Abstract
Background
This study aims to compare the image quality of second generation versus first generation 320-computed tomography coronary angiography (CTCA) in patients with heart rate ≥65 bpm as it has not been specifically reported.
Methods
Consecutive patients who underwent CTCA using second-generation-320-detector-row-CT were prospectively enrolled. A total of 50 patients with elevated (≥65 bpm) heart rate and 50 patients with controlled (<65 bpm) heart rate were included. Age and gender matched patients who were scanned with the first-generation-320-detector-row-CT were retrospectively identified. Image quality in each coronary artery segment was assessed by two blinded CT angiographers using the five-point Likert scale.
Results
In the elevated heart rate cohorts, while there was no significant difference in heart rate during scan-acquisition (66 vs. 69 bpm, P=0.308), or body mass index (28.5 vs. 29.6, P=0.464), the second generation scanner was associated with better image quality (3.94±0.6 vs. 3.45±0.8, P=0.001), and with lower radiation (2.8 vs. 4.3 mSv, P=0.009). There was no difference in scan image quality for the controlled heart rate cohorts.
Conclusions
The second generation CT scanner provides better image quality at lower radiation dose in patients with elevated heart rate (≥65 bpm) compared to first generation CT scanner.
Keywords: Image quality, computed tomography (CT), likert scale, 320-detector row, radiation dose
Introduction
Computed tomography coronary angiography (CTCA) is an established non-invasive imaging tool in assessing coronary artery disease (1). It is particularly useful for the exclusion of coronary artery disease because of its established high sensitivity and negative predictive value (2,3). Recently it has been shown to be a useful modality to assess patients with low to intermediate risk of suspected acute coronary syndromes presenting to the emergency department (4,5). To minimize radiation exposure, recent advances include the advent use of wide-detector scanners such as the 320 detector row scanner which has a 16 cm cranial-caudal coverage (6) and allows for acquisition of the whole coronary artery tree in one gantry rotation over less than one heartbeat (3,7).
The patients’ heart rate during image acquisition remains a critical determinant of radiation dose and image quality (8-10). Administration of beta blockers reduces heart rate and heart rate variability and results in better image quality (11). However, heart rate acceleration during image acquisition in response to intravenous contrast injection, anxiety and breath holding remains problematic (11-13). The ability to scan patients at higher heart rate with lower radiation exposure will significantly improve CTCA safety, applicability and may improve clinical efficiency. Compared to first generation 320 detector row scanner which has a gantry rotation time of 350 ms and a temporal resolution of 175 ms, the second generation detector row scanner has faster gantry rotation time of 275 ms and an improved temporal resolution of 137.5 ms. The image quality using second generation 320 detector-row CT scanner in patients with high heart rates during image acquisition when compared with the first generation 320 detector-row CT has not been specifically reported.
We hypothesize that the second generation 320-MDCT scanner with a combination of a faster gantry rotation, wide volume coverage, iterative reconstruction, automated exposure control and larger power generator provides better image quality with lower radiation exposure in patients with increased heart rate (≥65 bpm) compared to the first generation 320-MDCT scanner.
Methods
Study design
This study was carried out at a tertiary institution cardiac CT centre (Monash Medical Centre, Clayton, Australia). Consecutive patients who underwent CTCA with the second generation 320-MDCT (Aquilion ONE ViSION) scanner between November-December 2012 were included in this study. A total of 50 patients who had heart rate of ≥65 bpm at time of imaging were identified between 12 November 2012 and 18 December 2012 and were categorised into cohort 1. Another 50 patients who had heart rate of <65 bpm at time of imaging were identified between 12 November, 2012 and 3 December, 2012 and were categorised into cohort 3. We then retrospectively selected a cohort of patients with similar age and gender who were scanned with the first generation 320-MDCT (Aquilion ONE) scanner between September 2008 and October 2012. These patients were categorized as cohort 2 (heart rate ≥65 bpm) and cohort 4 (heart rate <65 bpm).
Study cohort
All patients who were clinically referred for CTCA at the institution during the study period were eligible for inclusion. Patients would be excluded if they were pregnant, less than 18 years of age, had estimated glomerular filtration less than 30 mL/min/1.73 m2 and had known contrast allergy. No patients met exclusion criteria.
Computed tomography protocol
Cardiovascular medications were ceased 48 hours prior to CTCA apart from beta-blockers. On arrival, an 18-gauge intravenous line was inserted in the right antecubital vein for administration of contrast. Oral and/or intravenous metoprolol was given if the resting heart rate was >60 bpm. If beta blocker was contraindicated, oral and/or intravenous ivabradine was given if the resting heart rate was >60 bpm. Cohort 1 and 3 patients were scanned on 320-detector row CT scanner (Aquilion ONE ViSION, Toshiba Medical Systems, Japan). Cohort 2 and 4 patients were scanned on the 320-detector-row CT scanner (Aquilion ONE, Toshiba Medical systems, Japan). The scan was acquired during injection of 75 mL of 100% Iohexal (Omnipaque 350) at 6 mL/s, followed by 50 mL of saline at 6 mL/s. Scanning was triggered manually when peak enhancement in the left ventricular cavity is achieved and no enhancement in the right ventricle is observed.
The scanning parameters on the Aquilion ONE ViSION scanner were: detector collimation 320 mm × 0.5 mm. The tube current was determined with use of automatic exposure control (SUREExposure3D, Toshiba Medical Systems) on the basis of X-ray attenuation on anterior-posterior and lateral scout images and the reconstruction kernel. Tube potential is manually set by the operator with the default set at 100 kVp, and is manually adjusted to 120 or 135 kVp when the automatic tube current selected is the maximum. The gantry rotation time was 275 ms and temporal resolution 137.5 ms. Prospective electrocardiogram gating was used covering 70-80% of the R-R interval. Images were reconstructed with a 512 × 512 matrix, 0.5 mm thick sections, and 0.25 mm increments by using kernel FC43, iterative reconstruction with adaptive iterative dose reduction 3D (AIDR3D, Toshiba Medical Systems) standard, and asymmetric cone bean reconstruction (14).
On the Aquilion ONE scanner the scanning parameters were: detector collimation 320 mm × 0.5 mm; tube current 300-500 mA [depending on body mass index (BMI)]; tube voltage 120 kV if BMI ≥25 (100 kV if BMI <25); gantry rotation time 350 ms; and temporal resolution 175 ms. Prospective electrocardiogram gating was used covering 70-80% of the R-R interval. Images scanned before August 2012 was reconstructed using the filtered back-projection technique with FCO4 algorithm while images scanned after August 2012 were reconstructed using AIDR 3D reconstruction.
For the first generation scanner, images acquired at heart rates ≤65 bpm, scanning was completed within a single R-R interval utilizing a 180º segment. In patients with a heart rate >65 bpm, data segments from two consecutive beats were used for multi-segment reconstruction. For the second generation scanner, if the heart rate was <70 bpm, scanning was completed within a single R-R interval utilizing a 180° segment. If the heart rate was ≥70 bpm, scanning was completed still within a single R-R interval utilizing a 180º segment but instead the window was widened to include systole and diastole (35-80%).
Analysis of image quality
Two experienced CT angiographers (DW and BK) evaluated the image quality on a per-segment basis using the 16 segment AHA model and each segment was rated by consensus agreement using a five point Likert scale. The Likert scale was defined as 1= poor, impaired image quality limited by excessive noise or poor vessel wall definition; 2= adequate, reduced image quality with poor vessel wall definition or excessive image noise, limitations in low contrast resolution remain evident; 3= good, impact of image noise, limitations of low contrast resolution and vessel margin definition are minimal; 4= very good, good attenuation of vessel lumen and delineation of vessel walls, relative image noise is minimal, coronary wall definition and low contrast resolution well maintained and 5= excellent, excellent attenuation of the vessel lumen and clear delineation of the vessel walls, limited perceived image noise (Figure 1) (15). Segments with diameter <1.5 mm or missing were not evaluated and were excluded from analysis.
Figure 1.
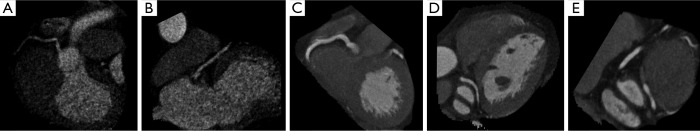
Examples of image quality according to Likert score (A-E).
Radiation dose estimation
The volume CT dose index (CTDI) and dose length product (DLP) were automatically generated by the machine and recorded for each patient during examination. Effective dose (ED, in units of mSv) was calculated using the formulate ED = DLP × k, where k is the conversion factor (k =0.014 mSv·mGy–1·cm–1) (8).
Statistical analysis
Continuous variables are expressed as mean ± SD or median (interquartile range) as appropriate, whereas categorical variables are expressed as percentage. Continuous and categorical variables were compared using t-test, Mann-Whitney or chi-square as appropriate. Interobserver variability was performed by calculating intraclass coefficient. Statistical analysis was performed with SPSS 20.0 (SPSS Inc, Chicago, IL, USA). A P value <0.05 was considered statistically significant.
Results
Clinical characteristics
Two hundred subjects were studied (50 patients in group 1, 2, 3 and 4 respectively). The mean age was 58.1±1.8 years in cohort 1; 58.3±1.8 years in cohort 2; 60.5±1.6 years in cohort 3; and 60.5±1.6 in cohort 4. There were 92 (46%) males. The patient characteristics are summarized in Table 1. A total of 2831 coronary segments were evaluated after exclusion of missing segments or if the size was too small (<1.5 mm in diameter).
Table 1. Baseline characteristics.
| Cohort 1 (n=50), 2nd generation scanner, HR ≥65 bpm | Cohort 2 (n=50), 1st generation scanner, HR ≥65 bpm | Cohort 3 (n=50), 2nd generation scanner, HR <65 bpm | Cohort 4 (n=50), 1st generation scanner, HR <65 bpm | P value | |
|---|---|---|---|---|---|
| Mean age ± SD | 58.1±1.8 | 58.3±1.8 | 60.5±1.6 | 60.5±1.6 | 0.61 |
| Male | 20 (40%) | 22 (44%) | 25 (50%) | 25 (50%) | 0.57 |
| BMI ± SD | 28.5±1.1 | 29.6±1.0 | 28.3±0.8 | 28.6±1.0 | 0.8 |
| Hypertension | 29 (58%) | 22 (44%) | 30 (60%) | 27 (54%) | 0.34 |
| Hypercholesterolemia | 28 (56%) | 20 (40%) | 22 (44%) | 30 (60%) | 0.31 |
| Diabetes mellitus | 13 (26%) | 5 (10%) | 7 (14%) | 12 (24%) | 0.27 |
| Smoking | 22 (44%) | 12 (24%) | 19 (38%) | 16 (32%) | 0.31 |
| Family history of ischaemic heart disease | 33 (66%) | 14 (28%) | 25 (50%) | 24 (48%) | 0.004 |
| Coronary stent | 1 (2%) | 0 (0%) | 1 (2%) | 0 (0%) | 0.57 |
| Previous coronary artery bypass surgery | 0 (0%) | 0 (0%) | 2 (4%) | 0 (0%) | 0.11 |
| Oral metoprolol | 32 (64%) | 40 (80%) | 22 (44%) | 21 (42%) | 0.04 |
| Intravenous metoprolol | 5 (10%) | 15 (30%) | 1 (2%) | 2 (4%) | <0.001 |
| Oral Ivabradine | 11 (22%) | 10 (20%) | 4 (8%) | 3 (6%) | 0.046 |
| Number of segments with >50% stenosis | 0.9±1.5 | 0.5±1.1 | 0.8±1.2 | 0.7±1.0 | 0.452 |
Overall, hypertension, hypercholesterolemia and family history were the most common associated risk factors and majority of patients were overweight with a mean BMI of 28-29 across all groups. At baseline, 120 of the 200 patients (60%) were given oral beta-blockers. More patients in the elevated heart rate cohorts (1 and 2) were given intravenous metoprolol (P<0.001) and oral ivabradine (P=0.046).
CT parameters
As shown in Table 2, there were no statistically significant difference in heart rate during acquisition between cohort 1 and 2 (66±14.7 vs. 69±14.4 bpm, P=0.308) and between cohort 3 and 4 (56±6.3 vs. 55±6.4 bpm, P=0.6). Majority of patients in the elevated heart rate cohorts, had heart rate between 65-75 bpm, with only 4 patients in cohort 1 and 5 patients in cohort 2 having heart rate of >75 bpm. Compared to first generation scanner, a significantly higher proportion of patients was scanned using lower tube potential of 100 kV using the second generation scanner. Overall, majority of scans were completed with one gantry rotation, with more patients requiring greater than one rotation in the higher heart rate groups.
Table 2. CT scanning parameters.
| Cohort 1 (n=50), 2nd generation scanner, HR ≥65 bpm | Cohort 2 (n=50), 1st generation scanner, HR ≥65 bpm | Comparison of cohort 1 vs. cohort 2, (P value) | Cohort 3 (n=50), 2nd generation scanner, HR <65 bpm | Cohort 4 (n=50), 1st generation scanner, HR <65 bpm | Comparison of cohort 3 vs. cohort 4, (P value) | |
|---|---|---|---|---|---|---|
| Heart rate at acquisition | 66±14.7 | 69±14.4 | 0.308 | 56±6.3 | 55±6.4 | 0.6 |
| Heart rate 65-75 bpm | 46 (92%) | 45 (90%) | 0.9 | 0 (0%) | 0 (0%) | 1 |
| Tube potential (100 kV) | 34 (68%) | 14 (28%) | 0.003 | 35 (70%) | 17 (34%) | 0.001 |
| Tube potential (120 kV) | 14 (28%) | 28 (46%) | 14 (28%) | 25 (50%) | ||
| Average tube potential | 107±10.7 | 117±13 | <0.001 | 106±9.8 | 116±13 | 0.001 |
| Average tube current | 630 (312) | 149 (491) | <0.001 | 580 (170) | 130 (216) | <0.001 |
| One beat scan (one gantry rotation) | 46 (92%) | 43 (86%) | 0.63 | 49 (98%) | 48 (96%) | 1 |
| Radiation dose (mSv) | 2.8 (2.7) | 4.5 (6) | 0.009 | 2.1 (1.3) | 3.4 (3.7) | 0.04 |
| AIR3D reconstruction | 50 (100%) | 38 (76%) | <0.001 | 50 (100%) | 44 (88%) | 0.027 |
Radiation dose
Patients scanned using the second generation scanner received significantly lower radiation dose (Table 2). When compared with the first generation scanner, the median estimated effective dose with the second-generation scanner was 35% less in the higher heart rate group (2.8 vs. 4.3 mSv, P=0.009) and 34% less in the controlled heart rate group (2.1 vs. 3.2 mSv, P=0.04).
Image quality
The scan image quality was better on the second generation scanner in patients with higher rate (≥65 bpm) compared to the first generation scanner (3.94±0.6 vs. 3.45±0.8, P=0.001) (Table 3). Otherwise there was no statistically significant difference in scan image quality between second and first generation scanner in patients with heart rate <65 bpm (4.11±1.5 vs. 3.73±0.4, P=0.091). Patients scanned with the second generation scanner had less median number of poor segments (Likert score of 1 or 2) per patient in the higher heart rate cohorts (0 vs.1, P=0.016) but not in the controlled heart rate cohorts (0 vs. 0, P=0.581).
Table 3. Comparison of image quality between groups.
| Likert scale | P value | Median (IQR) number of poor segments | P value | |
|---|---|---|---|---|
| Group 1 (2nd generation scanner, HR ≥65 bpm) | 3.94±0.6 | 0.001 | 0 [1] | 0.016 |
| Group 2 (1st generation scanner, HR ≥65 bpm) | 3.45±0.8 | 1 [2] | ||
| Group 3 (2nd generation scanner, HR <65 bpm) | 4.11±1.5 | 0.091 | 0 [0] | 0.581 |
| Group 4 (1st generation scanner, HR <65 bpm) | 3.73±0.4 | 0 [0] |
Interobserver variability
The interobserver variability for Likert score analysis was highly reproducible between observers in 100 randomly selected segments. The intraclass correlation coefficient was 0.9 (P<0.001).
Discussion
This study demonstrated that the second generation 320-CT scanner has the ability to provide better image quality at lower radiation dose compared to the first generation 320-MDCT scanner in patients with elevated heart rate (≥65 bpm). In addition, we showed that there was no statistical difference in image quality between the second generation and first generation 320-CT scanner in patients with controlled heart rate (<65 bpm). Recently Chen and colleagues demonstrated that the newer generation 320-MDCT scanner provided excellent image quality at lower radiation exposure across a wide range of body habitus and heart rate compared to the first generation 320-MDCT scanner. The majority of patients (78.5%) had heart rate <65 bpm in that study (16). Similarly, a retrospective study by Tomizawa demonstrated that the second generation 320-MDCT scanner tended to have superior image quality with reduced radiation exposure in the higher heart rate [66-75] group compared to the first generation 320-MDCT scanner, but it did not reach statistical significance (17). To the best of our knowledge, no other study has specifically explored whether the new generation scanner could provide better image quality at lower radiation dose in patients with elevated heart rate (≥65 bpm).
Image quality of CTCA depends on multiple key aspects of the imaging process (1). There are CT related parameters, including temporal resolution, tube potential, tube current and scan reconstruction methods. On the other hand patient related factors such as heart rate during acquisition and BMI also affect image quality. In this study, despite using low tube potential in cohorts of patients whom heart rate and BMI did not differ, the second generation 320 detector-row CT produced better image quality than the first generation scanner. We therefore postulate that the improvement in image quality is due to a combination of improved temporal resolution and scan reconstruction methods used in the second generation 320 detector-row CT.
The faster gantry rotation time of 275 ms in combination with up to 16 cm cranial-caudal volume coverage per rotation on the second generation 320 detector-row CT scanner enables single heart beat acquisitions in patients with heart rates of up to 75 beats per minute (16), as compared to up to 65 beats per minute from the first generation 320-MDCT scanner with a gantry rotation time of 350 ms (18). Also, the second generation scanner could produce a high tube current when low tube potential was used, thus images with similar contrast to noise ratios could be reconstructed with lower radiation dose. This allows better temporal uniformity of the image including more uniform contrast enhancement and the absence of misalignment artefacts in the z-direction (19). The second generation 320 detector-row scanner by permitting higher proportion of patients (46/50) with elevated heart rate to be imaged with one heart-beat acquisitions improved the overall image quality while maintaining low radiation in our study. It is however still prudent to emphasize that faster heart rate still resulted in inferior image quality and higher radiation dose despite advancement with wider volume scanners with 320-detector rows compared to patients with low heart rate (20,21). Therefore good heart rate control with beta-blockers remains an important strategy in achieving good image quality and low radiation dose (22). We advocate adherence to the current guidelines of employing appropriate rate lowering strategies prior to scanning. However, in cases where lower heart rate could not be achieved due to symptoms or hypotension, or unexpected acceleration of heart rate during acquisitions, the second generation 320 detector-row CT scanner would still likely to produce good quality images.
Patients with elevated heart rate (≥65 bpm) scanned with second generation 320-MDCT scanner had 35% reduction in median radiation dose while patients with heart rate <65 bpm had 34% reduction compared to the first generation 320-MDCT scanner. Despite having similar patient related factors (BMI, heart rate at acquisition) and CT related factors (prospective ECG gated imaging, one beat scan), the second generation scanner achieved lower radiation exposure compared to first generation scanner because of the following three factors: (I) lower tube potential (II) more third generation iterative reconstruction (AIDR3D) and (III) improved temporal resolution.
Tube potential determines the energy of the x-ray beam, which affects its penetrability and noise (8). A reduction in tube potential from 120 to 100 kV results in a 31% reduction in radiation dose (23) but a 20% increase in noise (8), if all other parameters are unchanged. In practice, to counter the negative effect of image noise by using lower tube potential, an increase in tube current maybe necessary. Around 70% of patients scanned with the second generation 320-MDCT scanner used a tube potential of 100 kV as compared to around 30% using the first generation scanner owing to the availability of a larger x-ray generator (100 kW) that can produce up to 900 mA (16). This reduction in tube potential resulted in reduced radiation exposure while maintaining image quality in our study.
One strategy to decrease radiation exposure is to employ noise-reducing iterative reconstruction algorithms (24). Iterative reconstructions can produce higher resolution images and reduced imaging artefacts and were adopted by CTCA in recent years (25). The use of adaptive iterative dose reduction in three-dimensions (AIDR3D) reconstruction is capable of achieving up to 50% radiation reduction while maintaining comparable image quality compared to filtered back projection techniques (26). The combination of AIDR3D and automated exposure control markedly reduced radiation exposure by utilisation of low tube potential while decreasing the associated noise problem. In our study, all patients scanned with second generation scanner had AIDR3D reconstruction as compared to 82% of those scanned with the first generation scanner.
Limitations
This is an observational single centre experience with limited number of patients in each cohorts. The image quality tested was limited to patients with a heart rate between 65-75 bpm, and the effect of higher heart rate remains to be studied. The diagnostic accuracy of the second generation 320-detector row CT compared to invasive angiography will need further evaluation but studies from first generation scanner showed highly comparable results (3,7,21).
Conclusions
Based on the results of the study, the CTCA images performed using the second generation 320-CT scanner were superior in quality and required a lower radiation dose in patients with elevated heart rate (≥65 bpm) when compared with the first generation 320-CT scanner.
Acknowledgements
DW and BK are supported by Australian NHF Post-Doctoral Fellowship and Robertson Family Fellowship.
Disclosure: The authors declare no conflict of interest.
References
- 1.American College of Cardiology Foundation Task Force on Expert Consensus Documents , Mark DB, Berman DS, et al. ACCF/ACR/AHA/NASCI/SAIP/SCAI/SCCT 2010 expert consensus document on coronary computed tomographic angiography: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Circulation 2010;121:2509-43 [DOI] [PubMed] [Google Scholar]
- 2.Budoff MJ, Dowe D, Jollis JG, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol 2008;52:1724-32 [DOI] [PubMed] [Google Scholar]
- 3.Nasis A, Leung MC, Antonis PR, et al. Diagnostic accuracy of noninvasive coronary angiography with 320-detector row computed tomography. Am J Cardiol 2010;106:1429-35 [DOI] [PubMed] [Google Scholar]
- 4.Litt HI, Gatsonis C, Snyder B, et al. CT angiography for safe discharge of patients with possible acute coronary syndromes. N Engl J Med 2012;366:1393-403 [DOI] [PubMed] [Google Scholar]
- 5.Ollendorf DA, Kuba M, Pearson SD. The diagnostic performance of multi-slice coronary computed tomographic angiography: a systematic review. J Gen Intern Med 2011;26:307-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rybicki FJ, Otero HJ, Steigner ML, et al. Initial evaluation of coronary images from 320-detector row computed tomography. Int J Cardiovasc Imaging 2008;24:535-46 [DOI] [PubMed] [Google Scholar]
- 7.Dewey M, Zimmermann E, Deissenrieder F, et al. Noninvasive coronary angiography by 320-row computed tomography with lower radiation exposure and maintained diagnostic accuracy: comparison of results with cardiac catheterization in a head-to-head pilot investigation. Circulation 2009;120:867-75 [DOI] [PubMed] [Google Scholar]
- 8.Halliburton SS, Abbara S, Chen MY, et al. SCCT guidelines on radiation dose and dose-optimization strategies in cardiovascular CT. J Cardiovasc Comput Tomogr 2011;5:198-224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weustink AC, Neefjes LA, Kyrzopoulos S, et al. Impact of heart rate frequency and variability on radiation exposure, image quality, and diagnostic performance in dual-source spiral CT coronary angiography. Radiology 2009;253:672-80 [DOI] [PubMed] [Google Scholar]
- 10.Steigner ML, Otero HJ, Cai T, et al. Narrowing the phase window width in prospectively ECG-gated single heart beat 320-detector row coronary CT angiography. Int J Cardiovasc Imaging 2009;25:85-90 [DOI] [PubMed] [Google Scholar]
- 11.Leschka S, Wildermuth S, Boehm T, et al. Noninvasive coronary angiography with 64-section CT: effect of average heart rate and heart rate variability on image quality. Radiology 2006;241:378-85 [DOI] [PubMed] [Google Scholar]
- 12.Svensson A, Ripsweden J, Rück A, et al. Heart rate variability and heat sensation during CT coronary angiography: Low-osmolar versus iso-osmolar contrast media. Acta Radiol 2010;51:722-6 [DOI] [PubMed] [Google Scholar]
- 13.Kang EJ, Lee J, Lee KN, et al. An initial randomised study assessing free-breathing CCTA using 320-detector CT. Eur Radiol 2013;23:1199-209 [DOI] [PubMed] [Google Scholar]
- 14.Van der Molen AJ, Joemai RM, Geleijns J. Performance of longitudinal and volumetric tube current modulation in a 64-slice CT with different choices of acquisition and reconstruction parameters. Phys Med 2012;28:319-26 [DOI] [PubMed] [Google Scholar]
- 15.Leipsic J, Labounty TM, Heilbron B, et al. Adaptive statistical iterative reconstruction: assessment of image noise and image quality in coronary CT angiography. AJR Am J Roentgenol 2010;195:649-54 [DOI] [PubMed] [Google Scholar]
- 16.Chen MY, Shanbhag SM, Arai AE. Submillisievert median radiation dose for coronary angiography with a second-generation 320-detector row CT scanner in 107 consecutive patients. Radiology 2013;267:76-85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tomizawa N, Maeda E, Akahane M, et al. Coronary CT angiography using the second-generation 320-detector row CT: assessment of image quality and radiation dose in various heart rates compared with the first-generation scanner. Int J Cardiovasc Imaging 2013;29:1613-8 [DOI] [PubMed] [Google Scholar]
- 18.Hsiao EM, Rybicki FJ, Steigner M. CT coronary angiography: 256-slice and 320-detector row scanners. Curr Cardiol Rep 2010;12:68-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Halliburton S, Arbab-Zadeh A, Dey D, et al. State-of-the-art in CT hardware and scan modes for cardiovascular CT. J Cardiovasc Comput Tomogr 2012;6:154-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yu SJ, Zhang L, Chen YF, et al. Effects of heart rate on image quality and radiation dose of “triple rule-out” 320-row-640-slice multidetector computed tomography scan in patients with acute chest pain. Zhonghua Yi Xue Za Zhi 2012;92:2652-5 [PubMed] [Google Scholar]
- 21.Sun G, Li M, Jiang XS, et al. 320-detector row CT coronary angiography: effects of heart rate and heart rate variability on image quality, diagnostic accuracy and radiation exposure. Br J Radiol 2012;85:e388-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mahabadi AA, Achenbach S, Burgstahler C, et al. Safety, efficacy, and indications of beta-adrenergic receptor blockade to reduce heart rate prior to coronary CT angiography. Radiology 2010;257:614-23 [DOI] [PubMed] [Google Scholar]
- 23.Bischoff B, Hein F, Meyer T, et al. Impact of a reduced tube voltage on CT angiography and radiation dose: results of the PROTECTION I study. JACC Cardiovasc Imaging 2009;2:940-6 [DOI] [PubMed] [Google Scholar]
- 24.Thibault JB, Sauer KD, Bouman CA, et al. A three-dimensional statistical approach to improved image quality for multislice helical CT. Med Phys 2007;34:4526-44 [DOI] [PubMed] [Google Scholar]
- 25.Leipsic J, Heilbron BG, Hague C. Iterative reconstruction for coronary CT angiography: finding its way. Int J Cardiovasc Imaging 2012;28:613-20 [DOI] [PubMed] [Google Scholar]
- 26.Chen MY, Steigner ML, Leung SW, et al. Simulated 50% radiation dose reduction in coronary CT angiography using adaptive iterative dose reduction in three-dimensions (AIDR3D). Int J Cardiovasc Imaging 2013;29:1167-75 [DOI] [PMC free article] [PubMed] [Google Scholar]


