Abstract
Imaging of the temporomandibular joint (TMJ) is continuously evolving with advancement of imaging technologies. Many different imaging modalities are currently used to evaluate the TMJ. Magnetic resonance imaging is commonly used for evaluation of the TMJ due to its superior contrast resolution and its ability to acquire dynamic imaging for demonstration of the functionality of the joint. Computed tomography and ultrasound imaging have specific indication in imaging of the TMJ. This article focuses on state of the art imaging of the temporomandibular joint. Relevant normal anatomy and biomechanics of movement of the TMJ are discussed for better understanding of many TMJ pathologies. Imaging of internal derangements is discussed in detail. Different arthropathies and common tumors are also discussed in this article.
Keywords: Temporomandibular joint, Magnetic resonance imaging, Imaging, Computed tomography, Anatomy, Pathologies
Core tip: “Imaging of the temporomandibular joint: An update” is a thorough review of the imaging techniques and imaging appearances of normal anatomy, anatomic variation and pathologies of the temporomandibular joint (TMJ). Numerous images are appropriately used for illustration of the key concepts of TMJ imaging. Nice blend of exquisite details and beautiful illustrative images is the main feature of this article. The purpose of this article is easy understanding of many difficult aspects of imaging of the TMJ.
INTRODUCTION
Pain related to the temporomandibular joint (TMJ) is common in the general population. Only about 3%-7% of the patients with pain related to TMJ seek medical attention[1,2]. Although TMJ disorders or dysfunctions are the most common clinical conditions for imaging referrals, pathologies specific to the bone and the joints are also common. Different imaging modalities are available to image the TMJ, each with inherent strengths and weaknesses. Magnetic resonance imaging (MRI) is the most widely used and is diagnostic technique of choice. In this article, we review the imaging techniques, anatomy pathology involving the TMJ with special emphasis on MRI findings.
Embryology and development of TMJ
The TMJ is one of the last diarthrodial joints to appear in utero and does not emerge in the craniofacial region until the 8th week of gestation. The maxilla, mandible, muscles of mastication, and biconcave disc develop embryologically from the first branchial arch through the 14th week of gestation. The TMJ is considerably underdeveloped at birth in comparison to other diarthrodial joints making it susceptible to perinatal and postnatal insults. The joint continues developing in the early childhood years as the jaw is utilized for sucking motions and eventually chewing.
ANATOMY OF TMJ
The TMJ is a ginglymoarthrodial synovial joint (latin:ginglymus = hinge joint) that allows both backward and forward translation as well as a gliding motion[3]. Similar to the other synovial joints in the body, the TMJ has a disk, articular surfaces, fibrous capsule, synovial fluid, synovial membrane, and ligaments. What makes this joint unique is the articular surfaces are covered by fibrocartilage instead of hyaline cartilage. The articular surfaces of the TMJ are formed inferiorly by the mandibular condyle and superiorly by the glenoid fossa (also known as mandibular fossa) and articular eminence of the temporal bone.
Articular surfaces
The mandibular component consists of the ovoid condylar process that is 15-20 mm wide in the transverse dimension and 8-10 mm wide in the antero-posterior dimension[3]. The appearance of the mandibular condyle is extremely variable between patients and in different age groups.
The cranial component of the TMJ lies below the squamous portion of the temporal bone anterior to tympanic plate. The articular fossa is formed entirely by the squamous portion of the temporal bone. The posterior part of the articular fossa is elevated to form the posterior articular ridge. In most individuals the posterior articular ridge becomes thicker on the lateral aspect and forms a cone shaped projection known as postglenoid process (PGP). The tympanosquamosal fissure lies at the posterior and lateral part of the glenoid fossa, between the squamous and tympanic portion of the petrous bone and separates the articular surface form the nonarticular surface of the glenoid fossa. Along the medial aspect of the glenoid fossa is the petrotympanic fissure anteriorly and the petrosquamous fissure posteriorly. The articular eminence (AE) forms the anterior boundary of the glenoid fossa. The AE is a transverse bony bar anterior to the glenoid fossa and medial to the posterior margin of the zygomatic process. The anterior slope of the AE is known as the preglenoid plane (PEP) and rises gently from the infratemporal surface of the squamous bone. The mandibular condyle and the articular disk travel anteriorly to the summit of the AE and onto PEP during wide mouth opening. The gentle anterior slope facilitates smooth backward movement of the condyle and disk from the anterior position back to neutral position. The articular tubercle is a small bony knob at the lateral aspect of the AE where the lateral collateral ligament attaches. The lateral border of glenoid fossa is slightly raised from the fossa joining the anterior tubercle with the PGP (Figure 1).
Figure 1.
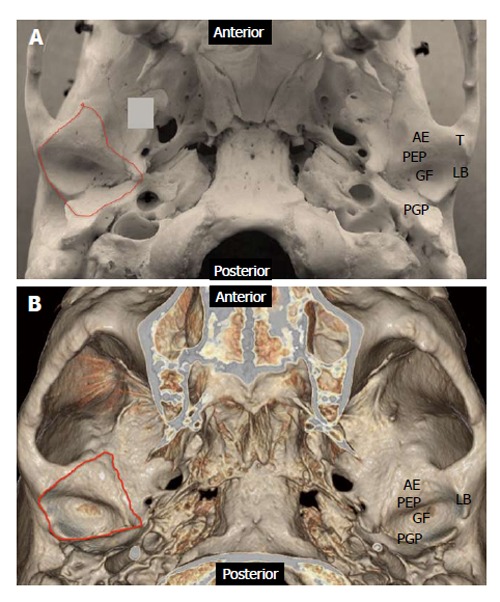
Anatomy of the cranial component of temporomandibular joint. A: Photograph of skull specimen; B: 3-D volume rendered image obtained from a temporal bone Redline demonstrates the capsular attachment. AE: Articular eminence; GF: Glenoid fossa; LB: Lateral border; PEP: Preglenoid plane; PGP: Postglenoid plane; T: Tubercle.
Articular disk
The articular disk is round or oval, biconcave, avascular fibrocartilage between the condyle and glenoid fossa. The disk is considerably thinner centrally in the intermediate zone. The triangular anterior band is approximately 2 mm in thickness and blends with the joint capsule. The posterior band is approximately 3 mm in thickness and continues as bilaminar zone (also known as retrodiscal region and posterior attachment), which consists of superior fibroelastic layer (also known as temporal lamina) that attaches to PGP and an inferior fibrous layer (also known as the inferior lamina) that attaches to the posterior condylar neck. The superior layer prevents slipping of the disk during wide mouth opening and the inferior layer prevents excessive rotation of the disk over the condyle. Both the lamina are separated by loose elastic fibers with blood vessels and nerves. These fibers attach to the posterior joint capsule and augments disk retraction during mouth closing. The bands are longer in the mediolateral dimension than in the antero-posterior dimension[4]. The smaller anterior band attaches anteriorly to the joint capsule, condylar head, and AE. Some patients have an additional antero-medial attachment to the superior belly of the lateral pterygoid muscle. Unlike its anterior and posterior attachments, the disk is not attached to the joint capsule medially and laterally. Instead, the disk is firmly attached to the medial and lateral poles of the mandibular condyle. This allows simultaneous movements of the disk and the condyle (Figure 2).
Figure 2.
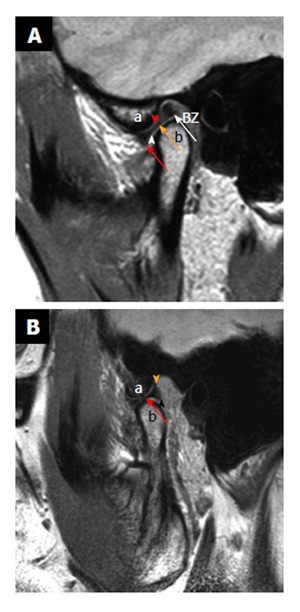
Normal anatomy. Sagittal proton density weighted closed mouth and open mouth view of magnetic resonance imaging. A: On the closed mouth view, the disk is located posterior to the articular eminence (the letter, a). It can be noted that the “bow-tie” shape of the disk: Thicker anterior band (red arrow) and posterior band (white arrow) with a thinner central zone (orange arrow). Bilaminar zone (BZ) is located posterior to the posterior band. It can also be noted that the inferior joint compartment (white arrowhead) between the disk and the mandibular condyle (the letter, b) and superior joint compartment (red arrowhead) between the articular eminence and the disk; B: On the open mouth view (in a different patient), the thinner intermediate zone (red arrow) of the disk is interposed between the articular eminence (the letter, a) and the condylar head (the letter, b) in a “bow-tie” fashion. Orange arrowhead demonstrates temporal lamina and black arrowhead indicate inferior lamina.
Muscles
The muscles of mastication (medial and lateral pterygoids, masseter, and temporalis) in addition to other accessory muscles help opening and closing of the jaw[4-6]. The lateral pterygoid in conjunction to the stylohyoid, mylohyoid and geniohyoid muscles is used to open the jaw. The temporalis, medial pterygoid, and masseter muscles close the jaw. The lateral pterygoid, part of the masseter muscle and the medial pterygoid assist in the anterior translation of the mandible. The protrusive muscles (helping forward movement) are used alternately to move the jaw laterally from side to side. Individual muscle origins and attachments are listed below[4,6].
Jaw-closing muscles/adductors
The masseter is the strongest muscle of mastication and has two parts that blend together anteriorly. The superficial part originates from the anterior two-thirds of the zygomatic arch and inserts on the lower one-third of the lateral surface of the mandibular ramus. The deep part originates from the entire zygomatic arch and inserts on the upper two-thirds of the ramus.
The medial pterygoid courses parallel to the masseter along the medial aspect of the mandible. The anterior part arises from the lateral surface of the palatine pyramidal process and the maxillary tuberosity. The posterior part originates from the pterygoid fossa and the medial surface of the lateral pterygoid plate. The medial pterygoid inserts on the inferomedial surface of the mandibular ramus.
The temporalis muscle originates from the temporalis fossa and inserts on the coronoid process and inner side of the mandibular ramus. The fibers also attach directly to the medial side of the coronoid process and ramus.
Jaw-opening muscles/abductors
The lateral pterygoid muscle has two bellies. The superior belly originates from the infratemporal surface of the greater wing of sphenoid. The inferior belly originates from the lateral surface of the lateral pterygoid plate. There is a wide gap between the two heads of the lateral pterygoid muscle that come together anterior to the TMJ. The fibers from the superior head primarily attach to the anteromedial surface of the mandibular neck at the pterygoid fovea. Additionally, in some patients part of the superior head directly attaches to the superomedial aspect of the joint capsule and extends to the anteromedial aspect of the articular surface. All of the fibers of the inferior head attach to the pterygoid fovea. Variability in the attachment of the lateral pterygoid muscle is reported with insertions of the muscle described only to the condyle or to the condyle, capsule, and the disk[7-9].
The superior belly helps maintain the physiologic position of the disk in the open mouth position. This is accomplished by pulling the disk forward with a combined translation and rotation while exerting forward pressure on both the condyle and the disk thus stabilizing their relationship to each other. The inferior belly pulls the condyle forward out of the fossa. When the inferior belly alternately contracts, this produces lateral movement of the jaw.
The digastric muscle has a posterior and an anterior belly united by an conjoined tendon. The posterior belly is attached to the mastoid process of the temporal bone and extends to the hyoid bone becoming continuous with the intermediate tendon. A fibrous loop attached to the hyoid holds the tendon in place. The anterior belly extends from the tendon to the digastric fossa on the lower aspect of mandible near the symphysis. Contraction of the digastric muscles pulls the symphysis menti backwards producing the retrusive and opening movements of the mandible.
The geniohyoid, myolohyoid, stylohyoid and infrahyoid muscles also have supportive role in mandibular movements that are beyond the scope of this review.
Biomechanics of TMJ movements
Jaw movement involves a high level of interaction and coordination between bilateral mandibular condyles, disk, muscles, and ligaments of the joints. The functional interactions within the TMJ are complex and incompletely understood[10,11]. A simplistic view of the complex interactions in open and closed mouth positions is described below.
In a normal joint, the thin intermediate zone of the disk is always interposed between the condyle and the temporal bone in both the closed-mouth and open-mouth positions. This is for the prevention of articular damage.
In the closed mouth position, the condyle is centered in the glenoid fossa. The disk is interposed between the condyle inferiorly and the glenoid fossa superiorly. The articular eminence is anterior to the disk (Figure 2). The normal disk is positioned such that the anterior band is in front of the condyle and the junction of the posterior band and bilaminar zone lie immediately above the condylar head near the 12 o’clock position[1,3,4,9,12-14]. However, some controversy exists over the range of normal position of the disk[1,3,4,14-18]. Drace et al[15] suggest that the junction of the posterior band and bilaminar zone should fall within 10 degree of vertical to be within 95 percentile of normal. There is significant variation in relationship of the posterior band and bilaminar zone in normal population, resulting in inappropriate classification of anterior disk displacement[16,18]. Rammelsberg et al[17] suggest that disk positions of up to +30° from the vertical be considered normal. Many other authors have proposed that the intermediate zone be the point of reference so that in a normal joint it is interposed between the condyle and the temporal bone in all joint positions[4,19,20]. Comparing to the different disk positions of 12, 11 and 10 o’clock, Orsini et al[19] found the intermediate zone criterion for disk displacement to be more stringent. Recently Provenzano Mde et al[20] have suggested similar conclusions (Figure 2).
IMAGING TECHNIQUES
A variety of modalities can be used to image the TMJ. This includes non-invasive imaging modalities such as conventional radiographs, ultrasound, Computed tomography (CT) and MRI to more invasive imaging such as arthrography. Each imaging modality has its uses.
Conventional radiographs have a limited role in evaluation of the TMJ. They can be used to evaluate only the bony elements of the TMJ. They do not give useful information when it comes to the non-bony elements such as cartilage or adjacent soft tissues. They also do not give useful information concerning joint effusions, which are commonly associated with pain and disc displacements. Another disadvantage concerning conventional radiographs is the problem of superimposition of adjacent structures. Many different views such as the submentovertex, transmaxillary, and the transcranial are used to reduce superimposition.
Ultrasound is a less expensive and easily performed imaging modality that can be used to evaluate the TMJ. This is simple way to look for the presence of a joint effusion[21]. Ultrasound is also used to evaluate cartilage as well as disk displacement with both open and closed mouth imaging[21]. It is used for image-guided injections for both diagnostic and therapeutic purposes[21]. Typically, a linear transducer of 8 MHz or higher is ideal. The patient should be lying supine with the transducer placed parallel to a line extending from the tragus of the ear to the lateral surface of the nose over the TMJ.
CT is useful to evaluate the bony elements of the TMJ as well as the adjacent soft tissues. CT is ideal for the evaluation of fractures, degenerative changes, erosions, infection, invasion by tumor, as well as congenital anomalies[21]. A typical imaging protocol is: 120 kV, 100 mA, 1 mm collimation, 1 mm/rotation (pitch), and imaged with a closed mouth. CT also allows 3D reconstructions, which can be used for evaluating congenital anomalies and fractures[21]. CT is predominantly done when there is suspicion of bony involvement from the MRI and if primary bony pathologies are suspected clinically. Relative advantages of CT over MRI include, exquisite bone details and 3D assessment of congenital, traumatic and postsurgical conditions.
Clinical evaluation of the TMJ can be nonspecific due to overlap of symptoms between internal derangement and myofacial pain dysfunction[1]. MRI should be part of the standard evaluation when an internal structural joint abnormality is suspected because MRI provides high resolution and great tissue contrast. This allows for a detailed evaluation of the anatomy was well as biomechanics of the joint through open and closed mouth imaging[1].
For optimal imaging of the TMJ, small bilateral surface coils with small field of view are used to achieve higher signal to noise ratio and simultaneous bilateral acquisition. Closed mouth coronal and axial T1 sequences are needed to evaluate the overall anatomy and bone marrow as well as the adjacent soft tissues to exclude other adjacent pathology. In our institution, axial T1 is obtained as a localizer[14]. Bilateral closed mouth and open mouth T2, proton density (PD) and dynamic sequences are obtained in a oblique sagittal plane. In our institution, dynamic images are obtained as rapid acquisition of static images using a single shot fast spin echo (SSFSE) proton density sequence during progressive opening and closing of the mouth. These images are displayed sequentially as a cine loop. Mouth opening devices such as Burnett opening devices may be used for incremental opening of the mouth controlled by the patient. It can be argued that passive mouth opening with a Burnet device might not reproduce the physiologic conditions occurring during mouth opening given the possible role of the lateral pterygoid muscle in disc stabilization during mouth opening. Oblique imaging entails 30° medial from the true sagittal plane[1]. Please see the table for specific MRI protocol[1]. A total of 8 sequences will need to be performed (Table 1).
Table 1.
Temporomandibular joint magnetic resonance imaging protocol
| Plane | Sequence | Slice thickness | TR | TE | Mouth open/closed |
| Axial | T1 | 2 mm, 0 skip | 500 | Minimal | Closed |
| Coronal | T1 | 3 mm, 0.5 skip | 500 | Minimal | Closed |
| Bilateral Sag Oblq | T2 and PD | 3 mm | 3500 | Min and 85 | Closed and open |
| Bilateral Sag Oblq | T2 | 3 mm | 1180-2000 | 64 | Dynamic cine |
PD: Proton density; TE: Echo time; TR: Repetition time.
Arthrography is an invasive imaging technique to evaluate the TMJ. This imaging modality requires injection of radiopaque contrast into the TMJ under fluoroscopic guidance. Once the contrast is injected, the joint can be evaluated for adhesions, disk dysfunction, as well as disk perforation based on how contrast flows in the joint. This modality is rarely used today because MRI can be used to evaluate the TMJ without being invasive, exposing the patient to a possibility of allergic reaction from the contrast, possibility of infection, or using radiation.
IMAGING APPEARANCE OF NORMAL TMJ
MRI
On MRI, marrow fat in the condyle has a high T1 signal intensity. The cortical bone and the disk have low signal intensity on both T1 and T2 weighted images because of low proton density and short T2[12]. Sometimes high T2 and PD signal intensity can be seen in the central portion of the disk similar to a centrally hydrated vertebral disk[1,4]. The disk is otherwise homogeneous, hypointense and biconcave in shape. The center of the posterior band may be slightly hyperintense due to presence of loose areolar tissue (Figure 2).
The disk’s posterior attachment has higher signal intensity than muscle on proton density and T1 weighted images secondary to fatty tissue. The bilaminar zone is visible as intermediate signal intensity structures.
In closed mouth position, the junction of the posterior band and posterior attachment normally lies above the condylar head near the 12 o’clock position. The posterior band and retrodiskal tissue are best depicted in the open mouth position. In open mouth position, the intermediate zone lies between the condyle and the articular eminence and the posterior band is against the posterior surface of the condyle[1,9] (Figure 2).
The superior belly of lateral pterygoid attaches to the anterior band of the disk. The inferior belly of the lateral pterygoid attaches to the anterior surface of the condylar neck with a thin linear hypointense fibrous band. This band is seen just inferior to the position of the disk, and can sometimes be mistaken for the disk, particularly when the disk is medially or laterally displaced[22].
In the coronal plane, the disk is crescent shaped and its medial and lateral borders are attached to the respective aspects of the condylar head and joint capsule. The lateral and medial capsules do not demonstrate any outward bulges beyond the borders in normal condition[1,22].
PATHOLOGIES RELATED TO ANATOMIC VARIATIONS
Anatomic variations in the TMJ can be symptomatic and/or have implications during arthroscopy and surgery. There can also be several variations in the appearance of the mandibular condyles including intra-individual variations between the two sides. The disease processes can be developmental, due to remodeling related to malocclusion, trauma or other secondary developmental abnormalities[3].
Bifid condyle
A bi-lobed or duplicated mandibular head is an infrequently encountered incidental imaging finding. While the etiology is unknown, theories include reminiscence of congenital fibrous septum and peripartum or early childhood trauma. The duplicated heads may lie in either an antero-posterior or transverse orientation. Dennison et al[23] have suggested that the term “bifid condyle” should be reserved for describing multiple condyles in the sagittal plane only. No treatment is required for asymptomatic patients. However surgery may be performed if there is displacement of the disc or ankylosis of the joint space (Figure 3).
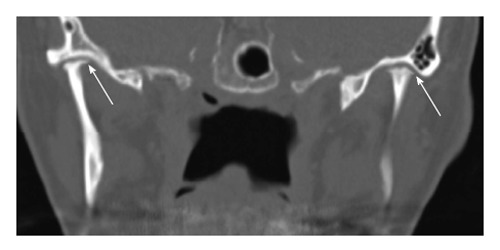
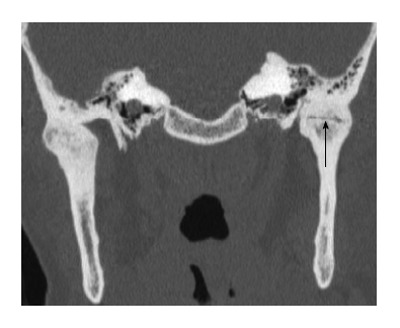
Figure 3.
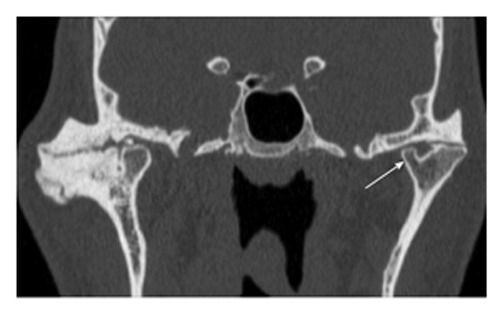
Bifid condyle. Coronal reformatted computed tomography image through the temporomandibular joint (TMJ) demonstrates bifid left mandibular condyle. It can be noted that one of the condyles (arrow) is smaller than the other. Advanced degenerative changes are noted in bilateral TMJ.
Foramen of Huschke
In some individuals there may be persistence of a developmental defect in the tympanic plate. The tympanic plate is present as an incomplete U-shaped cartilaginous ring at birth. Over time the ossification proceeds laterally and posteriorly leaving a defect in the floor of the external meatus, called the foramen tympanicum (foramen of Huschke). With growth of the mastoid process, this defect changes in position from inferior to anterior and usually closes by the 5th year of life. Rarely, a 3-4 mm defect persists and is found to be located at the antero-inferior aspect of the external auditory canal and posteromedial to the TMJ. These patients can present with a defect or polyp on the anterior wall of the external auditory canal (EAC) or with salivary otorrhea during mastication. TMJ tissue may also herniate into the EAC during mastication[24,25]. During arthroscopy, there can be inadvertent passage into the EAC resulting in otologic complications. This foramen also can act as a path of communication between the EAC and TMJ or infratemporal fossa allowing the spread of infection, inflammation or tumor[24,25] (Figure 4).
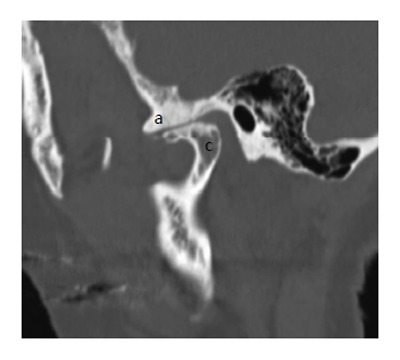
Figure 4.
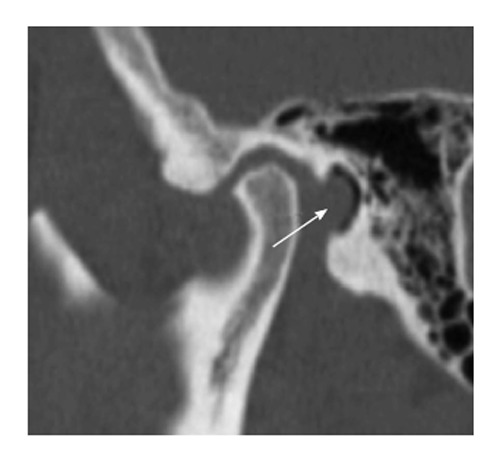
Foramen of Huschke. Sagittal reformatted computed tomography image through the temporomandibular joint demonstrates a focal defect (arrow) in the tympanic plate.
Condylar hypoplasia
Aplasia and hypoplasia of the mandibular condyle is secondary to non-development or underdevelopment of the condyle and can be congenital or acquired. Congenital aplasia or hypoplasia of the mandibular condyles is a rare anomaly and usually occurs as a part of more widespread 1st and 2nd branchial arch anomalies (e.g., Treacher-Collins syndrome). Acquired condylar hypoplasia may be secondary to local factors (trauma, infection, radiation) or systemic factors (toxic agents, rheumatoid arthritis, mucopolysaccharoidosis)[26]. Traumatic vaginal delivery has been implicated as a cause of hypoplasia[27]. Hypoplasia may involve one or both of the condyles. Unilateral disease produces mandibular rotation or tilt and associated facial asymmetry. The diagnosis of bilateral condylar hypoplasia may be delayed secondary to facial symmetry. Hypoplastic condyles are frequently complicated with ankylosis[28].
Idiopathic condylar resorption
Idiopathic condylar resorption (also known as condylysis or “cheerleader syndrome”) is primarily a disease of TMJ affecting teenage girls. There is rapidly progressive condylar erosion resulting in widening of the joint space with the chin becoming less prominent from retrognathia[29]. Many causes have been hypothesized including estrogen influence on osteogenesis, avascular necrosis, and TMJ internal derangement. Orthognathic surgery has been implicated as a cause of the disease but also is one of the corrective approaches for idiopathic condylar resorption (Figure 5).
Figure 5.
Idiopathic condylar resorption. Coronal reformatted computed tomography image through the temporomandibular joint of a young patient demonstrates bilateral severe condylar resorption (arrows) without any evidence of degenerative changes within the joint.
Condylar hyperplasia
Condylar hyperplasia is a rare disorder characterized by increased volume of the mandibular condyle, and is frequently associated with increased volume of the ramus and mandibular body[30]. Condylar hyperplasia is usually a unilateral process. This disease presents in the second and third decades of life during brisk periods of osteogenesis suggesting a hormonal influence upon the growth disturbance. Trauma has also been implicated in asymmetric condylar hyperplasia due to hypervascularity during healing producing inducing excessive osteogenesis. The hyperplasia produces facial asymmetry with the chin rotating away from the affected side[30]. Resection of the hyperplastic condyle causes the abnormal growth to cease and restores facial symmetry (Figure 6).
Figure 6.

Condylar hyperplasia. Panoramic reformation of the source computed tomography data including both the temporomandibular joints of a young patient demonstrates hyperplasia of the left condyle (arrowhead) in comparison to the right side. Associated hypertrophy of the ramus and the neck (arrow) of the left hemi-mandible is also noted.
Extensive pneumatization
Extensive pneumatization of the mastoid bone can involve the glenoid fossa and articular eminence. Knowledge of extensive pneumatization is necessary prior to surgery to prevent perforations. Complications can occur during TMJ surgery due to forceful flap retraction, dissection or with placement of screws in cases where fossa-eminence prostheses are required[31,32]. Pneumatization can also provide a path of minimal resistance and facilitate the spread of pathological tumors, inflammation, infection or fracture into the joint. For these reasons, a CT must be performed prior to TMJ surgery when extensive pneumatization is detected in the panoramic radiographs[31,32] (Figure 7).
Figure 7.

Extensive pneumatization. Coronal reformatted computed tomography image through the right temporomandibular joint demonstrates almost complete pneumatization of the glenoid fossa except the central part.
INTERNAL DERANGEMENT OF TMJ
Internal derangement (ID) is defined as a mechanical fault of the joint that interferes with smooth joint function. This is attributed to abnormal interaction of the articular disc, condyle and articular eminence. Associated clinical features include articular pain and articular noises[33]. Disc displacement is the most common cause of ID, though not all displaced discs are associated with derangement and not all derangements are caused by disc displacement[34]. Additionally, it is not clear whether the displaced disk is related to onset, progression or cessation of the pain. Loose bodies and adhesions in the joint can also result in derangement. Up to 34% of asymptomatic volunteers can have anterior disc displacement and 23% of patients with derangement can have normal disc position[18]. In most large MRI series approximately 80% of patients referred for diagnostic imaging of the TMJ demonstrate some form of disk displacement[35-37]. MRI is the imaging modality of choice for the diagnosis of internal derangement with an accuracy of 95% in assessing the disc position and form and 93% accuracy in assessing the osseous changes[38].
Disc displacement
The disc displacement is categorized based on the relation of the displaced disc with mandibular condyle. The displacement can be anterior, anterolateral, anteromedial, lateral, medial and posterior[39]. The most common pattern of disc displacement are either anterior and anterolateral accounting for more than 80% of the causes[37]. The disc displacement can be subclassified as anterior displacement with reduction (ADR) or anterior displacement with no reduction (ADNR) based on restoration of a normal relationship between the condyle and the disc on mouth opening (Figures 8 and 9). The disc displacement can be either complete or partial[35]. If the entire mediolateral dimension of the disc is displaced, it is referred to as complete displacement. On the other hand if only the medial or lateral portion of the disc is displaced, it is referred to as partial displacement. Partial disc displacement is commonly seen with ADR. Frequently the lateral part of the disc is displaced anteriorly while the medial part of the disc remains in normal position (rotational disk displacement)[40].
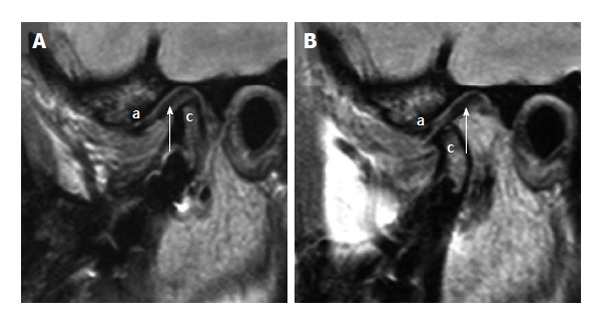
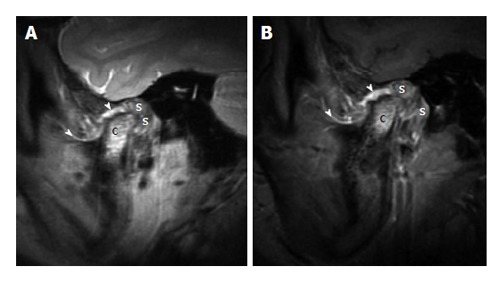
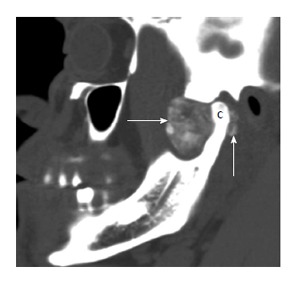
Figure 8.
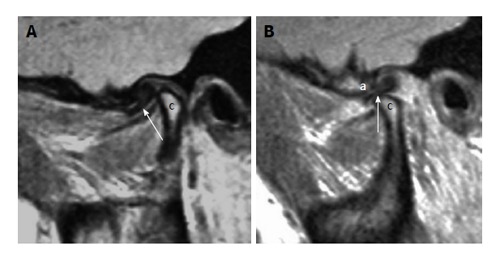
Anterior displacement with reduction. A: Sagittal proton density weighted magnetic resonance imaging (MRI) in the closed mouth position demonstrates anterior displacement of the disk (arrow) in front of the mandibular condyle (the letter, c); B: Sagittal proton density weighted MRI in the open mouth position demonstrates reduction of the disk (arrow) between the articular eminence (the letter, a) and the mandibular condyle (the letter, c).
Figure 9.
Anterior displacement with no reduction. A: Sagittal proton density weighted magnetic resonance imaging (MRI) in the closed mouth position demonstrates anterior displacement of the disk (arrow) related to the articular eminence (the letter, a) and anterior to the mandibular condyle (the letter c); B: Sagittal proton density weighted MRI in the open mouth position demonstrates no reduction of the disk (arrow) between the articular eminence (the letter, a) and the mandibular condyle (the letter, c).
In ADR, the anteriorly displaced disc returns to the normal position on mouth opening producing a “reciprocal click” (Figure 9). In ADNR, there is limited mouth opening and deviation of the jaw to the affected side (closed lock). Over time, stretching or perforation of the retrodiscal tissue causes deformation of the disk leading to an improvement in jaw excursion and reduced lateral deviation during mouth opening (Figure 10A). The posterior band of the disc remains anterior to the condyle even with mouth opening[41]. There is increased association of degenerative changes in the TMJ with the ADNR. Although TMJ disorder with ADR and normal condylar cortical bone may be stable for decades, it will eventually progress to ADNR. In a study with 55 patients, de Leeuw et al[42] have demonstrated 75% of the patients with long history (approximately 30 years) of TMJ internal derangement have ADNR.
Figure 10.
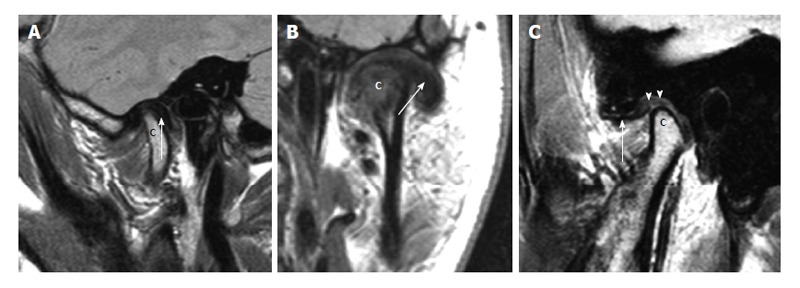
Other types of disk displacement. A: Posterior disk displacement. Sagittal proton density weighted magnetic resonance imaging (MRI) in the closed mouth position demonstrates posterior displacement of the disk (arrow) in relation to the mandibular condyle (the letter, c); B: Lateral disk displacement. Coronal proton density weighted demonstrates lateral displacement of the disk (arrow) in relation to the mandibular condyle (the letter, c); C: Pseudodisk. Sagittal proton density weighted MRI in the closed mouth position demonstrates anterior displacement of the disk (arrow) in front of the mandibular condyle (the letter, c). The thickening of the posterior attachments (arrowheads) superior to the mandibular condyle is seen as “pseudodisk”.
The exact mechanism for a disc displacement is unknown although trauma with injury to the posterior disc attachment is considered to be the most likely cause. Unenhanced MRI is the imaging modality of choice for evaluation of ID. During the early stage of ID the disc retains its normal shape, but over time it becomes deformed by thickening of the posterior band and thinning of the anterior band. This produces in a biconvex, tear-drop shaped or a rounded disc. The disc maintains a normal biconcave shape as long as it remains on top of the condyle during mouth opening[42]. Hence, presence of an irregular and rounded disc almost always indicates disc disease[43]. Other MRI findings that suggest disc disease include disc flattening, decrease in the normal intermediate to high signal intensity of the disc[44] and presence of tear or perforation in the chronic stage.
Posterior disc displacement is a rare entity and accounts for only 0.01% to 0.001% of all disc displacements[45]. The major clinical sign is a sudden onset of locked jaw in open position. MRI is helpful in the diagnosis by demonstrating displacement of the posterior band beyond 1° clock position[9] (Figure 10A). Review of patient’s clinical information is important before image interpretation as previous posterior disk plication can be mistaken for an acquired posterior disk displacement.
Anterolateral and antero-medial disk displacements are grouped under rotational displacements while the pure lateral and medial displacements are grouped under sideways displacement[46]. Isolated lateral displacement is rare (Figure 10B). Again these rotational and sideways displacements can be complete or partial and with or without disc reduction. Anterolateral displacement is the most common pattern[37].
Pseudodisk
A pseudo-disk is present in some patients with an anteriorly displaced disk. This has been postulated as an adaptive reaction to anterior disk displacement within the posterior disk attachment followed by subsequent connective tissue hyalinization that[47] appears as a band-like structure of low signal intensity replacing the normally bright signal of the posterior disk attachment[8,9,22] (Figure 10C).
Stuck disc
The “stuck disc” is a pathologic condition characterized by an immobile disc in relation to the glenoid fossa and the articular eminence. This is present in both open and closed mouth positions[9] and is likely related to the adhesions. It can occur with or without disc displacement and can be associated with pain and joint dysfunction due to limitation of condylar translation[48,49]. This diagnosis can be missed unless the TMJ is imaged in both open and closed mouth positions (Figure 11). Sagittal oblique cine imaging is particularly useful in evaluation of stuck disk.
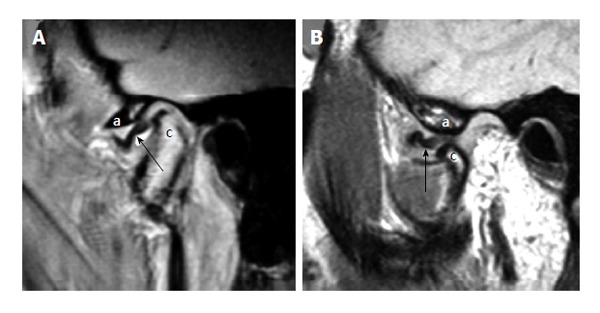
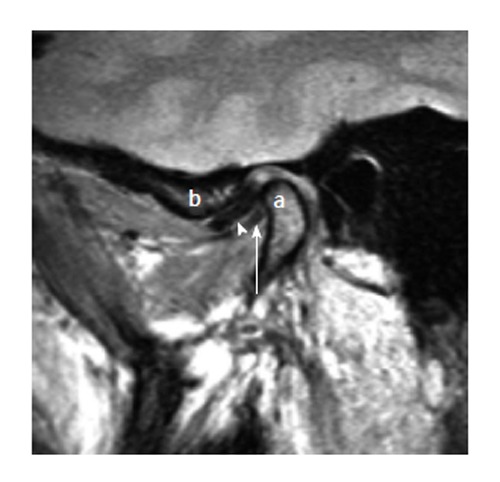
Figure 11.
Stuck disk. A: Sagittal proton density weighted magnetic resonance imaging (MRI) in the closed mouth position demonstrates apparently normal position of the disk (arrow) in relation to the mandibular condyle (the letter, c). The letter “a” demonstrates the articular eminence; B: Sagittal proton density weighted MRI in the open mouth position demonstrates no anterior movement of the disk (arrow) with the mandibular condyle (the letter, c), i.e., “stuck” to the glenoid fosssa. The articular eminence is denoted with letter “a”.
Perforated disc
Disc perforation is reported in 5% to 15% of deranged joints disc displacements[50]. It is more common in patients with ADNR than in ADR[51,52] and is usually seen in patients with advanced arthrosis. The prevalence of a perforated disc is higher in women than in men and prevalent in individuals over 80 years of age[53]. MRI findings of disc perforation include disc deformity (100%), disc displacement (81%), condylar bony changes (68%), joint effusion (23%) and non-visualization of temporal posterior attachment (TPA) of the disc (65%-68%)[54]. Conventional and MR arthrogram can be helpful in the diagnosis of a disc perforation by demonstrating opacification of both the joint compartments from a single lower compartment injection. If the disk perforation is suspected a fat suppressed T2 weighted MRI can be obtained in sagittal and coronal plane[55]. Absence of stretching/straightening of the posterior temporal disk attachment on mouth opening also suggests disk perforation.
Joint effusion
Joint effusion represents an abnormally large accumulation of intra-articular fluid and is commonly seen in symptomatic patients. A small amount of joint fluid can be seen in asymptomatic patients[56]. An effusion is more prevalent in painful than in non-painful joints[16]. Although not all patients with joint pain have effusion, patients with large effusions commonly experience pain and disc displacement[57].
T2 weighted MR sequence is the best sequence for the assessment of joint effusion. An early joint effusion is commonly seen surrounding the anterior band but larger effusions can occupy both superior and inferior joint space. A large effusion may have diagnostic value as it outlines the disc and sometimes even the disc perforation as well as retrodiscal tissue producing “arthrographic effect”[57]. Gadolinium enhanced T1 weighted imaging can be helpful in distinguishing a plain joint effusion from synovial proliferation. In patients with inflammatory arthropathies with associated synovial proliferation, the proliferating synovium enhances while the effusion does not[58].
Thickening of lateral pterygoid muscle attachment (double disk sign)
The exact role of lateral pterygoid muscle (LPM) in the TMJ function is still controversial although its suggested role is in generation of side-to-side and protrusive jaw forces[9]. There are electromyographic studies showing hyperactivity in the inferior attachment of the LPM in patients with TMJ internal derangement[59]. Several morphologic changes to the superior and inferior bellies of the LPM on MRI have been described. These include hypertrophy, atrophy and contractures in patients with ADNR of the TMJ with these morphologic changes having a significant association with the clinical symptoms of pain or restricted jaw opening[60]. It is suggested that there is significant association between the anterior disc displacement and attachment of the superior LPM to the disc alone and not to the condyle[61]. The interpreting radiologist should be aware of a potential pitfall of mistaking the thickened inferior LPM to an anteriorly displaced disc (“double disc sign”)[9] (Figure 12).
Figure 12.
Double disk sign (thickening of the lateral pterygoid muscle). Sagittal closed mouth proton density image demonstrates anterior displacement of the disk (arrow head). The thickened lateral pterygoid muscle near the mandibular condylar (the letter, a) attachment appear as linear hypointense structure (white arrow) inferior to the disk in the same orientation giving the appearance of “double disk”. The articular eminence is denoted with letter “b”.
Osteochondritis dissecans and avascular necrosis
Osteochondritis dissecans (OCD) and avascular necrosis (AVN) of the mandibular condyle are similar pathologic entities likely represent a spectrum of the same pathophysiology[62]. Common clinical features of OCD/AVN of the mandibular condyle include pain and joint disability[63]. Pain is commonly over the joint and along the third division of the trigeminal nerve. Other symptoms include ipsilateral headache, earache and spasm of masticator muscles. These can occur with or without limitation of joint movements[63].
MRI is the modality of choice for assessment of OCD/AVN of the mandibular condyle[63]. There is decreased marrow signal on T1 weighted sequences in cases of AVN. T2 weighted sequences demonstrate variable signal characteristics with early AVN, healing and OCD. Early AVN consistently exhibits high signal on T2WI and acute OCD typically demonstrated a hypointense central fragment surrounded by a zone of higher signal on both T1W and T2W sequences[63]. Although MRI is 78% sensitive and 84% specific for the diagnosis of AVN, the positive predictive value is only 54% because condylar sclerosis secondary to advanced TMJ degenerative changes have similar MRI appearances[64]. Radiologic changes of OCD and AVN of the mandibular condyle are frequently associated with joint effusion and internal derangement of the disc[65] (Figure 13).
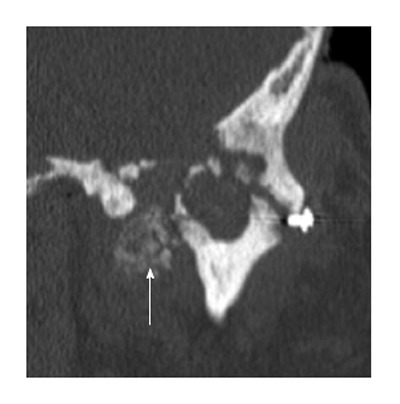
Figure 13.
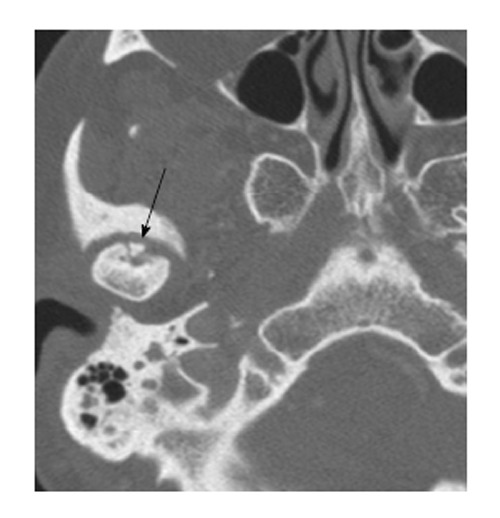
Osteochondritis dessicans. Axial computed tomography scan through the level of the temporomandibular joint demonstrates a tiny bone fragment (arrow) at the anterior aspect of the disk. It can be noted that there are linear lucency surrounding the bone fragment.
Loose bodies
Loose bodies in a synovial joint can be due to primary or secondary synovial chondromatosis. The primary type is associated with spontaneous cartilaginous metaplasia in the synovium, while the secondary type is due to incorporation of osteocartilaginous loose bodies in the synovium in the setting of degenerative joint disease[66]. Common clinical symptoms associated with loose bodies include pain, periauricular swelling, decreased range of jaw motion, crepitation and unilateral deviation of the jaw during mouth opening[67].
Panoramic radiographs of the TMJ may or may not demonstrate loose bodies[68]. High resolution CT[69,70] or MRI[70] can demonstrate small loose bodies within the TM joint space (Figure 14).
Figure 14.
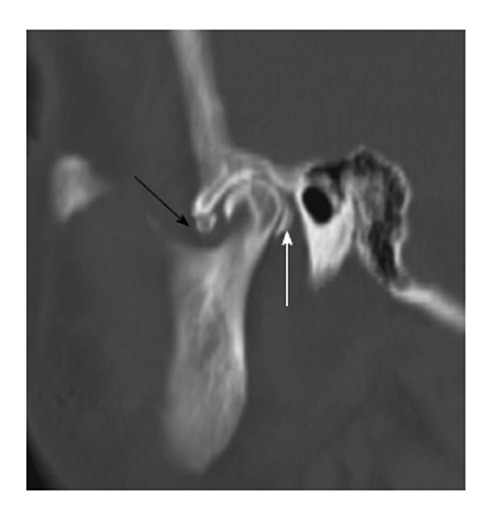
Loose bodies. Sagittal reformation of the axial dataset demonstrates multiple “loose bodies” in the joint cavities, anteroinferior to the articular eminence (black arrow) and immediately posterior to the mandibular condyle (white arrow).
Hypermobility
Patients with a hypermobile TMJ can present with an inability to close the jaw (open lock) after wide opening of the jaw. This occurs as a result of translation of the condyle beyond the margins of the anterior attachment of the TMJ capsule. Entrapment of the condyle along the anterior slope of the articular eminence results due to various biomechanical constraints, particularly masticator muscle activity[71].
In acute cases, there is little need for imaging studies as the open lock is clinically evident with a relevant clinical history of wide jaw opening or trauma. In chronic cases MRI can give information about the height and steepness of the articular eminences as well as the shape and position of the disc[72].
Ankylosis
Ankylosis of the TMJ can be due to fibrous adhesions or a bony fusion resulting in the restriction of jaw motion. It can occur as a sequel of previous infection, trauma surgery[73] and in patients with juvenile idiopathic arthritis or bifid mandibular condyles. MR arthrography is useful for the evaluation of fibrous adhesions and three-dimensional CT scan is necessary for surgical planning when bony fusion is suspected (Figure 15).
Figure 15.
Ankylosis. Coronal reformation of the axial dataset demonstrates complete ankylosis of the right temporomandibular joint (TMJ) and near complete ankylosis of the left TMJ with subtle residual joint space at the center (black arrow).
TMJ ARTHRITIS
Similar to other synovial joints in body, the TMJ is frequently involved in different inflammatory arthritides. Degenerative arthritis and arthritis secondary to crystalline deposition disease are also common in TMJ. Arthritis secondary to infection or trauma can occur at the TMJ. Arthritis of TMJ is discussed based on the pathophysiologic mechanism.
Inflammatory arthritis
Juvenile idiopathic arthritis: Juvenile idiopathic arthritis (JIA) is the most common rheumatic disease in childhood affecting girls more frequently than boys. The disease predominantly affects synovial joints. There are two peaks of onset, first being between the ages of 1 and 3 years and the second peak between 8 and 12 years[74]. The TMJ is involved in 17% to 87% of patients with JIA[74]. JIA can be systemic, polyarticular and pauciarticular. The TMJ is more commonly involved in patients with polyarticular joint involvement[75]. The typical presentation of TMJ involvement includes pain, joint tenderness, crepitation, stiffness and decreased range of motion. Bony ankylosis can develop in some patients as a late disease manifestation.
Orthopantomogram, CT, MRI and ultrasound have been used to evaluate TMJ JIA. Orthopantomogram and CT predominantly identify the bony erosions secondary to TMJ involvement. Both these techniques involve radiation exposure to young patients. MRI and ultrasound have gained popularity in evaluation of the TMJ in patients with JIA because these techniques have better soft tissue resolution allowing earlier diagnosis of TMJ involvement without any ionizing radiation. Acute TMJ arthritis typically demonstrates joint effusion and synovial thickening on T2 weighted imaging without any bony changes[76]. Enhancement of the joint or periarticular tissue is not a specific sign of acute TMJ arthritis because abnormal joint enhancement can be present even in healthy patients[76]. Condylar resorption can be better evaluated on non-fat suppressed T1 weighted sequence and suggests a more chronic TMJ arthritis[76] (Figure 16).
Figure 16.
Juvenile idiopathic arthritis. A: Sagittal proton density weighted magnetic resonance imaging (MRI) in the closed mouth position demonstrates increased signal at the mandibular condyle (the letter, c), extensive thickening of the synovium (the letter, s) in the retrodiscal regions. It can be noted that the thickening and increased signal of the synovium at other places (arrowheads); B: Sagittal fat suppressed post contrast T1 weighted MRI in the closed mouth position demonstrates enhancement of signal at the mandibular condyle (the letter, c), enhancement and extensive thickening of the synovium (the letter, s) in the retrodiscal regions. There is thickening and enhancement of the synovium at other places (arrowheads).
Rheumatoid arthritis: Rheumatoid arthritis (RA) is a chronic inflammatory disorder that predominantly affects the periarticular tissue such as synovial membrane, joint capsules, tendon, tendon sheaths and ligaments. Internal joint components are secondarily involved. The prevalence of RA in the general population is approximately 2%-2.5% with female predominance. The peak onset of disease is 40-60 years and approximately 50%-75% of patients with RA have TMJ involvement[77].
RA is a slowly progressive disease of insidious onset with progressive destruction of the articular/periarticular soft tissue and the adjacent bones resulting in joint deformity. The TMJ is involved at a later stage of disease. TMJ involvement causes deep, dull aching pain in the preauricular area, especially during chewing. Limited range of motion and morning stiffness can be present[78]. The mandibular condyle gradually resorbs as the disease progresses.
Radiographic features of RA include loss of joint space, condylar destruction, flattening with anterior positioning of the condyle. There may be flattening of the articular eminence and erosion of the glenoid fossa. Synovial proliferation is an early process in RA and can distinguish it from other types of arthritis[79]. Synovial proliferation is readily seen on MRI and can be seen in all patients[79]. A joint effusion is also comparatively more common in RA.
Degenerative (osteo)arthritis
Osteoarthritis (OA) is a chronic degenerative disease that characteristically affects the articular cartilage of synovial joints and is associated with simultaneous remodeling of the underlying subchondral bone with secondary involvement of the synovium. Osteoarthritis is the most common joint pathology affecting the TMJ[80]. There is a clear disparity between radiographic evidence of OA and symptoms. Population based studies demonstrate that minimal condylar flattening is present in up to 35% of asymptomatic patients while approximately 11% of patients have TMJ OA-related symptoms[80].
The most common symptom of TMJ OA is pain during chewing. The pain usually starts in the periarticular soft tissue and the masticator muscles that are in protective reflex spasm. Fatigue of masticator muscles, trismus, decreased range of motion, difficulty opening the mouth and joint crepitations are other common symptoms.
Radiologic hallmarks of TMJ OA are articular surface cortical bone irregularity, erosion and osteophyte formation[81]. Erosion is radiologically defined as focal area of decreased density at the cortical margin of the articular surface of the mandibular condyle and the subchondral region. Osteophyte formation typically occurs at a later stage in the disease and can stabilize and broaden the surface area of the joint in an attempt to better withstand axial loading forces. Different imaging modalities have been used with varying degree of success. There is still no general consensus as to which imaging modality should be the gold standard[81] (Figure 17).
Figure 17.
Degenerative changes. Sagittal reformation of the axial dataset demonstrates deformity of the mandibular condyle (the letter, c), extensive sclerosis of the articular eminence (the letter, a) and severe loss of joint space.
Metabolic arthritis/crystalline arthropathies
Calcium pyrophosphate dehydrate deposition disease: Calcium pyrophosphate dehydrate deposition disease (CPPD) is a metabolic arthropathy caused by the deposition of calcium pyrophosphate dehydrate crystals in and around joints, especially within the articular cartilage and fibrocartilage[82].
The spectrum of TMJ involvement ranges from asymptomatic disk calcification to a marked destruction of the joint with erosive changes in the mandibular condyle and the adjacent skull base. Common symptoms include pain and preauricular swelling with occasional hearing loss. Chewing can exacerbate the pain. Other less common symptoms include TMJ clicking, tinnitus, and malocclusion.
The radiographic appearance of CPPD is variable. Computed tomography demonstrates calcium deposition in the disk or periarticular tissue. On MRI, CPP deposits typically appear as hypointense material both on T1 and T2 weighted sequences. CT and MRI show erosions near both the condyle and fossa with adjacent CPPD deposits[82]. The erosions may extend into the skull base and into the middle cranial fossa. Involvement of other joints with chondrocalcinosis is a clue to the diagnosis. The differential diagnosis includes synovial chondromatosis, synovial osteochondroma, and osteosarcoma (Figure 18).
Figure 18.
Calcium pyrophosphate dehydrate deposition disease. Coronal reformation of the axial dataset demonstrates destruction of the left temporomandibular joint with erosion and deformity of both the mandibular condyle and the glenoid fossa. There is extensive extensive calcium pyrophosphate dehydrate deposition disease medial to the joint space (arrow).
Infectious arthritis
TMJ infection is usually secondary to direct extension of infection from the adjacent tissue into the joint. Systemic infections such as tuberculosis and syphilis can rarely involve the TMJ. TMJ infection is more common in the setting of immunosuppression and presence of other systematic diseases such as diabetes mellitus, rheumatoid arthritis and intravenous drug use, etc.
TUMORS AND TUMOR-LIKE CONDITIONS OF THE TMJ
Tumors and tumor-like conditions can affect the TMJ. These conditions may have similar presentations such as pain, swelling, and limitation of motion.
Synovial chondromatosis
Synovial chondromatosis (SC) is a benign condition with chondrometaplasia of the synovial membrane and formation of cartilaginous nodules. These nodules can become detached and form loose bodies which later calcify. Synovial chondromatosis typically involves large joints, such as the knee, hip, and elbow. It is uncommon for the temporomandibular joint to be affected by SC. SC typically involves the superior compartment of TMJ while involvement of the inferior compartment is rare and secondary to perforation of the articular disc. Uncommon findings include erosion of the mandibular condylar head, temporal skull base, and intracranial extension.
Patients typically present with preauricular pain, swelling, inflammation, limitation of motion, and articular noises. Some patients also report neurologic dysfunction, such as headache and hearing loss.
The diagnosis of TMJ synovial chondromatosis is difficult since it is a rare disease and can have similar findings to more common diseases, such as chondrocalcinosis, osteoarthritis, and chondrosarcoma. The radiologic findings of SC include calcified loose bodies, soft tissue swelling, widening of the joint space, irregularities of the joint surface, and sclerosis of the glenoid fossa and/or mandibular condyle. CT typically shows calcified nodules surrounding the mandibular condyle with degenerative changes of the condyle[83]. MRI typically shows mixed solid and fluid signal related to the metaplasia of the synovial tissue and the fluid component of the accumulated synovial secretions. The calcified nodules are T1/T2 hypointense with a surrounding T2 hyperintense effusion and proliferative synovium, which enhances after contrast administration. MRI is preferred in evaluation of SC over CT because of the ability to detect non-calcified loose bodies, lack of radiation, and visualization of the articular disc[84] (Figure 19).
Figure 19.
Synovial chondromatosis. Sagittal reformation of the axial dataset demonstrates extensive cloud-like calcification (arrows) filling and expanding the joint space anterior to the mandibular condyle (the letter, c). Calcification is also present posterior to the mandibular condyle.
Treatment is surgical removal of the loose bodies and excision of the metaplastic synovium. In end stage SC without synovial metaplastic activity, the treatment is often non-surgical with therapy aimed towards symptom relief.
Pigmented villonodular synovitis
Pigmented villonodular synovitis (PVNS) is a benign, non-neoplastic proliferative disorder of the synovial membranes of joints, bursae, and tendon sheaths. The disease is typically monoarticular and can involve any joint but is most often seen in the knee. Primary PVNS of the TMJ is rare. There are two forms of PVNS: nodular and diffuse. The most common nodular patterns of PVNS include giant cell tumor, xanthoma, xanthogranuloma, and myeloplaxoma, which affect a focal part of the synovium[85]. Diffuse PVNS affects nearly the entire synovium.
The exact etiology of PVNS is unclear. It was originally postulated to be an inflammatory response to an unknown stimulus. Other theories attribute it to repetitive intra-articular hemorrhage from trauma, altered lipid metabolism, or a benign neoplastic proliferation.
PVNS commonly presents as a slowly growing and non-tender swelling of the affected joint. Patients with involvement of the TMJ, can present with a preauricular mass with swelling, pain, tenderness, clicking, otalgia, and hearing loss.
The most sensitive method for the detection of PVNS is by MRI demonstrating T1/T2 hypointensity and blooming on the GRE sequences from paramagnetic hemosiderin deposition[86]. There may be moderate to intense inhomogeneous enhancement of the synovium. CT findings are usually nonspecific with bone erosion, subchondral cysts, and a soft tissue mass[87]. A joint effusion may be dense from the hemosiderin. The differential diagnosis of PVNS on MRI includes synovial chondromatosis, rheumatoid arthritis, synovial sarcoma, hemophilia, and synovial hemangioma.
Primary and secondary neoplasms, and other lesions
Osteochondroma is the second most common neoplastic lesion affecting the TMJ. Osteochondroma, osteoma, and condylar hyperplasia are often difficult to differentiate both clinically and on imaging. MR and CT may delineate the exact extent of the tumor and its relationship to anatomic structures within the TMJ.
Synovial cysts, ganglion cysts and simple bone cysts may also occur. Many benign primary bone neoplasms, such as chondroblastoma, osteoma, osteoid osteoma, osteoblastoma, ossifying fibroma and aneurysmal bone cyst can also involve the TMJ. Malignant primary bone neoplasms are extremely rare in TMJ but include chondrosarcoma and osteogenic sarcoma. There also can be extension of tumors from adjacent structures into the TMJ. Tumors from the external ear and parotid gland can extend into the TMJ. Less than 1% of all tumors metastasize into the maxillofacial region. Adenocarcinoma is the most common metastatic tumor of the jaw, making up about 70% of cases. Reported metastasis to TMJ includes breast, renal, lung, colon, prostate, thyroid, and testicular primary.
CONCLUSION
Imaging of TMJ should be performed on a case by case basis depending upon clinical signs and symptoms. MRI is the diagnostic study of choice for evaluation of disk position and internal derangement of the joint. CT scan for evaluation of TMJ is indicated if bony involvement is suspected and should be judiciously considered because of radiation risk. Understanding of the TMJ anatomy, biomechanics, and the imaging manifestations of diseases is important to accurately recognize and manage these various pathologies.
Footnotes
P- Reviewer: Franco AL, Rattan V, Ramirez Aristeguieta LM S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
References
- 1.Aiken A, Bouloux G, Hudgins P. MR imaging of the temporomandibular joint. Magn Reson Imaging Clin N Am. 2012;20:397–412. doi: 10.1016/j.mric.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 2.Guralnick W, Kaban LB, Merrill RG. Temporomandibular-joint afflictions. N Engl J Med. 1978;299:123–129. doi: 10.1056/NEJM197807202990304. [DOI] [PubMed] [Google Scholar]
- 3.Alomar X, Medrano J, Cabratosa J, Clavero JA, Lorente M, Serra I, Monill JM, Salvador A. Anatomy of the temporomandibular joint. Semin Ultrasound CT MR. 2007;28:170–183. doi: 10.1053/j.sult.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Sommer OJ, Aigner F, Rudisch A, Gruber H, Fritsch H, Millesi W, Stiskal M. Cross-sectional and functional imaging of the temporomandibular joint: radiology, pathology, and basic biomechanics of the jaw. Radiographics. 2003;23:e14. doi: 10.1148/rg.e14. [DOI] [PubMed] [Google Scholar]
- 5.Sava A, Scutariu M. Functional anatomy of the temporo-mandibular joint (II) Rev Med Chir Soc Med Nat Iasi. 2012;116:1213–1217. [PubMed] [Google Scholar]
- 6.Van Eijden TM, Korfage JA, Brugman P. Architecture of the human jaw-closing and jaw-opening muscles. Anat Rec. 1997;248:464–474. doi: 10.1002/(sici)1097-0185(199707)248:3<464::aid-ar20>3.3.co;2-4. [DOI] [PubMed] [Google Scholar]
- 7.Imanimoghaddam M, Madani AS, Hashemi EM. The evaluation of lateral pterygoid muscle pathologic changes and insertion patterns in temporomandibular joints with or without disc displacement using magnetic resonance imaging. Int J Oral Maxillofac Surg. 2013;42:1116–1120. doi: 10.1016/j.ijom.2013.01.022. [DOI] [PubMed] [Google Scholar]
- 8.Tomas X, Pomes J, Berenguer J, Mercader JM, Pons F, Donoso L. Temporomandibular joint soft-tissue pathology, II: Nondisc abnormalities. Semin Ultrasound CT MR. 2007;28:205–212. doi: 10.1053/j.sult.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 9.Tomas X, Pomes J, Berenguer J, Quinto L, Nicolau C, Mercader JM, Castro V. MR imaging of temporomandibular joint dysfunction: a pictorial review. Radiographics. 2006;26:765–781. doi: 10.1148/rg.263055091. [DOI] [PubMed] [Google Scholar]
- 10.Koolstra JH. Dynamics of the human masticatory system. Crit Rev Oral Biol Med. 2002;13:366–376. doi: 10.1177/154411130201300406. [DOI] [PubMed] [Google Scholar]
- 11.Lobbezoo F, Drangsholt M, Peck C, Sato H, Kopp S, Svensson P. Topical review: new insights into the pathology and diagnosis of disorders of the temporomandibular joint. J Orofac Pain. 2004;18:181–191. [PubMed] [Google Scholar]
- 12.Harms SE, Wilk RM. Magnetic resonance imaging of the temporomandibular joint. Radiographics. 1987;7:521–542. doi: 10.1148/radiographics.7.3.3448646. [DOI] [PubMed] [Google Scholar]
- 13.Katzberg RW. Temporomandibular joint imaging. Radiology. 1989;170:297–307. doi: 10.1148/radiology.170.2.2643133. [DOI] [PubMed] [Google Scholar]
- 14.Rao VM, Bacelar MT. MR imaging of the temporomandibular joint. Magn Reson Imaging Clin N Am. 2002;10:615–630. doi: 10.1016/s1064-9689(02)00011-9. [DOI] [PubMed] [Google Scholar]
- 15.Drace JE, Enzmann DR. Defining the normal temporomandibular joint: closed-, partially open-, and open-mouth MR imaging of asymptomatic subjects. Radiology. 1990;177:67–71. doi: 10.1148/radiology.177.1.2399340. [DOI] [PubMed] [Google Scholar]
- 16.Katzberg RW, Westesson PL, Tallents RH, Drake CM. Anatomic disorders of the temporomandibular joint disc in asymptomatic subjects. J Oral Maxillofac Surg. 1996;54:147–153; discussion 153-155. doi: 10.1016/s0278-2391(96)90435-8. [DOI] [PubMed] [Google Scholar]
- 17.Rammelsberg P, Pospiech PR, Jäger L, Pho Duc JM, Böhm AO, Gernet W. Variability of disk position in asymptomatic volunteers and patients with internal derangements of the TMJ. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:393–399. doi: 10.1016/s1079-2104(97)90248-1. [DOI] [PubMed] [Google Scholar]
- 18.Tallents RH, Katzberg RW, Murphy W, Proskin H. Magnetic resonance imaging findings in asymptomatic volunteers and symptomatic patients with temporomandibular disorders. J Prosthet Dent. 1996;75:529–533. doi: 10.1016/s0022-3913(96)90458-8. [DOI] [PubMed] [Google Scholar]
- 19.Orsini MG, Kuboki T, Terada S, Matsuka Y, Yamashita A, Clark GT. Diagnostic value of 4 criteria to interpret temporomandibular joint normal disk position on magnetic resonance images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:489–497. doi: 10.1016/s1079-2104(98)90380-8. [DOI] [PubMed] [Google Scholar]
- 20.Provenzano Mde M, Chilvarquer I, Fenyo-Pereira M. How should the articular disk position be analyzed? J Oral Maxillofac Surg. 2012;70:1534–1539. doi: 10.1016/j.joms.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 21.Vilanova JC, Barceló J, Puig J, Remollo S, Nicolau C, Bru C. Diagnostic imaging: magnetic resonance imaging, computed tomography, and ultrasound. Semin Ultrasound CT MR. 2007;28:184–191. doi: 10.1053/j.sult.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 22.Westesson PL O-YM, Sano T, Okano T. Anatomy, Pathology, and Imaging of the Temporomandibular Joint. In: Som PM, Curtin HD, ed , editors. Head and Neck Imaging-2 Volume Set, 5th Edition. St. Louis: Mosby; 2011. pp. 1547–613. [Google Scholar]
- 23.Dennison J, Mahoney P, Herbison P, Dias G. The false and the true bifid condyles. Homo. 2008;59:149–159. doi: 10.1016/j.jchb.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 24.Lacout A, Marsot-Dupuch K, Smoker WR, Lasjaunias P. Foramen tympanicum, or foramen of Huschke: pathologic cases and anatomic CT study. AJNR Am J Neuroradiol. 2005;26:1317–1323. [PMC free article] [PubMed] [Google Scholar]
- 25.Tozoglu U, Caglayan F, Harorli A. Foramen tympanicum or foramen of Huschke: anatomical cone beam CT study. Dentomaxillofac Radiol. 2012;41:294–297. doi: 10.1259/dmfr/62359484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tank W, Wright D, Iizuka T. Unilateral dysplasia of the mandibular condyle: report of a case. J Oral Maxillofac Surg. 1998;56:765–769. doi: 10.1016/s0278-2391(98)90816-3. [DOI] [PubMed] [Google Scholar]
- 27.Berger SS, Stewart RE. Mandibular hypoplasia secondary to perinatal trauma: report of case. J Oral Surg. 1977;35:578–582. [PubMed] [Google Scholar]
- 28.Kaneyama K, Segami N, Hatta T. Congenital deformities and developmental abnormalities of the mandibular condyle in the temporomandibular joint. Congenit Anom (Kyoto) 2008;48:118–125. doi: 10.1111/j.1741-4520.2008.00191.x. [DOI] [PubMed] [Google Scholar]
- 29.Wolford LM. Idiopathic condylar resorption of the temporomandibular joint in teenage girls (cheerleaders syndrome) Proc (Bayl Univ Med Cent) 2001;14:246–252. doi: 10.1080/08998280.2001.11927772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Angiero F, Farronato G, Benedicenti S, Vinci R, Farronato D, Magistro S, Stefani M. Mandibular condylar hyperplasia: clinical, histopathological, and treatment considerations. Cranio. 2009;27:24–32. doi: 10.1179/crn.2009.005. [DOI] [PubMed] [Google Scholar]
- 31.Ladeira DB, Barbosa GL, Nascimento MC, Cruz AD, Freitas DQ, Almeida SM. Prevalence and characteristics of pneumatization of the temporal bone evaluated by cone beam computed tomography. Int J Oral Maxillofac Surg. 2013;42:771–775. doi: 10.1016/j.ijom.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 32.Miloglu O, Yilmaz AB, Yildirim E, Akgul HM. Pneumatization of the articular eminence on cone beam computed tomography: prevalence, characteristics and a review of the literature. Dentomaxillofac Radiol. 2011;40:110–114. doi: 10.1259/dmfr/75842018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rudisch A, Innerhofer K, Bertram S, Emshoff R. Magnetic resonance imaging findings of internal derangement and effusion in patients with unilateral temporomandibular joint pain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:566–571. doi: 10.1067/moe.2001.116817. [DOI] [PubMed] [Google Scholar]
- 34.Cholitgul W, Nishiyama H, Sasai T, Uchiyama Y, Fuchihata H, Rohlin M. Clinical and magnetic resonance imaging findings in temporomandibular joint disc displacement. Dentomaxillofac Radiol. 1997;26:183–188. doi: 10.1038/sj.dmfr.4600239. [DOI] [PubMed] [Google Scholar]
- 35.Larheim TA, Westesson P, Sano T. Temporomandibular joint disk displacement: comparison in asymptomatic volunteers and patients. Radiology. 2001;218:428–432. doi: 10.1148/radiology.218.2.r01fe11428. [DOI] [PubMed] [Google Scholar]
- 36.Ribeiro RF, Tallents RH, Katzberg RW, Murphy WC, Moss ME, Magalhaes AC, Tavano O. The prevalence of disc displacement in symptomatic and asymptomatic volunteers aged 6 to 25 years. J Orofac Pain. 1997;11:37–47. [PubMed] [Google Scholar]
- 37.Paesani D, Westesson PL, Hatala M, Tallents RH, Kurita K. Prevalence of temporomandibular joint internal derangement in patients with craniomandibular disorders. Am J Orthod Dentofacial Orthop. 1992;101:41–47. doi: 10.1016/0889-5406(92)70080-T. [DOI] [PubMed] [Google Scholar]
- 38.Tasaki MM, Westesson PL, Raubertas RF. Observer variation in interpretation of magnetic resonance images of the temporomandibular joint. Oral Surg Oral Med Oral Pathol. 1993;76:231–234. doi: 10.1016/0030-4220(93)90210-u. [DOI] [PubMed] [Google Scholar]
- 39.Tasaki MM, Westesson PL, Isberg AM, Ren YF, Tallents RH. Classification and prevalence of temporomandibular joint disk displacement in patients and symptom-free volunteers. Am J Orthod Dentofacial Orthop. 1996;109:249–262. doi: 10.1016/s0889-5406(96)70148-8. [DOI] [PubMed] [Google Scholar]
- 40.Sano T, Yamamoto M, Okano T. Temporomandibular joint: MR imaging. Neuroimaging Clin N Am. 2003;13:583–595. doi: 10.1016/s1052-5149(03)00033-9. [DOI] [PubMed] [Google Scholar]
- 41.Som PM, Bergeron RT. Head and neck imaging. 2nd ed. St. Louis: Mosby Year Book; 1991. [Google Scholar]
- 42.de Leeuw R, Boering G, Stegenga B, de Bont LG. TMJ articular disc position and configuration 30 years after initial diagnosis of internal derangement. J Oral Maxillofac Surg. 1995;53:234–241; discussion 241-242. doi: 10.1016/0278-2391(95)90215-5. [DOI] [PubMed] [Google Scholar]
- 43.Suenaga S, Hamamoto S, Kawano K, Higashida Y, Noikura T. Dynamic MR imaging of the temporomandibular joint in patients with arthrosis: relationship between contrast enhancement of the posterior disk attachment and joint pain. AJR Am J Roentgenol. 1996;166:1475–1481. doi: 10.2214/ajr.166.6.8633468. [DOI] [PubMed] [Google Scholar]
- 44.Helms CA, Kaban LB, McNeill C, Dodson T. Temporomandibular joint: morphology and signal intensity characteristics of the disk at MR imaging. Radiology. 1989;172:817–820. doi: 10.1148/radiology.172.3.2772194. [DOI] [PubMed] [Google Scholar]
- 45.Chossegros C, Cheynet F, Guyot L, Bellot-Samson V, Blanc JL. Posterior disk displacement of the TMJ: MRI evidence in two cases. Cranio. 2001;19:289–293. doi: 10.1080/08869634.2001.11746180. [DOI] [PubMed] [Google Scholar]
- 46.Katzberg RW, Westesson PL, Tallents RH, Anderson R, Kurita K, Manzione JV, Totterman S. Temporomandibular joint: MR assessment of rotational and sideways disk displacements. Radiology. 1988;169:741–748. doi: 10.1148/radiology.169.3.3186996. [DOI] [PubMed] [Google Scholar]
- 47.Konttinen YT, Ainola M, Valleala H, Ma J, Ida H, Mandelin J, Kinne RW, Santavirta S, Sorsa T, López-Otín C, et al. Analysis of 16 different matrix metalloproteinases (MMP-1 to MMP-20) in the synovial membrane: different profiles in trauma and rheumatoid arthritis. Ann Rheum Dis. 1999;58:691–697. doi: 10.1136/ard.58.11.691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schellhas KP, Wilkes CH. Temporomandibular joint inflammation: comparison of MR fast scanning with T1- and T2-weighted imaging techniques. AJR Am J Roentgenol. 1989;153:93–98. doi: 10.2214/ajr.153.1.93. [DOI] [PubMed] [Google Scholar]
- 49.Roberts D, Schenck J, Joseph P, Foster T, Hart H, Pettigrew J, Kundel HL, Edelstein W, Haber B. Temporomandibular joint: magnetic resonance imaging. Radiology. 1985;154:829–830. doi: 10.1148/radiology.154.3.3969490. [DOI] [PubMed] [Google Scholar]
- 50.Katzberg RW, Westesson P-L. Diagnosis of the temporomandibular joint, 1e. Philadelphia: W. B. Saunders Co; 1993. [Google Scholar]
- 51.Cholitgul W, Petersson A, Rohlin M, Akerman S. Clinical and radiological findings in temporomandibular joints with disc perforation. Int J Oral Maxillofac Surg. 1990;19:220–225. doi: 10.1016/s0901-5027(05)80396-0. [DOI] [PubMed] [Google Scholar]
- 52.Kondoh T, Westesson PL, Takahashi T, Seto K. Prevalence of morphological changes in the surfaces of the temporomandibular joint disc associated with internal derangement. J Oral Maxillofac Surg. 1998;56:339–343; discussion 343-344. doi: 10.1016/s0278-2391(98)90111-2. [DOI] [PubMed] [Google Scholar]
- 53.Widmalm SE, Westesson PL, Kim IK, Pereira FJ, Lundh H, Tasaki MM. Temporomandibular joint pathosis related to sex, age, and dentition in autopsy material. Oral Surg Oral Med Oral Pathol. 1994;78:416–425. doi: 10.1016/0030-4220(94)90031-0. [DOI] [PubMed] [Google Scholar]
- 54.Kuribayashi A, Okochi K, Kobayashi K, Kurabayashi T. MRI findings of temporomandibular joints with disk perforation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:419–425. doi: 10.1016/j.tripleo.2007.11.020. [DOI] [PubMed] [Google Scholar]
- 55.Yura S, Nobata K, Shima T. Diagnostic accuracy of fat-saturated T2-weighted magnetic resonance imaging in the diagnosis of perforation of the articular disc of the temporomandibular joint. Br J Oral Maxillofac Surg. 2012;50:365–368. doi: 10.1016/j.bjoms.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 56.Larheim TA, Katzberg RW, Westesson PL, Tallents RH, Moss ME. MR evidence of temporomandibular joint fluid and condyle marrow alterations: occurrence in asymptomatic volunteers and symptomatic patients. Int J Oral Maxillofac Surg. 2001;30:113–117. doi: 10.1054/ijom.2000.0018. [DOI] [PubMed] [Google Scholar]
- 57.Westesson PL, Brooks SL. Temporomandibular joint: relationship between MR evidence of effusion and the presence of pain and disk displacement. AJR Am J Roentgenol. 1992;159:559–563. doi: 10.2214/ajr.159.3.1503025. [DOI] [PubMed] [Google Scholar]
- 58.Smith HJ, Larheim TA, Aspestrand F. Rheumatic and nonrheumatic disease in the temporomandibular joint: gadolinium-enhanced MR imaging. Radiology. 1992;185:229–234. doi: 10.1148/radiology.185.1.1523314. [DOI] [PubMed] [Google Scholar]
- 59.Lafrenière CM, Lamontagne M, el-Sawy R. The role of the lateral pterygoid muscles in TMJ disorders during static conditions. Cranio. 1997;15:38–52. doi: 10.1080/08869634.1997.11745991. [DOI] [PubMed] [Google Scholar]
- 60.Yang X, Pernu H, Pyhtinen J, Tiilikainen PA, Oikarinen KS, Raustia AM. MR abnormalities of the lateral pterygoid muscle in patients with nonreducing disk displacement of the TMJ. Cranio. 2002;20:209–221. doi: 10.1080/08869634.2002.11746213. [DOI] [PubMed] [Google Scholar]
- 61.Taskaya-Yilmaz N, Ceylan G, Incesu L, Muglali M. A possible etiology of the internal derangement of the temporomandibular joint based on the MRI observations of the lateral pterygoid muscle. Surg Radiol Anat. 2005;27:19–24. doi: 10.1007/s00276-004-0267-6. [DOI] [PubMed] [Google Scholar]
- 62.Schellhas KP, Wilkes CH, Fritts HM, Omlie MR, Heithoff KB, Jahn JA. Temporomandibular joint: MR imaging of internal derangements and postoperative changes. AJR Am J Roentgenol. 1988;150:381–389. doi: 10.2214/ajr.150.2.381. [DOI] [PubMed] [Google Scholar]
- 63.Schellhas KP, Wilkes CH, Fritts HM, Omlie MR, Lagrotteria LB. MR of osteochondritis dissecans and avascular necrosis of the mandibular condyle. AJR Am J Roentgenol. 1989;152:551–560. doi: 10.2214/ajr.152.3.551. [DOI] [PubMed] [Google Scholar]
- 64.Larheim TA, Westesson PL, Hicks DG, Eriksson L, Brown DA. Osteonecrosis of the temporomandibular joint: correlation of magnetic resonance imaging and histology. J Oral Maxillofac Surg. 1999;57:888–898; discussion 899. doi: 10.1016/s0278-2391(99)90001-0. [DOI] [PubMed] [Google Scholar]
- 65.Mesgarzadeh M, Sapega AA, Bonakdarpour A, Revesz G, Moyer RA, Maurer AH, Alburger PD. Osteochondritis dissecans: analysis of mechanical stability with radiography, scintigraphy, and MR imaging. Radiology. 1987;165:775–780. doi: 10.1148/radiology.165.3.3685359. [DOI] [PubMed] [Google Scholar]
- 66.Xiang S, Rebellato J, Inwards CY, Keller EE. Malocclusion associated with osteocartilaginous loose bodies of the temporomandibular joint. J Am Dent Assoc. 2005;136:484–489. doi: 10.14219/jada.archive.2005.0204. [DOI] [PubMed] [Google Scholar]
- 67.Von Arx DP, Simpson MT, Batman P. Synovial chondromatosis of the temporomandibular joint. Br J Oral Maxillofac Surg. 1988;26:297–305. doi: 10.1016/0266-4356(88)90047-2. [DOI] [PubMed] [Google Scholar]
- 68.Norman JE, Stevenson AR, Painter DM, Sykes DG, Feain LA. Synovial osteochondromatosis of the temporomandibular joint. An historical review with presentation of 3 cases. J Craniomaxillofac Surg. 1988;16:212–220. [PubMed] [Google Scholar]
- 69.Boccardi A. CT evaluation of chondromatosis of the temporomandibular joint. J Comput Assist Tomogr. 1991;15:826–828. doi: 10.1097/00004728-199109000-00019. [DOI] [PubMed] [Google Scholar]
- 70.van Ingen JM, de Man K, Bakri I. CT diagnosis of synovial chondromatosis of the temporomandibular joint. Br J Oral Maxillofac Surg. 1990;28:164–167. doi: 10.1016/0266-4356(90)90080-5. [DOI] [PubMed] [Google Scholar]
- 71.Nitzan DW. Temporomandibular joint “open lock” versus condylar dislocation: signs and symptoms, imaging, treatment, and pathogenesis. J Oral Maxillofac Surg. 2002;60:506–11; discussion 512-3. doi: 10.1053/joms.2002.31846. [DOI] [PubMed] [Google Scholar]
- 72.DaSilva AF, Shaefer J, Keith DA. The temporomandibular joint: clinical and surgical aspects. Neuroimaging Clin N Am. 2003;13:573–582. doi: 10.1016/s1052-5149(03)00043-1. [DOI] [PubMed] [Google Scholar]
- 73.Güven O. A clinical study on temporomandibular joint ankylosis. Auris Nasus Larynx. 2000;27:27–33. doi: 10.1016/s0385-8146(99)00045-0. [DOI] [PubMed] [Google Scholar]
- 74.Cannizzaro E, Schroeder S, Müller LM, Kellenberger CJ, Saurenmann RK. Temporomandibular joint involvement in children with juvenile idiopathic arthritis. J Rheumatol. 2011;38:510–515. doi: 10.3899/jrheum.100325. [DOI] [PubMed] [Google Scholar]
- 75.Twilt M, Mobers SM, Arends LR, ten Cate R, van Suijlekom-Smit L. Temporomandibular involvement in juvenile idiopathic arthritis. J Rheumatol. 2004;31:1418–1422. [PubMed] [Google Scholar]
- 76.Weiss PF, Arabshahi B, Johnson A, Bilaniuk LT, Zarnow D, Cahill AM, Feudtner C, Cron RQ. High prevalence of temporomandibular joint arthritis at disease onset in children with juvenile idiopathic arthritis, as detected by magnetic resonance imaging but not by ultrasound. Arthritis Rheum. 2008;58:1189–1196. doi: 10.1002/art.23401. [DOI] [PubMed] [Google Scholar]
- 77.Koh ET, Yap AU, Koh CK, Chee TS, Chan SP, Boudville IC. Temporomandibular disorders in rheumatoid arthritis. J Rheumatol. 1999;26:1918–1922. [PubMed] [Google Scholar]
- 78.Yoshida A, Higuchi Y, Kondo M, Tabata O, Ohishi M. Range of motion of the temporomandibular joint in rheumatoid arthritis: relationship to the severity of disease. Cranio. 1998;16:162–167. doi: 10.1080/08869634.1998.11746054. [DOI] [PubMed] [Google Scholar]
- 79.Kretapirom K, Okochi K, Nakamura S, Tetsumura A, Ohbayashi N, Yoshino N, Kurabayashi T. MRI characteristics of rheumatoid arthritis in the temporomandibular joint. Dentomaxillofac Radiol. 2013;42:31627230. doi: 10.1259/dmfr/31627230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tanaka E, Detamore MS, Mercuri LG. Degenerative disorders of the temporomandibular joint: etiology, diagnosis, and treatment. J Dent Res. 2008;87:296–307. doi: 10.1177/154405910808700406. [DOI] [PubMed] [Google Scholar]
- 81.Hussain AM, Packota G, Major PW, Flores-Mir C. Role of different imaging modalities in assessment of temporomandibular joint erosions and osteophytes: a systematic review. Dentomaxillofac Radiol. 2008;37:63–71. doi: 10.1259/dmfr/16932758. [DOI] [PubMed] [Google Scholar]
- 82.Matsumura Y, Nomura J, Nakanishi K, Yanase S, Kato H, Tagawa T. Synovial chondromatosis of the temporomandibular joint with calcium pyrophosphate dihydrate crystal deposition disease (pseudogout) Dentomaxillofac Radiol. 2012;41:703–707. doi: 10.1259/dmfr/24183821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kahraman AS, Kahraman B, Dogan M, Firat C, Samdanci E, Celik T. Synovial chondromatosis of the temporomandibular joint: radiologic and histopathologic findings. J Craniofac Surg. 2012;23:1211–1213. doi: 10.1097/SCS.0b013e3182564a6e. [DOI] [PubMed] [Google Scholar]
- 84.Wang P, Tian Z, Yang J, Yu Q. Synovial chondromatosis of the temporomandibular joint: MRI findings with pathological comparison. Dentomaxillofac Radiol. 2012;41:110–116. doi: 10.1259/dmfr/36144602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Giannakopoulos H, Chou JC, Quinn PD. Pigmented villonodular synovitis of the temporomandibular joint. Ear Nose Throat J. 2013;92:E10–E13. doi: 10.1177/014556131309200714. [DOI] [PubMed] [Google Scholar]
- 86.Kim KW, Han MH, Park SW, Kim SH, Lee HJ, Jae HJ, Kang JW, Chang KH. Pigmented villonodular synovitis of the temporomandibular joint: MR findings in four cases. Eur J Radiol. 2004;49:229–234. doi: 10.1016/S0720-048X(03)00099-8. [DOI] [PubMed] [Google Scholar]
- 87.Le WJ, Li MH, Yu Q, Shi HM. Pigmented villonodular synovitis of the temporomandibular joint: CT imaging findings. Clin Imaging. 2014;38:6–10. doi: 10.1016/j.clinimag.2013.08.011. [DOI] [PubMed] [Google Scholar]


