Sir,
Urinary tract infections (UTIs) are one of the most common infections encountered by physicians. The study was carried out to know the common bacteria causing UTI and their resistance pattern to commonly prescribed antibiotics at our hospital.
Patients were assigned into two categories: one group comprising of urine samples from patients admitted in the hospital for at least 48 h (hospital acquired urinary tract infection or HA-UTI), and another group comprising of urine samples from patients visiting the hospital on an outpatient basis or admitted for lesser than 48 h (community acquired urinary tract infection or CA-UTI).[1] Urine samples (1,378) were collected between 1st January 2012 and 30th June 2012 from cases suspected of having CA-UTI and HA-UTI. Patients were instructed to submit first morning mid stream clean catch urine (CCMS) samples; from catheterized indoor patients samples were collected by healthcare workers after disinfecting the port with 70% alcohol and then aspirating urine through the port with a sterile needle and syringe. The samples were processed as per standard procedures; antibiotic susceptibility testing was performed by the Kirby Bauer disc diffusion method as per Clinical and Laboratory Standards Institute (CLSI) recommendations.[2,3] Statistical analysis was done using Fisher's exact test. P value lesser than 0.05 was considered as statistically significant.
Results obtained in this study are shown in Tables 1 and 2. Of the 1,378 urine samples processed during the study period, 340 (24.7%) yielded urinary pathogens, of which 324 had significant bacteriuria and 16 had Candiduria. Gram-negative bacilli accounted for 281 (82%), gram-positive cocci for 43 (13%) and Candida sp. for 16 (5%) of the total pathogens. Escherichia coli was the predominant pathogen in both CA-UTI and HA-UTI cases. The next top 5 uropathogens after E. coli, causing HA-UTI in our hospital were Pseudomonas aeruginosa 21(17%); Candida sp. 14 (11.0%); Klebsiella sp. 11 (9%); Citrobacter sp. 10 (8%); and Enterococcus sp. 8 (7%), while those causing CA-UTI were Citrobacter sp. 18(8%); Klebsiella pneumoniae 17(8%); Enterococcus sp. 16(7%); Staphylococcus sp. 14 (6%) and Enterobacter sp. 9 (4%). E. coli was statistically associated more with CA-UTI and P. aeruginosa was statistically associated more with HA-UTI.
Table 1.
Frequency, percentage, and P-value of resistant gram-negative bacteria isolated from CA-UTI versus HA-UTI patients
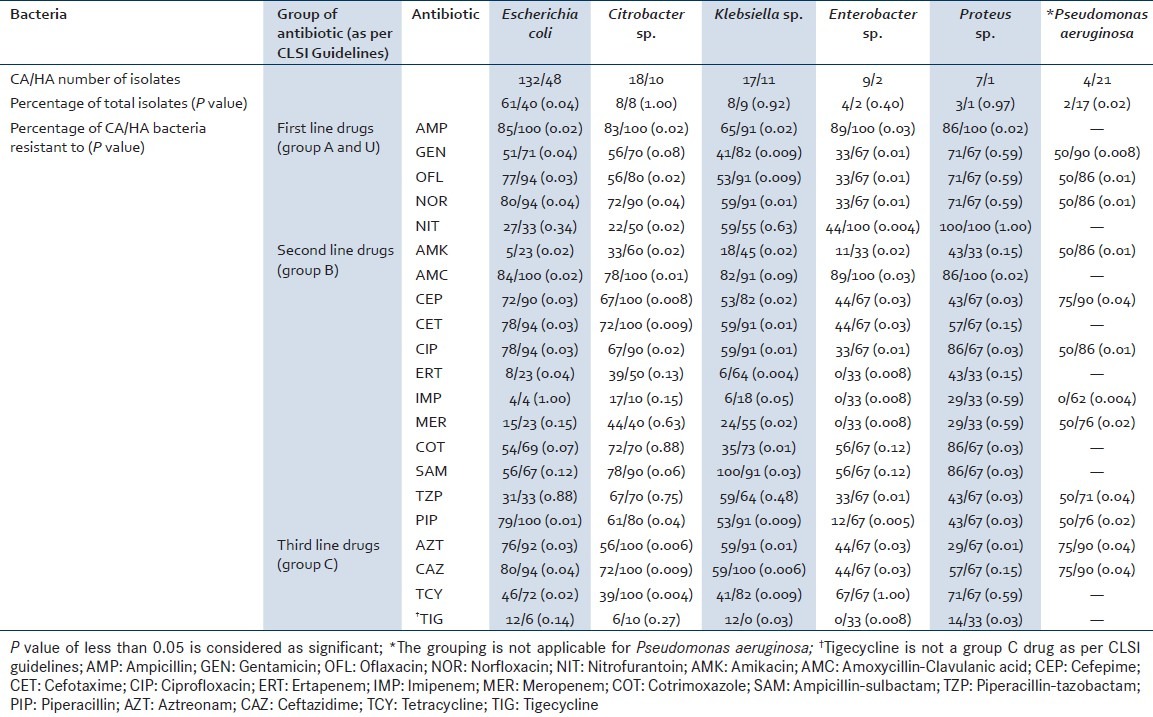
Table 2.
Frequency, percentage and P-value of resistant gram-positive bacteria isolated from CA-UTI versus HA-UTI patients
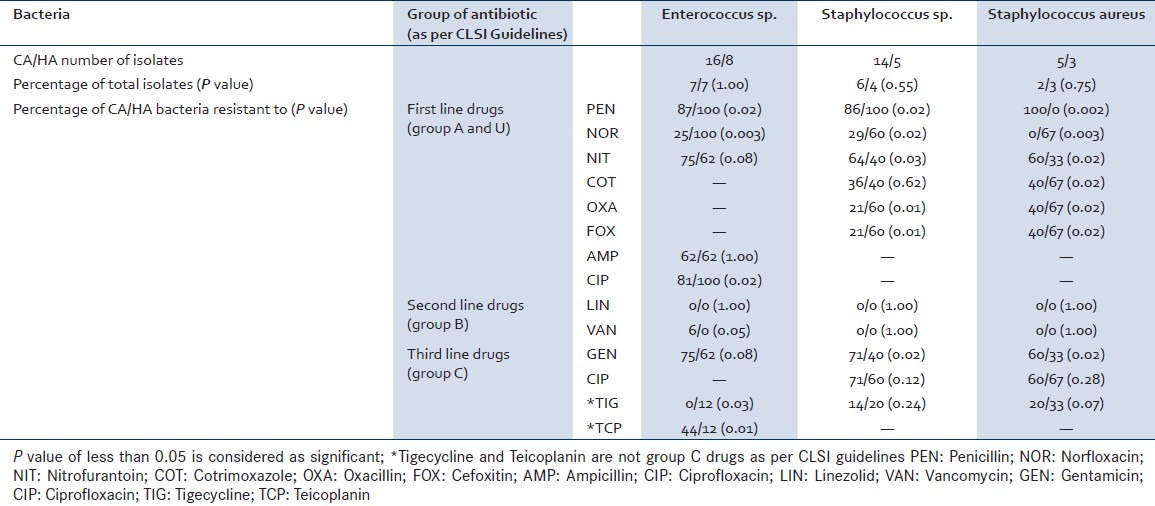
Resistance to ampicillin was more significantly associated with HA-UTI than CA-UTI among all the gram-negative pathogens. In case of P. aeruginosa, resistance to ceftazidime, cefepime, and aztreonam were more significantly associated with HA-UTI than CA-UTI. Among Staphylococcus aureus isolates, resistance was more significantly associated with HA-UTI than CA-UTI against cefoxitin, co-trimoxazole, and norfloxacin.
Our data indicates that E. coli is still the most frequent uro-pathogen causing UTI in the community and hospital settings, which is consistent with the literature.[4] The resistance rates of the isolates were significantly lower in outpatients than those of inpatients, a finding which is consistent with observations all over the world.[5]
Ampicillin, amoxicillin-clavulanic acid, TMP-SMX and ciprofloxacin did not have good in vitro coverage for many of the uro-pathogens isolated in this study. Nitrofurantoin is the only oral agent that remains relatively active against most uro-pathogens. Carbapenems, piperacillin-tazobactam, and amikacin showed good in vitro coverage of the uro-pathogens isolated in this study.
REFERENCES
- 1.Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC Definitions for Nosocomial Infections. In: Olmsted RN, editor. APIC Infection control and applied epidemiology: Principles and Practice. St Louis: Mosby; 1996. pp. A1–20. [Google Scholar]
- 2.Forbes BA, Sahm DF, Weissfeld AS, editors. Bailey and Scott's Diagnostic Microbiology. 12th ed. St. Louis Missouri: Mosby; 2007. Infections of the Urinary Tract; pp. 842–55. [Google Scholar]
- 3.Performance Standards for Antimicrobial Susceptibility Testing. 22nd informational supplement. Wayne: CLSI; 2012. Clinical and Laboratory Standards Institute. [Google Scholar]
- 4.Benwan KA, Sweigh NA, Rotimi VO. Etiology and susceptibility patterns of community- and hospital acquired urinary tract infections in a general hospital in Kuwait. Med Princ Pract. 2010;19:440–6. doi: 10.1159/000320301. [DOI] [PubMed] [Google Scholar]
- 5.Gupta K, Scholes D, Stamm WE. Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA. 1999;281:736–8. doi: 10.1001/jama.281.8.736. [DOI] [PubMed] [Google Scholar]


