Abstract
Tuberculosis (TB) surveillance in China is organized through a nationwide network of about 3200 hospitals and health facilities. In 2005, an electronic Tuberculosis Information Management System (TBIMS) started to be phased in to replace paper recording. The TBIMS collects key information on TB cases notified in TB care facilities, and exchanges real-time data with the Infectious Disease Reporting System, which covers the country’s 37 notifiable diseases. The system is accessible to authorized users at every level of the TB network through a password-protected website. By 2009 the TBIMS achieved nationwide coverage. Completeness of data on patient bacteriological end points improved remarkably over time. Data on about a million active TB cases, including drug-resistant TB, are included each year. The sheer scale of the data handling and the intricate functions that the China TBIMS performs makes it stand apart from the electronic information systems for TB adopted in other countries.
Keywords: surveillance, case-based, data quality
Introduction
In 2003, the spread of severe acute respiratory syndrome in China brought to light weaknesses in the country's public health surveillance system.1 The response of the Chinese government2 included the creation of an extensive web-based, real-time, Infectious Disease Reporting System (IDRS), which enables all health facilities across the country to report information on the 37 notifiable diseases within 24 h.3
Encouraged by the successful implementation of the IDRS, the Chinese Center for Disease Control and Prevention (China CDC) of the Ministry of Health—which is responsible for the National Tuberculosis (TB) Programme (NTP)—developed a separate web-based TB Information Management System (TBIMS) in 2005 to collect real-time TB data across the country. The TBIMS was designed to include more detail on TB cases reported and address challenges such as multidrug-resistant (MDR-TB) and HIV-associated TB. The users of TBIMS comprise all TB health facilities, including TB dispensaries and designated hospitals, at province, prefecture and county level.
This paper describes implementation of the TBIMS in China and reports on surveillance indicators since implementation. The limitations and opportunities for improvement are also discussed. Lessons learnt in China will be valuable for other countries that are planning to revise their TB surveillance systems.
Methods
Structure of TBIMS (V.2.1)
The TBIMS was constructed on an Oracle framework and supported by a dictionary of variables and a moderated user forum. Since 2011, TBIMS has been structured in three case-based databases:one for all pulmonary TB and extrapulmonary TB cases, one for patients with presumptive drug-resistant TB (DR-TB), and one for confirmed DR-TB cases. The three databases are linked with each other and exchange data in real time. For example, if one pulmonary TB case is treated unsuccessfully, this case is copied into the presumptive DR-TB patient database automatically. Likewise, if MDR-TB is diagnosed, then the case is copied into the DR-TB case database by the system.
Case definitions, data collection and reporting
Case definitions and the classification of treatment outcomes follow WHO recommendations.4–8 All TB-reporting facilities in China are required to report (i) confirmed TB cases seeking care via the TBIMS within 48 h and (ii) patients with presumptive TB to the IDRS, within 24 h. Should a patient first present for care at a general hospital, that hospital is required by law to report the individual using the IDRS and refer the case to TB dispensaries or TB hospitals. An interface between IDRS and TBIMS informs the TB units that a case within the same catchment area has been referred to that unit from the general hospital. The TB program supervisors can thus trace the patient to confirm whether they actually reached the TB health facility and, if TB was diagnosed, whether they were entered in the TBIMS.
The data on the TBIMS allows the disaggregation of cases by sex, age, location of residence and time of diagnosis, and can distinguish between migrant and settled populations. In addition to individual data on patients, the TBIMS regularly collects other information useful for program management. These include quarterly NTP activity reports from TB dispensaries at all levels, as well as annual reports on funding for TB control activities.
Data quality control
Firstly, a set of key variables are obligatory and logical check procedures are integrated into the TBIMS to ensure their completeness and accuracy. The system alerts the users with a popup window when there are quality control concerns about the entered data. For example, the date of onset should be earlier than the date of diagnosis.
Secondly, the TBIMS generates indicators for timeliness and completeness, such as the interval between the case seeking care and diagnosis, the interval between case diagnosis and case notification, and the interval between sputum examination and reporting result. Cases for which data quality concerns are outstanding are flagged.
Thirdly, users can only revise the data that they themselves have entered, although they can view data entered by subordinate users. The peripheral CDC staff have the right to validate data and check for duplicate records reported by different users. Every TB case for which treatment has been completed must be reconfirmed by the user, and if the user wants to modify the entered information, they must ask the upper-level user for permission.
Dissemination
The China CDC analyzes surveillance data from the TBIMS every quarter and publishes quarterly and annual analysis reports on national TB surveillance data. All these reports are shared with the Ministry of Health, with experts on TB control, and with all provincial TB dispensaries. At the same time, these TB dispensaries also produce quarterly and annual reports for use at the provincial and county level.
Interface between TBIMS and IDRS
IDRS is the main surveillance database for collection of infectious diseases data in China.9 This real-time internet-based surveillance system allows the identification of suspects and cases of major infectious diseases, monitors the trends of the epidemics, and allows early identification of outbreaks.
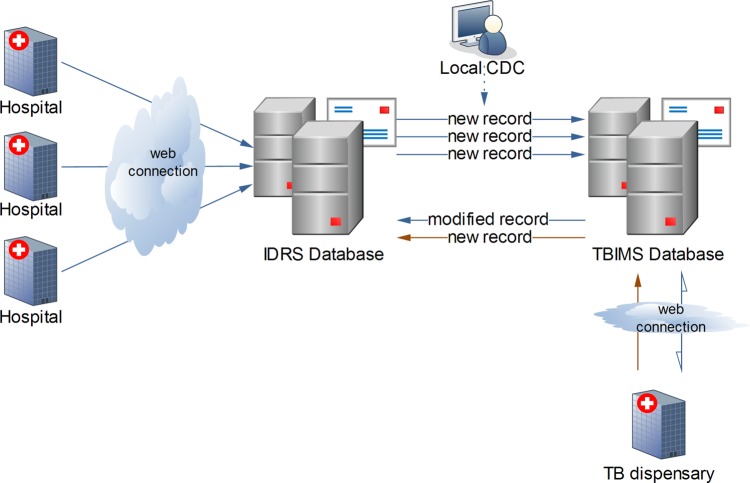
A special module in the TBIMS (the ‘Infectious Disease Report Card Management’) acts as the interface between IDRS and TBIMS (figure 1).
Figure 1.
Relationship between Tuberculosis Information Management System (TBIMS) and Infectious Disease Reporting System (IDRS). CDC, Center for Disease Control and Prevention.
Once data on individual cases reach the TBIMS, the user verifies the information on these patients and confirms or otherwise that the case will be managed by the TB dispensary. Once a patient’s profile is updated in the TBIMS, the data in IDRS is also simultaneously updated. Both the IDRS and TBIMS system administrators can identify repeated records by searching the database using a combination of the case name, identification number, birth date and occupation.
Human resource requirements of the TBIMS
Before the TBIMS formally came into being, China CDC held three training courses in 2005 to train about 400 staff from TB health facilities at province and prefecture level. These staff then trained those at county level through a cascade system. Since 2005, China CDC has held annual surveillance workshops to discuss how to solve existing issues about the TBIMS and how to improve the use of the system. At present, there are about 20 000 users in the TB health facilities across the whole country using the TBIMS. Most of them have a university qualification in a public health discipline.
Box 1. Main lessons and messages.
China successfully implemented an extensive, web-based TBIMS covering about 3200 reporting facilities across the country in 2005. The TBIMS and the paper-based surveillance system ran simultaneously for about 4 years, after which the paper-based system was discontinued (in 2009).
The TBIMS fits with the larger framework of infectious disease surveillance and provides the China CDC with the information necessary to assess the main indicators of TB case detection and management. Since its implementation, the system has improved the coherence of the data entered and their completeness. Data for about one million cases of active TB are managed by the system each year.
The main activities that were crucial to the successful operationalization of the TBIMS were the creation of the software, the provision and servicing of the computers, and the training and motivation of staff for its continued use and development.
The three databases making up the TBIMS are useful in tracking the trajectory of TB cases with presumptive or confirmed drug-resistant TB. Drug resistance is one of the major challenges in TB control in China as in many other places in the world. The system also has the potential to follow individual TB patients who migrate within China during their care.
The China TBIMS is unique in having to handle a huge burden of cases, several administrative levels, and diverse functions. The lessons learnt in its implementation could be useful for other large countries intent on modernizing their information management functions for infectious disease control.
China CDC, Chinese Center for Disease Control and Prevention; TBIMS, Tuberculosis Information Management System.
Results
The main lessons learnt and achievements are summarized in box 1.
Table 1.
Main lessons and messages
| 1 | |
| 2 | |
| 3 | |
| 4 | |
| 5 |
China CDC, Chinese Center for Disease Control and Prevention; TBIMS, Tuberculosis Information Management System.
Coverage and completeness
Since the first version of TBIMS was launched in 2005, the system has covered all 3200 TB-reporting units in China, and approximately 2700 TB cases/suspects are notified and entered into TBIMS every day.
Since 2005, the numbers of active TB cases entered into the TBIMS have averaged about one million annually. The paper-based surveillance system ran in parallel with the TBIMS from 2005 to 2008, and the difference between TB cases captured by the paper system and TBMIS over total TB cases notified in the paper system decreased from 0.27% to 0.03% over the same period of time. The paper-based system was therefore discontinued in 2009, as TBIMS was able to capture almost all TB cases notified in TB dispensaries. On the basis of the WHO estimates for China in 2011, notifications for new cases and relapses on the TBIMS represent about 90% of incident TB cases.10
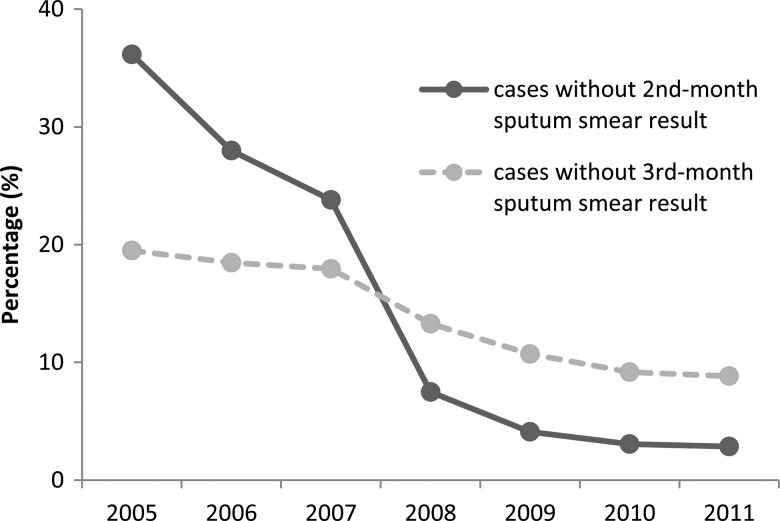
Validation procedures at data entry have reduced errors. Quick access to results helps practitioners to identify instances where results are missing or sputum not tested. All TB patients who have been treated over 2 months are required to have sputum smear results at the end of the 2nd month, and patients whose sputum smear results did not become negative at the end of 2nd month should have sputum smear results at the end of the 3rd month. The percentage of cases without a 2nd-month result entered decreased sharply between 2005 and 2011, reaching 3% in 2011 (figure 2). The percentage of cases without a 3rd-month result has also fallen from 20% to 9% since 2005.
Figure 2.
Percentage of tuberculosis cases without 2/3-month sputum smear results, 2005–2011.
Timeliness
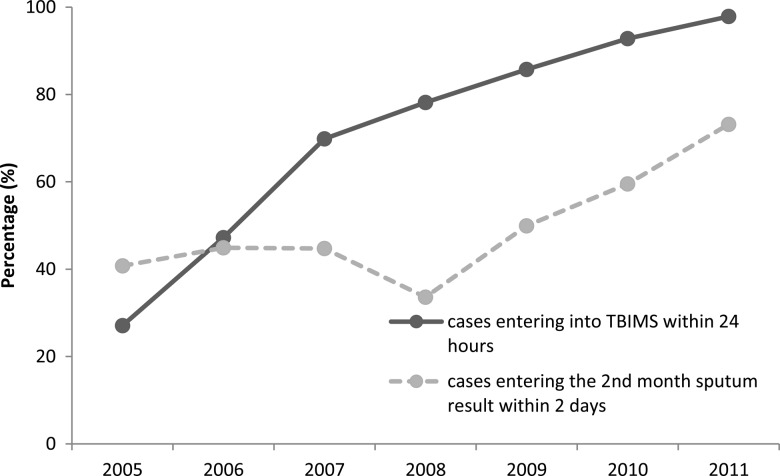
The time interval until data are captured on the TBIMS has been assessed using two indicators (figure 3). The percentage of cases with all forms of TB entered into the TBIMS within 24 h from detection has increased steadily from 2005 to 2011, reaching almost 100% in 2011. In addition, the percentage of cases with the 2nd-month sputum result entered within 2 days of issue, among all cases with a 2nd-month sputum result, is also increasing, although by 2011 about 25% of cases had a delay greater than 2 days.
Figure 3.
Timeliness of tuberculosis cases entered into the Tuberculosis Information Management System (TBIMS), 2005–2011.
Internal consistency
Pediatric TB cases (<12 years in China) are registered as ‘child’ under the field ‘occupation’ on the TBIMS. By cross-checking this field against the age field, we were able to therefore test for internal consistency. A steep decline was found in the percentage of TB cases with discordant data between 2005 and 2008, since when it has stabilized to below 5%.
Discussion
In a country with the geographical diversity, size and population of China, the development of a unified TB surveillance network with real-time data collection at different administrative levels has been a major achievement. The TBIMS has been cited by the WHO in a recent handbook aimed at helping countries to plan and develop electronic recording and reporting systems.11 There remain, however, several limitations to the TBIMS as well as opportunities for improvement.
First, the TBIMS can only interoperate with IDRS. Users in designated TB hospitals that do not belong to the CDC need to enter information about TB cases twice, once in the TBIMS and once in the Hospital Information System (HIS). This is very labor-intensive and prone to error. As part of the health sector reform, diagnosis and treatment of TB cases will be increasingly carried out by designated hospitals, and TB dispensaries—which nowadays account for 80% of cases on the TBIMS—will only retain public health functions such as patient follow-up, surveillance and training.12 If in the future the TBIMS provides an interface to exchange data with the HIS, then the designated hospital will only need to enter data once into the HIS, and this will then be exchanged with the TBIMS and in turn with the IDRS.
Second, at present in China, only pulmonary TB is a notifiable disease; extrapulmonary forms, even MDR-TB, are not notifiable. This means that, unless a patient with presumptive or confirmed MDR-TB visits a TB dispensary and or a designated TB hospital, that patient will not be captured by the surveillance system and in turn will not have access to diagnostic and treatment services. For this reason, it is important for the TBIMS to have the added possibility to link with the HIS and other health information systems—including the vital registration structures—to promote the development of a more comprehensive TB surveillance system.13
Third, some 230 million migrants face difficulty in accessing healthcare given that the entitlements are based on place of residence.14 This represents a major challenge to the country’s surveillance system. Currently, the primary user entering data into the TBIMS is located at the TB dispensary at county level, which diagnoses, treats and manages all TB cases and serves as the basic TB management unit. This information can only be seen at higher levels in the system, and no ‘horizontal’ access to information within the same prefecture is currently possible. With such a mobile population in need of healthcare, the surveillance system needs to adapt in order to adequately capture patient transfer.11
In conclusion, the TBIMS is a well-structured TB surveillance system that has served the NTP well. Its implementation has not only benefited TB care, by improving access to useful information, but has also rendered disease surveillance more comprehensive. However, the system will require continual development in the future—most notably greater coverage of data on MDR-TB and the migrant population—if it is to provide essential information to allow control of the TB epidemic in China. This will be an important next step on the pathway to achieving universal access to healthcare, which is the main motivation behind the ongoing health sector reforms in China.
Footnotes
Contributors: LW is responsible for the ideation of the article, and FH made the first draft of this paper and identified the main indicators. XD, SC and WC analyzed the data and are responsible for the accuracy of the references included. FS contributed to the design, writing and review of the paper. DF contributed to the writing of the article, the addition of some references, and replies to the reviewers. DF and FS are staff members of the WHO. The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the decisions or policies of the WHO.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ru X, Lu X, Li P. Blue book of China's Society: Society of China Analysis and Forecast (2004). Social Science Literature Publishing House, 2004. . [Google Scholar]
- 2.Wang L, Liu J, Chin DP. Progress in tuberculosis control and the evolving public-health system in China. Lancet 2007;369:691–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang L, Liu X, Huang F, et al. Engaging hospitals to meet tuberculosis control targets in China: using the Internet as a tool to put policy into practice. Bull World Health Organ 2010;88:937–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO. Implementing the stop TB strategy: a handbook for national tuberculosis control programmes. Geneva: World Health Organization, 2008. (WHO/HTM/TB/2008.401). [PubMed] [Google Scholar]
- 5.WHO. The global plan to stop TB 2011–2015: transforming the fight towards elimination of tuberculosis. Geneva: World Health Organization, 2010 [Google Scholar]
- 6.WHO. Guidelines for the programmatic management of drug-resistant tuberculosis. Geneva: World Health Organization, 2008. WHO/HTM/TB/2008.402 [PubMed] [Google Scholar]
- 7.WHO. Multidrug-resistant tuberculosis (MDR-TB) indicators. A minimum set of indicators for the programmatic management of MDR-TB in national tuberculosis control programmes. Geneva: World Health Organization, 2010. (WHO/HTM/TB/2010.11). [Google Scholar]
- 8.WHO. Definitions and reporting framework for tuberculosis-2013 revision. Geneva: World Health Organization, 2013. (WHO/HTM/TB/2013.2) [Google Scholar]
- 9.Jin S. Development of public health informatization in China. China Med Device Inform 2010;16:9–18 [Google Scholar]
- 10.WHO. Global tuberculosis report 2012. Geneva: World Health Organization, 2012. (WHO/HTM/TB/2012.6). [Google Scholar]
- 11.WHO. Electronic recording and reporting for tuberculosis care and control. Geneva: World Health Organization, 2012. (WHO/HTM/TB/2011.22) [Google Scholar]
- 12.The Central People's Government of the People's Republic of China. The notification of printing out ‘National Tuberculosis Programme (2011–2015)’. http://www.gov.cn/zwgk/2011-12/06/content_2012869.htm (accessed 22 Dec 2012).
- 13.Chan M, Kazatchkine M, Lob-Levyt J, et al. Meeting the demand for results and accountability: a call for action on health data from eight global health agencies. PLoS Med 2010;7:e1000223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Bureau of Statistics of China. Statistical Communique of the People's Republic of China on the 2011 National Economic and Social Development Beijing: National Bureau of Statistics of China, 2012 [Google Scholar]