Abstract
Oral mucosal melanoma is a rare malignancy with the tendency to metastasize and locally invade tissues more readily than other malignant tumor of the oral cavity. It occurs approximately four times more frequently in the oral mucosa of the upper jaw usually on the palate or alveolar gingiva. The chameleonic presentation of malignant melanoma, its asymptomatic condition, rarity of the lesion, poor prognosis and the necessity of a highly specialized treatment are factors that should be seriously considered by the involved health care provider. Herein we report a rare and interesting case of oral malignant melanoma of the maxillary anterior gingiva, which was clinically and histopathologically diagnosed with a brief review of literature, has been discussed.
Keywords: Melanocytes, oral malignant melanoma, pigmented lesions
Introduction
Oral malignant melanoma (OMM) was first described by Weber in 1859.[1] Malignant melanoma of the oral cavity is an extremely rare tumor arising from the uncontrolled growth of melanocytes found in the basal layer of the oral mucous membranes.[1,2] Melanocytes are neural crest-derived cells that migrate to the skin, mucous membranes and several other sites. The incidence of melanoma has been steadily increasing in the past several decades with an annual increase of 3-8% worldwide.[3] Most common form of melanoma are the cutaneous and the ocular form. Mucosal melanoma involving the sinonasal cavity, oral cavity, pharynx, larynx, and upper oesophagus[4] rare extremely are and accounts for only 0.5% of all oral neoplasms.[5] Nearly 80% of oral melanomas arise in the mucosa of the upper jaw, with the majority occurring on keratinizing mucosa of the palate and alveolar gingivae.[2] It occurs slightly more often in males 2.8:1 male to female ratio) and the age range is from. 20-83 years worth an average age of 56 years.[6]
The clinical presentation of this condition may vary widely which is divided into following five types: Pigmented nodular type, pigmented macular type, pigmented mixed type, non-pigmented nodular type and non-pigmented mixed type.[2,4,6] Non pigments forms of malignant melanoma often cannot be distinguished clinically from other benign or malignant oral tumors which can be diagnosed through biopsy. A pigmented lesion of the oral cavity should be viewed with suspicion since it does not possess clinical specificity.[7]
This manuscript reports a case of OMM of the maxillary anterior gingiva with cervical lymph node metastasis, which has been discussed with detailed investigations such as biochemical, histopathology, ultrasound and contrast enhanced computed tomography (CECT) to emphasize the necessity for early diagnosis and treatment of this deadly condition.
Case Report
A 42-year-old female patient [Figure 1] reported with the chief complaint of a painless, pigmented growth in the left anterior maxillary gingiva since 3 months, which started as a pin point lesion, progressed gradually, and extended to the palatal gingival margin. She gave no history of any systemic illness or trauma to the head and neck region. General physical examination was insignificant and her vital signs were under normal limits.
Figure 1.

Extra-oral photograph
Extraoral examination revealed solitary left submandibular lymph node which was palpable, tender and firm and fixed to the lower border of the mandible. A solitary cervical lymph node was also palpable in the right side about 3 × 3 cm in size, which was freely mobile, firm and non-tender [Figure 2]. On intraoral clinical examination, a non-tender pigmented growth was present on the left maxillary attached gingiva in relation to central and lateral incisors of about 2 × 3 cm in size approximately [Figure 3]. The growth was sessile with rough surface and the color of overlying mucosa of the growth was black with irregular periphery extending to the marginal gingiva of the adjacent tooth, the growth was extending to the palatal gingiva involving the rugae of hard palate extending from the maxillary right second premolar to left first premolar [Figure 4]. There was displacement of left central and lateral incisors due to the pigmented growth.
Figure 2.

Swelling in the submandibular region
Figure 3.

Growth in relation to labial gingiva
Figure 4.

Growth in relation to palatal gingiva
Correlating the patient's complaint, with the history and clinical examination a differential diagnosis of melanosis, amalgam tattoo, drug induced pigmentation, mucosal nevus, melanotic-macule, melano acanthoma and malignant melanoma was arrived. Melanosis is a common benign condition in the oral cavity, Amalgam restorations are not evident, there is no history of any recent medications, mucosal nevi are <0.5 cm in size, melanotic macule are less than 1 cm and are well-circumscribed lesion, melano acanthoma is also a benign tumor, but it can spread up to centimeters in few weeks, Malignant melanoma is a rare aggressive neoplasm, which represents 1-2% of oral malignancies.
A complete blood cell count, biochemical analysis, and urine analysis were insignificant and under normal limits. An intraoral periapical radiograph of the region along with a panoramic view revealed a radiolucent area with tooth displacement in relation to 21, 22 [Figure 5]. Ultrasonography reports revealed hyper-intense vascularity with low velocity waveform suggesting a large space occupying lesion of the neck indenting major vessels suggestive of malignancy, which necessitates correlation with CT picture. CECT revealed a well-defined in-homogenously enhancing hypodense nodule in the left premaxillary region with no bony erosion and also evidence of a large necrotic left level 2 cervical lymphadenopathy measuring 34 × 32 mm compressing and displacing left internal jugular vein [Figure 6].
Figure 5.

Orthopantomogram showing boneloss in relation to 21 and 22 region
Figure 6.

Computed tomography picture reveals necrotic lymphnode
The radiographic differential diagnosis that were considered are metastatic tumor, tuberculosis and lymphoma were included.
An incisional biopsy was performed the histopathological section shows parakeratinized stratified squamous epithelium with underlying connective tissue stroma. Connective tissue shows atypical melanocytes and melanin pigmentation throughout the stroma. Dysplastic features like cellular atypism and anisocytosis are seen in connective tissue stroma suggestive of malignant melanoma [Figure 7]. Work for distant metastases (CT scan of chest, brain and abdomen) was negative.
Figure 7.
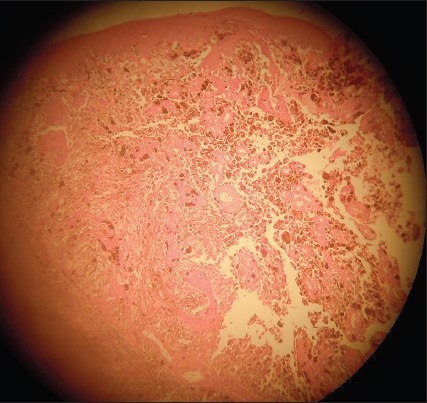
Hyperpigmentation reveals atypical melanocytes and melanin pigmentation
Based on the clinical examination, radiologic and histopathologic features a final diagnosis of malignant melanoma was arrived. Medical information was provided to the patient and her family regarding the diagnosis, staging, therapeutic options and prognosis. The patient was referred to a cancer institute for further management where she underwent 2 cycles of chemotherapy for which she failed to respond and eventually passed away.
Discussion
OMM may demonstrate significant heterogenecity in morphological features, developmental process and biological behavior that could render the clinical diagnosis extremely difficult.[2,6] The differential diagnosis includes melanotic macule, smoking associated with melanosis, post-inflammatory pigmentation, melanoplakia, melanoacanthoma, nevi, Addison's disease, Peutz-Jeghur syndrome, amalgam tattoo, Kaposi's sarcoma[7] and many other conditions sharing macroscopic characteristics and drug induced pigmentation more often the culprit is azidothymidine.[8]
Umedaa et al., described 3 growth phases of OMM: (1) A macular phase consisting of proliferation of dendrite melanocytes without apparent atypia and with simple hyperpigmentation in the basal cell layer and incontinence; (2) a pigmented plaque phase consisting of preinvasive tumor cell nests in the lower epithelial layer; and (3) a nodular phase consisting of spindle shaped or epithelloid tumor cells in the submucosa.[4,9]
Histologically, it resembles squamous cell, carcinoma, with large polyhedral cells with eosinophillic cytoplasm and sometimes exhibiting fusiform and mixed type of cells with downward invasion into the connective tissue.[9] Immunohistochemically, the typical melanoma is reactive for vimentin, S-100, protein, HMB-45, melan-A, tyrosinase and micropthalmia transcription factor.[8] Because of the differences in clinical features, histologic, characteristics, and prognosis, OM is not easily classified into the existing cutaneous melanoma categories (nodular, superficial spreading, lentigo maligna, and acral lentiginous melanoma[10,11]).
The 1995 Westop Banff workshop recommended that OMM should be classified separately from cutaneous lesions and terminology should include descriptive terms such as melanoma in-situ and invasive melanoma.[10] In association with these categories, two further types were considered. One type is described as invasive melanoma with an in-situ component (mixed in-situ and invasive oral mucosal melanomas) and the other type is defined as an atypical melanocytic proliferation (borderline lesion) to identify lesions that may have originated from an in-situ melanoma.[10]
Greene et al., proposed three criteria for the diagnosis of primary oral melanoma.[12]
Demonstration of malignant melanoma in the oral mucosa
Presence of the so-called “junctional activity” (i.e., melanocytes arranged along the basal layer of the surface epithelium) in the lesion
Inability to show malignant melanoma at any other primary site.[12]
In general, the growth of mucosal melanoma closely resembles the nodular pattern of its cutaneous counterpart. This characteristic, in part explains the poor prognosis of these lesions. Patients with lesions of less than 2 mm thick that have a significant survival advantage compared with those with lesions of greater than 2 mm.[13,14] The American joint committee on cancer does not have published guidelines for the staging of OMMs. A simple tumor, node, metastasis (TNM) classification of malignant tumors (TNM) clinical staging system for oral mucosal melanoma recognizes three stages and this system has been shown to be of prognostic value.[14,15]
The treatment policy for OMM is unclear, according to Pandey et al.[16] Medical therapy is not often beneficial with OM. Drug therapy (dacarbazine), therapeutic radiation and immunotherapy are used in the treatment of cutaneous melanoma, but, they are of questionable benefits to patients with OM.[17] Dacarbazine is not effective in the treatment of OM. However, dacarbazine in conjunction with interleukin-2 (IL-2) may have therapeutic value.[18,19] Other immunotherapeutic drugs that are occasionally used together are believed to activate killer T cells and inhibit suppressor T-cells, resulting in a reduction in the size of the melanoma. Surgery remains the preferred treatment. Recently, surgical excision with a course of IL-2 as adjunctive therapy to prevent or limit recurrence has been proposed. The prognosis for patients with OMM is relatively dismal, but early recognition and treatment greatly improve the prognosis.[20,21]
After surgical ablation, recurrence and metastasis are frequent events, and most patients die because of the disease in 2 years. Tumor vaccines are being widely used as adjuvant therapy for melanoma. Vaccines have potential for preventing recurrence and prolonging survival when patient has been rendered clinically tumor free by standard means, such as surgery but is known to be at high risk of recurrence.[22,23,24]
Systemic chemotherapy is used in patients with advanced Stage II or III melanoma in which response to therapy is associated with prolonged survival. It is generally agreed upon that melanomas are not radiosensitive. Irradiation therapy is used occasionally as a primary modality in the older population and in medically compromised patients.[25] A review of the literature indicates the 5 years survival rate to be within a broad range of 4.5-48%, but a large cluster occurs at 10-25%.
Conclusion
OMMs are rare, but aggressive tumors with very low survival rates which can metastasize rapidly. towing to its rarity, all pigmented lesions in the oral cavity should be examined with suspicion. The treatment of choice for oral melanomas is wide surgical resection with or without neck dissection depending upon chemotherapy as an adjuvant or palliative therapy. However, close patient monitoring is imperative to check for recurrence. Hence, the purpose of this manuscript is to emphasize on early diagnosis and to maintain high index of suspicion for those pigmented lesions occurring in the high risk sites such as palate and maxillary gingiva.
Acknowledgment
We would like to sincerely thank Dr. Paul Richard for referring the patient.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Ullah H, Vahiker S, Singh M, Baig M. Primary malignant mucosal melanoma of the oral cavity: A case report. Egypt J Ear Nose Throat Allied Sci. 2010;11:48–50. [Google Scholar]
- 2.Dimitrakopoulos I, Lazaridis N, Skordalaki A. Primary malignant melanoma of the oral cavity. Report of an unusual case. Aust Dent J. 1998;43:379–81. [PubMed] [Google Scholar]
- 3.Pour MS. Malignant melanoma of oral cavity. J Dent. 2007;4:44–51. [Google Scholar]
- 4.Cockerell CJ. The pathology of melanoma. Dermatol Clin. 2012;30:445–68. doi: 10.1016/j.det.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 5.Gu GM, Epstein JB, Morton TH., Jr Intraoral melanoma: Long-term follow-up and implication for dental clinicians. A case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:404–13. doi: 10.1016/s1079-2104(03)00320-2. [DOI] [PubMed] [Google Scholar]
- 6.Tanaka N, Mimura M, Ichinose S, Odajima T. Malignant melanoma in the oral region: Ultrastructural and immunohistochemical studies. Med Electron Microsc. 2001;34:198–205. doi: 10.1007/s007950100016. [DOI] [PubMed] [Google Scholar]
- 7.Magliocca KR, Rand MK, Su LD, Helman JI. Melanoma-in-situ of the oral cavity. Oral Oncol Extra. 2006;42:46–8. [Google Scholar]
- 8.Kumar SV, Swalin N. Oral malignant melanoma: A case report. Int J Oral Maxillofac Pathol. 2011;2:50–4. [Google Scholar]
- 9.Bancroft JD, Gamble M. 6th ed. Philadelphia: Churchill Livingston Elsevier Publishers Ltd; 2008. Theory and Practice of Histological Techniques; p. 725. [Google Scholar]
- 10.Femiano F, Lanza A, Buonaiuto C, Gombos F, Di Spirito F, Cirillo N. Oral malignant melanoma: A review of the literature. J Oral Pathol Med. 2008;37:383–8. doi: 10.1111/j.1600-0714.2008.00660.x. [DOI] [PubMed] [Google Scholar]
- 11.Clark WH, Jr, From L, Bernardino EA, Mihm MC. The histogenesis and biologic behavior of primary human malignant melanomas of the skin. Cancer Res. 1969;29:705–27. [PubMed] [Google Scholar]
- 12.Greene GW, Haynes JW, Dozier M, Blumberg JM, Bernier JL. Primary malignant melanoma of the oral mucosa. Oral Surg Oral Med Oral Pathol. 1953;6:1435–43. doi: 10.1016/0030-4220(53)90242-4. [DOI] [PubMed] [Google Scholar]
- 13.Patrick RJ, Fenske NA, Messina JL. Primary mucosal melanoma. J Am Acad Dermatol. 2007;56:828–34. doi: 10.1016/j.jaad.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 14.Balch CM, Buzaid AC, Soong SJ, Atkins MB, Cascinelli N, Coit DG, et al. New TNM melanoma staging system: Linking biology and natural history to clinical outcomes. Semin Surg Oncol. 2003;21:43–52. doi: 10.1002/ssu.10020. [DOI] [PubMed] [Google Scholar]
- 15.Prasad ML, Patel SG, Huvos AG, Shah JP, Busam KJ. Primary mucosal melanoma of the head and neck: A proposal for microstaging localized, Stage I (lymph node-negative) tumors. Cancer. 2004;100:1657–64. doi: 10.1002/cncr.20201. [DOI] [PubMed] [Google Scholar]
- 16.Pandey M, Abraham EK, Mathew A, Ahamed IM. Primary malignant melanoma of the upper aero-digestive tract. Int J Oral Maxillofac Surg. 1999;28:45–9. [PubMed] [Google Scholar]
- 17.Chidzonga MM, Mahomva L, Marimo C, Makunike-Mutasa R. Primary malignant melanoma of the oral mucosa. J Oral Maxillofac Surg. 2007;65:1117–20. doi: 10.1016/j.joms.2006.11.045. [DOI] [PubMed] [Google Scholar]
- 18.Umeda M, Komatsubara H, Shibuya Y, Yokoo S, Komori T. Premalignant melanocytic dysplasia and malignant melanoma of the oral mucosa. Oral Oncol. 2002;38:714–22. doi: 10.1016/s1368-8375(02)00008-8. [DOI] [PubMed] [Google Scholar]
- 19.Kowalski LP, Sanabria A. Elective neck dissection in oral carcinoma: A critical review of the evidence. Acta Otorhinolaryngol Ital. 2007;27:113–7. [PMC free article] [PubMed] [Google Scholar]
- 20.Meleti M, Leemans CR, Mooi WJ, Vescovi P, van der Waal I. Oral malignant melanoma: A review of the literature. Oral Oncol. 2007;43:116–21. doi: 10.1016/j.oraloncology.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 21.González-García R, Naval-Gías L, Martos PL, Nam-Cha SH, Rodríguez-Campo FJ, Muñoz-Guerra MF, et al. Melanoma of the oral mucosa. Clinical cases and review of the literature. Med Oral Patol Oral Cir Bucal. 2005;10:264–71. [PubMed] [Google Scholar]
- 22.Temam S, Mamelle G, Marandas P, Wibault P, Avril MF, Janot F, et al. Postoperative radiotherapy for primary mucosal melanoma of the head and neck. Cancer. 2005;103:313–9. doi: 10.1002/cncr.20775. [DOI] [PubMed] [Google Scholar]
- 23.Rapidis AD, Apostolidis C, Vilos G, Valsamis S. Primary malignant melanoma of the oral mucosa. J Oral Maxillofac Surg. 2003;61:1132–9. doi: 10.1016/s0278-2391(03)00670-0. [DOI] [PubMed] [Google Scholar]
- 24.Sivakumar G, Sivapathasundharam B, Karthiga KS. Malignant melanoma of the oral cavity – Case reports and review of literature. Indian J Dent Res. 2004;15:70–3. [PubMed] [Google Scholar]
- 25.Ulusal BG, Karatas O, Yildiz AC, Oztan Y. Primary malignant melanoma of the maxillary gingiva. Dermatol Surg. 2003;29:304–7. doi: 10.1046/j.1524-4725.2003.29068.x. [DOI] [PubMed] [Google Scholar]


