Abstract
INTRODUCTION
Papillary thyroid cancer (PTC) is the most common thyroid malignancy and usually spreads via lymphatic system. PTC can sometimes show microscopic vascular invasion, but rarely causes tumour thrombus in the internal jugular vein (IJV) or other great veins of the neck.
PRESENTATION OF CASE
We report a case of a 62-year-old female presented with symptomatic central neck mass. Clinical examination revealed a hard solitary right-sided thyroid nodule with ipsilateral cervical lymphadenopathy. Ultrasonography (US) confirmed the clinical diagnosis and visualised a dilated ipsilateral IJV. Fine-needle aspiration cytology revealed PTC cells so total thyroidectomy with right neck dissection was done. A tumour thrombus was discovered in the distended right IJV and was cleared successfully. The patient recovered well after the operation with no local or distant metastasis detected.
DISCUSSION
Tumour vascular spread is observed in tumours with angio-invasive features including follicular carcinoma of the thyroid gland where great cervical veins can be affected. PTC commonly spreads to the lymph nodes and vascular spread via direct intravascular extension is extremely rare. Neck US has an important role in the diagnosis, and operators should attempt to detect signs of tumour thrombi in all patients with thyroid masses. Aggressive surgical treatment with vascular repair is recommended whenever possible to minimise the risk of potentially fatal complications of the intraluminal masses.
CONCLUSION
Intravascular tumour extension of PTC is rare but with serious consequences. Diagnosis with neck US is possible but some cases are only discovered intraoperatively. Thrombectomy with vascular repair or reconstruction is usually possible.
Keywords: Thyroid, Papillary thyroid carcinoma, Internal jugular vein thrombus, Tumour thrombus, Thyroid malignancy
1. Introduction
Papillary carcinoma of the thyroid (PTC) is common and accounts for approximately 80% of all thyroid malignancies.1 Locally advanced disease is usually associated with dysphagia, dyspnoea, and dysphonia, but lymph node metastasis as the presenting complaint is also common. Direct spread to the regional great veins in PTC and other differentiated thyroid cancers is rare but has a high mortality rate.2 PTC can sometimes show microscopic vascular invasion, and rarely cause tumour thrombus in the IJV or other great veins of the neck.2,3 We present a case of a 62-year-old woman with IJV spread of PTC that subsequently developed into an anaplastic thyroid cancer.
2. Case presentation
A 62-year-old female patient was recently referred to our hospital with a 3-months history of an episodic, but progressively worsening stridor, exertional dyspnoea and dry cough. Clinical examination of the right side of the neck revealed a hard 3 cm × 5 cm solitary thyroid nodule with ipsilateral level III and IV cervical lymphadenopathy. No neck tenderness or dilated veins could be identified. Serum thyroid function tests were within normal limits (TSH 1.8 Miu/L, Free T3 4 pmol/L, Free T4 16.3 pmol/L), but thyroglobulin level was >115 IU/ml. Subsequent neck ultrasonography (US) confirmed a solitary thyroid nodule showing cystic changes and calcification with cervical lymphadenopathy. The ipsilateral IJV was also noted to be distended but the ultrasonographer was not able to comment on any intravascular masses. Fine-needle aspiration cytology of the thyroid nodule revealed a papillary thyroid carcinoma, and papillary thyroid cells in the enlarged lymph nodes. A fibre-optic laryngeal examination revealed a narrow glottis area with a postnasal drip, the vocal cords appeared normal, but with diminished mobility. Computed tomography (CT) imaging showed a large hypo dense nodule with areas of cystic degeneration and calcification occupying the right lobe of the thyroid gland and invading the left lobe (Fig. 1a) and a large, well defined, heterogeneously enhancing mass in the right anterior jugulo-digastric region representing a pathological lymph node partially compressing the right IJV (Fig. 1b). Surgery was considered for treatment and a total thyroidectomy with right neck dissection revealed a locally advanced thyroid neoplasm with superficial invasion of the trachea. Intraoperative palpation of the distended right IJV showed a 2 cm × 3 cm hard intraluminal mass. Longitudinal venotomy revealed a tumour thrombus with no endothelial adhesion and was easily removed (Fig. 2). The vein was repaired using 6-0 prolene and the tracheal invasion was shaved successfully.
Fig. 1.
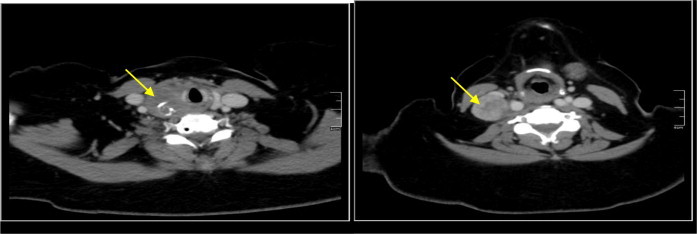
(a and b) Computed tomography (CT) images of the neck. The yellow arrow in the left image (a) points towards a large nodule with areas of cystic degeneration and calcification occupying the right lobe of the thyroid gland. The yellow arrow in the right image (b) denotes a well-defined mass at the right anterior jugular digastric region with multiple areas of necrosis. (For interpretation of the references to color in figure legend, the reader is referred to the web version of the article.)
Fig. 2.
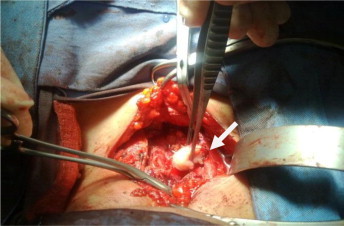
Intra operative photograph showing a tumour thrombus easily removed from the right IJV (arrow) via a longitudinal venetomy incision.
Histopathology and immunohistochemistry analysis of the right thyroid lobe mass and the tissue shavings of the trachea revealed stage (PT4bN1Mx) undifferentiated anaplastic carcinoma (Fig. 3a and b respectively). Histology of the right IJV intraluminal mass revealed a papillary thyroid carcinoma (Fig. 3c).
Fig. 3.
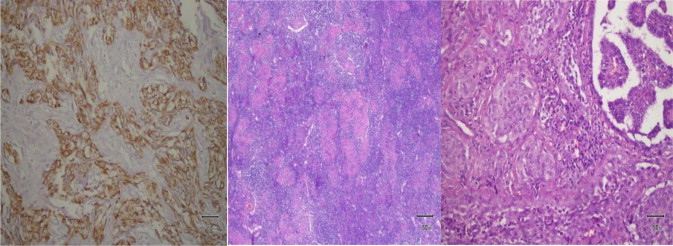
(a–c) Photomicrographs of the histological analysis of surgical resections. (a (left)) shows the right thyroid lobe with anaplastic carcinoma. Immunohistochemistry analysis expressed positive cytokeratin 7, positive thyroid transcription factor-1, positive vimentin, negative thyroglobulin and cytokeratin 20. (b (middle)) also shows anaplastic carcinoma pattern taken from shaved surface of the trachea. (c (right)) shows differentiated thyroid cancer of papillary type in the sample taken from the right IJV tumour thrombus.
The surgery was followed by ablative radioiodine plus external beam radiotherapy to the neck. The patient is alive and functional 16 months later with no signs of local recurrence or distant metastasis.
3. Discussion
In 1879, Kaufmann and graham reported the first two cases of vascular tumour thrombosis associated with thyroid cancer.2 Since then, only a few cases of thyroid carcinoma with a tumour thrombus in the jugular vein have been reported.2,4 Tumour thrombosis of large vessels is frequently observed in tumours with angio-invasive features such as hepatocellular carcinoma involving the portal vein or hepatic vein and renal cell carcinoma involving renal vein or inferior vena cava.5 Follicular and hurthle cell carcinomas of the thyroid gland also have well documented microscopic characteristics of microinvasion affecting the great cervical veins.3,6 On the other hand, PTC commonly spreads through lymphatics and haematogenous spread leading to distant organs metastasis is rare. Occurrence of intravascular extension with papillary thyroid cancers is even rarer and can vary in extent from the thyroid vessels up to the right atrium.6 Intravascular tumour extension usually starts at the thyroid veins with intraluminal invasion by malignant cells and deposition of fibrin, leading to continued growth.9 The tumour mass is usually surrounded by a fibrous capsule preventing the tumour cells from invading the endothelium and making resection more easy.6 This mechanism for intravascular extension of tumour cells by direct intraluminal spread should be differentiated than extra luminal vascular invasion by a locally spreading tumour, seen more often in anaplastic thyroid cancers, as management may differ in both cases.3 Nevertheless, any direct exposure of malignant cells to the circulation is an indicator of poor outcome with high probability of pulmonary and distant metastasis.7
Diagnosis of vascular tumour thrombosis by clinical examination is usually difficult as the presentation is dependent on the site and extent of the thrombus. However, the presence of dilated neck veins or unilateral upper limb swelling may indicate a more extensive involvement of larger veins as the subclavian vein or the superior vena cava (SVC). Preoperative US has an important role in the diagnosis, and operators should attempt to detect signs of tumour thrombi in all patients with thyroid masses.7 However, US is usually operator dependant and tumour thrombi can therefore be occasionally missed. Yoshimura et al.5 combined Doppler US with gallium-67 scintigraphy to identify the extent and features of the tumour thrombus of undifferentiated thyroid cancer.
Due to the rarity of thyroid cancer vascular thrombi, no established management guidelines exist. Intraluminal extension is not a contraindication for aggressive surgical treatment in differentiated thyroid cancers due to the relatively good prognosis of PTC as well as to decrease the risk of SVC obstruction, sudden death from airway occlusion, tumour embolism or fatal right atrial obstruction.6 Surgical options are dependent on the nature and extent of vascular involvement. In our case the tumour was not attached to the vascular wall which made thrombus extraction and vascular repair feasible. However, extensive vascular resection and reconstruction might be recommended in other cases whenever the vascular structures are not salvageable.6,8
4. Conclusion
Intravascular tumour extension of PTC is rare with potential serious complications. Preoperative diagnosis using neck US is possible but many cases are missed and diagnosis is made intraoperatively.2,7 All surgeons are therefore advised to check for signs of great veins involvement as thrombectomy with vascular repair or reconstruction is usually possible.
Conflict of interest
None.
Funding
None.
Ethical approval
Consent approval from the patient in question has been sought and is readily available upon request.
Author contributions
Mr Al-Jarrah and Dr Abou-Foul contributed equally to the writing of the article and acquisition of radiological and histological pictures and corresponding descriptions. Prof Heis contributed to the conception of project and review/correction of article before submission.
Key learning point.
-
•
Intravascular tumour extension of papillary thyroid cancer is rare with potential serious complications.
-
•
Preoperative diagnosis using neck ultrasound scan is possible but many cases are missed.
-
•
All papillary thyroid cancer surgeries should include checking the great veins of the neck for signs of tumour thrombosis.
-
•
Thrombectomy with vascular repair or reconstruction is usually possible with positive impact on the overall outcome.
References
- 1.Rosenbaum M.A., McHenry C.R. Contemporary management of papillary carcinoma of the thyroid gland. Expert Rev Anticancer Ther. 2009;9:317–329. doi: 10.1586/14737140.9.3.317. [DOI] [PubMed] [Google Scholar]
- 2.Koike E., Yamashita H., Watanabe S., Yamashita H., Nioguchi S. Brachiocephalic vein thrombus of papillary thyroid cancer: report of a case. Surg Today. 2002;2:59–62. doi: 10.1007/s595-002-8114-7. [DOI] [PubMed] [Google Scholar]
- 3.Gross M., Mintz Y., Maly B., Pinchas R., Muggia-Sullam M. Internal jugular vein tumour thrombus associated with thyroid carcinoma. Ann Otol Rhinol Laryngol. 2004;113:738–740. doi: 10.1177/000348940411300912. [DOI] [PubMed] [Google Scholar]
- 4.Chakravarthy V.K., Chandra Rao N.D., Chandra S.T. Study of papillary carcinoma of thyroid with uncommon sites of metastasis. Indian J Otolaryngol Head Neck Surg. 2010;62(2):198–201. doi: 10.1007/s12070-010-0031-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yoshimura M., Kawamoto A., Nakasone K., Kakizaki D., Tsutsui H., Serizawa H., Abe K. Gallium-67 accumulation to the tumour thrombus in anaplastic thyroid cancer. Ann Nucl Med. 2003;17:689–691. doi: 10.1007/BF02984976. [DOI] [PubMed] [Google Scholar]
- 6.Sugimoto S., Doihara H., Ogasawara Y., Aoe M., Sano S., Shimizu N. Intraatrial extension of thyroid cancer: a case report. Acta Med Okayama. 2006;60:135–140. doi: 10.18926/AMO/30734. [DOI] [PubMed] [Google Scholar]
- 7.Kobayashi K., Hirokawa M., Yabuta T., Fukushima M., Kihara M., Higashiyama T. Tumour thrombus of thyroid malignancies in veins: importance of detection by ultrasonography. Thyroid. 2011;21(May (5)):527–531. doi: 10.1089/thy.2010.0099. [DOI] [PubMed] [Google Scholar]
- 8.Patten D.K., Flora R., Tolley N., Palazzo F. Sporadic medullary thyroid carcinoma with a pedunculated intraluminal internal jugular vein recurrence: a case report and literature review. Int J Surg Case Rep. 2012;3(2):92–96. doi: 10.1016/j.ijscr.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Niederle B., Hausmaninger C., Kretschmer G., Polterauer P., Neuhold N., Mirza D.F. Intraatrial extension of thyroid cancer: technique and results of a radical surgical approach. Surgery. 1990;108:951–956. [PubMed] [Google Scholar]


