less comfortable was associated with seeing fewer patients having prenatal CMA testing. Respondents expressed a high degree of interest in additional education about prenatal CMA and counseling about uncertain results. Further genetic counselor education and training aimed at improving counselors’ personal comfort with uncertain results and communicating about them with patients is needed.
Keywords: Prenatal diagnosis, uncertainty, chromosomal microarray analysis, genetic counselor, education
Introduction
Chromosomal microarray analysis (CMA) can be used to detect small deletions or duplications of genetic material not detectable by traditional karyotyping techniques (Shaffer 2007). It has been recommended as a first tier test for evaluating children with developmental disabilities and multiple anomalies (Miller 2010). Because of the greater yield over traditional chromosomal analysis, CMA is being used increasingly in prenatal diagnosis and may replace karyotyping in high risk pregnancies (Brady 2014; Callaway 2013; Crolla 2014; Donnelly 2013; Hillman 2013a; Wapner 2012). The interpretation of some copy number variants (CNVs), however, is complicated and relies in part on the frequency of the CNV in healthy controls and information available in databases. Database information is usually based on phenotypes of children who had CMA testing done postnatally because of a clinical problem and is therefore potentially biased towards the severe end of the phenotypic spectrum (Benn 2013; Connelly 2013; Hehir-Kwa 2013).
Uncertainty about the expected phenotype associated with CNVs found in a prenatal microarray testing sample can lead to distress in the pregnant woman and her partner, and complicate decision-making (Bernhardt 2012; de Jong 2013; Hillman 2013b; Klugman 2013; Stark 2013). Although less well studied, positive prenatal testing results can also cause health professionals to experience distress (Menezes 2013). The negative impact of such results has been attributed to a variety of factors, including the task of breaking bad news, urgency in decision-making, and countertransference (Menezes 2013). When results are uncertain, the challenges to genetic counselors are magnified (Bernhardt 2012). In these situations, a variety of factors may lead to genetic counselor distress including their inability to provide precise outcome information, patients’ decisions to terminate pregnancies based on such results, and concerns about psychological harm to patients caused by uncertain results (Mikhaelian 2013).
When confronted with uncertainty, clinicians and patients alike attempt to address the resulting anxiety by gathering information to reduce uncertainty (Brashers 2013). Whether or not results are uncertain, genetic counselors routinely seek out and provide patients with all available information about genetic testing results so patients can make well-informed decisions. From the patient’s perspective, however, uncertainty may remain or be increased even when all available information has been discussed and understood. This is because much of the information about the implications of genetic test results is probabilistic and therefore inherently uncertain (for example, “there is a 20% risk for intellectual disability”). Moreover, there is often ambiguity about the magnitude of the risk (for example, “the risk of intellectual disability is between 5 and 30%”). The genetic counselor must then assist the patient in making a decision about the pregnancy in the face of considerable uncertainty and ambiguity.
As suggested by Rene Fox (1980) clinicians will face additional uncertainty when they are unable to distinguish between their own personal lack of knowledge and the limitations of the currently available information. This type of uncertainty is likely at the core of the observation that physicians with less clinical experience have more anxiety associated with uncertainty (Politi 2010). As they gain more clinical experience working with new testing technologies, many genetic counselors come to realize that uncertainty and ambiguity are part of the genetic testing and counseling process, and report accepting that some questions simply cannot be answered through information seeking (Runyon 2010). Indeed, with the advent of new genomic testing technologies, such as whole genome and whole exome sequencing, the frequency with which genetic counselors will be faced with uncertain information will increase. Paradoxically, patients may actually expect higher levels of certainty about predictions relating to health and development as they utilize new genomic testing modalities (Kenen 2011). Experts recognize, however, that variants of uncertain significance will be encountered frequently, and pathogenic changes will be found in genes that may or may not impact the patient’s phenotype (Kohane 2006; Stark 2013; Jacob 2013). This implies that genetic counselors will often be called upon to discuss information of uncertain consequence with patients, and when such information becomes available prenatally, decisions will need to be made quickly, and at a time that is particularly emotionally charged.
There have been few studies exploring how genetic counselors deal with uncertainty, and little guidance as to the types of education and training needed to help them assist patients making decisions in the face of uncertainty (Kenen 2011). Recognizing that uncertain results will be encountered more frequently as prenatal testing expands, we set out to understand the experiences of genetic counselors when counseling patients about uncertain prenatal microarray results, their comfort with various aspects of prenatal genetic counseling, and their interest in additional education and training about prenatal microarray testing.
METHODS
OVERVIEW
In this study, we first used qualitative methods to explore genetic counselors’ experiences providing pre- and post-test genetic counseling regarding prenatal microarray testing. Based on the findings from in-depth telephone interviews conducted with genetic counselors, we developed items for a survey to assess the prevalence of genetic counselors’ attitudes towards, experiences with, and educational needs regarding prenatal microarray testing. The study was approved by the Institutional Review Board of the University of Pennsylvania.
INTERVIEW POTION
Recruitment
Participants for the interview portion of this study included genetic counselors who participated in a multicenter prospective study “Prenatal Cytogenetic Diagnosis by Array-based Copy Number Analysis,” coordinated through Columbia University (study findings reported in Wapner 2012). One genetic counselor from each of the 29 participating centers was sent an email by the study principal investigator at Columbia University about the opportunity to participate in a telephone interview aimed at exploring their experience offering microarray testing to patients. Interested counselors then contacted the University of Pennsylvania research coordinator to provide consent and set up a time to be interviewed by phone. All interviews were conducted by the University of Pennsylvania study principal investigator.
Data Collection
Interviews were conducted using a semi-structured interview guide designed to elicit counselors’ experiences offering prenatal microarray testing, including pre- and post-test counseling, as a part of the NICHD-sponsored study. Informed consent was obtained before beginning the interview. Participants were asked to discuss one or more challenging case examples. The questions were open-ended and probes were used to encourage participants to elaborate on their responses. We also collected demographic data from each participant, including years of experience and the approximate number of patients seen who had opted to have prenatal microarray testing. The interviews lasted between 30 and 40 minutes and were audiorecorded.
Data Analysis
All audio recordings of the telephone interviews were transcribed verbatim. The de-identified transcripts were then imported into the qualitative analysis software NVivo 10 for coding and analysis. The study team developed and revised the codebook based on themes that arose from the data. Two investigators independently coded the transcripts after reaching standard intercoder reliability. In-depth analysis of the coded data was performed in order to evaluate the similarities and differences in the experiences of the participants.
SURVEY PORTION
Recruitment
Participants for the survey portion of the study were members of the National Society of Genetic Counselors (NSGC) who were recruited either through postings on NSGC on-line discussion forums or through personalized emails. Counselors were eligible to complete the survey if they had discussed prenatal microarray testing with at least one pregnant woman within the past year. We first posted an announcement of the survey and survey link on the NSGC Prenatal Counseling/Ultrasound Anomalies Special Interest Group (SIG) discussion forum. A week later, we posted an announcement of the survey on the NSGC main discussion forum, and then re-posted the announcement a week later. One week after that, we sent a personal email and survey link to 125 randomly selected genetic counselors who listed their specialty as prenatal counseling. We excluded those counselors to whom an incentive had been paid already for having completed a survey (see below). Surveys were completed between February and April of 2013.
Data Collection and Analysis
The survey instrument was developed by the study team and included a series of items to assess level of interest in education or training related to various aspects of prenatal testing, including microarray testing, using a 4-point scale ranging from 1 = not at all interested to 4 = very interested. Items assessing comfort with various aspects of prenatal genetic counseling, including counseling about a range of possible prenatal microarray results were also presented with a scale from 1 = very uncomfortable to 4 = very comfortable. Sociodemographic items were included to gather data about each counselor’s years of experience, number of patients having prenatal microarray testing, gender, age, race, and ethnicity.
An informed consent statement was included at the beginning of the survey, and respondents could complete the survey after checking a box indicating that he or she provided informed consent to participate. Survey responses were anonymous. At the end of the survey, respondents were taken to a second completely separate survey asking them to provide their email address so we could send them a $10 e-gift card.
Responses to the interest in education and comfort items were dichotomized in the middle. Data were analyzed using SPSS 16.0. Chi square analyses were performed to look for differences according to sociodemographic and practice variables.
RESULTS
Interview portion
Telephone interviews were conducted with 10 genetic counselors. All participating counselors were female. They had between 3 and 14 years experience as a genetic counselor (median = 6 years). Except for one, all counselors indicated that their experience in genetic counseling occurred exclusively in prenatal settings. They reported having seen between 8 and 400 women who opted to have prenatal microarray testing (median = 100).
Genetic counselors were greatly impacted by the uncertainty associated with some prenatal microarray results. This was most obvious during the portion of the interview when participants were asked to discuss their most challenging cases. All of the interviewees discussed one or more cases in which women received positive results, generally results of uncertain significance. Participants highlighted the lack of information about the implications of many copy number variants, resulting in their inability to provide patients with a numerical probability to express the likelihood of their baby having a problem. One counselor said:
…these cases are frustrating because also you’re not really able to put a number on what is your increased risk—what is the chance that this child actually is going to have autism? (PR13)
Other genetic counselors focused on uncertainty resulting from the phenotypic variability associated with many copy number variants, resulting in frustration for both the patient and the genetic counselor:
So it was a particularly hard case to give any sort of phenotypic range because it was anywhere from completely normal to mental retardation and developmental delay. …No percentages and really no additional information and no way to get additional information. So this case was very, very difficult because she was very insistent on having more information, which is completely understandable. It was frustrating for me because I couldn’t provide her any additional information. It was frustrating for her because she couldn’t get any. (PR17)
Another genetic counselor lamented about the lack of information about prognosis associated with many copy number variants:
It’s frustrating especially as this technology has taken off and there’s just not a lot of data about these esoteric deletions or duplications. All you can do is go to a family and say, “Well, we found a change, but there are only 3 cases in the literature and one’s walking around and fine and the other 2 have severe mental retardation.” (PR04)
Such situations are all the more difficult because the genetic counselor is regarded as an expert and accustomed to providing answers to patient questions:
I always want to be able to provide as much information so that a patient feels comfortable with what diagnosis we’re giving. I think for me what was most uncomfortable was just the limited amount of information that we could provide. …I think with a lot of things, the counseling piece of results isn’t out there as far as guidelines of what should we be telling patients for the range. (PR06)
Not being able to predict the type of result that might come from microarray testing was viewed as one of the drawbacks to prenatal CMA testing:
So, it’s a little bit of a black box with the microarray—you don’t really know what you’re getting into. Until you’ve got it. (PR04)
Dealing with uncertain results often left genetic counselors unsure of how to help patients make decisions about their pregnancies:
PR10: I was already very nervous about providing their results, because I didn’t know what I would do if it were me. So I knew that it was going to be difficult information to provide to someone, and I…I thought during the session that she took it well. She was overwhelmed. I had printed out the reports that were available; we went over those together. I made copies of them for her. But then when she said things like ‘I wish I didn’t know this information’ and ‘what am I supposed to do with this information?’, then I felt more like…I guess I didn’t really know what to say because I probably wouldn’t know what to do either.
Interviewer: Now presumably, in the course of providing counseling over the years, you’ve had other couples who have had results that are difficult to interpret. You know, small markers or whatever. Or haven’t you maybe?
PR10: No, I think this had been probably the most difficult results that I’ve had to deliver.
The counselors interviewed discussed how the phenotypic uncertainty associated with many copy number variants engendered significant distress for patients. This was especially true for the many patients who sought out microarray testing for reassurance that their baby was all right. One counselor said:
And they did a test to get reassurance that their child didn’t have Down syndrome. Not only did we not give them reassurance, but we added uncertainty. It was completely not what they went into the test expecting. (PR06)
Several genetic counselors discussed the relief they felt when one of the expert physicians associated with the study relayed uncertain findings to the patient. One counselor said:
PR07: “…. based on either a case report or the literature, the review board has felt that it needs to be reported because of the possibility of it manifesting differently.
Interviewer: And so how did you handle that particular information then?
PR07: [Expert Physician] calls the patient, which is nice.
Interviewer: What makes that nice?
PR07: Well, so you don’t have to do it yourself.
Other genetic counselors admitted to doubting themselves because they were not confident they were relaying all the information that could be known about a particular finding. In such cases, it was helpful when one of the expert physicians associated with the study volunteered to discuss the implications of the findings with a patient:
“I guess what helps me is that there’s somebody else saying the same thing I am and for patients like reinforcing the same information or lack thereof, is I guess can be helpful for them to at least accept the results.” (PR17)
One counselor talked about how she wished that there was someone else she could consult with to help interpret the implications of the patient’s uncertain microarray results.
PR05: I guess I couldn’t tell her exactly what it meant. I just told her about that condition but that I didn’t know if that would be what her baby actually had.
Interviewer: So were you feeling as though somebody out there had the information but you just weren’t able to tap into it?
PR05: I think if we ultimately just couldn’t tell her exactly what it meant, I needed somebody bigger than me to say that. It’s hard for me to make that call. …I felt like I just needed somebody else to say “we can’t really tell you.” I just felt kinda lost… like I was dealing with the case myself”.
Survey portion
In total, 193 genetic counselors responded to the survey, and 188 respondents completed all survey questions. One hundred nineteen counselors responded to the postings on the discussion forums. Seventy-four counselors (59.2% response rate) completed the survey after receiving the email invitation.
Information on sociodemographics and professional experience of survey respondents is included in Table I. Nearly all respondents were female and white, and the majority had less than 10 years of experience. The majority had offered prenatal microarray testing to fewer than 10 patients.
Table I.
Sociodemographics and professional experience of survey respondents
| Variable | % of total (n=193) |
|---|---|
|
| |
| Age (years) | |
| 20–29 | 31.9 |
| 30–39 | 44.3 |
| 40–49 | 14.6 |
| 50 and older | 9.2 |
|
| |
| Gender | |
| Female | 95.3 |
| Male | 4.7 |
|
| |
| Race | |
| White | 91.9 |
| Non-white | 8.1 |
|
| |
| Years in Practice | |
| < 5 | 37.9 |
| 5 – 10 | 27.9 |
| 11 – 20 | 24.7 |
| >20 | 9.5 |
|
| |
| # patients opting to have prenatal CMA | |
| none | 5.1 |
| 1 – 10 | 51.8 |
| 11 – 50 | 35.9 |
| >50 | 7.2 |
Comfort with various aspects of patient care relating to prenatal testing is included in Figure 1. Over 80% of counselors were comfortable with most aspects of counseling relating to prenatal diagnosis, including some circumstances in which the outcome might be uncertain, such as a mosaic result on CVS or a small marker chromosome found on amniocentesis. Sixty-seven percent of counselors were comfortable obtaining information to clarify the meaning of an uncertain microarray result, 59% were comfortable providing genetic counseling about an uncertain prenatal microarray result, and only 43% were comfortable helping a patient make a decision about terminating a pregnancy if there is an uncertain prenatal microarray result. In bivariate analysis looking for an association between comfort and years of experience, age, and volume of patients having CMA testing, the only significant differences were that counselors seeing more than 10 patients having testing were more likely to be comfortable providing genetic counseling about an uncertain prenatal microarray result (69%) than were counselors seeing 10 or fewer patients (52% comfortable; p =0.033). Counselors seeing more than 10 patients were also more comfortable helping patients make a decision about the pregnancy in the face of an uncertain prenatal microarray result (52% comfortable) than were counselors seeing fewer than 10 patients having testing (35%; p=0.035).
Figure 1.
Comfort with patient care relating to prenatal testing
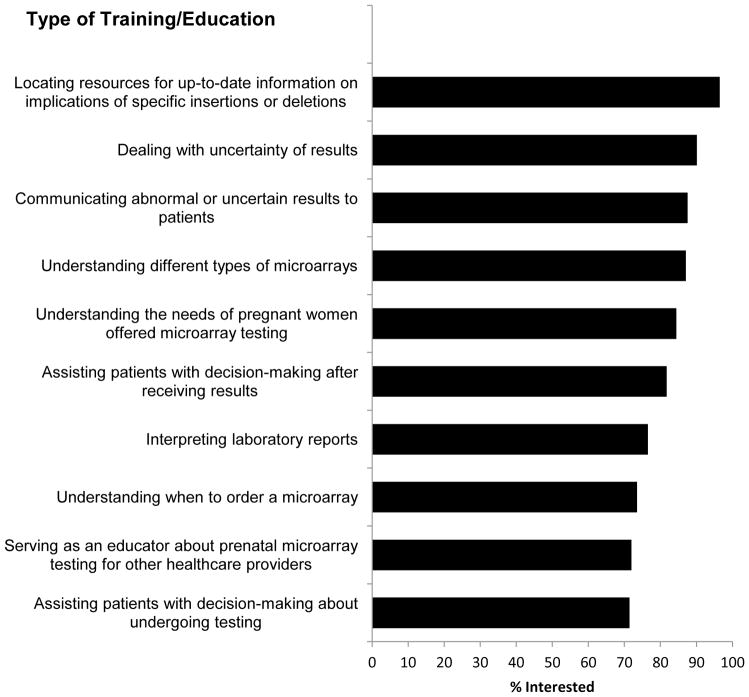
Data on interest in additional training or education relating to prenatal microarray testing are included in Figure 2. Respondents expressed the most interest in locating resources for up-to-date information on the implications of specific insertions or deletions (96% interested), dealing with the uncertainty of results (90% interested), and communicating abnormal or uncertain results to patients (88% interested). In bivariate analysis to look for an association between educational interests and years of experience, age, and volume of patients having CMA testing, the only significant differences were that counselors seeing 10 or fewer patients having testing were more likely to be interested in education relating to dealing with uncertain results (95%) than were counselors seeing more than 10 patients (83%; p=0.011), and counselors seeing 10 or fewer patients having testing were more likely to be interested in education relating to communicating abnormal or uncertain results to patients (93%) than were counselors seeing more than 10 patients (79%; p=0.008).
Figure 2.
Interest in additional training or education relating to prenatal CMA testing
DISCUSSION
Through interviews with genetic counselors, we found that counseling women about uncertain results is challenging. Our survey showed that nearly all prenatal genetic counselors are comfortable in situations where there are data available to quantify possible outcomes. Thus, most respondents would be comfortable providing counseling about prenatally diagnosed Down syndrome, an apparently balanced translocation, or an obviously abnormal prenatal microarray result. Fewer counselors were comfortable when there was less certainty about outcomes, such as a prenatal diagnosis finding of a variant of unknown significance on CMA. In such a situation, only 59% would be comfortable providing genetic counseling and only 43% would be comfortable helping a patient make a decision about pregnancy termination. Counselors who were less comfortable were significantly more likely to see fewer patients having prenatal CMA testing.
Genetic counselors expressed a high degree of interest in additional education about prenatal microarray testing, especially in education about locating resources for current information about the implications of uncertain results, as well as additional education and training about how to manage abnormal results, communicate about them with patients, and assist patients with decision-making after receiving results. Counselors seeing fewer prenatal CMA patients were more interested in additional education.
Our interviews confirmed that when a CNV is found on a prenatal sample, genetic counselors will routinely seek out information about the clinical implication of the CNV. Several CNV databases are available that provide up-to-date information about genotype-phenotype correlations (Callaway, 2013; Donnelly 2013). Additional information about the range of phenotypes associated with more common deletions and duplications is also being collected and summarized, and made available through the website www.prenatalmicroarray.org. Information in the databases, however, is based primarily on CNVs found in pediatric patients who were tested because of a clinical abnormality. Because of this, phenotypic information may be skewed towards the severe end of the spectrum, especially because there is wide variability in clinical involvement for many CNVs. Through the on-going NIH-supported study “Prenatal cytogenetic diagnosis by array-based copy number analyses,” cases with CNVs diagnosed prenatally are being identified and followed until age 3 in order to avoid the ascertainment bias that is inherent in postnatally identified patients (Donnelly 2013).
However, even when complete data is available about the expected phenotypic range associated with a particular CNV, uncertainty often remains. At best, the information may provide the probability of a problem, or a range of issues that might be associated with the deletion or duplication. In some cases, information is inconsistent or contradictory and leads to increased uncertainty and ambiguity. But, access to accurate and up-to-date information can reassure the counselor that she is as knowledgeable as possible about the implications of a finding, increasing her own confidence. She will likely be viewed by the patient as a competent and expert source of support who is a collaborator in information gathering and evaluation. The next part of her job will be to communicate the information to the patient, along with its associated uncertainties and ambiguities, and to help the patient make decisions based on the available facts.
These tasks are part of the widely-agreed upon goals of genetic counseling including educating patients and promoting informed decision-making (Veach 2007). Practice-based competencies to achieve these goals have been outlined by the Accreditation Council for Genetic Counseling (2013) and current genetic counselor graduate programs base their curricula on training students to demonstrate these competencies. The competencies, though broad and comprehensive especially with regard to counselor knowledge about genetics and risk communication, do not address how to promote informed decision-making when confronted with uncertain results. This is surprising, since uncertainty has always been part of genetic counseling. For example, results of molecular, cytogenetic and fetal ultrasound tests frequently yield uncertain findings. With more experience, many genetic counselors learn the best ways to help patients understand and accept uncertain information. But given the high degree of interest in education expressed by survey respondents, including those with considerable experience, it is clear that both genetic counseling students and practicing counselors need and want additional training in this area.
In other clinical arenas, important choices patients make are frequently based on a shared decision-making model in which patients and clinicians discuss available facts and share personal preferences and values. A trusting relationship in which the clinician knows the patient as a person, and understands her values, experiences and informational needs is central to shared decision-making (Epstein 2013; Han 2013). When there are uncertainties relating to potential outcomes, shared decision-making can promote patient autonomy through a patient-clinician partnership aimed at helping patients achieve clarity about their preferences in the face of complexity, inadequate evidence, and irreducible uncertainty. Evidence suggests that when there is a strong patient-clinician relationship, patients will feel increasingly competent to engage in the decision-making process when faced with high-stake choices in the face of uncertainty and ambiguity (Epstein 2013; Politi 2007).
Although patient autonomy is a cornerstone of genetic counseling, a shared decision-making model is rarely discussed in the context of genetic counseling. Several scholars have suggested that this absence relates to the central role of non-directiveness in genetic counseling. This focus may lead the genetic counselor to limit her own involvement in the deliberative process that is part of shared decision-making (Kessler 1997; White, 1997; Hunt 2005). Non-directiveness may also inhibit the counselor’s ability to utilize a full range of counseling techniques, knowledge and experience, thereby reducing her effectiveness in assisting patients who need to make important decisions in the midst of a crisis (Weil 2006).
In situations involving prenatal CMA results when information is unavailable or inconsistent, or when the genetic counselor feels insecure in her own state of knowledge, she may be even more reluctant to participate in decision-making (Bernhardt 2010). In her critique of non-directiveness, White (1997) suggested that counselors should focus less on being an expert providing information and more on the deliberative process in which the counselor and client mutually engage in problem solving. Such practice is reflected in the reciprocal-engagement model of genetic counseling that guides much of the current student training (Veach 2007). In this model, the practice of genetic counseling, including education, counseling, and support with decision making is modulated by the genetic counselor-patient relationship. Recent research has documented that although genetic counseling graduate program directors and practicing genetic counselors support the goals of the reciprocal-engagement model, the psychosocial skills that are integral to the model may be more challenging to develop and implement within a session (Hartman 2013).
As currently practiced, most genetic counseling sessions are predominated by presentation of clinical and genetic information with little time devoted to values clarification and facilitation of decision-making (Roter 2006; Ellington 2011). This is likely because genetic counselors are generally confident in their skills as information givers and less confident is their skills relating to the psychosocial components of genetic counseling (Borders 2006). As noted above, counselors’ over-reliance on adopting a non-directive stance may inhibit an interactive skills-based approach to genetic counseling. When information is uncertain or unavailable, a genetic counselor who is accustomed to being viewed as an expert may feel that her credibility is threatened, and may be unsure how to help the client (Sarangi and Clarke 2002; Braddock 2013). However, even when there is uncertainty or inadequate medical evidence, the process of the provider and patient engaging in shared decision-making has a positive effect on the patient’s confidence in her decision and trust in her provider. Adopting a model of shared decision-making is also associated with a reduction in the stress level of the clinician (Shaw 2013; Braddock 2013).
Study limitations
Qualitative studies aim to identify a broad range of experiences and our findings from the interview portion of the study were not intended to quantify the prevalence of any particular experience. In the interview portion of the study, a limitation is the small number of genetic counselors who were interviewed. Moreover, those genetic counselors who volunteered to be interviewed may have been systematically different from eligible counselors who were not interviewed. Furthermore, the eligible genetic counselors who were providing genetic counseling to women having microarrays as a part of the NIH-funded study may not be representative of prenatal genetic counselors in general. Likewise, those genetic counselors that completed a survey may differ from survey non-respondents.
Implications for practice and training
In this study, nearly all genetic counselors surveyed expressed interest in further education and training relating to dealing with uncertain results and communicating about them with patients. This training will need to be incorporated into both the didactic and clinical supervision portions of graduate school training and made available as continuing education for the practicing genetic counselor.
As discussed above, much of this communication and counseling should be taking place in the context of shared decision-making. Successful strategies for training other clinicians, primarily physicians, to engage in shared decision making are relevant for genetic counselor training. It is acknowledged that in order to help a patient make a decision under conditions of uncertainty, the clinician will need to take it upon herself to first become comfortable with uncertainty (Braddock 2013). This can be facilitated through a variety of self-care modalities aimed at helping the counselor to more globally attend to the anxiety that may result from uncertainties by becoming more in touch with herself. Engaging in contemplative practices, such as mindfulness, will allow the counselor to monitor her own feelings, biases, and assumptions, likely influencing her care of the patient This awareness will help her engage in active listening, identify indications of patient’s understanding and receptivity, and assist patients in making personal meaning of the information and choices offered (Epstein 2013). Reflective writing can be a powerful tool in expressing feelings associated with uncertainty and in supporting professional development by helping clinicians learn to cope with uncertainty (Nevalainen 2010). Peer support groups and formal individual supervision can serve as a forum for discussing distressing patient interactions and promoting self-care (Menzes 2013). Communication skills training workshops can enhance the skills of practicing genetic counselors by increasing confidence and allowing reflection on their own practice (Dunlop 2011). Many potential strategies to facilitate skills acquisition and to promote competence and confidence for genetic counselors have been outlined elsewhere (Peters 2010).
Research recommendations
Research is needed to identify the best ways to help genetic counselors accept the uncertainties associated with many new genetic testing technologies. Trials of some of the modalities outlined above could lead to implementation of programs to enhance counselors’ comfort with uncertainty and their ability to remain non-directive while engaging the patient in values-based decision-making. Current research assessing the process and outcomes of genetic counseling for genomic sequencing may also shed light on optimal ways to help patients make decisions based on uncertain information.
Research also is needed to understand both why genetic counselors have difficulty implementing a reciprocal engagement model of genetic counseling and possible ways to incorporate shared decision-making into genetic counselor practice. Novel approaches to graduate teaching and continuing education modalities need to be outlined and evaluated.
CONCLUSIONS
Chromosomal microarray testing on fetal samples obtained through CVS and amniocentesis is likely to play a major role in current and future prenatal care. With the recent announcement by several laboratories of the addition of a limited number of CNVs to their testing panels, it also is likely to be incorporated into non-invasive testing of fetal cell-free DNA obtained from maternal blood (Srinivasan 2013). As genetic testing, including prenatal microarray testing, is incorporated into mainstream clinical care, genetic counselors will increasingly be called upon to assist clinicians whose patients receive positive or uncertain results. Genetic counselors will need to have the skills to access information about the implications of results, training to assist patients who are making decisions in the face of uncertainty, and ongoing support as they are faced with challenging counseling sessions.
Acknowledgments
This study was supported by grant #5 UO1 HD055651 from the National Institute of Child Health and Human Development, and by grant # P50 HG004487 from the National Human Genome Research Institute. We wish to thank the genetic counselors who completed surveys and who consented to be interviewed. We also thank Danielle Soucier for her assistance with coding interview transcripts, and Melissa Savage for assistance with recruitment.
Footnotes
CONFLICTS OF INTEREST
Barbara A. Bernhardt, Katherine Kellom, Alexandra Barbarese, W. Andrew Faucett, and Ronald J. Wapner declare that they have no conflict of interest.
INFORMED CONSENT
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants who were included in the study.
References
- Accreditation Counsel for Genetic Counseling. [September 26, 2013];Practice-Based Competencies for Genetic Counselors. Accessed at www.gceducation.org.
- Benn PA. Prenatal counseling and the detection of copy-number variants. Genetics in Medicine. 2013;15:316–317. doi: 10.1038/gim.2013.16. [DOI] [PubMed] [Google Scholar]
- Bernhardt BA, Silver R, Rushton CH, Micco E, Geller G. What keeps you up at night? Genetics professionals’ distressing experiences in patient care. Genetics in Medicine. 2010;12(5):289–297. doi: 10.1097/GIM.0b013e3181db82d9. [DOI] [PubMed] [Google Scholar]
- Bernhardt BA, Soucier D, Hanson K, Savage MS, Jackson L, Wapner RJ. Women’s experiences receiving abnormal prenatal chromosomal microarray testing results. Genetics in Medicine. 2012;15(2):139–145. doi: 10.1038/gim.2012.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borders LD, Eubanks S, Callanan N. Supervision of psychosocial skills in genetic counseling. Journal of Genetic Counseling. 2006;15(4):211–223. doi: 10.1007/s10897-006-9024-9. [DOI] [PubMed] [Google Scholar]
- Braddock CH. Supporting shared decision making when clinical evidence is low. Medical Care Research and Review. 2013;70(1 suppl):129S–140S. doi: 10.1177/1077558712460280. [DOI] [PubMed] [Google Scholar]
- Brady PD, Delle Chiaie B, Christenhusz G, Dierickx K, Van Den Bogaert K, Menten B, et al. A prospective study of the clinical utility of prenatal chromosomal microarray analysis in fetuses with ultrasound abnormalities and an exploration of a framework for reporting unclassified variants and risk factors. Genetics in Medicine. 2014 doi: 10.1038/gim.2013.168. in press. [DOI] [PubMed] [Google Scholar]
- Brashers DE, Hogan TP. The appraisal and management of uncertainty: Implications for information-retrieval systems. Information Processing & Management. 2013;49(6):1241–1249. [Google Scholar]
- Callaway JL, Shaffer LG, Chitty LS, Rosenfeld JA, Crolla JA. The clinical utility of microarray technologies applied to prenatal cytogenetics in the presence of a normal conventional karyotype: a review of the literature. Prenatal Diagnosis. 2013;33(12):1119–1123. doi: 10.1002/pd.4209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crolla JA, Wapner R, Van Lith JM. Controversies in prenatal diagnosis 3: should everyone undergoing invasive testing have a microarray? Prenatal Diagnosis. 2014;34(1):18–22. doi: 10.1002/pd.4287. [DOI] [PubMed] [Google Scholar]
- de Jong A, Dondorp WJ, Macville MV, de Die-Smulders CE, van Lith JM, de Wert GM. Microarrays as a diagnostic tool in prenatal screening strategies: ethical reflection. Human Genetics. 2013:1–10. doi: 10.1007/s00439-013-1365-5. [DOI] [PubMed] [Google Scholar]
- Donnelly JC, Wapner RJ, Simpson JL. Can microarray analysis reveal additional abnormalities in prenatal diagnosis? Expert Review of Obstetrics & Gynecology. 2013;8(3):193–195. [Google Scholar]
- Dunlop KL, Barlow-Stewart K, Butow P, Heinrich P. A Model of Professional Development for Practicing Genetic Counselors: Adaptation of Communication Skills Training in Oncology. Journal of Genetic Counseling. 2011;20(3):217–230. doi: 10.1007/s10897-010-9340-y. [DOI] [PubMed] [Google Scholar]
- Ellington L, Kelly KM, Reblin M, Latimer S, Roter D. Communication in genetic counseling: cognitive and emotional processing. Health Communication. 2011;26(7):667–675. doi: 10.1080/10410236.2011.561921. [DOI] [PubMed] [Google Scholar]
- Epstein RM, Gramling RE. What is shared in shared decision making? Complex decisions when the evidence is unclear. Medical Care Research and Review. 2013;70(1 suppl):94S–112S. doi: 10.1177/1077558712459216. [DOI] [PubMed] [Google Scholar]
- Fox RC. The evolution of medical uncertainty. The Milbank Memorial Fund Quarterly. Health and Society. 1980;58(1):1–49. [PubMed] [Google Scholar]
- Han PK. Conceptual, Methodological, and Ethical Problems in Communicating Uncertainty in Clinical Evidence. Medical Care Research and Review. 2013;70(1 suppl):14S–36S. doi: 10.1177/1077558712459361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann JE, Veach PM, MacFarlane IM, LeRoy BS. Genetic Counselor Perceptions of Genetic Counseling Session Goals: A Validation Study of the Reciprocal-Engagement Model. Journal of Genetic Counseling. 2013:1–13. doi: 10.1007/s10897-013-9647-6. [DOI] [PubMed] [Google Scholar]
- Hehir-Kwa JY, Pfundt R, Veltman JA, de Leeuw N. Pathogenic or not? Assessing the clinical relevance of copy number variants. Clinical Genetics. 2013;84(5):415–421. doi: 10.1111/cge.12242. [DOI] [PubMed] [Google Scholar]
- Hillman S, McMullan DJ, Maher ER, Kilby MD. The use of chromosomal microarray in prenatal diagnosis. The Obstetrician & Gynaecologist. 2013a;15(2):80–84. [Google Scholar]
- Hillman SC, Skelton J, Quinlan-Jones E, Wilson A, Kilby MD. “If it helps…” the use of microarray technology in prenatal testing: Patient and partners reflections. American Journal of Medical Genetics Part A. 2013b;161A:1619–1627. doi: 10.1002/ajmg.a.35981. [DOI] [PubMed] [Google Scholar]
- Hunt LM, de Voogd KB, Castañeda H. The routine and the traumatic in prenatal genetic diagnosis: does clinical information inform patient decision-making? Patient Education and Counseling. 2005;56(3):302–312. doi: 10.1016/j.pec.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Kenen R, Ardern-Jones A, Lynch E, Eeles R. Ownership of uncertainty: Healthcare professionals counseling and treating women from hereditary breast and ovarian cancer families who receive an inconclusive BRCA1/2 genetic test result. Genetic Testing and Molecular Biomarkers. 2011;15(4):243–250. doi: 10.1089/gtmb.2010.0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler S. Psychological aspects of genetic counseling. XI. Nondirectiveness revisited. American Journal of Medical Genetics. 1997;72(2):164–171. doi: 10.1002/(sici)1096-8628(19971017)72:2<164::aid-ajmg8>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- Klugman S, Suskin B, Spencer BL, Dar PE, Bajaj K, Powers J, Merkatz IR. Clinical utility of chromosomal microarray analysis in prenatal diagnosis: report of first 6 months in clinical practice*. The Journal of Maternal-Fetal & Neonatal Medicine. 2013;(0):1–6. doi: 10.3109/14767058.2013.858243. [DOI] [PubMed] [Google Scholar]
- Kohane IS, Masys DR, Altman RB. The incidentalome. JAMA. 2006;296(2):212–215. doi: 10.1001/jama.296.2.212. [DOI] [PubMed] [Google Scholar]
- Menezes MA, Hodgson JM, Sahhar M, Metcalfe SA. “Taking Its Toll”: The Challenges of Working in Fetal Medicine. Birth. 2013;40(1):52–60. doi: 10.1111/birt.12029. [DOI] [PubMed] [Google Scholar]
- Mikhaelian M, Veach PM, MacFarlane I, LeRoy BS, Bower M. Prenatal chromosomal microarray analysis: a survey of prenatal genetic counselors’ experiences and attitudes. Prenatal Diagnosis. 2013;33:371–377. doi: 10.1002/pd.4071. [DOI] [PubMed] [Google Scholar]
- Miller DT, Adam MP, Aradhya S, Biesecker LG, Brothman AR, Carter NP, et al. Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. The American Journal of Human Genetics. 2010;86(5):749–764. doi: 10.1016/j.ajhg.2010.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nevalainen MK, Mantyranta T, Pitkala KH. Facing uncertainty as a medical student—a qualitative study of their reflective learning diaries and writings on specific themes during the first clinical year. Patient Education and Counseling. 2010;78(2):218–223. doi: 10.1016/j.pec.2009.07.011. [DOI] [PubMed] [Google Scholar]
- Peters JA. Genetic Counseling Practice: Advanced Concepts and Skills. Hoboken: Wiley-Blackwell; 2010. Genetic counselors: Caring mindfully for ourselves. [Google Scholar]
- Politi MC, Han PK, Col NF. Communicating the uncertainty of harms and benefits of medical interventions. Medical Decision Making. 2007;27(5):681–695. doi: 10.1177/0272989X07307270. [DOI] [PubMed] [Google Scholar]
- Politi MC, Légaré F. Physicians’ reactions to uncertainty in the context of shared decision making. Patient Education and Counseling. 2010;80(2):155–157. doi: 10.1016/j.pec.2009.10.030. [DOI] [PubMed] [Google Scholar]
- Roter D, Ellington L, Erby LH, Larson S, Dudley W. The genetic counseling video project (GCVP): models of practice. American Journal of Medical Genetics Part C: Seminars in Medical Genetics. 2006;142 (4):209–220. doi: 10.1002/ajmg.c.30094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarangi S, Clarke A. Zones of expertise and the management of uncertainty in genetics risk communication. Research on Language and Social Interaction. 2002;35(2):139–171. [Google Scholar]
- Shaffer LG, Bejjani BA, Torchia B, Kirkpatrick S, Coppinger J, Ballif BC. The identification of microdeletion syndromes and other chromosome abnormalities: cytogenetic methods of the past, new technologies for the future. American Journal of Medical Genetics Part C: Seminars in Medical Genetics. 2007;145 (4):335–345. doi: 10.1002/ajmg.c.30152. [DOI] [PubMed] [Google Scholar]
- Shaw J, Brown R, Heinrich P, Dunn S. Doctors’ experience of stress during simulated bad news consultations. Patient Education and Counseling. 2013;93(2):203–208. doi: 10.1016/j.pec.2013.06.009. [DOI] [PubMed] [Google Scholar]
- Srinivasan A, Bianchi DW, Huang H, Sehnert AJ, Rava RP. Noninvasive detection of fetal subchromosome abnormalities via deep sequencing of maternal plasma. The American Journal of Human Genetics. 2013;92(2):167–176. doi: 10.1016/j.ajhg.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark Z, Gillam L, Walker SP, McGillivray G. Ethical controversies in prenatal microarray. Current Opinion in Obstetrics and Gynecology. 2013;25(2):133–137. doi: 10.1097/GCO.0b013e32835ebb67. [DOI] [PubMed] [Google Scholar]
- Veach PM, Bartels DM, LeRoy BS. Coming full circle: a reciprocal-engagement model of genetic counseling practice. Journal of Genetic Counseling. 2007;16(6):713–728. doi: 10.1007/s10897-007-9113-4. [DOI] [PubMed] [Google Scholar]
- Wapner RJ, Martin CL, Levy B, Ballif BC, Eng CM, Zachary JM, et al. Chromosomal microarray versus karyotyping for prenatal diagnosis. New England Journal of Medicine. 2012;367(23):2175–2184. doi: 10.1056/NEJMoa1203382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weil J, Ormond K, Peters J, Peters K, Biesecker BB, LeRoy B. The relationship of nondirectiveness to genetic counseling: report of a workshop at the 2003 NSGC Annual Education Conference. Journal of Genetic Counseling. 2006;15(2):85–93. doi: 10.1007/s10897-005-9008-1. [DOI] [PubMed] [Google Scholar]
- White MT. “Respect for autonomy” in genetic counseling: An analysis and a proposal. Journal of Genetic Counseling. 1997;6(3):297–313. doi: 10.1023/a:1025628322278. [DOI] [PubMed] [Google Scholar]