Abstract
Background:
Soft-tissue defects around the knees are common in injured limbs and in the same injury the leg is often involved and the thigh is spared. Furthermore due to pliable and relatively lax skin, we have used inferiorly based thigh flap to reconstruct defects around knee joint.
Aims and Objectives:
The aim of this study is to evaluate the use of inferiorly based thigh flap to cover soft-tissue defects over the proximal one-third of the leg, patellar region, knee, and lower thigh.
Materials and Methods:
This study was conducted during the period between October 2011 and February 2013. Inferiorly based anteromedial thigh fasciocutaneous flap was performed on 12 patients and inferiorly based anterolateral thigh fasciocutaneous flap on four patients. The sites of the soft-tissue defects included patellar regions, infrapatellar region, upper one-third of leg, lower thigh, and over the knee joint.
Results:
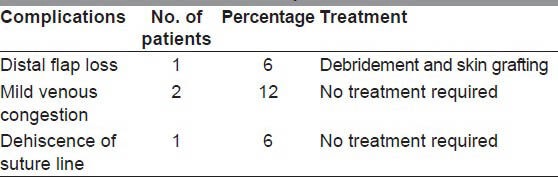
Patients were evaluated post-operatively in terms of viability of flap, the matching of the flap with the recipient site, and donor site morbidity. All the flaps survived well except one which developed distal marginal flap loss, one in which wound dehiscence was noticed, and two in which mild venous congestion was observed. Venous congestion in two patients subsided on its own within 3 days. One patient with wound dehiscence achieved complete healing by secondary intention. Patient who developed distal flap loss required debridement and skin grafting. No appreciable donor site morbidity was encountered. Skin colour and texture of the flap matched well with the recipient site.
Conclusions:
The inferiorly based thigh flap is a reliable flap to cover the defect over proximal one-third of the leg, patellar region, knee, and lower thigh.
KEY WORDS: Defect around the knee joint, inferiorly based thigh flap, perforator based flap
INTRODUCTION
Soft-tissue defects around the knees are common problems in the victims of trauma, post-operative wound or after arthroplasty and excision of various lesions, which is usually associated with bone and implant exposure.[1] Coverage of these defects requires appropriate planning to keep the knee joint functioning. Currently, various reconstructive options available are gastrocnemius flap,[2] sural fasciocutaneous flap,[3] and saphenous flap.[4] These flaps are harvested from the leg, which is usually involved in traumatized lower limb. In this series, therefore, inferiorly based thigh flap has been used, including anteromedial thigh fasciocutaneous flap and anterolateral thigh (ALT) fasciocutaneous flap in 16 patients having soft-tissue defects around the knee joint for the coverage.
Lu et al.[5] first confirmed the presence of at least one supragenicular fasciocutaneous perforator within 3 cm above the adductor tubercle. This perforator arises from the saphenous branch of the descending genicular artery, which accompanies two venae comitantes.[5] Inferiorly based anteromedial thigh fasciocutaneus flap can be taken from anteromedial aspect of thigh, which survives on supragenicular fasciocutaneous perforator.
In 1990, Hayashi and Maruyama[6] have reported the inferiorly based ALT fasciocutaneous flap based on the perforators of the lateral superior genicular artery (LSGA) for reconstruction of defects around the knee, popliteal region, lower third of the thigh, and upper one-third of the leg. Due to variable pathway of its pedicle, this flap was not used widely at that time. Since its description, there are few publications focusing clinical application of this flap.[7,8] It was found in these publications that this flap can be very useful for soft-tissue coverage around knee joints.
To the best of our knowledge, no publications are found that focus on simultaneous use of both inferiorly based anteromedial and anterolateral thigh flap for the reconstruction of defects around the knee joint. This leads to a more versatile use of inferiorly based thigh flap. In this series, we present our clinical experience with the use of inferiorly based thigh fasciocutaneous flap for the reconstruction of defects around the knee joint in 16 patients. These flaps have been potentially useful and advantageous for the coverage of these difficult regions.
MATERIALS AND METHODS
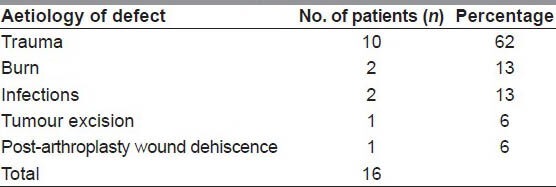
This prospective study was conducted in the period between October 2011 and February 2013. The sites of the soft-tissue defects included patellar region, infrapatellar region, upper one-third of leg, lower thigh, and over the knee joint [Table 1]. The aetiology of the defects were trauma (n = 10), burn (n = 2), infections (n = 2), tumour excision (n = 1), and post-arthroplasty wound dehiscence (n = 1) [Table 2]. Pre-operatively control of infection was confirmed by culture test.
Table 1.
Distribution of wound
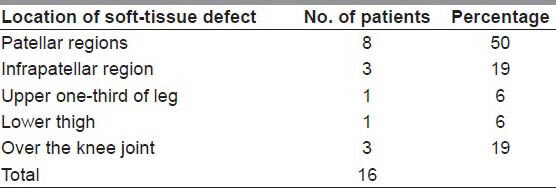
Table 2.
Aetiology of soft-tissue defect
The largest size of the defect was 28 cm × 10 cm, whereas the smallest size was 17 cm × 8 cm. The inferiorly based anteromedial thigh fasciocutaneous flap [Figures 1 and 2] was performed on 12 patients and inferiorly based ALT fasciocutaneous flap on four patients [Table 3 and Figure 3]. The size of the flaps ranged from 32 cm × 11 cm to 20 cm × 9 cm depending on the size of the defect.
Figure 1.
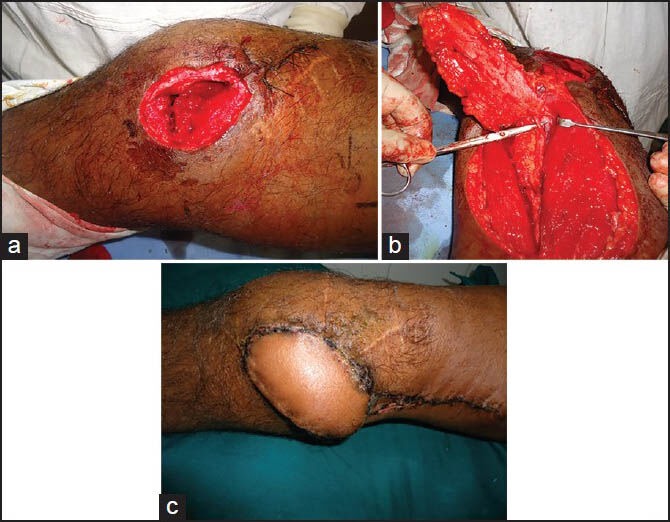
(a) Soft-tissue defect over the knee with exposed joint after debridement. (b) Inferiorly based anteromedial fasciocutaneous flap with supragenicular perforators identified. (c) Follow-up photograph
Figure 2.

(a) Soft-tissue defect over infrapatellar region before debridement. (b) intra-operative photograph after inferiorly based anteromedial thigh fasciocutaneous flap was raised. (c) Long term follow-up photograph
Table 3.
Types and sizes of flap used
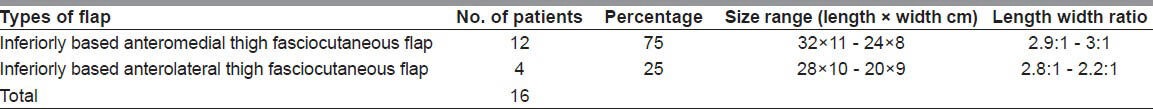
Figure 3.

(a) Unstable scar lateral part of right knee with involved leg. (b) Soft-tissue defect after debridement and arc of rotation of the inferiorly based anterolateral thigh fasciocutaneous flap. (c) Post-operative photograph showing well set flap and skin grafted donor site
SURGICAL ANATOMY
Anteromedial thigh flap
The saphenous artery originates from the descending genicular artery at 9.16 ± 1.36 cm proximal to the adductor tubercle, and it travels distally towards the knee joint within the adductor canal.[5] Saphenous artery and its venae comitantes give off supragenicular fasciocutaneous perforator and its venae comitantes, which supply the inferiorly based anteromedial thigh flap. The saphenous artery with its venae comitantes penetrates the adductor aponeurotic plate into a space formed by the Sartorius anteriorly and adductor magnus posteriorly at the distal part of the adductor canal.
The saphenous artery travels distally into the subcutaneous tissue between the sartorius and gracilis. In this course, saphenous artery is accompanied by the saphenous nerve and gives off 2-5 direct fasciocutaneous perforators and 2-6 musculocutaneous perforators. These perforators supply the overlying skin and underlying sartorius muscle. At least one supragenicular fasciocutaneous perforator always arises from the saphenous artery within 3 cm proximal to the adductor tubercle and it accompanies two venae comitantes.[5] Supragenicular fasciocutaneous perforator passes through the anterior margin of sartorius in 90% of cases and in remaining cases, it passes through the posterior margin of the sartorius. Supragenicular perforator divides into ascending and descending branches. The ascending branch anastomoses with subcutaneous branches arising from other perforators of the saphenous artery, thus, forms a subcutaneous vascular plexus to supply the skin overlying inferiorly based anteromedial thigh flap.
Anterolateral thigh flap
The lateral superior genicular artery originates from popliteal artery. It travels superolaterally and gives branches to the knee joint, vastus lateralis, and biceps femoris. It runs in the intermuscular space between vastus lateralis and biceps femoris. Then, it penetrates through the deep fascia proximal to the knee joint just above the lateral condyle of the femur and terminates as a skin perforator in this region.[9] The cutaneous perforators of LSGA penetrate through the deep fascia 5 cm proximal to the femoral condyle. The terminal branches of these perforators anastomose with musculocutaneous/septocutaneous perforators of the lateral circumflex femoral artery and perforator of profunda femoris and popliteal artery.[6]
SURGICAL TECHNIQUE
All the patients were operated under spinal anaesthesia in the supine position.
Anteromedial thigh flap
The axis of the flap is delineated by drawing a line between the medial femoral epicondyle and midpoint of the inguinal ligament on the anteromedial aspect of the thigh. Supragenicular fasciocutaneous perforator arises from the saphenous artery within 3 cm above the adductor tubercle, which is the pivot point of the flap. Pre-operatively, location of these perforators is confirmed using hand-held Doppler, recipient site is prepared, and the size of the defect is measured. The size and location of the flaps were designed by following basic principle of the plastic surgery of planning in reverse.
First of all, the lateral border of the flap was incised and dissection was performed in the subfascial plane towards the medial side. During this process, intermuscular septum between vastus medialis and sartorius was identified and incised. Then, supragenicular perforator was identified along the anterior border of sartorius. This perforator was found within 5 cm of adductor tubercle. After visualisation of perforator, superior and medial borders of flap were incised and dissection continued proximodistally. Flap was, then, transferred to the defect. Donor site was closed primarily in most of the cases. In addition, skin grafting was required in some cases.
Anterolateral thigh flap
First of all, a line was drawn on the anterolateral aspect of thigh between the anterior superior iliac spine and the lateral border of the patella. Using hand-held Doppler, cutaneous perforator was marked around the lower part of this line. Again, similar to anteromedial thigh flap, by following the principle of planning in reverse, flap was designed. Dissection was performed proximodistally in the subfascial plane and intermuscular septum between rectus femoris and the vastus lateralis muscle was incised. During the process of dissection, perforators were identified at the pre-operatively marked sites in the space between vastus lateralis and biceps femoris just proximal to the lateral condyle of femur. After identification of the perforators, flap was rotated about 5 cm above the patella and transferred at the recipient site. Donor site was skin grafted.
RESULTS
All the patients were evaluated post-operatively in terms of viability of flap, the matching of flap with the recipient site and donor site morbidity. All flaps survived completely except one in which distal flap loss was noted and three in which minor complications occurred, including mild venous congestion in two patients and wound dehiscence in one patient [Table 4]. Patient with distal flap loss required debridement and split thickness skin graft. Venous congestion in two patients subsided on its own within 3 days. One patient with ALT flap with suture line dehiscence achieved healing by regular dressings and antibiotics. The donor site healed well without major complications in all patients except acceptable minimal scar line and donor site skin graft. Two patients were dissatisfied with the appearance of the thigh due to skin graft. Skin colour and texture of the flap matching well with the recipient site was also observed.
Table 4.
Complications
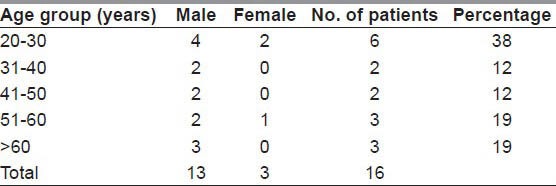
Majority of the patients (38%) were in the age group of 20-30 years and male:female ratio was 4:1 [Table 5].
Table 5.
Age and sex distribution
DISCUSSION
The aim of coverage of soft-tissue defect around the knee joint is to provide aesthetically acceptable appearance and maintain the function of joint.[10] There are many possible reconstructive options for the coverage of these defects. The flap can be harvested from the leg or thigh. Flap harvested from the leg can be muscle flap or fasciocutaneous flap. Muscle flaps are too bulky to provide better contouring to the knee. Fasciocutaneous flaps can be harvested, but it is difficult in a traumatised limb.
Local random flap can cover only small defect and has unreliable vascularity. Cross leg flap has difficulty in immobilising the limb for 3 weeks. The vastus lateralis is too bulky giving unacceptable appearance and donor site problem.[11] The gastrocnemius flap is one of the good alternatives, but the low volume of the distal part of the muscle is a disadvantage, which is incapable of providing good coverage in large defect in suprapatellar region.[2,12] The sural artery flap can also be used due to its thin and pliable nature, but its size is limited.[13,14] Free flap is one of the good options that provide good coverage in one stage, but its use is difficult as it requires expertise, long operating time, and deep location of recipient vessels in this region.[15]
Local advancement or rotation flaps is useful only for very small defects around the knee joint.[16] Moscatiello et al.[17] used skin islands from the distal anteromedial aspect of the thighs of six patients as local perforator flaps in order to reconstruct the peripatellar region and upper leg soft-tissue defects. They concluded that the propeller distal anteromedial thigh perforator flap can reliably be transferred based on the only one adequate perforator vessel, but the disadvantage is that it becomes a microsurgical technique where the dissection of the pedicle is performed by using binocular magnifying glasses.
Since thigh is usually spared in the traumatised limb, and due to pliable and relatively lax skin, it is convenient to harvest flap from this region. Depending upon the location of the defect around the knee joint, flap can be harvested from the anteromedial or antero-lateral thigh.
Lu et al.[18] performed their study on cadavers and confirmed the presence of supragenicular fasciocutaneous perforator within 3 cm above the adductor tubercle. These perforators originate from saphenous branch of the descending genicular artery. They performed their study on 11 patients with skin defects over the popliteal fossa, proximal 1/3 leg, and amputation stump below knee. Using distally based anteromedial thigh flaps, they successfully covered these defects and showed acceptable functional and cosmetic results in terms of movement at the knee joint and matching of skin paddle with the recipient site respectively.
Chou et al.[19] described the distally based anteromedial thigh fasciocutaneous island flap for patellar soft-tissue reconstruction in seven patients. These island flaps were based on cutaneous feeders’ vessels and perforator vessels in the muscle septum and deep fascia of the saphenous artery. In their series, all flaps survived uneventfully with only one having venous congestion.
In our series, we performed inferiorly based anteromedial thigh flap on 12 patients with a size ranging from 32 cm × 11 cm to 24 cm × 8 cm (length to width ratio 2.9:1-3:1). All the flaps survived well except two, out of which, one developed mild venous congestion, which subsided after removing compressive dressings, whereas other developed distal flap marginal necrosis which, required debridement and skin grafting.
Venous congestion is one of the common complications in distally based flaps. In the Chou et al. study, only one patients developed venous congestion which, subsided after removal of single stitch and compressive dressing. Lin et al. found that venous drainage is not liable to danger in distally based flap despite the presence of valves.[20]
The reasons for distal flap necrosis could not be clearly identified in our series. Compression of pedicle, infection, and poor general condition of the patient could be one of the reasons.
Zumiotti et al.[21] performed an anatomical and histomorphometrical study of the lateral genicular artery flap in 18 fresh cadavers and clinical results of knee reconstruction were demonstrated in four patients. They identified cutaneous perforator of the LSGA in all specimens at a mean distance up to the lateral condyle of the femur of 7.40 ± 2.77 cm and thus, they confirmed the constant location of the vascular pedicle.
It was concluded that inferiorly based thigh fasciocutaneous flap on the perforators of LSGA is a useful option in the reconstruction of the defects around the knee joint.
Al Moktader et al.[22] performed inferiorly based thigh flap on 15 patients on the perforators of LSGA for the reconstruction of defects around the knee joint. They had excellent outcome in all cases except one in which distal marginal flap necrosis was noticed that healed by debridement and dressings.
The inferiorly based thigh perforator flap (LSGAP flap) is closer than the distally based reverse flow ALT flap to the knee or popliteal region, making it more versatile for coverage of defects of these regions.[23]
In our series, all the ALT flap survived well except one in which suture line dehiscence was observed that achieved healing by regular dressings and antibiotics. Old age and infection could be the reasons of wound dehiscence in this case.
Thin tissue, adequate length of vascular pedicle with flexible arc of rotation, early ambulation, cosmetically acceptable appearance and minimal donor site morbidity makes the inferiorly based ALT flap, one of the good alternatives for soft-tissue reconstruction around the knee joint.[24]
Inclusion of the perforators in our series had several advantages. This helped in narrowing the base and increasing the length to breadth ratio of the flap. Narrowing the base also helped in increased rotation of the flap, and to some extent reducing the dog ear.
Regarding the donor site closure, various authors suggest closure in case the size is <8 cm. Donor defect more than 8 cm has to be skin grafted.[25,26] In our series, a donor defect of up to 9 cm was primarily closed, which depends upon laxity of the skin. Since anteromedial thigh skin is more lax as compared with anterolateral thigh, donor site closure in former one was comparatively easier than the later.
One of the advantages of this flap, especially in the Indian scenario, is that the donor site is hidden as compared with the donor sites of the proximally based sural or the gastrocnemius flaps, where the donor site is on the calf, and more prone to visibility as compared to the donor site on the thigh.
CONCLUSION
The inferiorly based thigh flap is a reliable flap to cover the defect over proximal one-third of the leg, patellar region, knee, and lower thigh. The main advantages of this flap are its ability to cover a large area with a hidden donor site.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Misra A, Niranjan NS. Fasciocutaneous flaps based on fascial feeder and perforator vessels for defects in the patellar and peripatellar regions. Plast Reconstr Surg. 2005;115:1625–32. doi: 10.1097/01.prs.0000161255.33398.bf. [DOI] [PubMed] [Google Scholar]
- 2.Ries MD, Bozic KJ. Medial gastrocnemius flap coverage for treatment of skin necrosis after total knee arthroplasty. Clin Orthop Relat Res. 2006;446:186–92. doi: 10.1097/01.blo.0000218723.21720.51. [DOI] [PubMed] [Google Scholar]
- 3.Satoh K, Fukuya F, Matsui A, Onizuka T. Lower leg reconstruction using a sural fasciocutaneous flap. Ann Plast Surg. 1989;23:97–103. doi: 10.1097/00000637-198908000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Torii S, Hayashi Y, Hasegawa M, Sugiura S. Reverse flow saphenous island flap in the patient with below-knee amputation. Br J Plast Surg. 1989;42:517–20. doi: 10.1016/0007-1226(89)90036-2. [DOI] [PubMed] [Google Scholar]
- 5.Lu LJ, Feng B, Gong X, Wang k, Liu Z, Wang D. Clinical study on retrograde fascial flap with a pedicle of supragenicular cutaneous artery arising from saphenous artery. Chin J Microsurg. 2004;27:10–2. [Google Scholar]
- 6.Hayashi A, Maruyama Y. The lateral genicular artery flap. Ann Plast Surg. 1990;24:310–7. doi: 10.1097/00000637-199004000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Hayashi A, Maruyama Y. Lateral intermuscular septum of the thigh and short head of the biceps femoris muscle: An anatomic investigation with new clinical applications. Plast Reconstr Surg. 2001;108:1646–54. doi: 10.1097/00006534-200111000-00032. [DOI] [PubMed] [Google Scholar]
- 8.Spokevicius S, Jankauskas A. Anatomy and clinical applications of a composite cutaneo-subcutaneous flap based on the lateral superior genicular vessels. J Reconstr Microsurg. 1995;11:15–20. doi: 10.1055/s-2007-1006505. [DOI] [PubMed] [Google Scholar]
- 9.Sobotta J. 19th ed. Rio de Janeiro: Guanabara Koogan; 1993. Atlas De Anatomia Humana; p. 70. 71, 77, 203, 364. [Google Scholar]
- 10.Hallock GG. Local knee random fasciocutaneous flaps. Ann Plast Surg. 1989;23:289–96. doi: 10.1097/00000637-198910000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Necmioglu S, Askar I, Lök V, Subasi M. Use of the vastus lateralis muscle flap with a grooving procedure in the surgical treatment of chronic osteomyelitis of the femur. Ann Plast Surg. 2004;53:570–6. doi: 10.1097/01.sap.0000134752.01294.d0. [DOI] [PubMed] [Google Scholar]
- 12.Gravvanis AI, Iconomou TG, Panayotou PN, Tsoutsos DA. Medial gastrocnemius muscle flap versus distally based anterolateral thigh flap: Conservative or modern approach to the exposed knee joint? Plast Reconstr Surg. 2005;116:932–4. doi: 10.1097/01.prs.0000180888.41899.a8. [DOI] [PubMed] [Google Scholar]
- 13.Umemoto Y, Adachi Y, Ebisawa K. The sural artery perforator flap for coverage of defects of the knee and tibia. Scand J Plast Reconstr Surg Hand Surg. 2005;39:209–12. doi: 10.1080/02844310410004964. [DOI] [PubMed] [Google Scholar]
- 14.Hallock GG. The medial sural (Medial Gastrocnemius) perforator local flap. Ann Plast Surg. 2004;53:501–5. doi: 10.1097/01.sap.0000116338.59679.12. [DOI] [PubMed] [Google Scholar]
- 15.Sharma RK, Nanda V, Makkar S, Parasher A. De-epithelialised fasciocutaneous turnover flap: An alternative for defects in lower thigh and knee joint. Indian J Plast Surg. 2004;37:40. [Google Scholar]
- 16.Chen CY, Hsieh CH, Kuo YR, Jeng SF. An anterolateral thigh perforator flap from the ipsilateral thigh for soft-tissue reconstruction around the knee. Plast Reconstr Surg. 2007;120:470–3. doi: 10.1097/01.prs.0000267432.03348.97. [DOI] [PubMed] [Google Scholar]
- 17.Moscatiello F, Masià J, Carrera A, Clavero JA, Larrañaga JR, Pons G. The ‘propeller’ distal anteromedial thigh perforator flap. Anatomic study and clinical applications. J Plast Reconstr Aesthet Surg. 2007;60:1323–30. doi: 10.1016/j.bjps.2007.02.027. [DOI] [PubMed] [Google Scholar]
- 18.Lu LJ, Gong X, Cui JL, Liu B. The anteromedial thigh fasciocutaneous flap pedicled on the supragenicular septocutaneous perforator: Application in 11 patients. Ann Plast Surg. 2011;67:275–8. doi: 10.1097/SAP.0b013e3181f89151. [DOI] [PubMed] [Google Scholar]
- 19.Chou LS, Chang KC, Lin TW, Chou HC. Distally based anteromedial thigh fasciocutaneous island flap for patellar soft tissue reconstruction. J Trauma. 2009;66:1146–51. doi: 10.1097/TA.0b013e31817156b4. [DOI] [PubMed] [Google Scholar]
- 20.Lin SD, Lai CS, Chiu CC. Venous drainage in the reverse forearm flap. Plast Reconstr Surg. 1984;74:508–12. doi: 10.1097/00006534-198410000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Zumiotti AV, Teng HW, Briceno NCQ, Lotierzo PH, Ishida LH, Montag E, et al. Lateral flap of the thigh based upon the lateral superior genicular artery: An anatomic and histomorphometric study and clinical applications. Acta Ortop Bras. 2005;13:24. [Google Scholar]
- 22.Al Moktader MA, Hassan M, Taman E, Taha A, Elawa S. Lateral superior genicular flap for reconstruction around the knee. Egypt J Plast Reconstr Surg. 2010;34:223–6. [Google Scholar]
- 23.Zhang G. Reversed anterolateral thigh island flap and myocutaneous flap transplantation. Zhonghua Yi Xue Za Zhi. 1990;70:676–8. 46. [PubMed] [Google Scholar]
- 24.Taniguchi Y, Kitano T, Shimoe T, Asai Y, Yoshida M. Superior lateral genicular artery flap for coverage of a soft tissue defect after total knee arthroplasty. J Reconstr Microsurg. 2009;25:479–82. doi: 10.1055/s-0029-1234026. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Q, Qiao Q, Yang X, Wang H, Robb GL, Zhou G. Clinical application of the anterolateral thigh flap for soft tissue reconstruction. J Reconstr Microsurg. 2010;26:87–94. doi: 10.1055/s-0029-1243292. [DOI] [PubMed] [Google Scholar]
- 26.Hong JP, Shin HW, Kim JJ, Wei FC, Chung YK. The use of anterolateral thigh perforator flaps in chronic osteomyelitis of the lower extremity. Plast Reconstr Surg. 2005;115:142–7. [PubMed] [Google Scholar]


