Abstract
Background:
The importance of adequate nutritional support in burned patients cannot be overemphasised. For adequate long-term compliance by the patients, diet should be formulated in accordance with their pre-burn dietary habits, religious beliefs, and tastes.
Patients and Methods:
A study was conducted in 42 consecutive patients suffering from 10% to 50% of 2nd and 3rd degree thermal burns with the aim to compare nutritional status, clinical outcome, and cost-effectiveness of vegetarian and non-vegetarian diets. The patients were divided into two groups depending upon their pre-injury food habits. Total calories were calculated by Curreri formula. Both groups were compared by various biochemical parameters, microbiological investigations, weight, status of wound healing, graft take, and hospital stay and they were followed for at least 60 days postburn.
Results:
The results were comparable in both groups. Vegetarian diet was found to be more palatable and cost-effective.
Conclusion:
Vegetarian diet is a safe and viable option for the patients suffering from burn injury. The common belief that non-vegetarian diet is superior to vegetarian diet is a myth.
KEY WORDS: Burns, diet, non-vegetarian, vegetarian, wound healing
INTRODUCTION
It is a common belief that non-vegetarian diets are superior to the vegetarian diets and people who take them are healthier and stronger. However, there are no scientific data to prove this. The people who are vegetarians take such foods due to ethical, moral, cultural, religious, or political reasons. It is well-established that vegetarian diet fulfils protein requirements and provides all the essential amino acids.[1,2] Similar studies have also been conducted in athletes, long distance runners, and bodybuilders.[3]
In spite of that, in our part of country it is customary to give meat and eggs in maximum tolerable quantity to patients recovering from any type of injury and whenever diet rich in calories with high protein is advised. The magnitude of nutritional demand in burn patients is virtually unsurpassed by any other disease process.[4] Even those who are otherwise vegetarians are forced to take meat and eggs for expected better recovery. This observation was constantly made in our burn unit. The question arises, is it really necessary for vegetarian burn patients to become non vegetarian; or remain vegetarian, but constantly live under the threat of doubts regarding complete recovery. To find an answer, we decided to conduct a study comparing outcome in burned patients taking vegetarian and non-vegetarian diets. In India, need for such a study was very important because of strong religious beliefs regarding vegetarian and non-vegetarian food.
PATIENTS AND METHODS
The study was conducted in the Department of Plastic Surgery of a tertiary referral teaching hospital having an 18 bedded burn unit. The patients suffering thermal burns involving 10-50% of total body surface area (TBSA) and between 15 and 50 years of age; who reported to our centre within 24 hours of sustaining the injury were included in the study over a period of 1 year. Among these, patients having pre-existing co morbidities such as respiratory disease, cardiac disease, renal disease, and diabetes mellitus were excluded from the study. Patients with inhalational burn injury were also excluded. A total of 42 patients were included in the study over period of 1 year. The patients were assigned to either of the two groups (Group A on vegetarian diet and Group B on non-vegetarian diet) depending on their preinjury food habits. Thus, 23 patients were included in Group A and 19 patients in Group B. After initial fluid resuscitation, patients were put on enteral diets within 24-48 hours of suffering burn injury. In patients who were unable to meet the requirement orally, nasogastric tube feeding supplementation was done.
Total energy requirement was calculated using Curreri formula.[5] We started one-fourth of the requirement at the time of admission and then progressed to full diet using the formula by 4th -5th post burn day. Vitamins and minerals were added to both groups according to the weight of the individual (in similar dose). The vegetarian and non-vegetarian constituents of the diet were modified according to the group of the patient using food exchange list. Nutritional status assessment was performed by measuring following parameters:
Serum albumin on day 1, 15, and 30.
Weight on day 0, 7, 15, 30, and 60. Initial weight was taken either before resuscitation or pre burn weight of the patient was recorded.
Nitrogen balance on day 1, 15, and 30.
Serum ferritin on day 15 and 30.
Microbiological investigations on weekly basis (wound swab culture and sensitivity, blood culture and sensitivity, urine culture, and sensitivity).
Uniform dressing protocol and antibiotic usage protocol was followed for both groups of patients. Antibiotics were given only if indicated due to presence of infection based on culture and sensitivity.
Weekly progress of the wounds before and after split skin grafting was recorded. Fair estimate of cost of nutrition in both groups was done during treatment. All the patients were followed for 60 days post burn.
OBSERVATIONS AND RESULTS
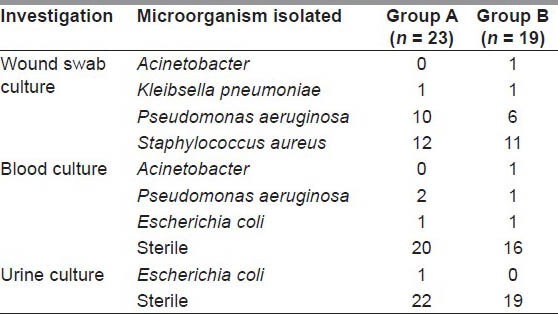
In Group A, age of patients ranged from 15 to 42 years (mean, 25.04 years) with burns ranging from 15% to 50% TBSA (mean, 33.39%). In Group B, age ranged from 15 to 50 years (mean, 25.21 years) with burns ranging from 15% to 45% TBSA (mean, 28.94%) as depicted in Figure 1. Haemoglobin and serum ferritin levels in both groups were comparable [Figures 2 and 3]. Results of serum albumin and total proteins in both the groups were equivocal [Figures 4 and 5]. Nitrogen balance in both groups were negative on 1st day, but was positive on 15th and 30th days [Figure 6]. Weight trends in both groups were comparable as shown in Figure 7. 31.8% in Group A and 36.2% in Group B showed weight loss, which was ranged from 1 to 4 kg at the end of 2 months follow-up. Hospital stay ranged from 10 to 60 days (mean, 27.79 days) in Group A and ranged from 11 to 60 days (mean, 27.26 days) in Group B patients [Figure 8]. Blood transfusions were required only in patients undergoing surgery. The number of units given were decided by the anaesthetist according to the blood loss. Results of microbiological investigations, and antibiotic requirement were also compared. The difference between two groups for wound swab culture (P value - 0.790), blood culture (P value - 0.703), and urine culture (P value - 0.358) were statistically not significant [Table 1]. Fifteen (65.2%) patients in Group A and 11 (58%) patients in Group B required systemic antibiotics during the stay. However, the difference between the two groups was not statistically significant (P value - 0.627).
Figure 1.
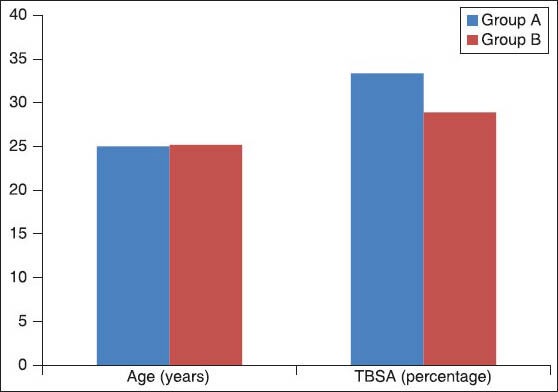
Age and percentage burns in the study group
Figure 2.
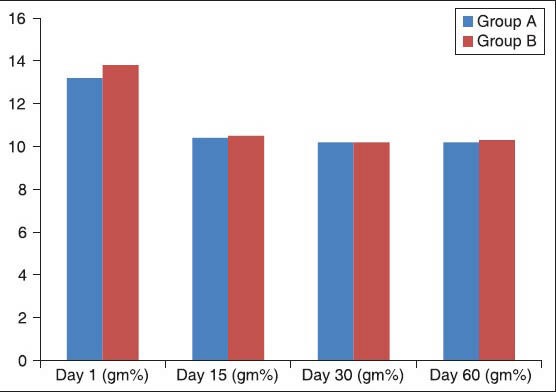
Hemoglobin levels during hospital stay
Figure 3.
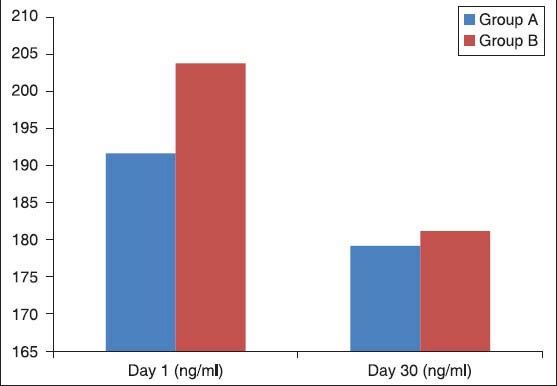
Serum ferritin levels
Figure 4.
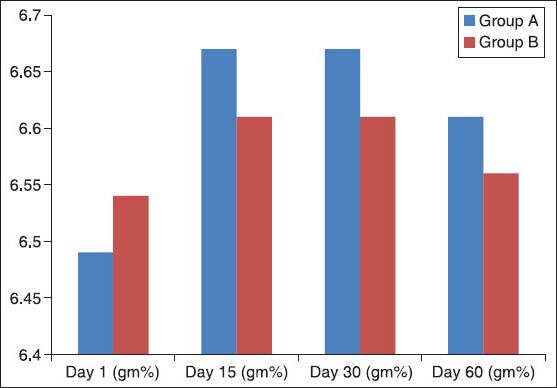
Total protein levels
Figure 5.
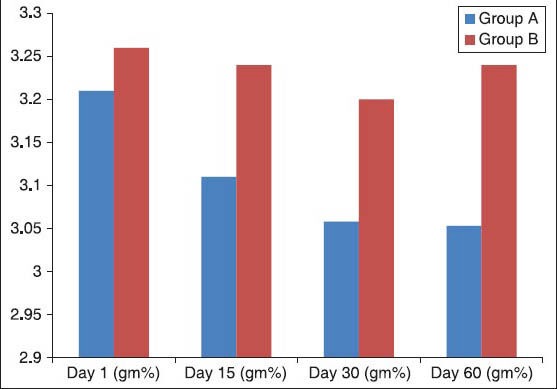
Serum albumin levels
Figure 6.
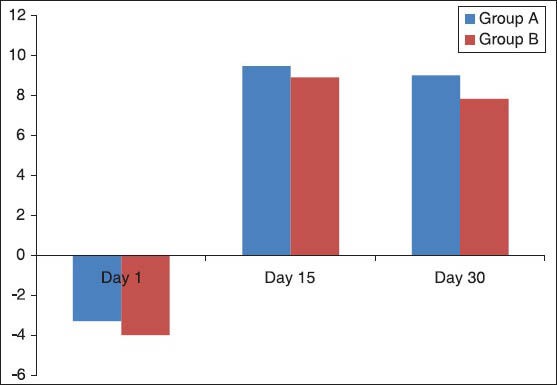
Nitrogen balance during stay
Figure 7.
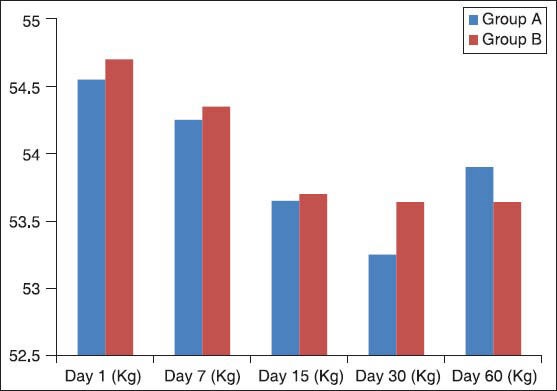
Weight variation during stay
Figure 8.
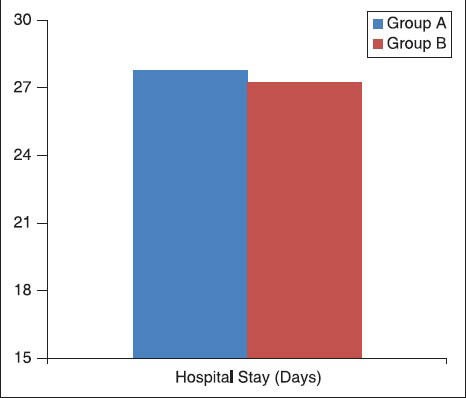
Average hospital stay among two groups
Table 1.
Microbiological profile among both groups during hospital stay
11 patients of Group A and 8 patients of Group B underwent split skin grafting for their burn wounds. Three patients of Group A and two patients of Group B could not complete the study since they developed sepsis and were put on parenteral nutrition and later on required ventilatory support. One patient of Group A had major graft loss and had to be grafted again. None among the remaining group of patients had any significant complications.
Effective cost of nutrition for each of the group was also analysed. As both groups primarily differed in the constituent for fulfilling the protein requirement; the cost of this constituent in Rupees per gram protein was calculated and is depicted in Figure 9. The cost of non-vegetarian diet was more than vegetarian diet.
Figure 9.
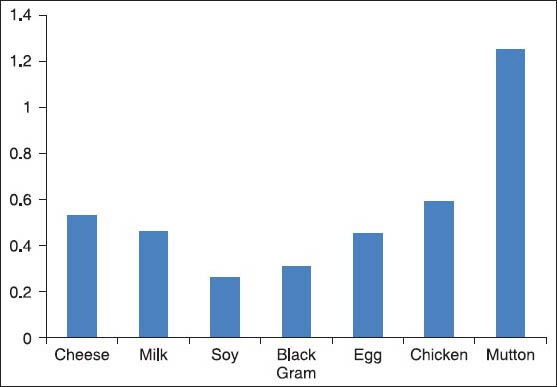
Average cost of protein (rupees per gram) derived from various sources
DISCUSSION
None of the studies ever conducted have proved that non vegetarian diet is superior to vegetarian diet.[6,7,8,9,10,11,12,13,14,15] In burned patients a study comparing non-vegetarian and vegetarian diet has never been conducted previously.
Curreri formula remains the gold standard[16] and was used in our study to calculate the energy requirements of the burned patients. These calculations overestimate the requirements by 20% and hence were used as target levels.[17] We provided 50-60% of total calories from carbohydrates in patients of both groups. It was in accordance with various studies, which showed that only 50-60% of total energy should be from carbohydrates.[4] Overfeeding has to be avoided because excessive carbohydrate feeding can increase oxygen production, cause hyperglycaemia and fatty liver.[18] The ability of burn patient to handle glucose is limited to 5 mg/kg/day, i.e., for an adult 500 g or 2000 cal/day. We provided 20% calories from proteins in patients of both groups. A high protein feed named as burn feed, prepared in our institute by the department of dietetics was provided to patients to meet the protein requirements adequately. In Group B, meat, chicken and eggs were included as replacement for vegetarian sources of proteins. High protein delivery of 1.5-3 g/kg body weight/day or 20-25% of total energy is the maximum required for burn patients.[17] Non protein calorie to nitrogen ratio should be maintained between 150:1-100:1 as done in our study.[18] Fat should constitute no more than 25-30% as energy, but in fact 15-20% of non-protein energy as fat is optimal.[18] We provided vitamins and minerals in equal doses in both study groups. Specific requirements of vitamins and minerals for burn patients have not been established however, provision of zinc and vitamins A and C has been suggested.[19] Early enteral feeding started within 24-48 hours of injury reduced caloric deficits. Target calories were achieved by 5th post burn day in all the patients. Only those five patients who developed sepsis and complications were supported by parenteral nutrition. No incidence of diarrhoea (loose stools more than 3/day) was seen. Gastric bloating was taken care of by advising small quantities of food at more frequent intervals and early mobility.
Anorexia and aversion to food were major hindering factors which prevented the intake of total calorie and protein intake. Patients were offered variations of diet to get maximum co-operation, but basic burn diet regimens as mentioned were followed. All patients on non-vegetarian diet showed aversion to meat, chicken and fish, but with a firm belief of this being a better choice took it with determination. Egg and soups were however, the preferred choice. Lactose intolerance was not seen in any of these patients. Early mobility was helpful in both groups.
Nutritional status of patients was assessed by serial measurements of serum albumin levels, nitrogen balance, serum ferritin levels and weight measurements in our study which are the simplest and easily available indicators of protein anabolism and nutritional status. In addition to that, weekly progress of wound healing, presence of slough and conversion from superficial to deep thickness was recorded. In wounds which were grafted, graft take and graft loss were recorded. Despite their limitations, many of these markers of nutritional status when trended or used collectively can help the clinician in monitoring day to day efficacy of diet in burn management.[4] In our study, we found the difference of serum protein and serum albumin levels in both groups was not statistically significant. The nitrogen balance was also comparable in two groups and the difference was not statistically significant. This observation is consistent with various studies, which shows that the protein intake in both groups are found to be adequate.[6] It has been found in various studies that protein intake in vegetarian and vegan diets is only slightly lower than in meat diets and can meet daily requirements for any person including athletes and bodybuilders.[20] Studies conducted in the United States, Great Britain, Canada, Australia, New Zealand and various European countries, confirmed that vegetarian diets provide more than sufficient protein intake as long as a variety of plant sources are available and consumed.[7]
In our study, the difference of haemoglobin levels between two groups was found to be clinically insignificant. Iron stores are lower in vegetarians because the iron from plant foods is poorly absorbed. The clinical importance of this, if any, is unclear because iron deficiency anaemia rates are found similar in vegetarians and non-vegetarians. The higher vitamin C content of vegetarian diets might improve iron absorption.[8] The preinjury nutritional status of the patient also influences the outcome. Major graft loss occurred in this patient of Group A and had to be grafted again. No other patient had major graft loss. None of the patients had conversion of burns from superficial to deep burns. Meat and chicken need cumbersome cooking whereas cheese can be taken raw and milk and egg by merely boiling. The adequate amount of calorie and protein intake is important rather than the source, whether vegetarian or non-vegetarian. Vegetarian food was however cost-effective and more palatable.
In our study, we have included patient <50% burns. Further studies can be conducted including patients of larger TBSA and larger number of patients. However, all parameters in burned patients are subjected to so many variations, which cannot be rigidly controlled or equalised such as, depth and distribution of burns, blood loss during surgeries, dressing changes, and mobility of the patients.
CONCLUSION
Provision of daily calorie and protein needs in burned patients is very tedious. Motivation and early mobility are required for compliance by patients. Nutritional status and clinical outcome remained unaffected whether patient was on non-vegetarian or vegetarian diet. However, vegetarian diet was found to be more palatable and cost-effective in our study. Thus, vegetarian diet remains a safe and viable option for the patients suffering from burn injury.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hunt JR. Bioavailability of iron, zinc, and other trace minerals from vegetarian diets. Am J Clin Nutr. 2003;78:633S–9. doi: 10.1093/ajcn/78.3.633S. [DOI] [PubMed] [Google Scholar]
- 2.Waldmann A, Koschizke JW, Leitzmann C, Hahn A. Dietary iron intake and iron status of German female vegans: Results of the German vegan study. Ann Nutr Metab. 2004;48:103–8. doi: 10.1159/000077045. [DOI] [PubMed] [Google Scholar]
- 3.Young VR, Pellett PL. Plant proteins in relation to human protein and amino acid nutrition. Am J Clin Nutr. 1994;59:1203S–12S. doi: 10.1093/ajcn/59.5.1203S. [DOI] [PubMed] [Google Scholar]
- 4.Rodriguez DJ. Nutrition in patients with severe burns: State of the art. J Burn Care Rehabil. 1996;17:62–70. doi: 10.1097/00004630-199601000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Curreri PW, Richmond D, Marvin J, Baxter CR. Dietary requirements of patients with major burns. J Am Diet Assoc. 1974;65:415–7. [PubMed] [Google Scholar]
- 6.Messina MJ, Messina VL. Gaithersburg, MD: Aspen Publishers; 1996. The Dietitian's Guide to Vegetarian Diets: Issues and Applications. [Google Scholar]
- 7.Davis B, Melina V. Summertown TN: Book Publishing Company; 2003. The New Becoming Vegetarian; pp. 57–8. [Google Scholar]
- 8.Craig WJ. Iron status of vegetarians. Am J Clin Nutr. 1994;59:1233S–7S. doi: 10.1093/ajcn/59.5.1233S. [DOI] [PubMed] [Google Scholar]
- 9.Freeland-Graves JH, Bodzy PW, Eppright MA. Zinc status of vegetarians. J Am Diet Assoc. 1980;77:655–61. [PubMed] [Google Scholar]
- 10.Sian L, Mingyan X, Miller LV, Tong L, Krebs NF, Hambidge KM. Zinc absorption and intestinal losses of endogenous zinc in young Chinese women with marginal zinc intakes. Am J Clin Nutr. 1996;63:348–53. doi: 10.1093/ajcn/63.3.348. [DOI] [PubMed] [Google Scholar]
- 11.Rosell M, Appleby P, Spencer E, Key T. Weight gain over 5 years in 21,966 meat-eating, fish-eating, vegetarian, and vegan men and women in EPIC-Oxford. Int J Obes (Lond) 2006;30:1389–96. doi: 10.1038/sj.ijo.0803305. [DOI] [PubMed] [Google Scholar]
- 12.Mattson MP. Dordrecht: Kluwer Academic Publishers; 2002. Diet-Brain Connection: Impaction on Memory, Mood, Ageing, and Disease. [Google Scholar]
- 13.Mozafar A. Is there vitamin B12 in plants or not? A plant nutritionist's views. Vegetarian Nutr Int J. 1997;12:50–2. [Google Scholar]
- 14.Herrmann W, Schorr H, Obeid R, Geisel J. Vitamin B-12 status, particularly holotranscobalamin II and methylmalonic acid concentrations, and hyperhomocysteinemia in vegetarians. Am J Clin Nutr. 2003;78:131–6. doi: 10.1093/ajcn/78.1.131. [DOI] [PubMed] [Google Scholar]
- 15.Antony AC. Vegetarianism and vitamin B-12 (cobalamin) deficiency. Am J Clin Nutr. 2003;78:3–6. doi: 10.1093/ajcn/78.1.3. [DOI] [PubMed] [Google Scholar]
- 16.Gottsclich MM, Irenton-Jones CS. The curreri formula: A landmark process for estimating the caloric needs of burn patients. Nutr Clin Pract. 2001;16:172–3. [Google Scholar]
- 17.Ahuja RB, Goel A. Nutrition in burns. Indian J Burns. 1993;1:50–6. [Google Scholar]
- 18.Deitch EA. Nutritional support of the burn patient. Crit Care Clin. 1995;11:735–50. [PubMed] [Google Scholar]
- 19.Prelack K, Dylewski M, Sheridan RL. Practical guidelines for nutritional management of burn injury and recovery. Burns. 2007;33:14–24. doi: 10.1016/j.burns.2006.06.014. [DOI] [PubMed] [Google Scholar]
- 20.Reeves MM, Capra S. Predicting energy requirements in the clinical setting: Are current methods evidence based? Nutr Rev. 2003;61:143–51. doi: 10.1301/nr.2003.apr.143-151. [DOI] [PubMed] [Google Scholar]


