Abstract
Objective
Researchers have yet to establish how interventions to increase physical activity influence specific self-efficacy beliefs. The current study sought to quantify the effect of interventions to increase physical activity among healthy adults on exercise task (EXSE) and barrier self-efficacy (BSE) via meta-analysis. Intervention characteristics associated with self-efficacy and physical activity changes were also identified.
Methods
A systematic database search and manual searches through reference lists of related publications were conducted for articles on randomized, controlled physical activity interventions. Published intervention studies reporting changes in physical activity behavior and either EXSE or BSE in healthy adults were eligible for inclusion.
Results
Of the 1,080 studies identified, 20 were included in the meta-analyses. Interventions had a significant effect of g = 0.208, 95% confidence interval (CI) [0.027, 0.388], p < .05, on EXSE; g = 0.128, 95% CI [0.05, 0.20], p < .05 on BSE; and g = 0.335 95% CI [0.196, 0.475], p < .001, on physical activity. Moderator analyses indicated shorter interventions that did not include structured exercise sessions effectively increased EXSE and physical activity, whereas long interventions improved BSE. Interventions that did not provide support increased BSE and physical activity levels. Further, interventions that did not require the use of daily exercise logs improved EXSE and physical activity behavior.
Conclusion
Interventions designed to increase physical activity differentially influenced EXSE and BSE. EXSE appeared to play a more significant role during exercise adoption, whereas BSE was involved in the maintenance of exercise behavior. Recommendations are offered for the design of future interventions.
Keywords: exercise intervention, psychosocial, exercise self-efficacy, randomized controlled trial, health behavior change
Despite the well-established health benefits of physical activity, such as reduced risk of cardiovascular disease (Fletcher et al., 1996) and obesity (Ohkawara, Tanaka, Miyachi, Ishikawa-Takata, & Tabata, 2007), only 32% of people in the United States regularly engage in the recommended levels of exercise (U.S. Department of Health and Human Services, 2011). Consequently, researchers have developed numerous multifaceted intervention approaches to increase physical activity behavior. A recent comprehensive metaanalysis (Conn, Hafdahl, & Mehr, 2011) indicated that such interventions have been modestly effective for increasing physical activity among samples of healthy adults. However, the psychological mechanisms underlying successful adoption and maintenance of regular exercise behavior by healthy adults remain poorly understood. Until researchers determine which psychological processes drive physical activity changes and identify methods that reliably enhance these constructs, it remains unlikely that interventions can be delivered optimally to improve physical activity behavior at a population level. By way of the present review and meta-analyses, we sought to (1) quantify the impact of interventions to increase physical activity in healthy adults on exercise task and barrier self-efficacy (EXSE and BSE, respectively), and (2) identify intervention components associated with changes in selfefficacy (SE) beliefs and physical activity behavior.
SE Beliefs Are Related to Physical Activity Behavior
SE has been used to describe one’s confidence in the ability to execute specific actions required to achieve specific outcomes (Bandura, 1997). Social– cognitive theorists have asserted that SE affects the selection of activities individuals choose to engage in, the degree of challenge they strive for when setting goals, and the amount of persistence and effort exuded in the pursuit of goals (Bandura, 1977, 1998). SE has been a key variable in theoretical approaches applied to improving physical activity levels, including social– cognitive theory (Bandura, 1997) and the transtheoretical model (Prochaska & DiClemente, 1983). SE has represented the strongest, most consistent psychological correlate of physical activity behavior (Kaewthummanukul & Brown, 2006; Sharma, Sargent, & Stacy, 2005; Sherwood & Jeffery, 2000) and plays a critical role in enacting positive exercise behavior changes (Burke, Beilin, Cutt, Mansour, & Mori, 2008; Courneya & McAuley, 1995; Dutton et al., 2009; Lewis, Marcus, Pate, & Dunn, 2002; Sherwood & Jeffery, 2000).
EXSE and BSE Represent Distinct Constructs
The predictive strength of an SE belief hinges on its specificity to the behavior of interest (Bandura, 1997). Therefore, a variety of SE constructs are relevant to exercise behavior. EXSE and BSE are two of the most frequently indexed and significant SE constructs related to physical activity behavior (Maddux, 1995; McAuley & Blissmer, 2000; McAuley & Mihalko, 1998). EXSE has referred to people’s perceived capabilities to complete a physical activity prescription or perform specified exercise tasks (McAuley, Lox, & Duncan, 1993). BSE has been defined as confidence to exercise in the face of common barriers to exercise participation, such as inclement weather, a busy schedule, and feeling tired (McAuley, 1992). Though EXSE and BSE are distinct constructs (McAuley, Jerome, Marquez, Elavsky, & Blissmer, 2003), they are often merged and broadly referred to as “exercise SE” in the literature. Most studies on exercise SE index either EXSE or BSE but rarely elucidate which construct is being measured. The use of such inconsistent terminology has led to a lack of clarity regarding the specific contributions of EXSE and BSE to exercise behavior change, as well as the most effective methods to modify each.
Though exercise SE represents one of the most intensively assessed constructs associated with exercise behavior, few studies have simultaneously measured physical activity intervention effects on both EXSE and BSE (Blanchard et al., 2007; Hughes, Seymour, Campbell, Whitelaw, & Bazzarre, 2009; McAuley, Jerome, Marquez, et al., 2003; McAuley, Mailey, et al., 2011). EXSE and BSE levels appear to vary differently across intervention time points. While some evidence has suggested EXSE plays a more important role early in exercise interventions during exercise behavior adoption (Blanchard et al., 2007) and BSE better predicts long-term changes in exercise behavior (i.e., maintenance of exercise participation in longitudinal interventions; Blanchard et al., 2007; Hughes et al., 2009), findings on temporal changes of EXSE and BSE throughout interventions and their respective contributions to exercise behavior have largely been equivocal (Hughes et al., 2009; McAuley, Jerome, Marquez, et al., 2003). It remains unclear whether meaningful temporal patterns of change in EXSE and BSE exist during interventions and if these changes influence exercise behavior in different ways. By assessing the effects of different intervention lengths on EXSE, BSE, and physical activity change, the present analysis will determine if exercise SE constructs are differentially related to different stages of exercise behavior change (i.e., adoption and maintenance).
Physical Activity Interventions Enhance Exercise SE
Convincing evidence has demonstrated that increases in SE are closely related to improvements in exercise behavior. Many physical activity interventions therefore include techniques to enhance SE beliefs (Marcus, King, Clark, Pinto, & Bock, 1996; Sherwood & Jeffery, 2000). Recent meta-analyses confirmed (Ashford, Edmunds, & French, 2010; Williams & French, 2011) that physical activity interventions significantly affect exercise SE (d = 0.26) in healthy adults. Further, many of the intervention components associated with improvements in SE (e.g., action planning and providing instruction) were also related (r = .690, p < .001) to increases in exercise behavior (Williams & French, 2011). Consistent with published reviews on the topic (Baranowski, Anderson, & Carmack, 1998; Lewis et al., 2002; Marcus et al., 1996; Sherwood & Jeffery, 2000; van Stralen, De Vries, Mudde, Bolman, & Lechner, 2009), these meta-analyses included all types of SE beliefs related to exercise (EXSE, BSE, scheduling, goal setting). Therefore, evidence of how interventions distinctly affect EXSE and BSE is currently lacking. Without assessing the effects of interventions on EXSE and BSE separately, researchers cannot determine if these constructs play different roles in changing exercise behavior.
Intervention Techniques Associated With Changes in SE and Physical Activity
In addition to establishing the effectiveness of physical activity interventions on increasing exercise SE, intervention techniques associated with the most positive outcomes (i.e., increases in physical activity behavior and SE, including both EXSE and BSE) must also be identified. Bandura’s (1977) conceptualization dictates that SE beliefs are developed from mastery experience, vicarious learning, verbal persuasion, and affective or physiological states. Accordingly, researchers have incorporated intervention techniques to target these sources of SE information. For example, structured exercise sessions potentially provide mastery experiences and counseling may be a form of verbal persuasion. The current analysis will determine how effectively these techniques increase exercise EXSE and BSE in an intervention setting.
Until recently, few investigations have focused on which attributes of commonly used physical activity interventions most effectively enhance exercise SE. Findings from two meta-analyses (Ashford et al., 2010; Williams & French, 2011) provided valuable information regarding the moderating role of a wide array of methods used in many theory-driven interventions, but key gaps in the literature remain. First, numerous physical activity intervention components (e.g., delivery mode) that have been identified as critical to achieving positive exercise behavior change (Conn et al., 2011) remain unexplored as moderators of SE improvement. Second, evidence has been equivocal in terms of whether methods like goal setting, providing feedback, and offering support (e.g., developing coping strategies and barrier identification through counseling or motivational interviewing) moderate the effects of interventions on SE and physical activity changes (Conn et al., 2011; Williams & French, 2011). Third, previous meta-analyses (Ashford et al., 2010; Williams & French, 2011) have been limited to interventions that explicitly targeted SE beliefs and included nonrandomized studies without control groups, which may have biased results. To minimize such bias, all randomized, controlled physical activity interventions reporting EXSE or BSE outcomes should be assessed to garner accurate effect size estimates of intervention effects on SE beliefs, regardless of whether the interventions specifically targeted SE.
Purpose of the Current Study
The purpose of the current study was to conduct a meta-analysis of randomized controlled physical activity interventions that included physical activity behavior and either EXSE or BSE as outcomes. Our aims were (1) to quantify the impact of interventions designed to increase physical activity in nonclinical populations on EXSE and BSE beliefs and (2) to identify intervention characteristics associated with changes in EXSE, BSE, and physical activity.
Method
Study Identification
A literature search was conducted in October, 2011. The electronic databases PsycInfo, PubMed, SPORTDiscus, and the Cochrane Library (1966–2011) were searched using the terms “self efficacy” AND exercise OR “physical activity” AND intervention OR trial OR program. Reference lists of included articles and relevant review articles were checked to identify additional articles. The first author determined the eligibility of identified studies by scanning titles and abstracts for inclusion criteria (described below). Full articles were obtained for titles that met the inclusion criteria and were independently reviewed by the first and second authors.
Inclusion Criteria
The current review included published, randomized controlled trials conducted in “healthy” adults in which the primary intervention being evaluated was designed to increase physical activity (including interventions that involved structured exercise sessions and those base on nonexercise approaches, such as physical activity education). Studies reporting change (or pre- and postscores) in EXSE or BSE and physical activity were eligible for inclusion, regardless of whether the intervention specifically targeted SE. Studies must have used EXSE assessments that indexed the participants’ level of confidence to fulfill the exercise prescription specified by the intervention. The BSE scales must have measured perceived confidence to exercise despite numerous challenging situations (e.g., bad weather, schedule conflict, etc.). Studies also must have used either a validated, reliable self-report index of physical activity or an objective measure of physical activity (e.g., pedometer or accelerometer). Further, included studies needed to contain relevant information required for calculating effect sizes for EXSE or BSE change and exercise behavior change (if the study met all inclusion criteria but did not provide adequate information to calculate effect sizes, the first author of the article was contacted to obtain this information).
Exclusion Criteria
Quasi-experimental, qualitative studies, surveys, case– control designs, case reports, prospective cohort studies, and crosssectional studies were excluded. Conference proceedings, unpublished studies, and articles written in any language other than English were not included.
Studies specifically targeting clinically defined populations, such as those recruiting participants on the basis of being obese or having a preexisting medical condition, were excluded. Studies involving adolescents or athletes also were not included. Trials were ineligible if interventions substantially (>25% of time) targeted nonexercise behaviors (e.g., diet). Studies were ineligible if the SE assessment did not explicitly index EXSE or BSE at baseline and within 1 week of the conclusion of the intervention. Studies using measures of physical activity that have not been validated or EXSE and BSE measures that were not consistent with Bandura’s (1997) conceptualization of SE and recommendations for creating SE assessments were excluded.
Data Extraction and Quality Assessment
Data were extracted from selected articles using a standardized coding form (data extraction and coding forms are available from the authors upon request). Studies were described in terms of author, publication year, population, and intervention characteristics. Specifically, studies were coded with respect to age (young, 18–40 years; middle-aged, 41–64; and old, ≥65 years), gender (high female, >50% female sample; and high male, >50% male sample), and whether participants were described as regular exercisers (met or exceeded Centers for Disease Control and Prevention/ American College of Sports Medicine [ACSM] guidelines; Pate et al., 1995) or sedentary/inactive (reported little to no physical activity). Intervention characteristics were also coded, including duration (short, ≤2 months; medium, 3–6 months; and long, ≥6 months), delivery mode (face-to-face or mediated through telephone, Internet, or mail), amount of contact participants received (minimal, ≤3 contacts; or frequent, ≥4 contacts), the required regular use of exercise logs (used or not used), the inclusion of structured exercise sessions, such as personal training, walking groups, or fitness classes (yes or no), the type of exercise goal provided (tailored to the individual or standardized for all participants), and whether support such as counseling or motivational interviewing was provided throughout the intervention to maintain participation (yes or no). Selected study characteristics are summarized in Table 1.
Table 1.
Description of Studies Included in the Meta-Analysis, by Year
| First author and year |
N | Agea | Gender (% female) |
Sedentary | Self-efficacy type |
Duration (weeks) |
Delivery | Contact | Logs | Structured exercise |
Exercise prescription |
Tailored goal |
Support |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Andersson (2011) | 40 (26 Trt; 14 Control) | 29 (8.93) | 68% | Yes | EXSE | 2 | Mediated | Minimal | Yes | No | No | No | No |
| Irvine (2011) | 211 (96 Trt; 115 Control) | 45 (9.7) | 42.20% | Yes | EXSE | 4 | Mediated | Frequent | No | No | Yes | No | Yes |
| Estabrooks (2011) | 85 (44 Trt; 41 Control) | 48.8 (11.9) | 61% | Yes | BSE | 12 | Face | Minimal | No | Yes | Yes | No | No |
| Armitage (2010) | 68 (32 Trt; 36 Control) | 27.5 (12.7) | 48% | No | EXSE | 4 | Face | Minimal | No | No | No | No | No |
| Morgan (2010) | 29 (14 Trt; 15 Control) | 59.8 (5.8) | 76% | Yes | EXSE | 15 | Face | Frequent | Yes | Yes | Yes | Yes | Yes |
| Crain (2010) | 982 (495 Trt; 487 Control) | 57.1 (5.1) | 72.40% | Yes | BSE | 104 | Mediated | Frequent | No | No | No | No | Yes |
| Wadsworth (2010) | 71 (34 Trt; 37 Control) | College age* | 100% | Yes | BSE | 24 | Mediated | Frequent | No | No | No | No | Yes |
| Lane (2010) | 176 (85 Trt; 91 Control) | 21–49 | 100% | Yes | EXSE | 6 | Mediated | Minimal | No | No | No | No | No |
| Opdenacker (2009) | 101 (53 Trt; 48 Control) | 53.7 (11.3) | 100% | No | BSE | 24 | Face | Frequent | Yes | No | Yes | Yes | Yes |
| Latimer (2008) | 169 (113 Trt; 56 Control) | 47.4 (12.0) | 76.10% | Yes | EXSE | 9 | Mediated | Frequent | No | No | Yes | No | No |
| Greaney (2008) | 966 (470 Trt; 496 Control) | 75 (6.7) | 72% | No | BSE | 104 | Mediated | Frequent | No | No | Yes | No | Yes |
| Resnick (2008) | 103 (64 Trt; 39 Control) | 73 (8.2) | 81% | No | BSE | 15 | Face | Frequent | No | Yes | Yes | No | Yes |
| Bennett (2008) | 72 (35 Trt; 37 Control) | 58.5 (10.5) | 90% | Yes | BSE | 24 | Mediated | Frequent | No | No | Yes | Yes | Yes |
| Blanchard (2007) | 98 (54 Trt; 44 Control) | 47.3 | 69.20% | Yes | EXSE | 12 | Face | Frequent | No | No | Yes | Yes | Yes |
| Elavsky (2007) | 86 (52 Trt; 34 Control) | 44.9 (3.6) | 100% | Yes | EXSE | 16 | Face | Frequent | Yes | Yes | Yes | Yes | Yes |
| Marcus (2007) | 225 (156 Trt; 69 control) | 44.5 | 82% | Yes | EXSE | 52 | Mediated | Frequent | Yes | No | Yes | Yes | No |
| Resnick (2002) | 17 (10 Trt; 7 Control) | 88 (3.7) | 100% | Yes | BSE | 24 | Face | Frequent | Yes | No | Yes | No | No |
| Hager (2002) | 269 (134 Trt; 135 Control) | 42 (6.4) | 56% | No | BSE | 6 | Mediated | Frequent | No | No | No | No | Yes |
| Marcus (1998) | 150 (78 Trt; 72 Control) | 44.3 (10.2) | 78% | Yes | EXSE | 24 | Mediated | Frequent | No | No | Yes | Yes | No |
| Cardinal (1997) | 23 (12 Trt; 11 Control) | 33.5 (8.7) | 100%, | No | BSE | 2 | Face | Frequent | No | No | No | No | No |
Note. Trt = treatment: EXSE = exercise self-efficacy: BSE = barrier self-efficacy.
Values are means with standard deviation in parentheses.
Mean age and standard deviation not reported.
To calculate estimates of intervention effects on EXSE, BSE, and physical activity behavior, pre- and postmeans, and standard deviations were recorded (where pre- and postmeans were missing, mean changes and F statistics were used). In the case of multiple postintervention measurement time points, only measurements taken immediately following the end of the intervention were abstracted. For studies implementing more than one treatment arm, only data related to the current review were used (e.g., if a physical activity intervention, a control intervention, and a relaxation intervention were conducted, only data from the first two were used). If more than one intervention arm met criteria for inclusion, data were combined to create pooled estimates. For the three studies that included both EXSE and BSE as outcome measures, only an effect size for EXSE was included in the meta-analysis to avoid violating the assumption of independence. EXSE was chosen because the present meta-analysis focused on interventions to promote physical activity adoption in mostly sedentary or inactive individuals and EXSE appears to play a more important role in exercise adoption than BSE.
Study design quality was assessed independently by two of the authors (TJH and KRM) in terms of adequacy of reporting randomization, blinding of outcome assessment, and proportion of participants lost to follow-up using the previously validated 5-point Jadad scale (see Jadad et al., 1996 for a full description). Any disagreements were resolved by discussion.
Data Synthesis and Analysis
Effect sizes, using Hedge’s g, were estimated using pre- and posttest means, standard deviations, and group n, or next through the use of mean differences between an intervention and a control group and associated standard deviations and F ratio. Two effect sizes were calculated from each study (one for either EXSE or BSE and one for physical activity). Random-effects and mixed effects modeling were selected for the overall and moderator analyses, respectively, to account for variance between studies due to differing populations and study design. Three separate random effects models were used to assess intervention effects on EXSE, BSE, and physical activity behavior. Q-statistics were calculated for each model to assess heterogeneity between studies. Subsequent analyses were conducted on subgroups of studies to explore the effects of potential moderating variables. Potential publication bias was indexed using a fail-safe N calculation and visual examination of funnel plots and fill and trim analyses (Duval & Tweedie, 2000). All analyses were conducted using Comprehensive Meta-Analysis software (Version 2, Biostat, Englewood, NJ).
Results
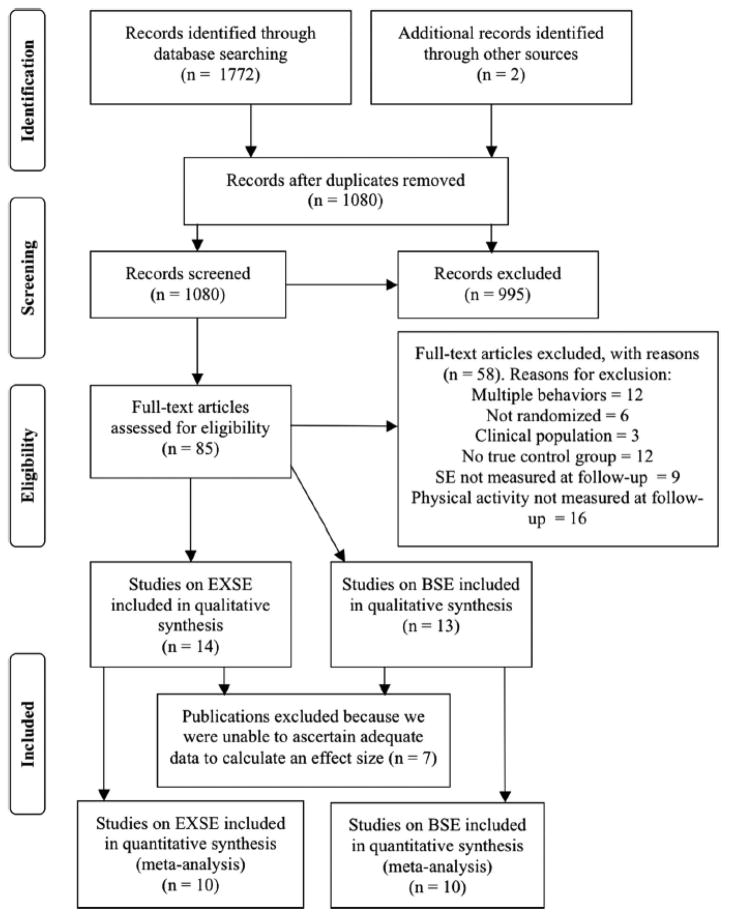
The search strategy described above identified a total of 1,772 potentially relevant articles. Of these, 694 results were excluded for duplicate records (e.g., the same article appearing in both the Cochrane Library and Psych Info search), 995 were excluded after title/abstract review, and an additional 58 were excluded after full-text review (see Figure 1), resulting in 14 studies on EXSE and 13 studies on BSE being included in the current study. After seven studies were excluded from the meta-analysis because of inadequate information to ascertain an effect size, a total of 20 studies (10 for EXSE and 10 for BSE) with a total of 3,941 participants were included in the current meta-analyses (included studies are indicated by an asterisk in the reference list).1
Figure 1.
PRISMA flowchart for study inclusion.
Description of Included Articles
The age of participants in the included studies ranged from 18 to 94 years with a mean of 45.5 years (SD = 16.9). The majority of the participants (62.9%) included in the meta-analyses were middle-aged, and 9.59% were categorized as young adults and 27.6% were older adults. In addition, the majority (90%) of the included studies reported mostly female samples. Of the two studies that reported a majority male sample, the proportion of females included was near 50%. Fourteen of the studies reported >60% Caucasian samples, one reported a >60% African American sample (Resnick, Luisi, & Vogel, 2008), and five did not provide details on race. All participants were “healthy” (i.e., no clinical reason to be included in intervention). Sixty-one percent were described as sedentary or inactive prior to involvement in the intervention.
The duration of the interventions included in the current review varied greatly, with a range of 2 to 104 weeks, with a mean duration of 24.2 weeks (SD = 29.7). Six of the interventions lasted between 2 weeks and 2 months, 11 of the interventions were of medium length (3–6 months), and three of the interventions were longer than 6 months. All of the outcomes of interest were assessed within 1 week of the end of the intervention. Notably, outcome measures were typically administered using the same channels through which interventions were delivered (i.e., either in person or through a mediated method). Only four of the interventions were conducted in a group setting, and the remaining 16 interventions were administered individually. Though most interventions included frequent participant contact (>6 interactions), four interventions limited contact to one intervention session that included baseline testing and two subsequent assessment time points.
The majority (85%) of the studies evaluated interventions that used multiple behavioral change techniques. Thirty percent of the interventions required the use of daily activity logs to enhance self-monitoring behaviors, and 20% included structured exercise sessions designed to increase adherence to the intervention and to teach participants how to exercise appropriately. Additionally, 65% of the interventions gave participants a specific exercise prescription. Of the interventions that specified an exercise prescription, 58% developed tailored goals for each individual, whereas the remainder designated the ACSM physical activity guidelines (five used the post-2008 guidelines) as the prescription. Although 35% of the interventions recommended that participants engage in moderate to vigorous intensity physical activity, the remainder did not specify the intensity of exercise that participants should perform. Other common intervention characteristics included educational sessions that focused on the benefits of physical activity, the risks of a sedentary lifestyle, strategies to become and remain active (provided by 90% of the included studies), and support to maintain or increase participation, which was provided by 55% of the interventions. Of the included interventions, 65% were compared with no-treatment or standard care control groups, whereas 35% of interventions were compared with active control groups that received an alternative treatment (e.g., neutral messages about physical activity) that were not designed to increase physical activity behavior.
Study Quality
Study quality scores computed using the 5-point Jadad scale (Jadad et al., 1996) ranged from 1 to 5, and the mean Jadad score for the included studies was 2.2 ± 0.89. Although all of the studies were randomized trials, only 30% adequately described appropriate randomization procedures, and none of the studies were described as double-blind. Eighty percent of the studies adequately described dropouts and withdrawals. The interclass correlation coefficient for Jadad scores between the two reviewers was α = .97.
Meta-Analyses Results
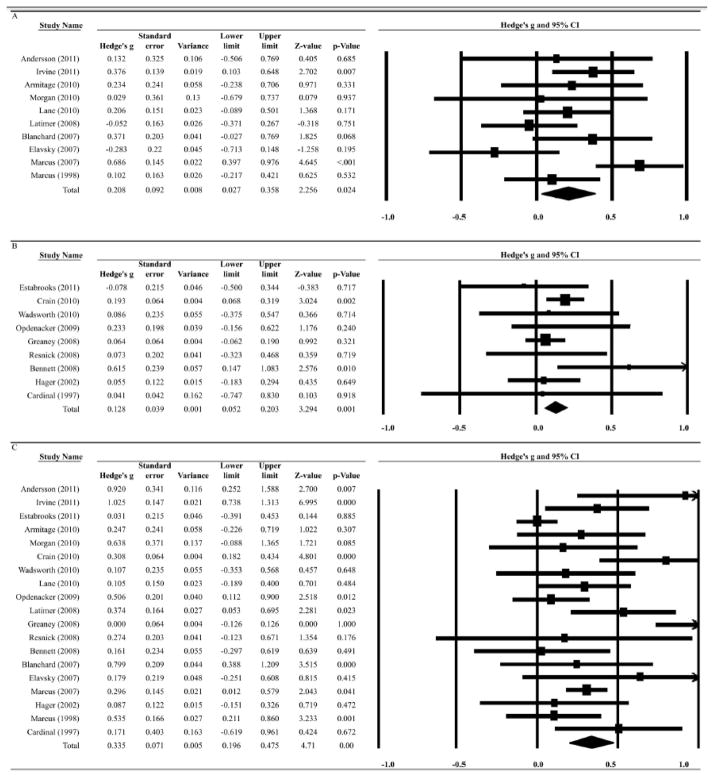
The effect of interventions designed to increase physical activity behavior on EXSE varied by study, from g = −0.283 to 0.686 (Figure 2A). The mean of the distribution of effects, weighted by sample size, indicated a significant small effect of physical activity interventions on EXSE, g = 0.208, 95% CI [0.027, 0.388], p < .05.
Figure 2.
Forest plots for studies included in the EXSE (A), BSE (B), and physical activity (C) meta-analyses, by publication year. “Study weight indicated by size of marker in the Forest plot. Total effect size indicated by diamond.
There was also a small but significant effect of interventions on BSE, with g = 0.170, 95% CI [0.015, 0.324], p < .05. When an outlier (Resnick, 2002) with an extreme effect size (d = 2.60) was removed from the analysis because it significantly increased the heterogeneity of the sample, the effect size on BSE dropped to 0.128, 95% CI [0.05, 0.20], with a range of −0.078 to 0.615 (Figure 2B). This study was omitted from all subsequent analyses.
Included interventions had a small to moderate effect on physical activity behavior, with g = 0.335, 95% CI [0.196, 0.475], p < .001, and an effect size range of 0 to 1.025 (Figure 2C). These results suggest that participants receiving these interventions reported significantly higher EXSE, BSE, and physical activity levels compared with participants in the control conditions.
Homogeneity analyses revealed that that variance in effect sizes for each of the models, EXSE (Q = 20.61, p < .05), BSE (Q = 7.909 p < .001), and physical activity (Q = 65.40, p < .001), differed significantly from that explained by random sampling error alone. Therefore, moderator analyses were conducted separately for EXSE, BSE, and physical activity to systematically search for possible sources of heterogeneity.
Moderator Analyses Results
Separate moderator analyses were conducted for each outcome variable of interest (EXSE, BSE, and physical activity) to enable comparisons of which population and intervention characteristics were associated with change in these constructs (see Table 2). Not all of the selected participant and intervention characteristics could be explored as potential moderators for EXSE, BSE, and physical activity change because an inadequate number of studies (≤1) including these techniques were available (indicated by dashes in Table 2).
Table 2.
Moderator Effects Across EXSE, BSE, and Physical Activity
| EXSE
|
BSE
|
PA
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| d | k | n | P | d | k | n | P | d | k | n | P | |
| Participant characteristics | ||||||||||||
| Age | ||||||||||||
| 18–40 | 0.203 | 3 | 284 | 0.088 | 0.075 | 2 | 94 | 0.713 | 0.232 | 5 | 378 | 0.058 |
| 41–65 | 0.202 | 7 | 968 | 0.115 | 0.154 | 4 | 1437 | 0.004 | 0.421 | 11 | 2405 | < 0.001 |
| >65 | — | — | — | — | 0.191 | 3 | 1141 | 0.197 | 0.034 | 3 | 1141 | 0.568 |
| Gender | ||||||||||||
| High female (>50%) | 0.172 | 8 | 973 | 0.138 | — | — | — | — | 0.276 | 17 | 3645 | < 0.001 |
| High male (≥50%) | 0.340 | 2 | 279 | 0.005 | — | — | — | — | 0.659 | 2 | 279 | 0.090 |
| Baseline activity | ||||||||||||
| Regular exercisers | — | — | — | — | 0.074 | 4 | 1462 | 0.156 | 0.143 | 6 | 1530 | 0.072 |
| Sedentary or inactive | — | — | — | — | 0.193 | 5 | 1210 | 0.076 | 0.403 | 13 | 2394 | < 0.001 |
| Intervention characteristics | ||||||||||||
| Duration | ||||||||||||
| ≤ 2 months | 0.276 | 4 | 495 | 0.002 | 0.054 | 2 | 292 | 0.641 | 0.419 | 6 | 787 | 0.037 |
| 2–6 months | 0.040 | 5 | 532 | 0.702 | 0.174 | 5 | 432 | 0.117 | 0.361 | 10 | 964 | < 0.001 |
| >6 months | — | — | — | — | 0.129 | 2 | 1948 | 0.047 | 0.190 | 3 | 2173 | 0.108 |
| Delivery | ||||||||||||
| Face to face | 0.098 | 4 | 0.543 | 0.081 | 4 | 312 | 0.476 | 0.356 | 8 | 593 | < 0.001 | |
| Mediated | 0.259 | 6 | 0.023 | 0.142 | 5 | 2360 | 0.021 | 0.328 | 11 | 3631 | < 0.001 | |
| Contact | ||||||||||||
| Minimal | 0.203 | 3 | 284 | 0.088 | 0.163 | 4 | 1161 | 0.005 | 0.247 | 7 | 1445 | < 0.001 |
| Frequent | 0.202 | 7 | 968 | 0.115 | 0.128 | 5 | 1511 | 0.081 | 0.391 | 12 | 2479 | < 0.001 |
| Exercise logs | ||||||||||||
| Used | 0.164 | 4 | 380 | 0.546 | — | — | — | — | 0.404 | 5 | 481 | < 0.001 |
| Not used | 0.202 | 6 | 872 | 0.003 | — | — | — | — | 0.306 | 14 | 3443 | < 0.001 |
| Structured exercise | ||||||||||||
| Yes | 0.199 | 2 | 115 | 0.289 | — | — | — | — | 0.287 | 3 | 218 | 0.038 |
| No | 0.272 | 8 | 1137 | 0.002 | — | — | — | — | 0.340 | 16 | 3706 | < 0.001 |
| Exercise goal type | ||||||||||||
| Tailored | 0.209 | 5 | 588 | 0.248 | 0.401 | 2 | 173 | 0.034 | 0.428 | 7 | 761 | < 0.001 |
| General | 0.170 | 2 | 380 | 0.425 | 0.054 | 3 | 1114 | 0.360 | 0.342 | 5 | 1534 | 0.104 |
| Support | ||||||||||||
| Yes | 0.159 | 4 | 424 | 0.340 | 0.110 | 6 | 1582 | 0.051 | 0.365 | 10 | 2106 | < 0.001 |
| No | 0.231 | 6 | 828 | 0.059 | 0.168 | 3 | 1090 | 0.005 | 0.305 | 9 | 1818 | 0.005 |
Note, d, k, n, and p are moderator variables used. Bolded values denote significance. — = an inadequate number of studies (≤ 1) were available to conduct a moderator analysis. EXSE = exercise self-efficacy; BSE = barrier self-efficacy; PA = physical activity.
Age
Middle-age was associated with significant effects on BSE (g = 0.154, p < .004). Similarly, interventions increased physical activity behavior in middle-age adults to a reliably greater degree than in young and old adults, mixed effects Q(18) = 13.27, p < .001.
Gender
Increases in EXSE were associated with samples in which the majority of participants were men (g=0.340, p<.005). In contrast, significant increases in physical activity were associated with samples that had a higher percentage of women (g = 0.276, p < .001).
Activity level
Interventions on sedentary or inactive participants increased physical activity behavior to a reliably greater degree than interventions that included previous exercisers, mixed effects Q(18) = 4.97, p = .026.
Intervention duration
Short interventions significantly increased EXSE (g = 0.276, p = .002). Only long interventions were associated with gains in BSE (g = 0.129, p < .05). Short and medium length interventions were associated with significant increases in physical activity behavior, with effects of g = 0.419, p = .037 and g = 0.361, p < .001, respectively.
Intervention delivery
Mediated interventions significantly increased EXSE (g = 0.259, p = .023). Mediated interventions and interventions delivered face-to-face resulted in changes in physical activity, with effects of g = 0.328, p < .001 and g = 0.356, p < .001, respectively.
Contact
Comparatively less contact with participants resulted in increased BSE (g = 0.163, p = .005). Interventions that frequently contacted participants and minimal contact interventions increased physical activity behavior, with effects of g = 0.391, p < .001 and g = 0.247, p < .001, respectively.
Exercise logs
Interventions that did not require participants to use exercise logs elevated EXSE (g = 0.202, p < .05). Interventions that did require the use of exercise logs and those that did not require the use of logs increased physical activity, with effects of g = 0.404, p < .001 and g = 0.306, p < .001, respectively.
Structured exercise
Interventions that did not include structured exercise improved EXSE to a reliably greater degree than interventions that required participants to attend structured exercise sessions, mixed effects Q(9) = 5.13, p = .024. Interventions that did not include structured exercise and those with structured exercise increased physical activity, with effects of g = 0.340, p = .038 and g = 0.287, p < .001, respectively.
Exercise goals
Tailoring exercise goals to each participant improved BSE (g = 0.401, p = .034) and physical activity behavior (g = 0.428, p < .001).
Support
Interventions that did not provide support (i.e., counseling, motivational messages) increased BSE (g = 0.168, p < .005). Both interventions that provided support and those that did not provide support increased physical activity, with effects of g = 0.365, p < .001 and g = 0.305, p < .005, respectively.
Publication Bias
Funnel plots (not shown) for each of the overall meta-analyses all displayed a scattering of plots across the horizontal axis. When filled (using fill and trim analysis for publication bias; Duval & Tweedie, 2000), the plots demonstrated the potential for missing studies with smaller sample sizes and smaller effects. Filling in the plot with symmetrical studies demonstrating negative results titrated the effect slightly to g = 0.177 on physical activity behavior and negligibly on EXSE and BSE. The fail-safe N calculation suggested that 22, 11, and 327 studies would be required to bring the current effect of interventions on EXSE, BSE, and physical activity behavior, respectively, to non significance, suggesting that the effect is not likely to be affected by unpublished null results.
Discussion
The primary aim of the present meta-analysis was to quantify the effectiveness of interventions to increase physical activity among healthy adults at improving EXSE and BSE. We also sought to identify participant and intervention characteristics associated with positive changes in EXSE, BSE, and physical activity. Interventions to increase physical activity had a small but significant effect on BSE and a slightly larger effect on EXSE. These interventions also had a moderate positive effect on physical activity behavior, which aligns with the findings of Conn et al. (2011). Moderator analyses identified that positive changes in EXSE and physical activity occurred when interventions were short and did not include structured exercise sessions. Conversely, longer interventions led to increases in BSE. Interventions that provided tailored exercise goals successfully improved BSE and physical activity behavior.
A somewhat counterintuitive finding was that interventions that increased physical activity and were the most effective at changing exercise SE beliefs did not include several common intervention components, such as face-to-face delivery, frequent contact, daily exercise logs, and support. The presence of these intervention techniques was also associated with moderate changes in physical activity, but no changes in exercise SE. Our findings illustrate that interventions distinctly affect EXSE and BSE, and that different intervention approaches are associated with EXSE and BSE improvements. Further, although the presence of certain intervention components produced initial enhancements in physical activity, interventions without these techniques led to higher activity levels as well as increased exercise SE. Because high exercise SE predicts long-term behavior change (McAuley, Jerome, Elavsky, Marquez, & Ramsey, 2003; Sniehotta, Scholz, & Schwarzer, 2005), omitting certain intervention components may yield more lasting physical activity changes.
Physical Activity Interventions Differentially Affect EXSE and BSE
Our data support that EXSE and BSE represent distinct constructs and are differentially influenced by intervention approaches. Although interventions enhanced both SE beliefs, the magnitude of the effect on EXSE was greater than that on BSE. Short-duration interventions increased EXSE, but only longer interventions interventions altered BSE. These findings substantiate McAuley, Jerome, Elavsky, et al.’s (2003) suggestion that BSE represents a more stable belief, whereas EXSE is more readily modified, particularly during early phases of an intervention.
As posited by Blanchard et al. (2007), the observed temporal differences in EXSE and BSE change may indicate that EXSE plays an important role in exercise adoption and BSE is involved in the maintenance of exercise behavior. Considering how EXSE and BSE are conceptualized and the circumstances surrounding measurement time points, these results should be expected. For example, sedentary individuals likely possess low EXSE upon entering intervention programs because they are unaccustomed to exercising and do not have mastery experiences to draw from (McAuley, Szabo, Gothe, & Olson, 2011). Enrollment in even a short-term intervention can provide exercise experiences that can influence EXSE (Bandura, 1998; McAuley, Jerome, Elavsky, et al., 2003). The frequency of exercise directly relates to EXSE (Blanchard et al., 2007; Sherwood & Jeffery, 2000); thus, individuals who transition from a sedentary or inactive lifestyle to participating in regular physical activity should undergo initial improvements in EXSE. Because of the malleability of EXSE beliefs early in interventions, care should be taken to provide abundant positive exercise mastery experiences during the preliminary intervention phase.
BSE, on the other hand, appears to remain stable until individuals have integrated regular physical activity into their daily routines and have learned to cope with various barriers to exercise (e.g., inclement weather, fatigue, etc.). Acquiring successful mastery experiences of overcoming common barriers takes time, which is reflected in the observed temporal changes of BSE. Though enhancements in BSE were observed in the longest duration interventions, these changes appear to be too small to effectively maintain physical activity in the current sample. Based on a combination of the current findings and previous results, EXSE should be targeted during the exercise adoption stage and BSE should be emphasized when attempting to maintain long-term exercise behavior change.
Participant Characteristics Are Related to Increases in SE and Physical Activity
Age
Interventions enhanced BSE and physical activity among healthy, middle-aged adults. A potential explanation for this finding is that barriers to exercise that are most salient to middle-aged adults can be more readily addressed and overcome with intervention, compared with barriers typically reported by younger and older adults (Ebben & Brudzynski, 2008). Middle-aged adults rank lack of time due to varying work schedules and responsibilities as their most significant barrier to exercise. Health concerns, such as arthritis, are more prominent barriers among older adults (Lattimore et al., 2011), whereas younger adults indicate “laziness” and “having other priorities” prevents them from exercising regularly (Ebben & Brudzynski, 2008). Interventions to increase physical activity commonly teach participants how to integrate exercise into their daily routines, but providing support for overcoming health concerns and changing priorities is less prevalent. As such, these results demonstrate that interventions must address a wider range of exercise barriers to change exercise behavior across the life span.
Activity level
Prior meta-analytic findings indicate that interventions on sedentary or inactive participants produce larger effects on physical activity, compared with interventions on previously active adults (Conn et al., 2011). The present data are congruent with the finding that baseline activity level moderates intervention effects on physical activity. Interventions appear to be more successful at getting people who do not regularly exercise to add modest amounts of physical activity to their routines than increasing exercise levels of active people. Activity status before the intervention was not related to BSE changes likely because of the stable nature of BSE beliefs. All but one of the studies using EXSE as an outcome measure involved sedentary or inactive participants, which prohibited a moderator analysis. Future research is required to determine whether baseline activity status impacts the effect of interventions on EXSE.
Including Specific Intervention Components Improves SE and Physical Activity
Duration
Interventions that lasted between 2 weeks and 2 months resulted in positive changes in EXSE and physical activity. A multitude of studies have demonstrated that EXSE beliefs typically vary the most during the initial stage of an intervention and predict early levels of physical activity (Blanchard et al., 2007; Hughes et al., 2009; McAuley, Jerome, Elavsky, et al., 2003). Accordingly, EXSE appears to underlie exercise adoption. The effect of interventions on EXSE seems to wane after participants learn to exercise properly and develop exercise experiences.
Exercise goals
The provision of tailored or individualized exercise goals, as opposed to a standard exercise goal given to an entire intervention group (e.g., exercise at moderate intensity for 30 min a day, 5 days a week), was associated with gains in BSE and physical activity. Though tailoring intervention components represents a common behavior-change strategy, previous research indicates tailored interventions provide little-to-no additional effect on physical activity change than standardized approaches (Conn et al., 2011; Noar, Benac, & Harris, 2007; Williams et al., 2011). However, few studies have specifically assessed the impact of tailored goal-setting compared with standardized goal-setting in a physical activity intervention context (Noar et al., 2007). Limited evidence suggests standardized, group goals are most effective when participants are already active and have high levels of exercise SE (Burke, Shapcott, Carron, Bradshaw, & Estabrooks, 2010), in which case, sedentary or inactive participants with low SE beliefs should benefit more from individualized goals. Our results affirm that individualized goals result in higher BSE and physical activity levels in an intervention setting composed of sedentary and inactive individuals. To fulfill standardized exercise goals, sedentary and inactive participants must adopt recommended exercise levels immediately, which may seem like an overwhelming task and fail to motivate change. Conversely, tailored exercise goals can address current activity levels, work schedules, and other perceived barriers to facilitate behavior change.
Excluding Certain Intervention Techniques Increases SE Beliefs and Physical Activity
Delivery
In contrast to prior findings (Conn et al., 2011), mode of intervention delivery did not significantly moderate the effects of interventions on physical activity. Face-to-face and mediated delivery methods both increased physical activity. Face to- face interventions were not associated with improvements in exercise SE beliefs, but increases in EXSE and BSE were observed when intervention delivery was mediated by phone, mail, or website. Face-to-face delivery may effectively improve physical activity because participants’ pay more attention to intervention messages given in person. However, face-to-face interventions require participants to attend sessions at intervention sites, which may increase perceptions of barriers. Mediated interventions enable participants to receive intervention messages without interfering with work schedules or involving travel expenditures, leading to higher levels of BSE.
Many of the interventions delivered in person involved structured exercise sessions (Elavsky & Mcauley, 2007; Estabrooks et al., 2011; Morgan, Tobar, & Snyder, 2010; Resnick et al., 2008), making it difficult to disentangle the effects of delivery mode and structured exercise on EXSE. Structured exercise or face-to-face interventions may make participants feel dependent on intervention programs, whereas learning to exercise regularly at home without supervision may provide more meaningful mastery experiences that increase EXSE.
Contact and support
Though frequency of contact and presence of support did not moderate physical activity changes, minimal contact and the absence of support were associated with higher BSE. Support strategies and contact typically entail verbal persuasion approaches, which were implicated by Bandura (1977) as one of the major sources of SE beliefs. These data corroborate previous findings (Ashford et al., 2010) that verbal persuasion does not improve SE among healthy adults in an intervention context.
Exercise logs
Our findings contribute to mounting evidence that daily monitoring of physical activity does not improve exercise SE beliefs (Williams & French, 2011). Keeping daily exercise logs resulted in physical activity changes. However, physical activity and EXSE improvements were observed when logs were not used. Prompt self-monitoring represents an effective behavioral approach for increasing physical activity levels (Michie, Abraham, Whittington, McAteer, & Gupta, 2009). Perhaps counterintuitively, recording daily exercise did not lead to similar improvements in EXSE. Daily exercise logs may provide negative feedback even when participants are exercising more often, but are failing to attain their exercise goals. Such negative feedback may preclude the development of positive EXSE beliefs, particularly during the exercise adoption stage. Accordingly, exercise logs should be implemented with caution, because individuals with low EXSE set lower exercise goals (Dishman, Vandenberg, Motl, Wilson, & DeJoy, 2010), report more negative feelings about exercise (McAuley, Szabo et al., 2011), and are less successful at realizing plans to exercise (Luszczynska, Schwarzer, Lippke, & Mazurkiewicz, 2011). In sum, individuals with low EXSE are unlikely to maintain regular physical activity routines despite experiencing initial increases in activity. Logs may be beneficial when used after the exercise adoption phase when EXSE beliefs are higher.
Structured exercise
Interventions that did not include structured exercise sessions enhanced EXSE and physical activity. Structured exercise sessions require participants to exercise at specific locations at designated times and limit exercise options, which leads to less change in physical activity. This contrasts with Conn et al.’s (2011) assertion that the presence of supervised exercise sessions is associated with better physical activity outcomes, but supports previous research illustrating home-based interventions are just as, or even more effective, at increasing physical activity, compared with center-based approaches (King, Haskell, Taylor, Kraemer, & DeBusk, 1991). Structured exercise sessions may fail to change EXSE because participants are not provided with opportunities to build mastery experiences exercising without a trainer and feel reliant on the program. Interventions requiring participants to select their own mode of exercise and perform without trainers give people more autonomy (Ekkekakis, 2009) and make them actively engage in learning how to incorporate exercise into their routines, resulting in higher EXSE and physical activity levels. Alternatively, participants in structured exercise interventions may experience increases in EXSE but report lower postintervention EXSE because they are more concerned about their abilities to exercise outside of a structured setting, compared with individuals who trained without supervision.
Another viable explanation for why interventions without structured exercise components increase EXSE is that unsupervised individuals may misjudge the intensity of their workouts, leading to inflated feelings of EXSE. Trainers often teach participants how to exercise with proper form and to maintain prescribed exercise intensity. EXSE may remain low in structured exercise settings when individuals unfamiliar with physical activity learn how difficult it is to exercise at the prescribed intensity. Participants with little exercise experience who do not participate in a structured program do not receive feedback about their exercise form or intensity. Thus, these participants could unknowingly exercise at a lower intensity than prescribed or perform exercises with improper form and develop a false sense of confidence regarding their ability to complete their workouts. None of the explanations for why the absence of structured exercise sessions leads to improved EXSE and physical activity can be confirmed with the current data. Future research should be directed to resolving the basis of these findings.
Strengths and Limitations
To our knowledge, the current study is the only meta-analysis of randomized controlled trials investigating the independent effects of interventions to promote physical activity on EXSE and BSE. This investigation established that interventions to increase physical activity differentially affect EXSE and BSE. A second novel contribution of the present study included delineating the most effective participant characteristics and intervention components for improving EXSE, BSE, and physical activity. We found little evidence of publication bias. Therefore, the effects observed in this meta-analysis are likely a good estimate of the overall mean effects of interventions on EXSE, BSE, and physical activity.
Limitations of the current study involved the relatively small number of articles included in the meta-analysis and the presence of significant heterogeneity even after moderator analyses. Therefore, pooled effect sizes should be interpreted with caution. The current meta-analysis provides novel, preliminary evidence that different intervention techniques should be used to target EXSE and BSE. Notably, the list of intervention components and participant participant characteristics (e.g., gender) explored in the current analysis was not exhaustive due to the exclusion of studies not meeting our inclusion criteria and an inadequate amount of published information. The inability to comprehensively assess the influence of all intervention and participant characteristics prohibits making definitive recommendations regarding which intervention components should be included or avoided in future interventions.
Although there was minimal evidence of publication bias in the current review, because studies with small or nonsignificant effects are less likely to be published (Begg, 1994), the potential influence of publication bias cannot be excluded. Fail-safe N analyses indicated that a large number of studies with null results would be required to significantly adjust the current effects to nonsignificant. Fill-and-trim analyses revealed that the effects were reduced negligibly when the funnel plot was filled with studies demonstrating symmetrical negative effects.
Recommendations and Future Directions
Interventions designed to promote physical activity should target SE to enact lasting behavioral changes. Many interventions to increase physical activity improve SE beliefs and physical activity, but the magnitude of success among these interventions remains variable. As demonstrated by the current analysis, inconsistencies in SE and physical activity change can be explained by interventions using a range of different approaches, some of which may actually impede the development of SE or fail to target the appropriate exercise SE belief.
Interventions should emphasize learning to exercise in participants’ typical environments and teach strategies to incorporate exercise into daily routines without supervision. Such strategies encourage participants to acquire mastery experiences independently, resulting in SE gains. Interventions involving frequent contact, support, and structured exercise sessions are likely less successful at improving SE because they foster reliance on interventions to maintain behavior change. Minimizing interventionist contact and support enables participants to build mastery experiences in an ecologically valid context. Even more effort should be devoted to instilling a sense of independence from the intervention when treatments are delivered face-to-face, because participants do not appear to increase EXSE or BSE when they have to attend intervention sites to receive treatment. Reducing contact and support should not only enhance SE beliefs and resultant physical activity levels, but also improve the cost-effectiveness of interventions. In sum, this meta-analysis supports the notion that EXSE and BSE are differentially improved by interventions to promote physical activity and can be targeted using specific techniques. Interventionists must implement techniques that not only increase physical activity, but also improve EXSE and BSE to produce lasting behavior changes.
Contributor Information
Torrance J. Higgins, Department of Applied Physiology & Kinesiology, University of Florida
Kathryn R. Middleton, Department of Clinical & Health Psychology, University of Florida
Larry Winner, Department of Statistics, University of Florida.
Christopher M. Janelle, Department of Applied Physiology & Kinesiology, University of Florida
Kathryn R. Middleton, Department of Psychiatry & Human Behavior, Alpert Medical School of Brown University & The Miriam Hospital
References
- *.Andersson EK, Moss TP. Imagery and implementation intention: A randomised controlled trial of interventions to increase exercise behaviour in the general population. Psychology of Sport and Exercise. 2011;12(2):63–70. [Google Scholar]
- *.Armitage CJ, Arden MA. A volitional help sheet to increase physical activity in people with low socioeconomic status: A randomised exploratory trial. Psychology & health. 2010;25(10):1129–45. doi: 10.1080/08870440903121638. [DOI] [PubMed] [Google Scholar]
- Ashford S, Edmunds J, French DP. What is the best way to change self-efficacy to promote lifestyle and recreational physical activity? A systematic review with meta-analysis. British journal of health psychology. 2010;15(2):265–88. doi: 10.1348/135910709X461752. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychological review. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-Efficacy: The Exercise of Control. New York: Freeman; 1997. [Google Scholar]
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychology & Health. 1998;13(4):623–649. [Google Scholar]
- Baranowski T, Anderson C, Carmack C. Mediating variable framework in physical activity interventions. How are we doing? How might we do better? American Journal of Preventive Medicine. 1998;15(4) doi: 10.1016/s0749-3797(98)00080-4. [DOI] [PubMed] [Google Scholar]
- Begg CB. In: The handbook of research synthesis. Cooper H, Hedges LV, editors. New York: Russell Sage Foundation; 1994. [Google Scholar]
- *.Bennett JA, Young HM, Nail LM, Winters-stone K, Hanson G. A Telephone- Only Motivational Intervention to Increase Physical Activity in Rural Adults. Nursing Research. 2008;57(1):24–32. doi: 10.1097/01.NNR.0000280661.34502.c1. [DOI] [PubMed] [Google Scholar]
- *.Blanchard CM, Fortier M, Sweet S, O’Sullivan T, Hogg W, Reid RD, Sigal RJ. Explaining physical activity levels from a self-efficacy perspective: the physical activity counseling trial. Annals of behavioral medicine: a publication of the Society of Behavioral Medicine. 2007;34(3):323–8. doi: 10.1007/BF02874557. [DOI] [PubMed] [Google Scholar]
- Burke SM, Shapcott KM, Carron AV, Bradshaw MH, Estabrooks PA. Group goal setting and group performance in a physical activity context. International Journal of Sport and Exercise Psychology. 2010;8(3):245–261. [Google Scholar]
- Burke V, Beilin LJ, Cutt HE, Mansour J, Mori TA. Moderators and mediators of behaviour change in a lifestyle program for treated hypertensives: a randomized controlled trial (ADAPT) Health education research. 2008;23(4):583–91. doi: 10.1093/her/cym047. [DOI] [PubMed] [Google Scholar]
- *.Cardinal BJ. Effects of behavioral monitoring on physical activity and psychosocial determinants of exercise behavior. Social Behavior and Personality. 1997;25(1):13–18. [Google Scholar]
- Conn VS, Hafdahl AR, Mehr DR. Interventions to increase physical activity among healthy adults: meta-analysis of outcomes. American journal of public health. 2011;101(4):751–8. doi: 10.2105/AJPH.2010.194381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courneya KS, McAuley E. Can short-range intentions predict physical activity participation. Perceptual and motor skills. 1993;77(1):115–22. doi: 10.2466/pms.1993.77.1.115. [DOI] [PubMed] [Google Scholar]
- Courneya KS, McAuley E. Cognitive mediators of the social influence-exercise adherence relationship: a test of the theory of planned behavior. Journal of behavioral medicine. 1995;18(5):499–515. doi: 10.1007/BF01904776. [DOI] [PubMed] [Google Scholar]
- *.Crain AL, Martinson BC, Sherwood NE, O’Connor PJ. The long and winding road to physical activity maintenance. American journal of health behavior. 2010;34(6):764–75. doi: 10.5993/ajhb.34.6.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishman RK, Vandenberg RJ, Motl RW, Wilson MG, DeJoy DM. Dose relations between goal setting, theory-based correlates of goal setting and increases in physical activity during a workplace trial. Health education research. 2010;25(4):620–31. doi: 10.1093/her/cyp042. [DOI] [PubMed] [Google Scholar]
- DuCharme KA, Brawley LR. Predicting the intentions and behavior of exercise initiates using two forms of self-efficacy. Journal of behavioral medicine. 1995;18(5):479–97. doi: 10.1007/BF01904775. [DOI] [PubMed] [Google Scholar]
- Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. Journal of the American Medical Association. 1999;281(4):327–334. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- Dutton GR, Tan F, Provost BC, Sorenson JL, Allen B, Smith D. Relationship between self-efficacy and physical activity among patients with type 2 diabetes. Journal of behavioral medicine. 2009;32(3):270–277. doi: 10.1007/s10865-009-9200-0. [DOI] [PubMed] [Google Scholar]
- Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Ebben W, Brudzynski L. Motivations and barriers to exercise among college students. Journal of Exercise Physiology Online. 2008;11(5) [Google Scholar]
- Ekkekakis P. Let Them Roam Free? Sports Medicine. 2009;39(10):857–888. doi: 10.2165/11315210-000000000-00000. [DOI] [PubMed] [Google Scholar]
- *.Elavsky S, Mcauley E. Exercise and self-esteem in menopausal women: a randomized controlled trial involving walking and yoga. American Journal of Health Promotion. 2007;22(2):83–92. doi: 10.4278/0890-1171-22.2.83. [DOI] [PubMed] [Google Scholar]
- *.Estabrooks PA, Smith-Ray RL, Almeida FA, Hill J, Gonzales M, Schreiner P, Van Den Berg R. Move More: Translating an efficacious group dynamics physical activity intervention into effective clinical practice. International Journal of Sport and Exercise Psychology. 2011;9(1):4–18. [Google Scholar]
- Fletcher GF, Balady G, Blair SN, Blumenthal J, Caspersen C, Chaitman B, Epstein S, et al. Statement on exercise: benefits and recommendations for physical activity programs for all Americans. Circulation. 1996;94(4):857–862. doi: 10.1161/01.cir.94.4.857. [DOI] [PubMed] [Google Scholar]
- *.Greaney ML, Riebe D, Ewing Garber C, Rossi JS, Lees FD, Burbank PA, Nigg CR, et al. Long-term effects of a stage-based intervention for changing exercise intentions and behavior in older adults. The Gerontologist. 2008;48(3):358–67. doi: 10.1093/geront/48.3.358. [DOI] [PubMed] [Google Scholar]
- *.Hager RL, Hardy A, Aldana SG, George JD. Evaluation of an Internet, stage- based physical activity intervention. American Journal of Health Education. 2002;33(6):329–337. [Google Scholar]
- Hovell M, Sallis J, Hofstetter R, Barrington E, Hackley M, Elder J, Castro F, et al. Identification of correlates of physical activity among Latino adults. Journal of community health. 1991;16(1):23–36. doi: 10.1007/BF01340466. [DOI] [PubMed] [Google Scholar]
- Hughes SL, Seymour RB, Campbell RT, Whitelaw N, Bazzarre T. Best-practice physical activity programs for older adults: findings from the national impact study. American journal of public health. 2009;99(2):362–368. doi: 10.2105/AJPH.2007.131466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Irvine AB, Philips L, Seeley J, Wyant S, Duncan S, Moore RW. Get moving: a web site that increases physical activity of sedentary employees. American journal of health promotion. 2011;25(3):199–206. doi: 10.4278/ajhp.04121736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJK, Gavaghan DJ, McQual HJ. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Controlled Clinical Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- King AC, Haskell WL, Taylor CB, Kraemer HC, DeBusk RF. Group- vs Home-Based Exercise Training in Healthy Older Men and Women: A Community-Based Clinical Trial. Journal of the American Medical Association. 1991;266(11):1535–1542. [PubMed] [Google Scholar]
- *.Lane A, Murphy N, Bauman a, Chey T. Randomized controlled trial to increase physical activity among insufficiently active women following their participation in a mass event. Health Education Journal. 2010;69(3):287–296. [Google Scholar]
- *.Latimer AE, Rench TA, Rivers SE, Katulak NA, Materese SA, Cadmus L, Hicks A, et al. Promoting participation in physical activity using framed messages: an application of prospect theory. British journal of health psychology. 2008;13(4):659–81. doi: 10.1348/135910707X246186. [DOI] [PubMed] [Google Scholar]
- Lattimore D, Wilcox S, Saunders R, Griffin S, Fallon E, Hooker S, Durstine JL. Self-reported barriers of middle-aged and older adults entering a home-based physical activity program. Health Promotion. 2011;9(2):15–28. [Google Scholar]
- Lewis BA, Marcus BH, Pate RR, Dunn AL. Psychosocial mediators of physical activity behavior among adults and children. American journal of preventive medicine. 2002;23(2 Suppl):26–35. doi: 10.1016/s0749-3797(02)00471-3. [DOI] [PubMed] [Google Scholar]
- Li F, McAuley E, Harmer P, Duncan TE, Chaumeton NR. Tai Chi enhances self-efficacy and exercise behavior in older adults. Journal of Aging and Physical Activity. 2001;9(2):161–171. [Google Scholar]
- Luszczynska A, Schwarzer R, Lippke S, Mazurkiewicz M. Self-efficacy as a moderator of the planning-behaviour relationship in interventions designed to promote physical activity. Psychology & health. 2011;26(2):151–66. doi: 10.1080/08870446.2011.531571. [DOI] [PubMed] [Google Scholar]
- Maddux JE. Looking for common ground: A comment on Kirsch and Bandura. In: Maddux JE, editor. Self-efficacy, adaptation and adjustment. New York: Plenum; 1995. pp. 377–386. [Google Scholar]
- *.Marcus BH, Bock B, Pinto B, Forsyth L. Efficacy of an individualized, motivationally-tailored physical activity intervention. Annals of Behavioral. 1998;13:174–180. doi: 10.1007/BF02884958. [DOI] [PubMed] [Google Scholar]
- Marcus BH, King TK, Clark MM, Pinto BM, Bock BC. Theories and techniques for promoting physical activity behaviour. Sports medicine. 1996;22(5):321–331. doi: 10.2165/00007256-199622050-00005. [DOI] [PubMed] [Google Scholar]
- *.Marcus BH, Napolitano MA, King AC, Lewis BA, Whiteley JA, Albrecht A, Parisi A, et al. Telephone versus print delivery of an individualized motivationally tailored physical activity intervention: Project STRIDE. Health psychology. 2007;26(4):401–9. doi: 10.1037/0278-6133.26.4.401. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Research quarterly for exercise and sport. 1992;63(1):60–6. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- McAuley E. The role of efficacy cognitions in the prediction of exercise behavior in middle-aged adults. Journal of behavioral medicine. 1992;15(1):65–88. doi: 10.1007/BF00848378. [DOI] [PubMed] [Google Scholar]
- McAuley E, Blissmer B. Self-efficacy determinants and consequences of physical activity. Exercise and sport sciences reviews. 2000;28(2):85–8. [PubMed] [Google Scholar]
- McAuley E, Jerome GJ, Elavsky S, Marquez DX, Ramsey SN. Predicting long-term maintenance of physical activity in older adults. Preventive Medicine. 2003a;37(2):110–118. doi: 10.1016/s0091-7435(03)00089-6. [DOI] [PubMed] [Google Scholar]
- McAuley E, Jerome GJ, Marquez DX, Elavsky S, Blissmer B. Exercise self- efficacy in older adults: Social, affective, and behavioral influences. Annals of Behavioral Medicine. 2003b;25(1):1–7. doi: 10.1207/S15324796ABM2501_01. [DOI] [PubMed] [Google Scholar]
- McAuley E, Lox C, Duncan TE. Long-term maintenance of exercise, self-efficacy, and physiological change in older adults. Journal of gerontology. 1993;48(4):218–24. doi: 10.1093/geronj/48.4.p218. [DOI] [PubMed] [Google Scholar]
- McAuley E, Mailey EL, Mullen SP, Szabo AN, Wójcicki TR, White SM, Gothe N, et al. Growth trajectories of exercise self-efficacy in older adults: influence of measures and initial status. Health psychology. 2011;30(1):75–83. doi: 10.1037/a0021567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAuley E, Mihalko SL. Measuring exercise-related self-efficacy. In: Duda J, editor. Advances in sport and exercise psychology measurement. Morgantown: Fitness Information Technology; 1998. pp. 370–390. [Google Scholar]
- McAuley E, Szabo A, Gothe N, Olson EA. Self-Efficacy: Implications for Physical Activity, Function, and Functional Limitations in Older Adults. American Journal of Lifestyle Medicine. 2011;5(4):361–369. doi: 10.1177/1559827610392704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Morgan AL, Tobar D, Snyder L. Walking toward a new me: the impact of prescribed walking 10,000 steps/day on physical and psychological well-being. Journal of physical activity & health. 2010;7(3):299–307. doi: 10.1123/jpah.7.3.299. [DOI] [PubMed] [Google Scholar]
- Neupert SD, Lachman ME, Whitbourne SB. Exercise self-efficacy and control beliefs: effects on exercise behavior after an exercise intervention for older adults. Journal of aging and physical activity. 2009;17(1):1–16. doi: 10.1123/japa.17.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological bulletin. 2007;133(4):673–93. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- Ohkawara K, Tanaka S, Miyachi M, Ishikawa-Takata K, Tabata I. A dose-response relation between aerobic exercise and visceral fat reduction: systematic review of clinical trials. International journal of obesity (2005) 2007;31(12):1786–97. doi: 10.1038/sj.ijo.0803683. [DOI] [PubMed] [Google Scholar]
- Oman RF, King AC. Predicting the adoption and maintenance of exercise participation using self-efficacy and previous exercise participation rates. American journal of health promotion. 1998;12(3):154–61. doi: 10.4278/0890-1171-12.3.154. [DOI] [PubMed] [Google Scholar]
- *.Opdenacker J, De Bourdeaudhuij I, Auweele YV, Boen F. Psychosocial mediators of a lifestyle physical activity intervention in women. Psychology of Sport and Exercise. 2009;10(6):595–601. [Google Scholar]
- Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, Buchner D, et al. Physical activity and public health: A recommendation from the Centers for Disease Contol and Prevention and the American College of Sports Medicine. Journal of the American Medical Association. 1995;273:402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- Poag K, McAuley E. Goal setting, self-efficacy, and exercise behavior. Journal of Sport and Exercise Psychology. 1992;14(4):352–360. [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. Journal of consulting and clinical psychology. 1983;51(3):390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- *.Resnick B. Testing the effect of the WALC intervention on exercise adherence in older adults. Journal of Gerontological Nursing. 2002;28(6):40–49. doi: 10.3928/0098-9134-20020601-10. [DOI] [PubMed] [Google Scholar]
- *.Resnick B, Luisi D, Vogel A. Testing the Senior Exercise Self-efficacy Project ( SESEP) for use with urban dwelling minority older adults. Public health nursing. 2008;25(3):221–234. doi: 10.1111/j.1525-1446.2008.00699.x. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Hovell MF, Hofstetter RC. Predictors of adoption and maintenance of vigorous physical activity in men and women. Preventive medicine. 1992;21(2):237–251. doi: 10.1016/0091-7435(92)90022-a. [DOI] [PubMed] [Google Scholar]
- Sharma M, Sargent L, Stacy R. Predictors of leisure-time physical activity among African American women. American journal of health behavior. 2005;29(4):352–359. doi: 10.5993/ajhb.29.4.7. [DOI] [PubMed] [Google Scholar]
- Sherwood NE, Jeffery RW. The behavioral determinants of exercise: implications for physical activity interventions. Annual review of nutrition. 2000;20:21–44. doi: 10.1146/annurev.nutr.20.1.21. [DOI] [PubMed] [Google Scholar]
- Sniehotta FF, Scholz U, Schwarzer R. Bridging the intention–behaviour gap: Planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychology & Health. 2005;20(2):143–160. [Google Scholar]
- Kaewthummanukul T, Brown KC. Determinants of employee Participation in Physical Activity. American Association of Occupational Health Nurses Journal. 2006;54(6):249–261. doi: 10.1177/216507990605400602. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Healthy People 2010 Final Review. Washington, D.C: U.S. Government Printing Office; 2011. pp. 22-2–14. [Google Scholar]
- *.Wadsworth D, Hallam JS. Effect of a Web Site Intervention on physical activity of college females. American Journal of Health Behavior. 2010;34(1):60–69. doi: 10.5993/ajhb.34.1.8. [DOI] [PubMed] [Google Scholar]
- Williams DM, Papandonatos GD, Jennings EG, Napolitano M, Lewis B, Whiteley J, Bock BC, et al. Does tailoring on additional theoretical constructs enhance the efficacy of a print-based physical activity promotion intervention? Health psychology. 2011;30(4):432–441. doi: 10.1037/a0023084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams SL, French DP. What are the most effective intervention techniques for changing physical activity self-efficacy and physical activity behaviour--and are they the same? Health education research. 2011;26(2):308–322. doi: 10.1093/her/cyr005. [DOI] [PubMed] [Google Scholar]
- van Stralen MM, De Vries H, Mudde AN, Bolman C, Lechner L. Determinants of initiation and maintenance of physical activity among older adults: a literature review. Health Psychology Review. 2009;3(2):147–207. [Google Scholar]