Abstract
Active engagement in life is a critical factor for successful aging. Research indicates that community engagement is strongly associated with health and well-being in late life. However, less is understood regarding the influence of neighborhood conditions on health and well-being, particularly in older African-American adults. The current study describes a convenience sample of older African Americans (N = 501, mean age = 70.7 [range 55-95] years) living in Detroit. The specific goal is to examine the relationships between their perceptions of neighborhood conditions, level of community engagement, and their health and well-being. Survey findings reveal a sample of highly engaged older African Americans in reasonable health who perceive their neighborhoods favorably. Regression analysis results indicate that community engagement is closely associated with both neighborhood perceptions and well-being in this sample. We propose that community engagement or “participation” mediates the relationship between neighborhood conditions and well-being for older African Americans living in Detroit.
Introduction
Accumulated evidence suggests that better health and community engagement lead to greater well-being later in life. Rowe and Khan (1997) defined successful aging as the absence of disease and disability, high levels of physical and cognitive functioning, and active engagement in life. The literature on successful aging suggests that to comprehensively understand “living well” and “being well,” one must attend to factors beyond the aging body, including the social and physical environment in which one lives. Researchers argue further that the subjective experiences related to the interaction between aging bodies and an ever-changing social and physical world exert a meaningful force on overall health and well-being (Cernin, Lysack, & Lichtenburg, 2011; Strawbridge, Wallhagen, & Cohen, 2002). Gerontology theorists and researchers also point to the complex relationships between the environment, both home and extended, and health and functioning in older adults (Lawton & Nahemow, 1973; Rowles, 1983; Stark, 2001; Wahl, Fänge, Oswald, Gitlin, & Iwarsson, 2009; Yen, Michael, & Perdue, 2009). This research leaves little doubt that the actual place (i.e., physical location in which one lives), shapes the activities that are possible to engage in there, and in that way, ultimately contributes to health (Yen, Shim, Martinez, & Barker, 2012). Accordingly, researchers from several disciplines (e.g., public health, gerontology) have increasingly focused on the role that neighborhood conditions play in health and well-being in older adults, using both objective and subjective measures. Despite this commitment, however, the impact of neighborhood conditions on the health and well-being of minority older adults living in urban environments are less studied.
Investigating these relationships is essential since there is compelling evidence that speaks to the intersection of these factors. According to data from the National Social Life, Health, and Aging Project (NSHAP), age is positively associated with increased participation in social activities (e.g., volunteering, religious events) in part because older adults have more time after they retire from paid work (Cornwell, Laumann, & Schumm, 2008). Participation in one's social world is seen to be a significant factor for maintaining overall health and well-being. Greater community engagement and social participation, in turn, are associated with better health in old age and much reduced risk of mortality— as significant an effect as smoking, drinking, exercise and diet (Holt-Lunstad, Smith & Layton, 2010). Further, Corwin and colleagues found that both African-American and white older adults cited social activity as an important contributor to aging well (Corwin, Laditka, Laditka, Wilcox, & Lin, 2009). Studies focusing on older African Americans exclusively have produced similar results. Strong associations between community engagement and physical and emotional health have been found in recent studies with older African-American women (Fothergill, Ensminger, Robertson, Green, Thorpe, & Juon, 2011). Other research suggests that older African American women with less social activity may be at an increased risk for depression (Husaini, Moore, Castor, Neser, Whitten-Stovall, Linn, et al., 1991).
Given the important relationship between social engagement and well-being in older adults, it is imperative to understand barriers to the achievement of these valued outcomes. Neighborhood conditions have been identified as one such barrier. There is substantial evidence linking poor neighborhood conditions with decreased social participation. Bowling and Stafford (2007), in a cross-sectional survey of older people living in Britain, found that individuals living in less affluent residential areas engage in less social activity. More recently, Beard and colleagues (2009) used census data and environmental information to study the effects of neighborhood conditions on older adults in New York City. Their findings indicate that factors commonly associated with some urban living conditions, such as high crime and low socioeconomic status, may significantly impact the ability of older adults to remain active. Findings from such studies suggest that older adults living in disadvantaged neighborhoods could face greater barriers to participation compared to those living in more affluent areas.
While studies indicate associations between community engagement and well-being and between community engagement and neighborhood conditions, support for a causative relationship between neighborhood and health and well-being is more limited. Although there are studies that show perceived neighborhood problems are linked to poorer self-rated health (e.g., Bowling, Barber, Morris, & Ebrahaim, 2006; Krause, 1998), after a comprehensive review of the literature, Yen and colleagues concluded that there is only modest evidence to suggest that neighborhood conditions play a causative role in the health and well-being of older adults (Yen et al., 2009). In other words, the literature has shown mixed results, often dependent upon the variables included in the study and how they were measured. As Jorm (2005) notes, there is some evidence for an association between social support and social networks, but since there have been no intervention trials, clear evidence of a causal connection is lacking.
There is stronger evidence that older adults may be susceptible to the effects of adverse living conditions due to prolonged exposure to such environments coupled with an increased reliance on limited community resources (Beard et al., 2009; Bowling & Stafford, 2007). The conclusion of many is that those living in poor socioeconomic environments, such as inner-city African-American seniors, may be at increased risk for diminished well-being as a result of their surroundings. However, it is plausible that the reverse is true. There are studies in Detroit, Michigan and elsewhere that show that African-American seniors are resilient and able to adapt well to adverse situations (Byrnes, Lichtenberg, & Lysack, 2006; Jang, Borenstein-Graves, Haley, Small, & Mortimer, 2003). In Detroit, at least, the historical and cultural dimensions of community engagement are highly relevant. Racial tensions in the 1960s produced an exodus of large numbers of predominantly white citizens to the suburbs while the remaining predominantly Black population was left to live in what has become decades of poverty and urban decay. Those who did stay through the years now find themselves living in very low-density neighborhoods with few amenities. Yet, there is research to suggest that this common history of oppression and disadvantage may in fact be positive to the degree that it fosters an ability for African-American older adults to deal with challenges in later life and maintain a sense of well-being (Lawton, Rajagopal, Brody, & Kleban, 1992; Roth, Haley, Owen, Clay, & Goode, 2001). The assertion is that their shared history as survivors of racial and economic difficulties may provide conditions for community engagement to occur. Baldwin, Jackson, Okoh, and Cannon (2010) have studied psychological resources like optimism and racial stress in African Americans and confirm this idea. Taken together, such findings suggest that disadvantaged neighborhoods with a large population of seniors may nevertheless have a high proportion of resilient and well-adjusted individuals.
In sum, the literature indicates that active community engagement in the places that older adults live is strongly associated with well-being. Yet, the evidence supporting a neighborhood-well-being relationship in a large population of vulnerable citizens, such as inner-city African-American seniors, is limited. The purpose of this article is to:
investigate how older African Americans living in urban environments rate their community engagement, neighborhood conditions, and health and well-being; and
explore the relationships among these factors in this population.
Methods
Participants
Five hundred and one participants (n = 501) were recruited from a Participant Registry of African-American elders (Chadiha, Washington, Lichtenberg, Green, Daniels, & Jackson, 2011) who were willing to take part in research studies (see Procedure for details). The study participants were aged 55 to 95 years with an average age of 70.73 years (SD = 8.6 years). Chadiha et al. (2011) compared the overall demographic characteristics of the Participant Registry to those who took part in a population-based randomly sampled health survey and found that the Participant Registry individuals had the same prevalence of chronic diseases, but had somewhat greater functional abilities than the random sample. The study sample was 86% female, which reflects a somewhat greater proportion of females than in a previous Detroit Central City Survey which found 70% was female (Chapleski, 2002), but is not inconsistent with other studies of older African-American adults (e.g., Dennis & Neese, 2000; Manly, Byrd, Touradji, & Stem, 2004).
Procedures
Participants were recruited from volunteers in the Healthier Black Elders Center (HBEC), a joint collaboration between Wayne State University's (WSU) Institute of Gerontology and University of Michigan's Institute of Social Research (Chadiha et al., 2011). After receiving IRB and HBEC approval, trained community volunteers contacted PRP members and asked if they would like to participate in a telephone interview lasting approximately 45-60 minutes. If the respondent agreed, a trained interviewer called back to arrange a date and time for the interview. Inclusion criteria were being African American and aged 55 or above. Exclusion criteria were not speaking English, hearing difficulties that prevented clear communication over the telephone, and an inability to understand the survey questions due to apparent cognitive difficulties. Exclusion criteria were assessed solely by the interviewer in real time as they undertook the interview. Besides the 501 participants who completed the interview, 55 other eligible PRP members were invited to participate. Of these, 37 were not available after 4 attempts to schedule the phone interview, 10 were “not interested” or refused, 3 telephone numbers were disconnected and the prospective participants could not be reached, and 2 were deemed “not sufficiently cognizant” to understand the interview questions. An additional three participants did not complete the interview and these data were not included. Each participant who completed an interview was mailed a $15 CVS gift card.
Measures
Community Engagement
Community engagement was assessed using the Community Integration Measure (CIM) (McColl, Davies, Carlson, Johnston, & Minnes, 2001). The 10-item CIM was first validated on community-dwelling adults with brain injury, their family members, and college students (McColl et al., 2001). Subsequently, the CIM has been used to study older individuals with a variety of health conditions and physical disabilities including spinal cord injury (Lysack, Komanecky, Kabel, Cross, & Neufeld, 2007). The CIM asks respondents if they:
feel like they belong in their community;
know their way around their community;
know the rules;
feel accepted;
can be independent in their community;
like where they live;
feel close to others;
know people well enough to say hello;
have fun things to do; and
have productive activities to do in their community.
Each item is scored on a 5-point scale where 1 = always disagree, 2 = sometimes disagree, 3 = neutral, 4 = sometimes agree, and 5 = always agree. The maximum score is 50, with higher scores indicating greater community integration. The instrument has high internal consistency (Cronbach's alpha = 0.87) (McColl et al., 2001). For the current study the Cronbach's alpha was 0.834.
Neighborhood Perceptions
The Neighborhood Environment Scale (NES) (Crum, Lillie-Blanton, & Anthony, 1996) was used to investigate how participants perceived their neighborhoods. The measure is an 18-item survey consisting of True/False questions, several of which are “reverse-coded.” After the survey is completed, the items are coded so that a poor perception is assigned a “1” and a favorable perception receives a “0.” A total score for the NES is obtained by summing the individual item scores. Possible total scores range from 0 to 18, with higher scores indicating less favorable views of one's neighborhood. The survey includes several items about crime and safety, such as “There are plenty of safe places to walk in my neighborhood” and “Every few weeks, some adult gets beat up or mugged in my neighborhood.” The NES reports a high degree of internal consistency (Kinder Richardson 20 [KR-20] = 0.85) (Crum et al., 1996). KR-20 for the current sample was 0.838.
Well-Being
The Social Production Function Instrument for the Level of Well-Being (SPF-IL) was developed and validated for older adults using a series of studies in the Netherlands (Cramm, van Dijk, & Nieboer, 2013; Nieboer, Lindenberg, Boomsma, & Van Bruggen, 2005). According to its developers, well-being is essential to study in older adults since it is broader than health and provides insight into one's life as whole. For these researchers, well-being is defined as an individual's appraisal of his or her life situation as a whole; the totality of pleasures and pains, or quality of life. The SPF-IL is 15-item measure of well-being and it provides a total score along with scores on five subscales (affection, behavioral confirmation, status, comfort, and stimulation). Subscale scores were not included in the current study. Items are scored on a scale (0 = never, 1 = sometimes, 2 = often, 3 = always), resulting in an optimal well-being score of 45. Cramm, van Dijk, and Nieboer (2013) reported a Cronbach's alpha for the SPF-IL to be 0.850. In the current study it was 0.852.
Health and Mobility
Health was conceptualized using five variables in the LIFHE dataset. Self-rated health was scored as “poor,” “fair,” “good,” “very good,” or “excellent.” Self-rated health is correlated with objective health measures and mortality risk (Idler & Benyamini, 1997; Mossey & Shapiro, 1982).
Participants were also presented with a list of health problems (e.g., diabetes, cancer, heart disease) and asked to indicate whether or not they currently had any of these conditions. The question was self-reported; there was no independent confirmation that the condition was diagnosed by a physician. The sum of these was termed total health problems.
Previous research with older adults has shown single-item depression questions can yield valid and reliable results, even when collapsing response categories (Mahoney, Drinka, Alber, Gunter-Hunt, Matthews, Gravenstein, et al., 1994; Yochim, Mast, & Lichtenberg, 2003). We therefore used a simple depression question: “During the past month, how much of the time have you felt downhearted and blue?” There were six response options from “1 = none of the time” to “6 = all of the time.” Given the distribution of the study data, for analysis purposes we receded the responses as “1 = none of the time,” “2 = a little of the time,” and “3 = at least some of the time.” (No respondent indicated “6 = all of the time.”)
Cognition was another health-related variable assessed. Individuals were asked “Are your memory, thinking skills, or ability to reason worse than a year ago (Y/N)?”
Self-rated disability (“Do you think of yourself as having a disability (Y/N)?”) was the fifth health indicator. The single-item questions on depression, cognition, and disability were modeled after the single-item self-rated health measure used in the medical literature, which continues to surpass all other measurement options as the most powerful predictor of health and mortality (Idler & Benyamini, 1997; Mossey & Shapiro, 1982).
Finally, participants were asked about their mobility. Specific questions included whether or not they used specialized equipment or mobility devices (Y/N) and if they currently drove (Y/N) an automobile.
Data Analysis
Descriptive statistics were conducted on variables related to sociodemographics, community engagement neighborhood perceptions, well-being, and health and mobility. Cronbach's alpha coefficients were calculated for the full scales of the CIM and SPF-IL to determine internal consistencies. Kruder Richardson Formula 20 (KR-20) was employed to calculate internal consistency of the NES scale because of its dichotomous response choices. Mean rankings for the CIM, NES, and SPF-IL questions were also conducted to determine most concerning items related to engagement, neighborhood perceptions, and well-being.
Spearman's rho correlations were calculated to assess bivariate relationships among sociodemographic and survey variables, with primary importance placed on identifying the strongest correlates to community engagement, neighborhood perceptions, and well-being. Similarly, we estimated three stepwise regression models (dependent variables of engagement, neighborhood perceptions, and well-being) where the independent variables considered for the models were those found to be significant in the bivariate analyses. The significance level alpha was set at p < 0.05 for all statistical analysis. As a statistical note, and due to the skewed nature of the NES and CIM data, for the regression analyses the NES scale was dichotomized at the median (median = 3 out of a possible 18) so that scores from 0-2 were considered more favorable ratings and those above 2 were less favorable, and the CIM scale was dichotomized at the median (median = 45 out of a possible 50). Tests showed that the distribution of the SPF-IL data in this sample was approximately normal.
Results
Descriptive Statistics
Sociodemographics, Health, and Mobility
Participants in the study consisted of 501 African Americans aged 55 and over. The response rate for the telephone survey was 90% (501/555). Their average age was 71 years and participants ranged in age from 55 to 95 years (SD = 8.6 years). The sample was predominately female (N = 431, 86%) and urban, with nearly 83% residing within the city of Detroit. To a large degree this reflects the actual gender distribution of older African Americans in urban neighborhoods (Lichtenberg, Cameron, Duris, Ensberg, Heidebrink, Horst, et al., 2009; Manly et al., 2004). Nearly one-third of the sample (30%) were widowed and nearly half (46%) lived alone. They had lived in their current homes for more than 2 decades (mean = 21 years; range = 1 month to 66 years on average), With respect to education, 41% had some education beyond high school and an additional 30% had a 4-year college degree. While at first glance the level of education appears “high,” similar rates of post-secondary education have been reported in the literature for the cohort of ethnically minority individuals, now elderly, who benefitted tremendously from the automobile manufacturing and related economic boom of metropolitan Detroit in the 1950s and 60s (Chapleski, 2002). The participants reported reasonable levels of health: 63% rated their health as “good” or “very good” although they also reported 3.7 health problems, on average. Just over a quarter responded “yes” to the self-rated disability question. With regard to mental health, the sample was in good spirits for the most part; 70% reported feeling “downhearted or blue” either “none of the time” or “a little of the time.” However, nearly a third indicated some form of cognitive decline over the past year. Nonetheless, the sample was relatively independent and mobile: although one-third of the sample reported using mobility aids (e.g., canes, walkers) and having specialized equipment in the home (e.g., bath seat, grab bars), three-quarters of the sample reported they were driving. Table 1 presents more details on the sample characteristics.
Table 1. Sociodemographics, Health, and Mobility.
| Sociodemographics | Mean ± SD or Freq (%) |
|---|---|
| Age (yrs.) | 70.7 ± 8.6 |
| Gender | 431 (86.3) females, 70 (13.7) males |
| Marital status | Divorced = 150 (30.3) |
| Married = 120 (24.0) | |
| Never married = 49 (9.8) | |
| Separated = 14 (2.8) | |
| Single = 8 (1.6) | |
| Unmarried couple = 1 (0.2) | |
| Widowed = 152 (30.3) | |
| Education | HS grad or less = 151 (30.1) |
| Some college or tech school = 206 (41.1) | |
| 4 yr. college degree or more = 143 (28.5) | |
| Financial satisfaction | Completely satisfied = 41 (8.2) |
| Very satisfied = 77 (15.4) | |
| Somewhat satisfied = 241 (48.1) | |
| Not at all = 138 (27.5) | |
| Lives alone | No = 270 (53.9), Yes = 231 (46.1) |
| Years in current residence | 21.0 ± 16.8 |
| Health | |
| Self-rated health | Poor = 27 (5.4) |
| Fair = 116 (23.2) | |
| Good = 219 (43.7) | |
| Very good = 97 (19.4) | |
| Excellent = 39 (7.8) | |
| Depression | None of the time = 192 (38.3) |
| A little of the time = 159 (31.7) | |
| At least some of the time = 150 (29.9) | |
| Cognitive decline in past year | No = 351 (70.1), Yes = 150 (29.9) |
| Self-rated disability | No = 359 (71.7), Yes = 142 (28.3) |
| Total health problems | 3.7 ± 2.4 |
| Mobility | |
| Drives | No = 115 (23.0), Yes = 385 (76.8) |
| Mobility aids | No = 365 (72.9), Yes = 136 (27.1) |
| Specialized equipment | No = 328 (65.5), Yes = 169 (33.7) |
Community Engagement
Individuals in this study reported a very high degree of community engagement (Table 2). The sample mean for the CIM was 43.9, with a median score of 45.0 (Q1 = 41, Q3 = 49) out of a possible score of 50. Means on the individual items ranged from 3.91 to 4.75 out of 5. The sample scored very high on questions related to community familiarity. For example, the two highest scoring items were “I know my way around this community” (mean = 4.75) and “I know a number of people in this community well enough to say hello and have them say hello back” (mean = 4.74). Conversely, questions with the lowest means surrounded opportunities for community participation. Such items included “There are things that I can do in the community for fun in my free time” (mean = 4.01) and “I have something to do in this community during the main part of my day that is useful and productive” (mean = 3.91).
Table 2. Item Rarkings for the CIM, NES, and SPF-IL.
| Rank | Item | Mean (SD) |
|---|---|---|
| CIMa | Total score | 43.9 (6.0) |
| 1 | I have things to do in this community that are useful and productive. | 3.91 (1.24) |
| 2 | There are things I can do in this community for fun. | 4.01 (1.22) |
| 3 | I like where I'm living now. | 4.18 (1.20) |
| 4 | I feel like I'm a part of this community, like I belong here | 4.22 (1.02) |
| 5 | There are people I feel close to in this community. | 4.32 (99) |
| 6 | I know the rules in this community and I can fit with them. | 4.46 (90) |
| 7 | I feel I am accepted in this community. | 4.58 (77) |
| 8 | I can be independent in this community. | 4.70 (63) |
| 9 | I know people in this community well enough to say hello. | 4.74 (60) |
| 10 | I know my way around in this community. | 4.75 (56) |
| NESb | Total score | 4.4 (3.8) |
| 1 | In my neighborhood I see signs of racism at least once a week. | .07 (25) |
| 2 | In my neighborhood drug dealers have the most money | .09 (29) |
| 3 | Most adults in my neighborhood don't respect law. | .11 (31) |
| 4 | Every few weeks some kid gets beat up or mugged. | .12 (33) |
| 5 | Every few weeks some adult gets beat up or mugged. | .13 (34) |
| 6 | I often see drunk people on the street in my neighborhood. | .16 (37) |
| 7 | The people often steal or damage each others property | .19 (.39) |
| 8 | People don't take care of each other or protect others from crime. | .19 (.39) |
| 9 | For people in the neighborhood going to church is not important | .20 (.40) |
| 10 | There are a lot of poor people who don't have money for basic needs. | .21 (.41) |
| 11 | Almost every day, I see homeless people in the neighborhood | .22 (.41) |
| 12 | I have seen people using or selling drugs in my neighborhood. | .24 (.43) |
| 13 | I don't feel safe when walking around by myself. | .32 (.47) |
| 14 | Many yards have broken bottles and trash lying around. | .33 (.47) |
| 15 | There are not plenty of safe places to walk in my neighborhood. | .40 (.49) |
| 16 | Within walking distance, there is not a park to walk to. | .44 (.50) |
| 17 | The people in my neighborhood aren't the best people. | .46 (.50) |
| 18 | There are abandoned or boarded-up buildings in my neighborhood. | .61 (.49) |
| SPF-ILc | Total score | 30.7 (7.3) |
| 1 | Are your activities challenging to you? | 1.34 (.95) |
| 2 | Do people think you do better than others? | 1.64 (.83) |
| 3 | In the past few months have you felt perfectly healthy? | 1.70 (.91) |
| 4 | In the past few months have you felt physically comfortable? | 1.83 (.91) |
| 5 | Do people find you an influential person? | 1.93 (.89) |
| 6 | In the past few months have you felt relaxed? | 1.99 (.90) |
| 7 | Do people pay attention to you? | 2.02 (.86) |
| B | Are you known for things you have accomplished? | 2.03 (.96) |
| 9 | Do people help you if you have a problem? | 2.04 (.93) |
| 10 | How often are you fully concentrated when doing something? | 2.07 (.78) |
| 11 | Do others appreciate your role in the group? | 2.16 (.88) |
| 12 | Do you feel that people really love you? | 2.36 (.83) |
| 13 | Do you really enjoy your activities? | 2.39 (.81) |
| 14 | Do you feel useful to others? | 2.49 (.78) |
| 15 | Do other people find you reliable? | 2.68 (.60) |
Higher CIM scores indicate more engagement 1 = always disagree, 2 = sometimes disagree 3 = neutral, 4 = sometimes agree 5 = always agree.
Higher NES scores indicate poorer neighborhood perceptions; 0 = not true, 1 = true Items have been reworded here (eg., “do” charged to “don't”) to illustrate consistencies with coding conventions.
Higher SPF-IL scores indicate greater well-being; 0 = never 1 = sometimes, 2 = often, 3 = always.
Neighborhood Perceptions
As a whole, study participants reported highly favorable perceptions of their neighborhoods. The sample mean and median were 4.4 and 3.0, respectively, out of a possible score of 18 (see Table 2). Higher NES scores reflect poorer neighborhood perceptions. Item rankings revealed that questions related to safety and accessibility (e.g., “There are plenty of safe places to walk to in my neighborhood” or “The people in my neighborhood aren't the best people”) were rated among the highest of all NES questions, i.e., perceived the least favorably.
Well-Being
Though the sample reported high degrees of familiarity with their community (CIM) and high levels of engagement in them as well as favorable perceptions of their neighborhoods (NES), scores for well-being were more moderate (Table 2). Sample mean and median scores on the SPF-IL were 30.7 and 32.0, respectively, out of an optimal well-being score of 45. Consistent with the item rankings from the CIM, participants demonstrated the lowest mean score on the SPF-IL item “Are your activities challenging to you?” (mean = 1.31). The two questions that were positively endorsed most strongly were: “Do people find you reliable?” (mean = 2.68) and “Do you feel useful to others?” (mean = 2.49).
Associations among Community Engagement, Neighborhood Perceptions, and Weil-Being
Correlations
Spearman rho correlations revealed significant associations between community engagement, neighborhood perceptions, and well-being. Of all the bivariate associations, the strongest relationship was between engagement (CIM total) and neighborhood perception (NES total) (r = −.562, p < .001). However, community engagement was also related to well-being, evidenced by a significant correlation between CIM total and SPF-IL total scores (r = .361, p < .001). Though a significant correlation was also observed between neighborhood perceptions and well-being, the association was much weaker (r = −.183, p < .001). Of additional note, self-rated health was positively correlated with both well-being (r = .361, p < .001) and engagement (r = .138, p = .002) and negatively correlated with neighborhood perceptions (r = .109, p = .023). The most robust correlations are presented in the regression tables (Tables 3A-C).
Table 3. Variables Associated with Community Engagement, Neighborhood Perceptions, and Well-Being: Correlations and Betas.
| A. Dependent variable = Community engagement (logistic regression models using forward selection) | ||||
|---|---|---|---|---|
|
| ||||
| rs | B | S.E. (B) | Exp (B) | |
| Step 1 | ||||
| Neighborhood perceptions (NES) | −.334 | .040 | .709*** | |
| Cox and Snell R2 = .229 | ||||
| Nagelkerke R2 = .305 | ||||
| Step 2 | ||||
| Neighborhood perceptions (NES) | −.562*** | −.334 | .041 | .716*** |
| Well-being (SPF-IL) | .361*** | −.074 | .016 | 1.077*** |
| Δ Cox and Snell R2 = .038 | ||||
| Δ Nagelkerke R2 = .041 | ||||
|
| ||||
| Final model: Chi-square (df = 2) = 132.71***, Cox and Snell R2 = .267, Nagelkerke R2 = .356 | ||||
|
| ||||
| Note: Correlations conducted with CIM, NES, and SPF-IL total scores as continuous variables. | ||||
| B. Dependent variable = Neighborhood perceptions (logistic regression models using forward selection) | ||||
|---|---|---|---|---|
|
| ||||
| rs | B | S.E. (B) | Exp (B) | |
| Step 1 | ||||
| Engagement (CIM) | −.250 | .031 | .779*** | |
| Cox and Snell R2 = .223 | ||||
| Nagel kerke R2 = .301 | ||||
| Step 2 | ||||
| Engagement (CIM) | −.562*** | −.254 | .031 | .776*** |
| Age | −.181*** | −.047 | .014 | .954** |
| Δ Cox and Snell R2 = .022 | ||||
| Δ Nagelkerke R2 = .029 | ||||
|
| ||||
| Final model: Chi-square (df = 2) = 120.13***, Cox and Snell R2 = .245, Nagelkerke R2 = .330 | ||||
|
| ||||
| Note: Correlations conducted with NES, and CIM total scores as continuous variables. | ||||
| C. Dependent variable = Well-being (stepwise Iinear regression models) | ||||
|---|---|---|---|---|
|
| ||||
| rs | B | S.E. (B) | (B) | |
| Step 1 | ||||
| Self-rated health | 2.770 | .333 | .373*** | |
| Adjusted R2 = .137 | ||||
| Step 2 | ||||
| Self-rated health | 2.526 | .324 | .341*** | |
| Engagement (CIM) | .317 | .055 | .253*** | |
| Δ Adjusted R2 = .061 | ||||
| Step 3 | ||||
| Self-rated health | .361*** | 2.258 | .323 | .304*** |
| Engagement (CIM) | .361*** | .309 | .054 | .247*** |
| Cognitive decline | −.256*** | −3.140 | .697 | −.194*** |
| Δ Adjusted R2 = .035 | ||||
|
| ||||
| Final model: F(3, 427) = 44.28***, Adjusted R2 = .233 | ||||
|
| ||||
| Note: Correlations were conducted with SPF-IL and CIM total scores as continuous variables. | ||||
p < .05;
p < .01;
p < .001.
Regression Models
To determine the sets of factors most closely associated with community engagement, neighborhood perceptions, and well-being, we estimated three (step-wise) regression models. The direction of the associations among engagement, neighborhood perceptions, and well-being are not known, and hence we developed regression models using each of these factors as dependent variables. The covariates considered for possible inclusion in these models were socio-demographic factors and other variables shown to be significantly related to at least one of the dependent variables in bivariatc analysis. The list included: age, gender, education (HS or less, some college, 4-year degree or more), self-rated health (poor, fair, good, very good, excellent), number of health conditions, depression (none, a little, or at least some of the time), disability status (Y/N), and cognitive decline (Y/N), and two of neighborhood perceptions, engagement and well-being, depending on the particular regression model. Logistic regression analyses using forward selection was conducted for the dependent variables of community engagement and neighborhood perceptions. For the dependent variable of well-being, stepwise linear regression analysis was performed.
Model 1
Dependent variable = community engagement (Table 3A)—A logistic regression model demonstrated that, neighborhood perception (Step 1; Chi-square (1) = 110.2, p < .001) explained approximately 22.9% (Cox and Snell R2) to 30.5% (Nagelkerke R2) of the variance in community engagement. In Step 2, well-being (Chi-square (2) = 131.7, p < .001) was added to the model, resulting in an additional 3.8% (Cox and Snell R2) to 4.1% (Nagelkerke R2) of explained variance (total explained variance = 26.7% and 35.6%, respectively).
None of the other potential covariates added significantly to the model. In the final model, for each I point increase in the NFS score, the odds of better engagement is reduced by a factor of 0.78, and for each 1 point increase in the SPF-1L score, the odds of better engagement is increased by a factor of 1.077.
Model 2
Dependent variable = neighborhood perceptions (Table 3B)— Logistic regression resulted in an initial model with CIM total score (community engagement) as the sole independent predictor of neighborhood perceptions (Step 1; Chi-square (1) = 107.0, p < .001). The addition of age (Chi-square (2) = 119.0, p < .001) in Step 2 resulted in a final model with Cox and Snell and Nagelkerke R2 values of .245 and .330, respectively, indicating that engagement and age accounted for approximately one-quarter to one-third of the variance in neighborhood perception. Based on the odds ratios [Fxp(B)], the final model implies that an increase of 1 point in the CIM total score results in the odds of poorer (above median score) neighborhood perception decreasing by a factor of 0.78. Similarly, older age is related to better neighborhood perceptions; for each year increase in age, the odds of having a poorer perception of one's neighborhood are reduced by a factor of 0.95. Notably, well-being was not a significant factor associated with neighborhood perceptions after taking into account CIM total score and age. Also, none of the health measures were related to neighborhood perception in the final model.
Model 3
Dependent variable = well-being (Table 3C)—Stepwise linear regression revealed that self-rated health was the factor most related to well-being (Step 1; F(1, 425) = 69.0, p < .001) accounting for about 14% of the variance. This was expected because approximately half of the questions on the SPF-1L are related to physical health and well-being. However, engagement was the second most influential variable for predicting well-being. After self-rated health, total CIM score (community engagement) explained an additional 6.1 % of the variance (Step 2, F(2, 424) = 53.6, p < 0.001) in well-being. Finally, in Step 3, cognitive decline was entered into the model (F(3, 423) = 44.0, p < .001). This final model accounted for 23.3% of the variance in well-being. The model indicates that better self-rated health and increased community engagement, imply better well-being, and that reporting a decline in memory over the past year has a negative impact on well-being. Notably, neighborhood perceptions were not a significant factor in explaining well-being after accounting for the influence of self-rated health, community engagement, and cognitive decline.
Discussion
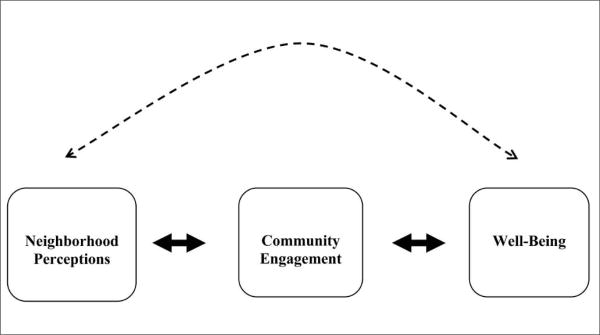
This study described 501 older adults living in Detroit and examined relationships among their neighborhood perceptions, engagement in the community, and health and well-being. The predominately female sample was in fair to good health and reported positive well-being overall. Several important findings emerged from the data. First, this sample of older African Americans were highly integrated and engaged in their communities. Second, they rated their neighborhoods very favorably. Third, neighborhood perceptions and well-being were not highly related, although our observation of a significant correlation suggests some level of association between these variables. Finally, and perhaps most significant of all, community engagement, was associated with both neighborhood perceptions and well-being. As the regression analyses shows (Table 3C), community engagement (CIM score) was a significant predictor of well-being (SPL-IL score) alongside of health factors. After age, community engagement was also the only significant predictor of neighborhood perceptions (NES score) (Table 3B). As a result of these findings, we contend that community engagement plays a pivotal role in the well-being of older African American adults, not only directly but also by serving as a mechanism through which neighborhood conditions influence health and well-being (sec Figure 1).
Figure 1.
Proposed model for the relationships among neighborhood perceptions community engagement, and well-being
The model we propose in Figure 1 has three components:
the relationship between the neighborhood and community engagement;
the relationship between engagement and well-being; and
the relationship between neighborhood and well-being.
Evidence for the first two relationships comes from our regression models showing that community engagement is tied to both neighborhood perceptions and well-being (Table 3). Such findings are consistent with a substantial literature on older adults' engagement and participation (Beard et al., 2009; Bowling & Stafford, 2007; Corwin et al, 2009; Fothergill et al., 2011; Husaini et al., 1991). Though past studies have demonstrated associations between engagement and well-being in various ethnic groups of older adults, including African Americans (e.g., Fothergill et al., 2011), our study is one of the first to provide evidence for a relationship between engagement and neighborhood conditions in a sample comprised exclusively of older African Americans.
Closer examination of the sample and how they rated their neighborhoods and community engagement provides additional insight as to why neighborhood perceptions and engagement are related. Participants in the current study reported high degrees of community integration (mean = 43.9 out of 50) and also very few concerns with their neighborhoods (mean = 4.4. out of 18). Upon initial examination, these findings were unexpected. However, research has shown that significant “place attachment” develops in older adults over time (Rowles, 1983). On average, our study participants had lived in their current homes in these neighborhoods for more than 20 years. According to Rowles (1983), frequent social contact with the same people over many years fosters strong social tics, strong feelings of group identification, and even greater group solidarity. Thus, consistent with this literature, neighborhood perceptions in this study may have been more positive than objective observers might have expected because the study participants were community “insiders” who looked past the physical realities of abandoned buildings to valued social bonds and networks that are invisible to outsiders. That is not to say, however, that problems in the neighborhood do not affect engagement or even well-being. For example, the item “There are plenty of safe places for me to walk in my neighborhood” ranked highest (least favorably) on the NFS. On the CIM, the two most negatively rated items involved a lack of fun or productive community activities. Similarly, the lowest ranked well-being question was “Are your activities challenging to you?” Taken together, these rankings suggest that older African Americans in Detroit are concerned with opportunities for productive and stimulating activities that they can perform safely within their communities.
Unlike the first two components of our model that involve community integration, interpreting the relationship between neighborhood conditions and well-being was less clear. Neighborhood perceptions and well-being were significantly correlated, although the magnitude of this correlation was low. Further, neighborhood perceptions and well-being were not predictive of one another in the regression model. At best, this suggests some minimal level of association between the two. Intuitively, while it may seem that neighborhood conditions and health and well-being are related, previous literature shows that others are also cautious in proposing such a relationship. For example, after a lengthy review of the literature in this area, Yen and colleagues (2009) concluded that there was limited evidence to directly link neighborhood conditions with health and well-being in older adults. We argue that this holds for older African-American adults as well. Our model takes it a step further, though, by proposing not only that these two variables are not directly related, but also that community engagement mediates this indirect association.
Research suggests that an element of this mediating function of community engagement may be related to the characteristics of the individuals residing in those neighborhoods. For example, Osborne and colleagues (2011) showed how participation in community activities is largely contingent upon neighborhoods where members are well known to each other and trust each other. As these researchers argue, without a sufficient level of familiarity, community members do not engage and cooperate in as many community activities. Yen, Shim, Martinez, and Barker (2012) have very recently reported on a qualitative study to uncover the mechanisms by which older adults use physical places like neighborhoods and activities to remain socially engaged and healthy in later life. Again, a key factor for community engagement appears to be shared personal characteristics and experiences. These researchers found that in ethnically diverse neighborhoods, racial tensions can negatively influence older adults' community engagement. They write: “Feeling different than, being taken advantage of, or overlooked by racially and ethnically dissimilar neighbors appears to constitute a source of environmental press with negative effects on neighborhood engagement” (p. 9). This finding leads us to ask whether in our sample that was 100% African American and drawn from neighborhoods in the city of Detroit which are nearly 90% Black we should expect exceptionally strong community engagement and perhaps well-being too. According to this line of thinking, the shared history as survivors of racial and economic difficulties for decades may be the underlying foundation for community engagement to occur. Baldwin, Jackson, Okoh, and Cannon (2010) have studied psychological resources like optimism and racial stress in African Americans and confirm this idea.
Yet, it must be reiterated that the lowest community engagement scores were on items related to opportunities for “fun activities” and for participation in “meaningful productive activities.” Since there is considerable evidence linking community engagement with health and well-being (e.g., Corwin et al., 2009) this finding is a concern. We ask here whether well-being, which was already reasonably high, could have been even higher if the neighborhoods in which the sample resided were more attractive and positive places to live. Our findings demonstrate the crucial role that social spaces play in maintaining robust social networks and, consequently, feelings of inclusion and community engagement and social participation. There is a need to build and maintain such “healthy neighborhoods” for older residents to ensure that older people have engaging social spaces to be physically and mentally active.
There are several limitations to the current study that should be acknowledged and considered for future research. First, this was a sample of convenience utilizing a cross-sectional design. Therefore, while we may appear to suggest causality or direction regarding the associations between neighborhood, community engagement, and well-being, this establishment of causality requires new longitudinal studies. While it is reasonable to propose that neighborhood conditions affect engagement, which, in turn, affects well-being, it is certainly plausible that the reverse is true. In other words, one's well-being could impact community engagement to the extent that it would then influence older adults' feelings about their neighborhoods. Second, the study participants were community-minded older adults, mostly educated women, who, by virtue of their involvement with the Institute of Gerontology, demonstrated a desire for life-long learning and a willingness to share their knowledge with others. In addition, their outlook now as a cohort of older adults was shaped by unique historical events. They weathered significant racial and social disruption and stayed positively committed to improving neighborhood conditions in a city that continues to struggle with poverty and racism. Accordingly, our findings cannot be extrapolated beyond the sample studied to the general population of older people in Detroit. Third, there are limitations in study measures. For example, the NFS, with its orientation to observations of neighborhood conditions over a short period of time (e.g., “in the last week,” “every few weeks”) may have resulted in more positive neighborhood ratings than would have been the case with a measure that asked for ratings based on some longer duration. Although we believe this was a minor influence on study findings, like others (Hipp, 2010; Yen et al., 2012) we call for more research to develop stronger measures of neighborhood and neighborhood connectedness in studies of older adults.
Study results suggest new directions for future research, including conducting longitudinal studies on the neighborhood perceptions, community engagement, and well-being of older African Americans. Further, studies need to validate measures of neighborhood perceptions in older African-American adults and consider objective measures and other forms of community engagement. As Hipp (2010) has pointed out, it is also important to determine in more detail what “neighborhood” is actually being studied. A rich literature in the social sciences has shown that neighborhood satisfaction docs not always match the objective reality of the physical urban environment (e.g., Byrnes et al., 2006; Duck & Rawls, 2012; Wen, Hawkley, & Cacioppo, 2006). Likely, a combination of methodologies, using objective and subjective measures will be required to disentangle the complex relationships between the physical spaces in which older adults live and the social experiences and behaviors encountered there that ultimately contribute to well-being.
Conclusion
Study results show that strong community engagement is possible in neighborhoods that objectively are disadvantaged. Older residents in these neighborhoods can also report high levels of community engagement and positive well-being. Study findings also point to the power of neighborhood cohesion that comes with long residence and shared experience. Older African-American adults in this study had strong community integration and community engagement that may support health and well-being. This study focused on understanding how community engagement might enhance well-being in older adults, and it is one of very few studies with an older African-American sample. More research should be undertaken to discover how to harness community cohesion to maintain and improve neighborhood conditions for all older minorities. Additional research should also be conducted to evaluate how older minority adults use their neighborhoods and in what way investments in disadvantaged neighborhoods can improve their daily lives.
Acknowledgments
We would like to thank Pat Rencher, education coordinator at the Healthier Black Elderly Center (HBEC) and all of the volunteers at HBEC.
Footnotes
This study was supported by a grant from the National Institutes of Health, 5P30 AG015281, the Michigan Center for Urban African American Aging Research, and the Wayne State University President's Research Enhancement Program for Urban Initiatives.
References
- Baldwin DR, Jackson D, Okoh I, Cannon RL. Resiliency and optimism: An African American senior citizens perspective. Journal o f Black Psychology. 2010;37(1):24–41. doi: 10.1177/0095798410364394. [DOI] [Google Scholar]
- Beard JR, Blaney S, Gerda M, Frye V, Lovasi GS, Ompad D, et al. Neighborhood characteristics and disability in older adults. The Journals of Gerontology: Series B. 2009;64(2):252–257. doi: 10.1093/geronb/gbn018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowling A, Barber J, Morris R, Ebrahim S. Do perceptions of neighborhood environment influence health? Baseline findings from a British survey of aging. Journal of Epidemiology and Community Health. 2006;60(6):476–483. doi: 10.1136/jech.2005.039032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowling A, Stafford M. How do objective and subjective assessments of neighborhood influence social and physical functioning in older age? Findings from a British survey of ageing. Social Science & Medicine. 2007;64(12):2533–2549. doi: 10.1016/j.socseimed.2007.03.009. [DOI] [PubMed] [Google Scholar]
- Byrnes M, Liehtenberg P, Lysack C. Environmental press, aging in place, and residential satisfaction of urban older adults. Journal of Applied Social Science. 2006;23(2):50–77. doi: 10.1177/19367244062300204. [DOI] [Google Scholar]
- Cernin PA, Lysack C, Lichtenberg PA. A comparison of self-rated and objectively measured successful aging constructs in an urban sample of African American older adults. Clinical Gerontologist: The Journal of Aging and Mental Health. 2011;34(2):89–102. doi: 10.1080/07317115.2011.539525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chadiha LA, Washington OGM, Lichtenberg PA, Green CR, Daniels KL, Jackson JS. Building a registry of research volunteers among older urban African Americans: Recruitment processes and outcomes from a community-based partnership. The Gerontologist. 2011;51(S1):S106–S115. doi: 10.1093/geront/gnr034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapleski E. Facing the future: 2002 city of Detroit needs assessment of older adults. Detroit, MI: Wayne State Institute of Gerontology, Center for Urban Studies, Center for Healthcare Effectiveness Research, University Press; 2002. A report for the city of Detroit Department of Senior Citizens. [Google Scholar]
- Cornwell B, Laumann EO, Schumm LP. The social connectedness of older adults: A national profile. American Sociological Review. 2008;73:185–203. doi: 10.1177/000312240807300201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corwin SJ, Laditka JN, Laditka SB, Wilcox S, Liu R. Attitudes on aging well among older African Americans and whiles in South Carolina. Preventing Chronic Disease. 2009;6(4):A113. doi: 10.1093/geront/gnp084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramm JM, van Dijk HM, Nieboer AP. The importance of neighborhood social cohesion and social capital for the well-being of older adults in the community. The Gerontologist. 2013;53(1):142–152. doi: 10.1093/geront/gns052. [DOI] [PubMed] [Google Scholar]
- Crum RM, Lillie-Blanton M, Anthony JC. Neighborhood environment and opportunity to use cocaine and other drugs in late childhood and early adolescence. Drug & Alcohol Dependence. 1996;43(3):155–161. doi: 10.1016/S0376-8716(96)01298-7. [DOI] [PubMed] [Google Scholar]
- Dennis BP, Neese JB. Recruitment and retention of African American ciders into community-based research: Lessons learned. Archives of Psychiatric Nursing. 2000;14(1):3–11. doi: 10.1016/s0883-9417(00)80003-5. [DOI] [PubMed] [Google Scholar]
- Duck W, Rawls A. Interaction orders of drug dealing spaces: Local orders of sense making in a poor black American place. Crime, Law, & Social Change. 2012;57(1):33–75. doi: 10.1007/s10611-011-9353-y. [DOI] [Google Scholar]
- Fothergill KE, Ensminger ME, Robertson J, Green KM, Thorpe RJ, Juon HS. Effects of social integration on health; A prospective study of community engagement among African American women. Social Science & Medicine. 2011;72(2):291–298. doi: 10.1016/j.socscimed.2010.10.024. doi: 10.1016/j.socseimed.2010.10.024PMCID: PMC3031118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hipp J. Tract levels effects of structural characteristics measured at the micro-neighborhood and tract levels. Urban Studies. 2010;47(12):2517–2536. doi: 10.1177/0042098009359950. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: A metaanalytic review. PLoS Medicine. 2010;7(7):e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husaini BA, Moore ST, Castor RS, Neser W, Whitten-Stovall R, Linn JG, et al. Social density, stressors, and depression: Gender differences among the Black elderly. Journal of Gerontology. 1991;46(5):P236–P242. doi: 10.1093/geronj/46.5.P236. [DOI] [PubMed] [Google Scholar]
- Idler E, Benyamini Y. Self-rated health and mortality: A review of twenty seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Jang Y, Borenstein-Graves A, Haley W, Small B, Mortimer J. Determinants of a sense of mastery in African American and White older adults. Journal of Gerontology, Series B. 2003;58(4):S221–S224. doi: 10.1093/geronb/58.4.S221. [DOI] [PubMed] [Google Scholar]
- Jorm AF. Social networks and health: It's time for an intervention trial. Journal of Epidemiology and Community Health. 2005;59:537–538. doi: 10.1136/jech.2004.031559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause N. Neighborhood deterioration, religious coping, and changes in health during late life. Gerontologist. 1998;38(6):653–664. doi: 10.1093/geront/38.6.653. doi: l0.1093/geront/38.6.653. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Nahemow L. Ecology and the aging process. In: Eisdorfer C, Lawton MP, editors. The psychology of adult development and aging. Washington, DC: American Psychological Association; 1973. pp. 619–674. [DOI] [Google Scholar]
- Lawton P, Rajagopal D, Brody E, Kleban M. The dynamics of care-giving for a demented elder among Black and White families. Journal of Gerontology: Social Sciences. 1992;47:S156–S164. doi: 10.1093/geronj/47.4.s156. [DOI] [PubMed] [Google Scholar]
- Lichtenberg PA, Cameron M, Duri's S, Ensberg M, Heidebrink J, Horst M, et al. Doing more with less: The Michigan Dementia Coalition. Generations: Journal of the American Society on Aging. 2009;33(1):60–64. [Google Scholar]
- Lysack C, Komanecky M, Kabel A, Cross K, Neufeld S. Environmental factors and their role in community integration after spinal cord injury. Canadian Journal of Occupational Therapy. 2007;74:243–254. doi: 10.1177/00084174070740S304. [DOI] [PubMed] [Google Scholar]
- Mahoney J, Drinka TJK, Alber R, Gunter-Hunt G, Matthews C, Gravenstein S, et al. Screening for depression: Single question versus GDS. Journal of the American Geriatric Society. 1994;42:1006–1008. doi: 10.1111/j.1532-5415.1994.tb06597.x. [DOI] [PubMed] [Google Scholar]
- Manly JJ, Byrd DA, Touradji P, Stern Y. Acculturation, reading level, and neuropsychological test performance among African American elders. Applied Neuropsychology: Adult. 2004;11(1):37–46. doi: 10.1207/s15324826an1101_5. [DOI] [PubMed] [Google Scholar]
- McColl MA, Davies D, Carlson P, Johnston J, Minnes P. The community integration measure: Development and preliminary validation. Archives of Physical Medicine & Rehabilitation. 2001;82:429–434. doi: 10.1053/apmr.2001.22195. [DOI] [PubMed] [Google Scholar]
- Mossey JM, Shapiro E. Self-rated health: A predictor of mortality among the elderly. American Journal of Public Health. 1982;72:800–808. doi: 10.2105/AJPH.72.8.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nieboer A, Lindenberg S, Boomsma A, Van Bruggen AC. Dimensions of well-being and their measurement; The SPF-IL Scale. Social indicators Research. 2005;73:313–353. doi: 10.1007/s11205-004-0988-2. [DOI] [Google Scholar]
- Osborne K, Ziersch A, Baum F, Gallaher G. Australian Aboriginal urban residents' satisfaction with living in their neighborhood: Perceptions of the neighborhood socio-cultural environment and individual socio-demographic factors. Urban Studies. 2012;49(11):2459–2477. [Google Scholar]
- Roth DL, Haley WE, Owen JE, Clay OJ, Goode KT. Latent growth models of the longitudinal effects of dementia caregiving: A comparison of African-American and white family caregivers. Psychology and Aging. 2001;16:427–436. [PubMed] [Google Scholar]
- Rowe JW, Khan RL. Successful aging. The Gerontologist. 1997;37(4):433–440. doi: 10.1093/geront/37.4.433. [DOI] [PubMed] [Google Scholar]
- Rowles GD. Place and personal identity in old age: Observations from Appalachia. Journal of Environmental Psychology. 1983;3:299–313. doi: 10.1016/S0272-4944(83)80033-4. [DOI] [Google Scholar]
- Stark S. Creating disability in the home; The role of environmental barriers in the United States. Disability and Society. 2001;16:37–49. doi: 10.1080/713662037. [DOI] [Google Scholar]
- Strawbridge WJ, Wallhagen MI, Cohen RD. Successful aging and well-being: Self-rated compared with Rowe and Kahn. The Gerontologist. 2002;42(6):727–733. doi: 10.1093/geront/42.6.727. [DOI] [PubMed] [Google Scholar]
- Wahl HW, Fänge A, Oswald F, Gitlin LN, Iwarsson S. The home environment and disability-related outcomes in aging individuals: What is the empirical evidence? The Gerontologist. 2009;49:355–367. doi: 10.1093/geront/gnp056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen M, Hawkley LC, Cacioppo JT. Objective and perceived neighborhood environment, individual SES and psychosocial factors, and self-rated health: An analysis of older adults in Cook County, Illinois. Social Science & Medicine. 2006;63:2575–2590. doi: 10.1016/j.socscimed.2006.06.025. [DOI] [PubMed] [Google Scholar]
- Yen IH, Michael YL, Perdue P. Neighborhood environment in studies of health of older adults: A systematic review. American Journal of Preventive Medicine. 2009;37(5):455–463. doi: 10.1016/j.amepre.2009.06.022. doi: 10.1016%2Fj.amepre.2009.06.022PMCID: PMC2785463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen I, Shim J, Martinez A, Barker J. Older people and social connectedness: How place and activities keep people engaged. Journal of Aging Research. 2012 doi: 10.1155/2012/139523. Article ID 139523 10 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yochim B, Mast B, Lichtenberg P. Cerebrovascular risk factors and depressed mood in inner city older adults. Clinical Psychologist. 2003;7:11–20. doi: 10.1093/gerona/59.12.1290. [DOI] [Google Scholar]