Abstract
Introduction:
Amnion allograft has been used in the field of medicine for its exceptional wound-modulating properties. However, in the field of dentistry, only a limited number of reports have explored its potential in healing of oral wounds.
Materials and Methods:
Amnion allograft in conjunction with coronally advanced flap has been used in the management of gingival recession.
Results:
A complete coverage along with excellent esthetics and an improvement in gingival biotype was observed at 6 months postoperatively.
Discussion:
Because of its inherent wound-modulating properties, amnion allograft may be used to enhance periodontal wound healing and enable tissue regeneration such as that in the coverage of gingival recession.
Conclusion:
Amnion allograft may provide an alternative to other conventional methods of treating gingival recession.
Keywords: Amnion allograft, gingival biotype, gingival recession
Introduction
Gingival recession is the display of the root surface of the tooth characterized by displacement of the gingival margin apically from the cementoenamel junction. It is associated with a multitude of esthetic and functional problems, including poor esthetics, root caries, tooth hypersensitivity and pulp hyperemia. Over the years, various treatments of gingival recession have evolved including pedicle and free soft tissue grafts.[1] Most of these autogenous grafts have the limitations of donor morbidity, creation of a second surgical site and limited availability. Keeping these pitfalls in mind, allografts present an attractive option for the coverage of gingival recession.
The amnion is a membrane building the amniotic sac that surrounds and protects an embryo. The amniotic membrane is a tissue of fetal origin and is composed of three major layers: A single epithelial layer, a thick basement membrane and an avascular mesenchyme.[2] It contains no nerves, muscles or lymphatics and can be easily separated from the underlying chorion. The fetal membrane was first used for the transplantation of skin in 1910.[3] With improvements in the processing and storage technologies, amniotic membrane has found application in various fields of medicine, including management of burns; reconstruction of the oral cavity, bladder and vagina; tympanoplasty; arthroplasty and so on.[4] Recently, this multipurpose tissue has found application in the field of periodontics. Velez and co-workers[5] analyzed the effects of cryopreserved amniotic membrane (CAM) on periodontal soft tissue healing and observed that it was effective in helping cicatrization, wound healing, epithelization, facilitated migration and reinforced adhesion. Another report by Gurinsky[6] demonstrated that the processed allograft amnion may provide an effective alternative to autograft tissue in the treatment of recession defects. Here, we present a case where an amnion membrane has been used for the management of gingival recession.
Materials and Methods
A 32-year-old female patient reported with a chief complaint of tooth hypersensitivity in the upper right back tooth region since 3 months. Her medical and family history was noncontributory.
On clinical examination, a Millers Class II recession[7] was observed in relation to the tooth number #14 measuring 3 mm vertically and horizontally. The patient had a thin gingival biotype.[8] The treatment plan consisted of placement of an amnion membrane (Tissue bank, Tata Memorial Hospital, India) in conjunction with a coronally advanced gingival flap. An informed consent was obtained from the patient for the same. The patient was given oral hygiene instructions and supragingival scaling and root planing was performed. After obtaining adequate anesthesia using Lignocaine hydrochloride 2%, two oblique beveled incisions, one on the mesial aspect and the other on the distal aspect of the recession site, to raise a trapezoidal flap followed by two vertical incisions extending into the alveolar mucosa were given. A trapezoidal flap was elevated, following which the exposed root surface was thoroughly planed. Tetracycline solution (1 mg/mL) was applied to the root surface for 2 min, and this was followed by thorough saline irrigation. After the flap was raised, the recession width and height were measured using a UNC-15 probe and the membrane size was calculated as 2 mm more on all sides (apically, mesially and distally) to be of sufficient dimension to cover the recession. The membrane was then placed over the root surface and the flap was sutured back in position with 4-0 nonresorbable silk sutures [Figure 1a-f]. Keeping in mind the adhesive properties of the amnion, the membrane was not sutured. Postoperative instructions, diclofenac sodium (50 mg) twice daily for 3 days and a chlorhexidine mouthrinse 0.2% twice daily for 2 weeks were prescribed to the patient.
Figure 1.
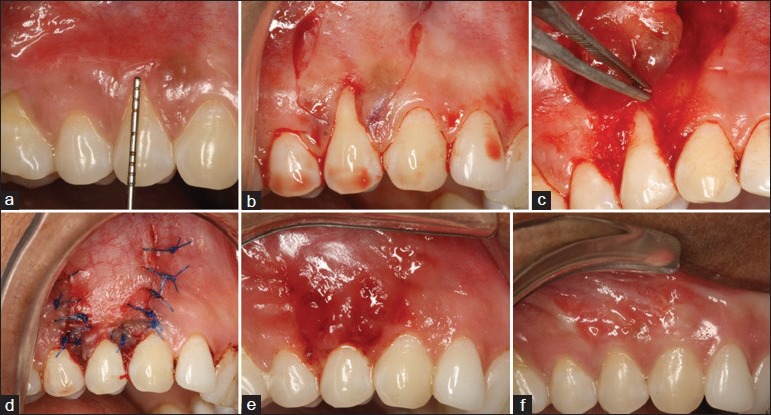
(a) Preoperative gingival recession (3 mm), (b) oblique and releasing incisions given, (c) recipient bed prepared, amnion allograft being placed, (d) flap coronally advanced and sutured, (e) healing after 10 days and (f) 6 months postoperative healing showing complete root coverage and esthetic color match
The patient was recalled after 10 days for suture removal and was followed-up till 6 months. Complete root coverage, with excellent tissue contour and color blend, was observed over the period of follow-up. Also, the tissue biotype was observed to be enhanced as compared with baseline, as assessed using the probe transparency method.[8]
Discussion
Gingival tissue has been compared with fetal tissues in its structure, fibroblast phenotype and scarless healing.[9] Amnion membrane is an allograft with many unique properties that make it a promising new substitute in the field of periodontics. It contains a variety of specialized proteins such as fibronectin, laminin, proteoglycans, glycosaminoglycans and collagen type IV, V and VII. It not only provides a matrix for cellular migration and proliferation but also enhances the wound healing process.[10] It contains a large number of cytokines including transforming growth factor-β/α, vascular endothelial growth factor, epidermal growth factor, platelet-derived growth factor-β/α and fibroblast growth factor. It has been reported to be nonimmunogenic, to reduce inflammation, reduces scar tissue, has antibacterial properties, reduces pain at the site of application and acts as a natural biological barrier.[10] Such wound modulating properties make it an interesting new option for application in oral wound healing.
Complete and stable root coverage is the ultimate goal of any root coverage procedure. In the present case, we observed that amnion allograft resulted in a complete (100%) root coverage and an excellent color match to the recipient site. The results were stable for 6 months posttreatment and no recurrence of recession was observed. Another interesting finding was the enhancement of gingival biotype (from initial thin to thick) as measured by the probe transparency method. A thick biotype has a tendency toward maintaining a more stable soft tissue in various periodontal surgical procedures.[8] Hence, all the optimum desired results as an allograft for root coverage were achieved by amnion allograft.
The results from the present report are encouraging and demonstrate that the amnion allograft is well tolerated by the gingival tissues and results in excellent healing. More studies exploring the potential of this allograft in periodontal therapies are required. This report paves a way for future studies that may investigate its application in other fields of periodontal and oral surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Bouchard P, Malet J, Borghetti A. Decision-making in aesthetics: Root coverage revisited. Periodontol 2000. 2001;27:97–120. doi: 10.1034/j.1600-0757.2001.027001097.x. [DOI] [PubMed] [Google Scholar]
- 2.Ilancheran S, Moodley Y, Manuelpillai U. Human fetal membranes: A source of stem cells for tissue regeneration and repair? Placenta. 2009;30:2–10. doi: 10.1016/j.placenta.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 3.Davis JW. Skin transplantation with a review of 550 cases at the Johns Hopkins Hospital. John Hopkins Med J. 1910;15:307–96. [Google Scholar]
- 4.Niknejad H, Peirovi H, Jorjani M, Ahmadiani A, Ghanavi J, Seifalian AM. Properties of the amniotic membrane for potential use in tissue engineering. Eur Cell Mater. 2008;15:88–99. doi: 10.22203/ecm.v015a07. [DOI] [PubMed] [Google Scholar]
- 5.Velez I, Parker WB, Siegel MA, Hernandez M. Cryopreserved amniotic membrane for modulation of periodontal soft tissue healing: A pilot study. J Periodontol. 2010;8:1797–804. doi: 10.1902/jop.2010.100060. [DOI] [PubMed] [Google Scholar]
- 6.Brian G. A novel dehydrated amnion allograft for use in the treatment of gingival recession: An observational case series. J ImpAdvCli Dent. 2009;1:11–6. [Google Scholar]
- 7.Miller PD., Jr A classification of marginal tissue recession. Int J Periodontics Restorative Dent. 1985;5:8–13. [PubMed] [Google Scholar]
- 8.Kan JY, Morimoto T, Rungcharassaeng K, Roe P, Smith DH. Gingival biotype assessment in the esthetic zone: Visual versus direct measurement. Int J Periodontics Restorative Dent. 2010;30:237–43. [PubMed] [Google Scholar]
- 9.Larjava H, Wiebe C, Gallant-Behm C, Hart DA, Heino J, Häkkinen L. Exploring scarless healing of oral soft tissues. J Can Dent Assoc. 2011;77:b18. [PubMed] [Google Scholar]
- 10.Fetterolf DE, Snyder RJ. Scientific and clinical support for the use of dehydrated amniotic membrane in wound management. Wounds. 2012;24:299–307. [PubMed] [Google Scholar]


