Abstract
Purpose:
The aim of the present study was to compare the periosteal fenestration (PF) and free mucosal graft (FMG) techniques in mandibular anterior region to increase the vestibular depth.
Methodology:
A total of 20 systemically healthy cases (10 patients in each group) with shallow vestibular depth and reduced width of attached gingiva in lower anterior region were included in the present study. Clinical parameters recorded included Gingival index (GI), Plaque index (PI), Oral hygiene index simplified (OHI S), Vestibular depth (VD), width of attached gingiva and post operative discomfort.
Findings:
The results at the end of 3 months showed that the mean GI, PI, OHI S decreased significantly and remained low throughout the study period. The mean gain in percentage of vestibular depth at the end of 3 months for group 1(PF) was 48.4% with relapse of 7.2% from the baseline. For group 2 (FMG), the mean gain in percentage of vestibular depth at the end of 3 months for was 50% with relapse of 6.2% from the baseline. The mean gain in percentage of attached gingiva at 3 months for group 1 and 2 was 65.9% and 74%, respectively. In comparison of group 1 and 2, group 2 showed better results in terms of increasing the vestibular depth and attached gingiva than group 1 although the intergroup comparison was not statistically significant.
Conclusion:
When aim of the clinician is to treat a patient with shallow vestibule together with reduced width of attached gingiva, the use of periosteal fenestration yields similar results to that of FMG.
Keywords: Free mucosal graft, periosteal fenestration, shallow vestibule
Introduction
For many years, presence of an “adequate” amount of gingiva was considered a keystone for the maintenance of periodontal health.[1] The concept of mucogingival surgery was introduced in 1950s. Initially these procedures included correction of the relationship between the gingiva and the oral mucous membrane regarding problems associated with attached gingiva, shallow vestibule and high frenum attachments. Later Miller[2] included additional procedures in this field and term “periodontal plastic procedures” was accepted by the World Workshop in Clinical Periodontics in 1996. Bohannan[3] in studying procedures for deepening the vestibule found that it is necessary to expose bone at the depth of the incision to achieve a lasting result. This gave rise in the early 1960s to the periosteal separation technique by Corn[4] which did produce the apical scar and a deepened vestibule.
A variety of vestibuloplasty procedures are in vogue with each having its own merits and demerits. In early twentieth century, use of skin grafts to augment atrophic ridges was reported. To date one of the most widely used mucogingival procedure to increase the width of attached gingiva is transplantation of free mucosa described by Bjorn[5] in 1963. The high predictability of this technique in humans has been well documented in histological, cytological and clinical studies.[6] These grafts have an advantage over skin grafts in the sense that presence of hair follicles by their growth later in the graft made this procedure less in demand; in addition autogenous gingival grafts carries the genetic nature of the keratinized mucosa. Further technological advancements came in the form of autologous cultured sheets of mucosa but these procedures caused more shrinkage of augmented tissue.[7,8,9] Hence, it sounds logical enough to compare the two procedures namely, Periosteal Fenestration and Free Mucosal Graft for increasing the vestibular depth since there is scarcity of studies comparing these two procedures.
Materials and Methods
Patient selection
A randomized controlled clinical trial was conducted on study subjects to evaluate the increase in vestibular depth with PF and FMG. Sample sizes of 20 patients aged between 18-40 years with good systemic health were selected from OPD in the Department of Periodontology, Subharti Dental College and Hospital, Meerut. Diagnosis was made on the basis of clinical signs such as shallow vestibular depth and reduced width of attached gingiva. The inclusion criteria consisted of (1) presence of site-related conditions, e.g. shallow vestibule, reduced amount of attached gingiva (≤1 mm), (2) good systemic health, (3) radiographic evidence of sufficient bone adjacent to the involved site, (4) n-o mobility of involved teeth. The exclusion criteria consisted of (1) systemic diseases that affect the periodontium, (2) poor oral hygiene, (3) pregnancy, (4) steroid therapy, (5) non-compliant patients, (6) bleeding disorders, (7) smokers and tobacco chewers. The patients selected on the above criteria were then explained about the treatment procedure, associated risks and benefits and their written consent was obtained. These patients were divided into two groups, i.e. Group 1 (PF) and 2 (FMG), comprising of 10 patients each.
Methodology
Clinical parameters recorded included: GI, Loe and Sillness; PI, Sillness and Loe; OHI-S, Greene and vermillion; Vestibular depth; Width of attached gingiva; Patient discomfort evaluation. GI, PI, OHI-S, vestibular depth were recorded at baseline, 1 and 3 months. Width of attached gingiva was recorded at baseline and 3 months and postoperative discomfort was evaluated at 1 week and after 1 month. Surgical procedures were performed one week following phase I therapy in both the groups. Radiographs of the sites were recorded pre-operatively. Vestibular depth was measured with the help of digital Vernier calipers and with periodontal probe [Figures 1 and 2] on the mid facial aspect of lower central and lateral incisors (gingival margin to mucogingival junction) and average of these four teeth was taken.
Figure 1.
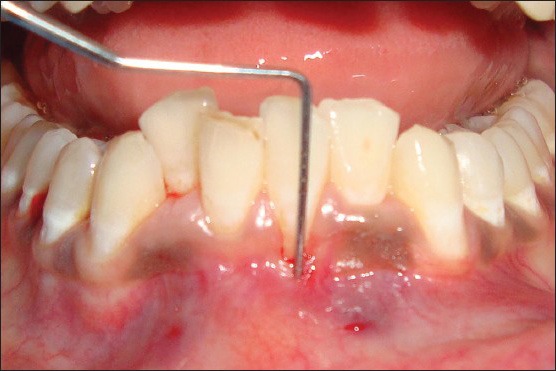
Pre-operative vestibular depth
Figure 2.

Pre-operative vestibular depth
Surgical technique
Group 1 (PF)
After injecting local anesthesia (Xylocaine Hydrochloride 2% with 1:80,000 adrenaline), at the site of surgery, horizontal incision was given at the existing mucogingival line to the required depth (4-6 mm) and by blunt dissection, the periosteum and adherent fibrous tissue were detached apically and the labial alveolar plate was thus exposed. Ochsenbein chisels and round carbide burs were used to create periosteal fenestration [Figure 3]. The depth of fenestration was 1 to 1.5 mm. The wound so created was covered with periodontal pack.
Figure 3.
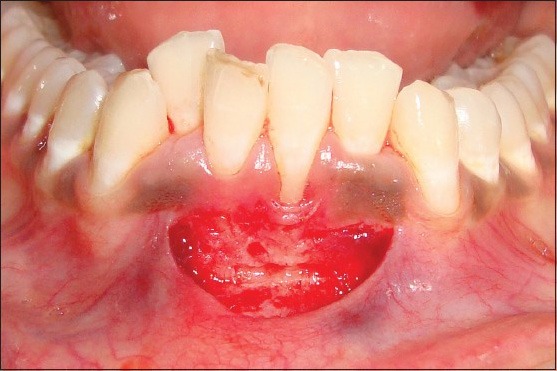
Fenestration given at the base of the defect
Group 2 (FMG)
Recipient site preparation
After local anesthesia was obtained at the recipient site, with a no 15 surgical blade held at approximately 90 degrees to the gingival surface; a superficial incision was made at the MGJ. The lip was retracted firmly as the incision was made. The periosteal recipient bed was then prepared by sharp dissection in an apical direction with blade held nearly parallel to the alveolar process.
Donor site
The apico-coronal dimension of graft in the area to be augmented was approximately 4-6 mm [Figure 4]. The foil template was prepared and positioned on the periosteal bed. The graft area was outlined, extending from the palatal root of the first molar and the distal line angle of the canine. The thickness of the graft was kept close to 1.5 mm and dissection was done with a no. 15 blade kept parallel to the epithelial outer side of the graft. Once the donor tissue was released, pre-formed palatal stents were placed to decrease post-operative discomfort. The graft was examined and excessive fatty tissue and irregularities were scraped with no. 15 blade.
Figure 4.
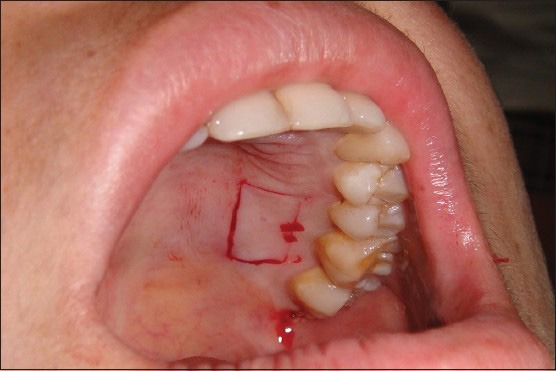
Graft procurement from palate
The graft was sutured to the recipient site so that the external bevel of the recipient site corresponds with the internal bevel at the coronal aspect of the graft. This type of “lap joint” virtually eliminated the thick bulgy appearance that occurred at the graft-bed junction if a “butt joint” is used. Sutures were placed at each end of the graft [Figure 5]. No sutures were given at the base of the graft. Following graft stabilization, firm pressure with a damp gauze was applied for several minutes to assure only a thin fibrin clot exist beneath the donor tissue.
Figure 5.

Graft placed at recipient site
Post-operative care
After the surgical procedure, patients in both the groups were then given post-operative instructions and medications (analgesics: Ibuprofen 400 mg TDS and antibiotics: Amoxicillin 500 mg TDS) for 5 post-operative days. They were given the following instructions: Avoid intake of hot food for the first 24 hours, avoid any undue trauma to the treated site, not to brush the teeth on treated site for at least 14 days. All the patients were placed on 0.2% chlorhexidine gluconate rinse, twice daily for 3 weeks and recalled at regular intervals.
Post-operative recall visit
Patients of both groups were recalled post-operatively at 1, 7, 14, 30 and 90 days. Periodontal dressing and sutures were removed after 14 days. Clinical parameters which were recorded at baseline were re-recorded post-operatively at 1 and 3 months [Figures 6 and 7]. The patients were reinforced with oral hygiene instructions at every visit.
Figure 6.

3 months post-operative
Figure 7.

3 months post-operative
Statistical analysis
All the values were expressed in the form of mean, standard deviation and standard error of mean. The parameters were compared using Paired ‘t’ test for intra group comparison and Unpaired ‘t’ test for intergroup comparison at similar time i.e. baseline, 1 month and 3 months. The analysis was performed by the data analysis software through Microsoft Excel.
Results
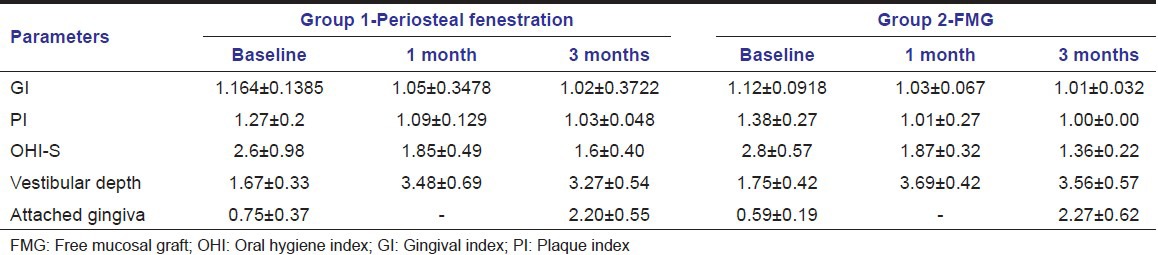
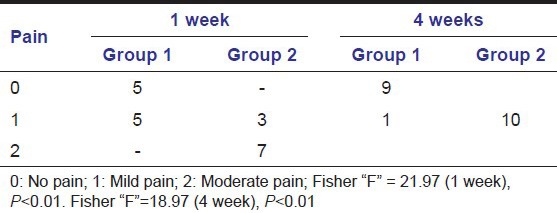
During the course of the study, wound healing was uneventful in both the groups. Table 1 shows mean and S.D. of both groups at different time points for different parameters. The results at the end of 3 months showed that the mean GI, PI, OHI-S decreased significantly and remained low throughout the study period. The mean gain in percentage of vestibular depth at the end of 3 months for group 1 was 48.4% with relapse of 7.2% from the baseline. For group 2, the mean gain in percentage of vestibular depth at the end of 3 months for was 50% with relapse of 6.2% from the baseline. The mean gain in percentage of attached gingiva at 3 months for group 1 and 2 was 65.9% and 74%, respectively (Graph 1). In inter-group comparison, group 2 showed better results in terms of increasing the vestibular depth and attached gingiva than group 1 although intergroup comparison was not statistically significant [Table 2]. The use of palatal donor tissue increases morbidity, the risk of surgical complications and post-operative pain in group 2. The most obvious difference between the two procedures is post-operative pain, which was significantly greater in patients treated with FMG. At 1 week, 7 patients reported of moderate pain treated with FMG [Table 3].
Table 1.
Mean and SD of both groups at different time points for different parameters
Graph 1.
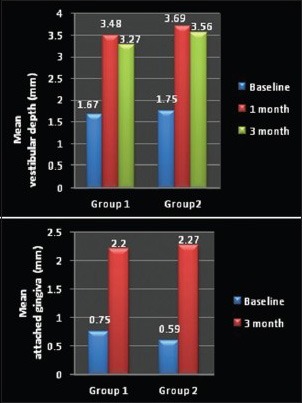
Comparative analysis between group 1 and 2 (attached gingiva and vestibular depth)
Table 2.
Inter-group comparison at different time points (unpaired “t” test)
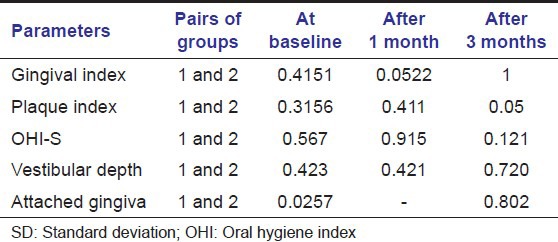
Table 3.
Subjective evaluation of post-operative discomfort
Discussion
It has been shown that with less than 1 mm of attached gingiva, gingival health cannot be established.[10] Although Bowers[11] mentioned that it may be sufficient to maintain proper oral hygiene. Corn[12] laid emphasis on the fact that apico coronal height of attached gingiva ought to exceed at least 3 mm. Therefore, the purpose of this present randomized controlled clinical trial was an endeavor to investigate the potentiality of attaining gain in vestibular depth and attached gingiva using periosteal fenestration and FMG, which were correlated with clinical outcomes at one and three months. The present study focused on answering the question of whether one method is superior to other for gingival augmentation.
GI, PI and OHI-S were recorded in the present study to assess patient compliance in maintaining oral hygiene. The mean GI at baseline was 1.164 ± 0.138 and at 1 month it reduced to 1.05 ± 0.347. At 3 months, GI further decreased to 1.02 ± 0.372, showing a mean decrease of 0.03 (2.8%), which was statistically insignificant. The scores of PI in group 1 reduced from baseline (1.27 ± 0.2) to one month (1.09 ± 0.12) and from baseline to three months (1.03 ± 0.04). For OHI-S, the scores in the same group reduced from baseline (2.6 ± 0.98) to one month (1.85 ± 0.49) and from baseline to three months (1.6 ± 0.4).
Wade[13] carried out deepening of the inferior labial vestibule according to the technique of Edlan and Mejchar on 25 patients aged 17-55 years. The Plaque Index pre-operatively was 1.70 ± 0.31 and 0.88 ± 0.20 post-operatively (P < 0.05). The correlation coefficient between the plaque scores suggests that there was a definite relation which was strengthened as a result of the operation. It was concluded that when there is only a limited amount or no gingival tissue on the labial aspect of the mandibular anterior teeth, but no pockets, the technique provides a predictable way in which gingival health can be achieved and maintained.
Various techniques have been described for vestibular extension, which includes submucosal vestibuloplasty, Kazanjian technique[14] and soft tissue grafting vestib uloplasty.[15] The results of present investigation, seems to offer basic and objective information concerning vestibular fornix extension. First, it is clear that vestibular depth can be increased and second, that this increase, once achieved, is relatively stable following the active healing period. In group 1 vestibular deepening by PF was performed which was found to be simple surgical technique. It involved initial incision at mucogingival junction which was extended 4-6 mm apically. At the base of the operative field, periosteum was removed, and fenestration was created. This fenestration created a scar which prevented post-surgical narrowing of the attached zone. Results obtained from the present study showed that mean gain in vestibular depth obtained by PF at 3 months was 48.4% which was statistically significant.
Conclusion
From this study the following conclusions can be drawn:
Both the treatment modalities resulted in significant gain in vestibular depth and width of attached gingiva
Mean vestibular depth at 3 months for group 1 was 48.4% with relapse of 7.2% from the baseline. While in group 2, at the end of 3 months it was 50% with relapse of 6.2% from the baseline
Mean gain in vestibular depth was greater in FMG group than PF but the difference was not statistically significant
Mean gain in width of attached gingiva was greater for FMG group (2.27 mm ± 0.62 mm) than PF group (2.20 mm ± 0.55 mm) but the difference was not statistically significant.
Limitations
The following limitations were observed in the present study
The small sample size in the present study was limited to 20 subjects. A larger sample size would yield better results
In the present study the time duration of recall was 3 months. Long-term analysis is needed to determine the stability of the results, since creeping attachment occurs highest till 9 months
The operator was the assessor in the present study therefore possibility of operator bias to some extent cannot be denied.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Nabers CL. Repositioning the attached gingiva. J Periodontol. 1954;25:38–9. [Google Scholar]
- 2.Miller PD., Jr Regenerative and reconstructive periodontal plastic surgery. Mucogingival surgery. Dent Clin North Am. 1988;32:287–306. [PubMed] [Google Scholar]
- 3.Bohannan HM. Studies in the alteration of vestibular depth III. Vestibular incision. J Periodontol. 1963;34:209–15. [Google Scholar]
- 4.Corn H. Periosteal separation-Its clinical significance. J Periodontol. 1962;33:140–53. [Google Scholar]
- 5.Bjorn H. Free transplantation of gingiva propria. Swedish Dent J. 1963;22:684–9. [Google Scholar]
- 6.Schmid MO, Mörmann W, Bachmann A. Mucogingival surgery. The subperiosteal vestibule extension. Clinical results 2 years after surgery. J Clin Periodontol. 1979;6:22–32. doi: 10.1111/j.1600-051x.1979.tb02287.x. [DOI] [PubMed] [Google Scholar]
- 7.McGuire MK, Nunn ME. Evaluation of the safety and efficacy of periodontal applications of a living tissue-engineered human fibroblast-derived dermal substitute. I. Comparison to the gingival autograft: A randomized controlled pilot study. J Periodontol. 2005;76:867–80. doi: 10.1902/jop.2005.76.6.867. [DOI] [PubMed] [Google Scholar]
- 8.Imberman M. Gingival augmentation with an acellular dermal matrix revisited: Surgical technique for gingival grafting. Pract Proced Aesthet Dent. 2007;19:123–8. [PubMed] [Google Scholar]
- 9.McGuire MK, Scheyer ET, Nevins ML, Neiva R, Cochran DL, Mellonig JT, et al. Living cellular construct for increasing the width of keratinized gingiva: Results from a randomized, within-patient, controlled trial. J Periodontol. 2011;82:1414–23. doi: 10.1902/jop.2011.100671. [DOI] [PubMed] [Google Scholar]
- 10.Hall WB. Proceedings of the World Workshop in Clinical Periodontics. Chapter VII. Chicago: American Academy of Periodontology; 1989. Gingival augmentation/mucogingival surgery; pp. 5–7. [Google Scholar]
- 11.Bowers G. A study of the width of attached gingiva. J Periodontol. 1963;34:201–9. [Google Scholar]
- 12.Corn H. Periosteal separation-Its clinical significance. J Periodontol. l962;3:140–53. [Google Scholar]
- 13.Edlan A, Mejchar B. Plastic surgery of the vestibulum in periodontal therapy. Int Dent J. 1963;13:593. [Google Scholar]
- 14.Kazanjian VH. Surgical operations as related to satisfactory dentures. Dent Cosmos. 1924;66:387. [Google Scholar]
- 15.Fröschl T, Kerscher A. The optimal vestibuloplasty in preprosthetic surgery of the mandible. J Craniomaxillofac Surg. 1997;25:85–90. doi: 10.1016/s1010-5182(97)80050-9. [DOI] [PubMed] [Google Scholar]


