Abstract
INTRODUCTION
Amyloid goiter (AG) is characterized by enlargement of the thyroid gland as a result of extensive amyloid deposition in a bilateral and diffuse manner.
PRESENTATION OF CASE
A 58-year-old male patient was diagnosed of Crohn's Disease (CD). He was admitted to our clinic with complaint of respiratory distress and rapid growth swelling in the neck. Ultrasound examination revealed huge multinodular goiter on both sides of thyroid gland. We performed bilateral total thyroidectomy. Pathological evaluation revealed AG.
DISCUSSION
Amyloid leads to degeneration in tissues, thereby disrupts the function of the relevant organs. It is important to distinguish AG from other reasons of goiter, particularly thyroid medullary cancer that can cause amyloid deposition in thyroid gland. Secondary amyloidosis frequently involves thyroid gland at microscopic level, but rarely causes goiter. An analysis of current literature revealed that only few cases of AG occurred secondary to CD. Herein we presented a case of AG who has rapidly growing goiter that associated with CD.
CONCLUSION
AG must be kept in mind in case of rapidly growing goiter, especially in patients with chronic inflammatory bowel diseases.
Keywords: Goiter, Amyloidosis, Crohn's disease, Amyloid goiter
1. Introduction
Amyloid is an amorphous and proteinaceous material that accumulates in tissue and causes amyloidosis.1 It may effect a single organ or cause systemic involvement.2,3 Amyloidosis is classified as primary or secondary. The latter accompany to neoplasms or chronic inflammatory diseases. “Serum Amyloid A” is an acute phase reactant that accumulates in various organs of patients with secondary amiloidosis.1,4,5 In 1948, Olson et al. reported the first case of secondary amyloidosis caused by Crohn's disease (CD).6 Amyloid accumulates in thyroid gland in case of amyloidosis or medullary thyroid cancer. Amyloid depots exist in thyroid gland at microscopic level up to 50–80% in patients with systemic amyloidosis.7 These patients are mostly euthyroid and usually present with pressure symptoms due to rapidly growing thyroid gland.8–10 Herein, we reported a very rare cause of AG, which developed during the course of CD.
2. Presentation of case
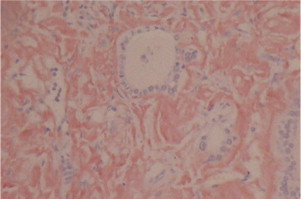
A 58-year-old male patient with intermittent diarrhea for about 20 years, endoscopic biopsy performed to confirm the CD. Symptoms were treated with budesonide and 5-aminosalicylic acid orally. After six months, therapy was discontinued because of drug intolerance. Afterwards, patient was admitted to hospital with rapidly growing swelling of neck, respiratory distress, dyspnea and fatigue. Physical examination revealed rather large thyroid gland as multi-nodular pattern on both lobes (Fig. 1). Thyroid function tests were all within the normal in range. Ultrasonography (USG) examination revealed that the size of the left lobe was 137 mm × 103 mm × 35 mm and right was 119 mm × 76 mm × 43 mm. Thyroid tissue was detected as diffuse heterogeneous and micro-nodular pattern. Multiple nodules were also detected bilaterally with the largest of them is measured 19 mm in size. Cervical and thoracic computed tomography examination showed an excessive growth of the thyroid gland and its lower boundaries extended to the mediastinum. Thyroid scintigraphy showed a heterogeneous distribution of radioactivity in both lobes. Fine-needle aspiration biopsy (FNAB) revealed a benign thyroid tissue. We performed total thyroidectomy. Thyroid tissue was extremely soft and fragile, macroscopically. And right lobe of the thyroid gland was 12 cm × 7.5 cm × 4.5 cm and left lobe was 14 cm × 10.5 cm × 3.5 cm in size (Fig. 2). There were nodular and diffuse areas in the cross-sectional samples, and the microscopic evaluation revealed extracellular amorphous proteinaceous material widely deposited in the stroma with Hematoxylin and Eosin (H&E) staining (Fig. 3). Crystal violet and Congo red also showed a positive staining (Figs. 4 and 5). There were no malignancies or inflammatory diseases detected, unless CD. Therefore we consider the patient as an amyloid goiter due to CD. Patient discharged second day after operation, without any complications. Amyloid deposition was not observed in biopsy specimen taken during colonoscopy. There were no recurrence or other organ involvement associated with amyloidosis after 24-month follow-up.
Fig. 1.

The appearance of multinodular goiter in the neck.
Fig. 2.

Macroscopic aspect of thyroidectomy specimen.
Fig. 3.

Extracellular amorphous material is deposited widely in the stroma (H&E).
Fig. 4.

Crystal violet showed a positive staining for amyloid.
Fig. 5.
Congo red showed a positive staining for amyloid.
3. Discussion
Amyloid is a fibrillar protein that accumulates in various organs and disrupts the function of these organs.11 It is determined microscopically as an intercellular and semi-transparent material. Amyloid has many subtypes that two of them are the major. Despite the similarity in their staining patterns, amyloid is not a single chemical entity. Therefore, it will be more appropriate to describe amyloidosis as a heterogeneous group of diseases characterized by fibrillar protein deposits that have similar staining characteristic.12,13
Amyloidosis is classified as primary and secondary. In primary amyloidosis, amount of monoclonal plasma cells increase in bone marrow, similarly immunoglobulin light chains (AL type) increase in the affected tissue. Secondary amyloidosis accompanies malignancies or chronic inflammatory diseases such as tuberculosis, rheumatoid arthritis, ankylosing spondylitis, cystic fibrosis, bronchiectasis and inflammatory bowl disease.6 Approximately, 75% of patients with secondary amyloidosis that accompanying to CD are male, just as our case.14–16 It was reported in autopsy studies that amyloid deposition is found in the thyroid gland of 50% of primary amyloidosis and 80% of secondary amyloidosis.7,8,17 AG is observed in about 0.04% of cases with primary systemic amyloidosis, and these patients have poorer prognosis.9,18 Symptoms depend on the involved organ.
Amyloid deposition in thyroid gland was first published by Rokitansky in 1855. Beckmann reported a clinically visible thyroid enlargement due to amyloidosis in 1858.19,20 The association of CD with amyloidosis is a rare entity that first time reported by Moschkowitz in 1936.14,15,21 Afterwards, Olson et al. reported a case of secondary amyloidosis related to CD, in 1948.6 Since then, some similar cases and reviews reported by various authors, between 1982 and 2009.22,23 Greenstein et al. investigated and reported 3050 patients with inflammatory bowel disease in 1992. According to this report, 22 (1.29%) of 1708 patients with CD were complicated by secondary amyloidosis.24,25 Nevertheless AG is very rare in this group of patients. So far, only few AG cases secondary to CD were reported in the literature.6,26–29
Earlier articles suggest that thyroid gland tends to enlarge rapidly within few weeks or months, in patients with AG.11 Rapidly growing thyroid gland due to amyloid involvement may cause compressive symptoms such as dyspnea, and dysphagia, as in our case. In case of rapidly growing thyroid gland AG should also be come to mind such as anaplastic cancer and lymphoma. The structure of thyroid gland is usually in form of diffuse goiter in patients with AG, but sometimes cystic or nodule-like solid lesions may coexisted.11,22 In our patient, it was remarkable that thyroid tissue was excessively soft and fragile. Sometimes AG may be clinically asymptomatic and rarely present with thyroiditis-like condition.10,30 Thyroid function tests are determined generally in normal range, even in patients with wide thyroid involvement. Hypothyroidism or hyperthyroidism are seen less frequently.10,22 In our case, free T3, free T4 and TSH levels were all within the normal in range. Kimura et al. reported that serum thyroglobulin level could be higher than normal range in patients with AG, due to destruction of thyroid follicles by amyloid deposition.7
Meyers and Janowits reported that 29.4% of patients with CD had renal amyloidosis at autopsy, but only 1% was diagnosed during lifetime.31 Most of the cases with secondary amyloidosis are discovered by proteinuria or nephrotic syndrome due to renal amyloidosis.32 Renal involvement is frequently observed in amyloidosis related to CD, and diagnosed with pathological verification. In our patient, blood urea nitrogen and creatinine levels were all within the normal in range.
Amyloid disrupts normal histological pattern of thyroid gland by infiltrating the parenchyma. Fine needle aspiration cytology (FNAC) is a safe and effective procedure for the diagnosis of thyroid amyloidosis. FNAC allows exclusion of thyroid malignancies such as medullary thyroid carcinoma. However it may be inconclusive due to insufficient cellular material. Therefore, definitive diagnosis of AG generally rests on the histologic evaluation of surgical specimens, as in our case.33 Microscopic examination generally shows extracellular amorphous, eosinophilic, and proteinaceous material in patients with amyloidosis. Focal lymphocytic thyroiditis and foreign body reaction commonly coexist with the amyloid infiltration.34 Amyloid has positive stainining with Congo red, Thioflavin T and Crystal violet. Congo red staining has a diagnostic sensitivity of 70–90% with FNAC from a symptom-giving organ.34–36 Amyloid material appears as cherry red and it also shows apple-green birefringence when observed with a polarizing microscope.37
4. Conclusion
Existence of amyloid deposition in thyroid gland without systemic involvement is very rare clinical condition that can observe in course of CD. Analysis of current literature is revealed that only few cases of AG are reported related to CD. As a result, in case of rapidly growing neck mass, AG should be taken into consideration for the differential diagnosis such as anaplastic thyroid carcinoma and lymphoma. Nevertheless, cellular morphology must be examined carefully for differential diagnosis of medullary carcinoma in case of existence of amyloid deposition in thyroid gland. Screening tests for chronic inflammatory diseases should be made in patients with AG. It may be suitable to examine the thyroid gland and analyze the serum thyroglobulin level, in order to detect secondary amyloidosis at an early stage in patients with CD.
Conflict of interest
Ibrahim Ali Ozemir and other co-authors have no conflict of interest.
Funding
There is no source of funding used for research.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. Göztepe Education and research hospital ethics committee approved this research.
Author contributions
Ibrahim Ali Ozemir, Cagrı Bilgic and Rafet Yigitbasi studied concept. Ibrahim Ali Ozemir, Sinan Aslan, Ebru Zemheri, Haydar Yalman and Baris Bayraktar are involved in data collection. Ibrahim Ali Ozemir, Cagrı Bilgic, Sinan Aslan, Baris Bayraktar analysed the data. Ibrahim Ali Ozemir and Rafet Yigitbasi wrote the paper.
Key learning point.
-
•
In case of rapidly growing goiter, AG must be kept in mind, such as anaplastic cancer and lymphoma of thyroid gland.
References
- 1.Kisilevcky R. Amyloid and amyloidosis: differences, common themes, and practical considerations. Mod Pathol. 1991;4:514–518. [PubMed] [Google Scholar]
- 2.Gertz M. Immunoglobin light chain amyloidosis: 2011 update on diagnosis, risk-stratification, and management. Am J Hematol. 2011;86:181–186. doi: 10.1002/ajh.21934. [DOI] [PubMed] [Google Scholar]
- 3.Pettersson T., Konttinen Y.T. Amyloidosis – recent developments. Semin Arthritis Rheum. 2010;39:356–368. doi: 10.1016/j.semarthrit.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 4.Sinha R.N., Plehn J.F., Kinlaw W.B. Amyloid goiter due to primary systemic amyloidosis: adiagnostic challenge. Thyroid. 1998;8:1051–1054. doi: 10.1089/thy.1998.8.1051. [DOI] [PubMed] [Google Scholar]
- 5.Kapadia H.C., Desai R.I., Desai I.M., Parikh N.R. Amyloid goiter: a case report. Indian J Pathol Microbiol. 2001;44:147–148. [PubMed] [Google Scholar]
- 6.Habu S., Watanobe H., Kımura K., Suda T. A case of amyloid goiter secondary to Crohn's disease. Endocr J. 1999;46:179–182. doi: 10.1507/endocrj.46.179. [DOI] [PubMed] [Google Scholar]
- 7.Kimura H., Yamashita S., Ashizawa K., Yokoyama N., Nagataki S. Thyroid dysfunction in patients with amyloid goiter. Clin Endocrinol (Oxf) 1997;46:769–774. doi: 10.1046/j.1365-2265.1997.1841000.x. [DOI] [PubMed] [Google Scholar]
- 8.Hamed G., Heffes C.S., Shmookler B.M., Wenig B.M. Amyloid goiter: a clinicopathological study of 14 cases and review of the literature. Am J Clin Pathol. 1995;104:306–312. doi: 10.1093/ajcp/104.3.306. [DOI] [PubMed] [Google Scholar]
- 9.Siddiqui M.A., Gertz M., Dean D. Amyloid goiter as a manifestation of primary systemic amyloidosis. Thyroid. 2007;17:77–80. doi: 10.1089/thy.2006.0045. [DOI] [PubMed] [Google Scholar]
- 10.Villamil C.F., Massimi G., D’Avella J., Cole S.R. Amyloid goiter with parathyroid involvement. Arch Pathol Lab Med. 2000;124:281–283. doi: 10.5858/2000-124-0281-AGWPI. [DOI] [PubMed] [Google Scholar]
- 11.Goldsmith J.D., Lai M.L., Daniele G.M., Tomaszewski J.E., Li-Volsi V.A. Amyloid goiter: report of two cases and review of the literature. Endocr Pract. 2000;6:318–323. doi: 10.4158/EP.6.4.318. [DOI] [PubMed] [Google Scholar]
- 12.Merlini G., Seldin D.C., Gertz M.A. Amyloidosis: pathogenesis and new therapeutic options. J Clin Oncol. 2011;29:1924–1933. doi: 10.1200/JCO.2010.32.2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hemminki K., Li X., Forsti A., Sundquist J., Sunquist K. Incidence and survival in non-hereditary amyloidosis in Sweden. BMC Publ Health. 2012;12:974. doi: 10.1186/1471-2458-12-974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wester A.L., Vant M.H., Fausa O. Secondary amyloidosis in inflammatory bowel disease: a study of 18 patients admitted to Rikshospitalet University Hospital, Oslo, from 1962 to 1998. Inflamm Bowel Dis. 2001;7:295–300. doi: 10.1097/00054725-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Greenstein A.J., Sachar D.B., Panday A.K., Dikman S.H., Meyer S., Heimann T. Amyloidosis and inflammatory bowel disease. A 50-year experience with 25 patients. Medicine (Baltimore) 1992;71:261–270. doi: 10.1097/00005792-199209000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Guardiola-Arévalo A., Alcántara-Torres M., Valle-Muñoz J., Lorente-Poyatos R.H., Romeo-Gutierrez M., Rodriguez-Merio R. Amyloidosis and Crohn's disease. Rev Esp Enferm Dig. 2011;103:268–274. [PubMed] [Google Scholar]
- 17.Uzum G., Kaya F.O., Uzum A.K., Kucukyilmaz M., Gunes M.E., Duzkoylu Y. Amyloid goiter associated with amyloidosis secondary to rheumatoid arthritis. Case Rep Med. 2013:792413. doi: 10.1155/2013/792413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gertz M.A., Kyle R.A. Secondary systemic amyloidosis: response and survival in 64 patients. Medicine (Baltimore) 1991;70:246–256. [PubMed] [Google Scholar]
- 19.Nessim S., Tamilia M. Papillary thyroid carcinoma associated with amyloid goiter. Thyroid. 2005;15:382–385. doi: 10.1089/thy.2005.15.382. [DOI] [PubMed] [Google Scholar]
- 20.Beckman O. Ein Fall vor amyloider degeneration. Virchows Arch Pathol Anat. 1858;13:94–98. [Google Scholar]
- 21.Moschkowitz E. The clinical aspects of amyloidosis. Ann Intern Med. 1936;10:73–89. [Google Scholar]
- 22.Amado A., Ondiviela R., Palacios S., Casanova D., Manzanos J. Fast growing goiter as the first clinical manifestation of systemic amyloidosis. Postgrad Med J. 1982;58:171–172. doi: 10.1136/pgmj.58.677.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abdou A.G., Kandil M.A. A case of amyloid goiter associated with intrathyroid parathyroid and lymphoepithelial cyst. Endocr Pathol. 2009;20:243–248. doi: 10.1007/s12022-009-9089-8. [DOI] [PubMed] [Google Scholar]
- 24.Greenstein A.J., Janowitz H.D., Sachar D.B. The extra-intestinal complications of Crohn's disease and ulcerative colitis: a study of 700 patients. Medicine (Baltimore) 1976;55:401–412. doi: 10.1097/00005792-197609000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Fausa O., Nygaard K., Elgjo K. Amyloidosis and Crohn's disease. Scand J Gastroenterol. 1977;12:657–662. doi: 10.3109/00365527709181699. [DOI] [PubMed] [Google Scholar]
- 26.D’Antonio A., Franco R., Sparano L., Terzi G., Pettinato G. Amyloid goiter: the first evidence in secondary amyloidosis. Report of five cases and review of literature. Adv Clin Path. 2000;4:99–106. [PubMed] [Google Scholar]
- 27.Gallardo G.L., Moya M.P., Rey M.D., Arroyo M.J., Dávila F.M. Amyloid goiter secondary to Crohn's disease. Endocrinol Nutr. 2009;56:384–386. doi: 10.1016/S1575-0922(09)72459-3. [DOI] [PubMed] [Google Scholar]
- 28.Kazdaghli Lagha E., M'sakni I., Bougrine F., Laabidi B., Ben Ghachem D. Amyloid goiter: first manifestation of systemic amyloidosis. Eur Ann Otorhinolaryngol Head Neck Dis. 2010;127:108–110. doi: 10.1016/j.anorl.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 29.Febrero B., Ríos A., Rodríguez J.M., Ferri B., Polo L. Giant amyloid goiter in Crohn's disease. Endocr Pathol. 2012;23:260–263. doi: 10.1007/s12022-012-9220-0. [DOI] [PubMed] [Google Scholar]
- 30.Tokyol C., Demir S., Yilmaz S., Topak N., Paþali T. Amyloid goiter with hyperthyroidism. Endocr Pathol. 2004;15:89–90. doi: 10.1385/ep:15:1:89. [DOI] [PubMed] [Google Scholar]
- 31.Meyers S., Janowits H.D. Complications of Crohn's disease. In: Berk J.E., Haubrich W.S., Kalser M.H., Roth J.L.A., Schaffner F., editors. Bockus gastroenterology. 4th ed. WB Saunders; Philadelphia, London: 1985. pp. 2294–2305. [Google Scholar]
- 32.Schmidt H., Riemann J.F. Amyloidosis in Crohn's disease. Dtsch Med Wochenschr. 1983;108:795–797. doi: 10.1055/s-2008-1069644. [DOI] [PubMed] [Google Scholar]
- 33.Khullar A., Sharma A., Goel A., Bagchi N., Soni V., Baijal M. Amyloid goiter: a rare case report. Indian J Surg. 2006;68:104–105. [Google Scholar]
- 34.Nijhawan V.S., Marwaha R.K., Sahoo M., Ravishankar L. Fine needle aspiration cytology of amyloid goiter: a report of four cases. Acta Cytol. 1997;41:830–834. doi: 10.1159/000332711. [DOI] [PubMed] [Google Scholar]
- 35.Ozdemir B.H., Uyar P., Ozdemir F.N. Diagnosing amyloid goiter with thyroid aspiration biopsy. Cytopathology. 2006;17:262–266. doi: 10.1111/j.1365-2303.2006.00399.x. [DOI] [PubMed] [Google Scholar]
- 36.Himmetoglu C., Yamak S., Tezel G.G. Diffuse fatty infiltration in amyloid goiter. Pathol Int. 2007;57:449–453. doi: 10.1111/j.1440-1827.2007.02122.x. [DOI] [PubMed] [Google Scholar]
- 37.Di Crescenzo V., Garzi A., Petruzziello F., Cinelli M., Catalano L. Nodular goiter with amyloid deposition in an elderly patient: fine-needle cytology diagnosis and review of the literature. BMC Surg. 2013;13:43. doi: 10.1186/1471-2482-13-S2-S43. [DOI] [PMC free article] [PubMed] [Google Scholar]


