Abstract
INTRODUCTION
Inversion of the uterus is an extremely rare complication of the non-puerperal period and is commonly caused by benign submucous, especially fundal, leiomyomas. A case of a totally inverted cervix due to a prolapsed huge cervical leiomyoma mimicking chronic non-puerperal uterine inversion in a perimenopausal woman is presented.
PRESENTATION OF CASE
A 52-year-old perimenopausal woman was admitted to our clinic with an ulcerated, necrotic, infected and swollen prolapsed mass. Gynecologic history revealed that she was advised myomectomy because of her cervical myoma 2 years ago but she refused to have an operation as she believed that her positive thoughts would shrink the myoma. Presumed diagnosis before surgery was chronic non-puerperal uterine inversion. An intraoperative diagnosis was totally inverted cervix due to a huge cervical leiomyoma. Vaginal hysterectomy without adnexectomy, was performed.
CONCLUSION
This is the first case in the literature which a totally inverted cervix due to a prolapsed huge cervical leiomyoma. Cervical fibroids can grow in perimenopausal period and in extremely rare cases can cause total cervical inversion.
Keywords: Cervical inversion, Prolapsed leiomyoma, Uterine inversion, Vaginal hysterectomy
1. Introduction
Uterine fibroids are the most common tumors of uterus which develop in 20–40% of reproductive age women, but cervical leiomyomas are less than 5% of all leiomyomas.1 Pedunculated uterine myomas or submucosal cervical myomas may protrude through the cervical canal and into the vagina and may become necrotic and occasionally infected due to inadequate blood supply.2,3 In some cases, they can cause uterine inversion. Inversion of the uterus is a very rare complication of the non-puerperal period and is commonly caused by benign submucous, especially fundal, leiomyomas.4
Herein, we present a huge, necrotic, ulcerated and prolapsed cervical leiomyoma causing inversion of the cervix and mimicking non-puerperal uterine inversion. To our knowledge this is the first case in the literature which a totally inverted cervix due to a prolapsed huge cervical leiomyoma mimicking chronic non-puerperal uterine inversion in a perimenopausal woman.
2. Case presentation
A 52 year-old woman, gravida 4, parity 3, abortus 1, was admitted to our clinic with the following complaints: lower abdominal pain and a mass protruding from the vulva for 6 months. She had an abdominal myomectomy 14 years ago and received three units of blood. A cervical myoma uteri 5 cm in diameter was diagnosed 2 years ago in a private hospital and surgery was recommended. She refused operation at that time, believing that her positive thoughts would shrink the mass. She had nine months history of a sensation of something coming out per vaginum, with blood-stained leucorrhoea. Six months ago a protrusion developed from the vagina with severe pain. She did not go to any hospital because she still believed that the mass would disappear with her positive thinking. Before admission to our clinic she tried herbal treatment methods and continued to think positively with the hope that her genital mass would shrink. After six months, she decided to apply to our hospital when the mass became ulcerated, infected and sensitive.
General examination was unremarkable, pulse rate was 94 beats per minute, blood pressure was 140/90 mm Hg, and respiratory rate was 21 cycles per minute. The abdominal examination was normal. A 13 cm × 8 cm solid, inflammated, ulcerated, necrotic mass, protruding from the vaginal introitus was remarkable on pelvic examination and the body of the cervix could not be visualized separate from the mass. Despite the fact that she was perimenopausal period, her leiomyoma grew from 5 cm to 13 cm in two years period. Transvaginal ultrasonographic examination could not be performed because of the unreducible, protruded sensitive vulvar mass. Additionally, the uterus could not recorded during pelvic ultrasonography. Preoperative presumed clinical diagnosis was chronic non-puerperal inversion of the uterus due to submucous leiomyoma. Patient desired hysterectomy without adnexectomy and a vaginal hysterectomy was scheduled.
Pelvic examination under anesthesia, revealed a mass arising from a dilated inverted cervix, and cervical rugae were covering the external surface of the mass (Fig. 1). On bimanual examination the uterus and adnexes were palpated. Intraoperative diagnosis changed to a totally inverted cervix due to a huge prolapsed cervical myoma (Fig. 2). Hysterectomy was begun by the vaginal route. The anterior dissection was carried out and the uterovesical fold opened. The uterine vessels were clamped, cut, and transfixed, then posterior cul-de-sac was opened. Uterine corpus and fundus were normal in appearance. The cornual structures were divided and secured to complete the hysterectomy vaginally. The ovaries appeared normal and were not removed. Macroscopic examination of the operative specimen confirmed the diagnosis of a totally inverted cervix due to a huge prolapsed cervical leiomyoma (Fig. 3). Histopathological examination of the specimen confirmed the diagnosis of a submucous leiomyoma arising from the cervix of the uterus. There were no complications in the postoperative period and the patient was able to be discharged on the third postoperative day.
Fig. 1.

Prolapsed necrotic, ulcerated cervical leiomyoma, (a) necrotic mass, (b) inverted cervix’ rugae.
Fig. 2.
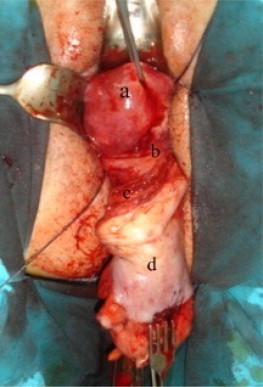
Cervical inversion due to prolapsed myomas with normal uterus, (a) uterus, (b) external cervical os, (c) inverted cervix, and (d) leiomyoma.
Fig. 3.
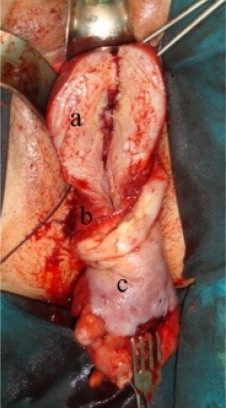
Normal appearance of uterus with prolapsed cervical myoma, (a) normal myometriun and uterine cavity, (b) inverted cervix, and (c) cervical myoma.
3. Discussion
Cervical leiomyomas are extremely rare and the incidence is reported at about 0.6% in total hysterectomy specimens.5 Cervical leiomyomas can be categorized as extracervical type (subserosal location) and intracervical type (occur within the cervix). The complications of cervical leiomyomas include pressure effects on the bladder or urethra, degenerative phenomena, intermenstrual bleeding, pain (pelvic cramping), prolapse with infection and torsion.6 When we searched the literature we did not see any incidents of reported cervical inversion due to cervical leiomyoma. To our knowledge this is the first case of a totally inverted cervix due to a huge prolapsed cervical myoma simulating uterine inversion.
Uterine inversion is a rare complication of the puerperium and a non-puerperal inversion is an extremely rare occurrence. Usually, non-puerperal uterine inversion presents after 45 years and is mostly related to benign myomas and rarely associated with malignancies.7 The mechanism of tumor-related inversion is not clear but it is thought to be due to the distension and emptying of the uterine cavity, thin uterine walls, fundic localization of the tumor, the expulsive contractions of the uterus, and the weight of the tumor itself.8,9
Based on the literature search only one cervical inversion was found. Sivasuriya et al.10 report a case of inversion of a partly effaced and dilated cervix into the lower uterine segment at the time of cesarean section. This case was an example of puerperal cervical inversion, but our case differs in that our patient displayed non-puerperal cervical inversion due to prolapsed cervical leiomyoma growing during the perimenopausal period.
Uterine inversion is suspected when gynecologic examination detects a protruding mass in the vagina or vulva and the uterine fundus cannot be palpated by bimanual examination. The determining findings are an impalpable fundus and an invisible cervix.11 Clinical diagnosis of chronic non-puerperal uterine inversion is difficult, especially if vaginal examination cannot be performed. In our case, there was a protruding mass in the vulva, the cervix could not be visualized separately from the mass and the uterine fundus could not be palpated. These findings made us strongly consider the possibility of non-puerperal uterine inversion.
Ultrasonography might be a useful tool for diagnosis. Sonographic characteristics of complete uterine inversion are a ‘U’-shaped uterine cavity in the longitudinal plane.12 We could not perform transvaginal USG and unfortunately pelvic ultrasonography did not provide any additional information. Examination done under anesthesia revealed an inverted cervix covering the mass and a fundus by bimanual palpation and the intraoperative diagnosis was changed to a totally inverted cervix due to a huge prolapsed cervical leiomyoma simulating uterine inversion.
Prolapsed leiomyoma treatment is vaginal myomectomy or hysterectomy. Our patient desired hysterectomy without adnexectomy and vaginal hysterectomy was performed and the patient's postoperative course was uneventful.
We report a case of totally inverted cervix due to a huge cervical leiomyoma mimicking non-puerperal uterine inversion in a perimenopausal woman. Cervical fibroids can grow in perimenopausal period and in rare cases can cause total cervical inversion.
Conflict of interest
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Nilgun Ozturk Turhan, Serap Simavlı, and Ikbal Kaygusuz helped for study design, study collection, and writing. Burcu Kasap involved in writing.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-No Derivative Works License, which permits non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- 1.Buttram V.C., Jr., Reiter R.C. Uterine leiomyomata: etiology, symptomatology, and management. Fertil Steril. 1981;36:433–445. doi: 10.1016/s0015-0282(16)45789-4. [DOI] [PubMed] [Google Scholar]
- 2.Ben-Baruch G., Schiff E., Menashe Y., Menczer J. Immediate and late outcome of vaginal myomectomy for prolapsed pedunculated submucous myoma. Obstet Gynecol. 1988;72:858–861. doi: 10.1097/00006250-198812000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Golan A., Zachalka N., Lurie S., Sagiv R., Glezerman M. Vaginal removal of prolapsed pedunculated submucous myoma: a short, simple, and definitive procedure with minimal morbidity. Arch Gynecol Obstet. 2005;271:11–13. doi: 10.1007/s00404-003-0590-x. [DOI] [PubMed] [Google Scholar]
- 4.de Vries M., Perquin D.A. Non-puerperal uterine inversion due to submucous myoma in a young woman: a case report. J Med Case Rep. 2010;4:21. doi: 10.1186/1752-1947-4-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tiltman A.J. Leiomyomas of the uterine cervix: a study of frequency. Int J Gynecol Pathol. 1998;17:231–234. doi: 10.1097/00004347-199807000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Mayadeo N.M., Tank P.D. Non-puerperal incomplete lateral uterine inversion with submucous leiomyoma: a case report. J Obstet Gynaecol Res. 2003;29:243–245. doi: 10.1046/j.1341-8076.2003.00109.x. [DOI] [PubMed] [Google Scholar]
- 7.Lupovitch A., England E.R., Chen R. Non-puerperal uterine inversion in association with uterine sarcoma: case report in a 26-year-old and review of the literature. Gynecol Oncol. 2005;97:938–941. doi: 10.1016/j.ygyno.2005.02.024. [DOI] [PubMed] [Google Scholar]
- 8.Lascarides E., Cohen M. Surgical management of nonpuerperal inversion of the uterus. Obstet Gynecol. 1968;32:376–381. [PubMed] [Google Scholar]
- 9.Krenning R.A., Dorr P.J., de Groot W.H., de Goey W.B. Non-puerperal uterine inversion. Case report. Br J Obstet Gynaecol. 1982;89:247–249. doi: 10.1111/j.1471-0528.1982.tb03625.x. [DOI] [PubMed] [Google Scholar]
- 10.Sivasuriya M., Herath H.P. Inversion of cervix uteri at caesarean section. Br Med J. 1976;1:746–747. doi: 10.1136/bmj.1.6012.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kopal S., Seckin N.C., Turhan N.O. Acute uterine inversion due to a growing submucous myoma in an elderly woman: case report. Eur J Obstet Gynecol Reprod Biol. 2001;99:118–120. doi: 10.1016/s0301-2115(01)00346-3. [DOI] [PubMed] [Google Scholar]
- 12.Hu C.F., Lin H. Ultrasound diagnosis of complete uterine inversion in a nulliparous woman. Acta Obstet Gynecol Scand. 2012;91:379–381. doi: 10.1111/j.1600-0412.2011.01332.x. [DOI] [PubMed] [Google Scholar]


