Abstract
Ebolaviruses naturally infect a wide variety of cells including macrophages and dendritic cells, and the resulting cytokine and interferon-α/β responses of infected cells are thought to influence viral pathogenesis. The VP35 protein impairs RIG-I-like receptor dependent signaling to inhibit interferon production, and this function has been suggested to promote the ineffective host immune response characteristic of ebolavirus infection. To assess the impact of VP35 on innate immunity in biologically relevant primary cells, we used a recombinant Newcastle disease virus encoding VP35 (NDV/VP35) to infect macrophages and conventional dendritic cells, which primarily respond to RNA virus infection via RIG-I like pathways. VP35 suppressed not only IFN but also TNF-α secretion, which are normally produced from these cells upon NDV infection. Additionally, in cells susceptible to the activity of VP35, IRF7 activation is impaired.
In contrast, NDV/VP35 infection of plasmacytoid dendritic cells, which activate IRF-7 and produce interferon through TLR-dependent signaling, leads to robust interferon production. When plasmacytoid dendritic cells deficient for TLR signaling were infected, NDV/VP35 was able to inhibit interferon production. Consistent with this, VP35 was less able to inhibit TLR-dependent versus RIG-I-dependent signaling in vitro. These data demonstrate that ebolavirus VP35 suppresses both interferon and cytokine production in multiple primary human cell types. However, cells that utilize the TLR pathway can circumvent this inhibition, suggesting the presence of multiple viral sensors enables the host to overcome viral immune evasion mechanisms.
Keywords: Ebolavirus, dendritic cell, IRF7 interferon
Introduction
Ebolaviruses, which cause systemic viral infections that lead to severe hemorrhagic fever, infect a wide variety of cell types in vivo.1–3 Antigen presenting cells, particularly macrophages and dendritic cells, have been implicated as early targets of infection that play important roles in viral pathogenesis.1, 4 For example, ebolavirus infection of macrophages results in proinflammatory cytokine and tissue factor production, responses that may attract to sites of infection additional target cells, promote endothelial permeability and activate coagulation cascades.1 Ebolavirus infection of dendritic cells (DCs) does not result in their full activation, and this may contribute to insufficient or ineffective immune response observed in cases of fatal infections.5
An important attenuator of host responses to ebolavirus infection is the VP35 protein. The essential role for VP35 in pathogenesis is highlighted by the mild disease phenotype and attenuated replication observed in mice and guinea pigs infected with ebolaviruses encoding mutated VP35s.6–8 Initial studies demonstrated that this viral protein targets the RIG-I signaling pathway, preventing activation of IRF3 and production of interferon-α/β (IFN) from infected cells.9–11 Subsequent in vitro experiments have shown that VP35 inhibits the activity of the IRF3/7 kinases IKKε and TBK1,12, 13 which lie in the RIG-I pathway. In addition, structural studies demonstrate that VP35 can compete with RIG-I for binding to double-stranded RNA, precluding the proper recognition and response to virus replication.14, 15
RIG-I is a cytoplasmic sensor of viral infection that is essential for the induction of IFN in fibroblasts and conventional dendritic cells (cDCs),16 but not in plasmacytoid dendritic cells (pDCs). Cytokine production normally elicited in response to infection with negative strand RNA viruses such as Sendai, Newcastle disease virus, VSV and influenza A is reduced in cells from RIG-I knock-out cells.17 The RIG-I pathway is also crucial for ebolavirus replication as demonstrated by the fact that activation of RIG-I prior to infection greatly suppresses ebolavirus infection.18 Thus, the ability of VP35 to interfere with RIG-I binding to virus derived RNA or to inhibit the downstream kinases could explain the ability of ebolavirus to suppress IFN production from infected cells.
In spite of VP35 IFN suppressing functions, the sera from some individuals infected with ebolavirus contain high levels of IFN-α,19, 20 and experimentally infected animals upregulate interferon induced genes.7, 21 One possible explanation for this apparent contradiction is that some cell type(s) overcome or evade the VP35 IFN suppression function to produce IFN in response to infection.22 In light of the aforementioned studies demonstrating the inhibitory effect of the ebolavirus on immune functions, we sought to determine the extent to which the VP35 protein can inhibit IFN-α/β production in primary human monocytes, macrophages and dendritic cells, and to what extent VP35 may also modulate expression of other immune mediators produced by these cells.
In our experimental system, cDCs respond to NDV infection with robust IFN and TNF-α production and express several interferon-induced genes (ISGs). We observed that while monocytes, macrophages, and cDCs show an impaired ability to produce IFN when infected with NDV/VP35, pDCs produce large amounts of IFN when infected with the same virus, suggesting that this DC subset may resist the IFN inhibitory action of ebolavirus.
In cell types that exhibit impaired IFN production in the presence of VP35, we observe a lack of phosphorylation and nuclear translocation of IRF7, a key regulator of IFN production. Our results confirm the importance of the RLR pathway in response to viral infection, and suggest that a proinflammatory response may contribute to viral suppression. This study also demonstrates that cellular heterogeneity of the immune system provides non-redundant signaling pathways that act to circumvent the effect of viral antagonists of the innate immune response.
Results
Expression of Ebolavirus protein VP35 reduces the IFN normally produced upon NDV infection
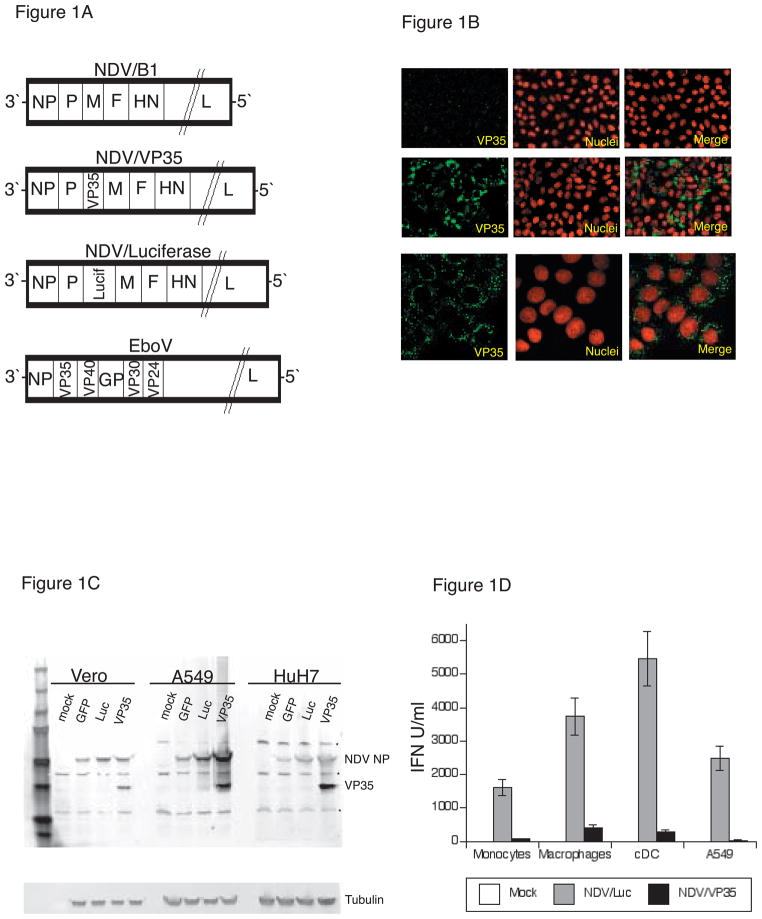
Newcastle disease virus has been shown to be an excellent tool to study the induction of the antiviral response in dendritic cells.23–28 NDV serves as a model negative-strand RNA virus of relevance to ebolavirus as both paramyxoviruses and filoviruses produce nucleic acid species that trigger an anti-viral response through the RIG-I like receptor (RLR) pathway.29 An advantage of NDV is that, unlike ebolaviruses, experiments using the recombinant, avirulent NDVs can be conducted under BSL2 conditions. It is also noteworthy that, because NDV is an avian virus, it does not naturally encode effective inhibitors of the human innate immune pathways.30 Because of these properties, we utilized the NDV reverse genetics system to generate a model negative-strand RNA virus encoding the filoviral protein VP35 (NDV/VP35). The structure of the resulting NDV/VP35 genome, as well as other recombinant NDVs used in this study are shown in Figure 1A. NDV encoding firefly luciferase (NDV/Luc) was used as a comparison throughout this study.31, 32
Figure 1. Ebolavirus protein VP35 reduces the IFN normally produced upon NDV infection.
A. Genome organization of NDVs used in this study
B. Vero cells infected with NDV/VP35 were fixed and stained for the expression of the Ebola VP35 protein (green) and nuclei (red). Top rows: 1 h after infection; middle rows: 24 h after infection. Bottom row: Confocal images of NDV/VP35 infected Vero cells 24 h after infection.
C. Tissue culture cells were infected with various NDVs at MOI 2 and lysed 20–24 hpi. Lysates were analyzed for the expression of NDV NP and Ebola VP35 by Western blot.
D. Primary immune cells and A549 cells were infected with NDVs at MOI 2. At 20 hpi, supernatants were analyzed for IFN by bioassay as described in Methods and Materials. GFP = NDV/GFP, Luc = NDV/Luciferase, VP35 = NDV/VP35. (*) indicates non-specific bands from the rabbit polyclonal antibody raised against NP.
Infection of Vero cells with NDV/VP35 resulted in expression of VP35 in the cytoplasm, with prominent punctae in some cells (Figure 1B), which is similar to the reported subcellular location of VP35 expressed from ebolavirus.33, 34 Western blot analysis revealed similar amounts of NDV NP protein in Vero cells infected with NDV/Luc and NDV/VP35 (Figure 1C), demonstrating that the two viruses are replicating to the same degree in these cells. NDV/Luc and NDV/VP35 infection of HuH7 cells also resulted in similar amounts of NDV NP expression. However, when A549 cells, which were used as a representative non-immune cell that can mount and IFN-α/β response to infection and that is readily infected with ebolavirus, 18 were infected under the same conditions as Vero and HuH7 cells, NDV/VP35 infected cells had significantly greater amounts of NP protein than NDV/Luc infected cells. Infection with a third virus, NDV/GFP, resulted in similar amounts of NP expression in Vero, A549 and HuH7 cells. These results are consistent with the inability of Vero and HuH7 cells to produce IFN in response to NDV infection,35, 36 rendering these cells unable to interfere with the replication of NDV/Luc and NDV/VP35. In contrast, A549 cells normally produce IFN after infection,37 which would suppress the replication of NDV.
The enhanced expression of NDV NP from NDV/VP35 indicated enhanced replication and suggested that VP35 was preventing IFN production. We therefore performed a bioassay to measure the amount of IFN produced from NDV infected A549 cells. The supernatants of A549 cells infected with NDV/Luc contained approximately 70-fold more IFN than supernatants from A549 cells infected NDV/VP35 (Figure 1D). The bioassay results agree with previous reports demonstrating that exogenously expressed VP35 can inhibit the production of IFN in response to such stimuli as virus infection and double stranded RNA.10, 11, 38, 39 Based on these results, we conclude that the VP35 protein can function as an inhibitor of IFN production when expressed within the context of a negative-strand RNA virus infection, promoting replication of the virus in IFN competent cells.
VP35 inhibits IFN and TNF-α production in NDV infected cDCs
Since immune cells of the monocytic lineage have been shown to be early targets of ebolavirus infection, we infected human monocytes, and monocyte-derived macrophages and dendritic cells with NDV/VP35 and determined the levels of IFN produced by these cells. In all three primary cell types, NDV/LUC infection led to robust IFN production, but in contrast, NDV/VP35 infection gave only small amounts of IFN from the same cells, demonstrating the capability of VP35 to function in biologically relevant primary human antigen presenting cells (Figure 1D). We next examined the temporal response of cDCs (obtained from two different human donors) to infection with NDVs. In the first 8 hpi, cDCs infected with either NDV/Luc or NDV/VP35 produced a small amount of IFN (~200 U/ml). After 12 hpi, cDCs infected with NDV/Luc produced an excess of 1500 U/ml of IFN, whereas cDCs infected with NDV/VP35 produced less than 300 U/ml (Figure 2A). QPCR analysis confirmed that the induction of IFN alpha and IFN beta transcripts seen in NDV/Luc infection was absent in NDV/VP35 infection (Supplemental Figure S1A). However, we did not observe significant induction of IFN-γ, IL6 or IL8 from cDCs infected with either virus (Supplemental Figure S1B).
Figure 2. Conventional dendritic cells (cDC) infected with NDV/VP35 produce low amounts of IFN and TNF-α.
A. cDC were infected with the indicated NDV at MOI 2, and analyzed for IFN using a bioassay (n=4). B. cDC from two different human donors (donor A, open symbol; donor B, closed symbol) were infected with either NDV/Luc (squares) or NDV/VP35 (circles). At the indicated time, supernatants were separated from cells and analyzed for IFN by bioassay. P < 0.01 (Student’s t-test).
B. Supernatants obtained in 2A were analyzed for TNF-α by ELISA. P < 0.01 (Student’s t-test).
We also observed an induction of RANTES, MIP-1β (Supplemental Figure S1B) and TNF-α in NDV/Luc infected cells, but not in NDV/VP35 infected cells. ELISA analysis confirmed that there was less secretion of TNF-α in cells infected with NDV/VP35 (Figure 2B, Supplemental Figure S1A). These results demonstrate that VP35 is not only an inhibitor of IFN secretion from cDCs; VP35 can also inhibit the normal production of chemokines and select proinflammatory cytokines from cDCs in response to viral infection.
Plasmacytoid dendritic cells (pDCs) require functional TLR signaling to produce IFN in response to NDV/Luc and NDV/VP35 infection
Although the suppression of IFN production in cDCs infected with ebolavirus has been observed in ex vivo infections, high levels of IFN in the sera of humans and non-human primates infected with ebolavirus have been reported.4, 19–21, 40 Since our results demonstrated that NDV/VP35 was able to suppress IFN from cDCs and macrophages, which rely on the RLR pathway to activate IRF7 in response to virus infection,41 we hypothesized that pDCs might be insensitive to the effect of VP35 since these dendritic cells can produce IFN using the TLR pathway. Therefore, we examined the IFN response of pDCs to our recombinant NDVs.
At 20 hpi, cDCs infected with NDV/Luc produced approximately 6000 U/ml of IFN, while cDCs infected with NDV/VP35 produced less than 500 U/ml under the same conditions. However, infection of pDCs with either NDV/Luc or NDV/VP35 resulted in a rapid and robust IFN production within 8 hpi (Figure 3A). At 20 hpi, pDCs produced an excess of 100,000 U/ml of IFN irrespective of the virus, demonstrating that the NDV/VP35 virus was unable to inhibit the rapid and robust pDCs response to viral infection. We confirmed that both cDCs and pDCs were infected and expressing VP35 using immunofluorescent microscopy (Supplemental Figure S2A, B).
Figure 3. The TLR signaling pathway is resistant to the inhibitory effect of VP35.
A. cDCs (left panel) and pDCs (right panel) were infected with NDV/Luc (square), or NDV/VP35 (circles), and at the indicated time points, supernatants were harvested and analyzed for IFN by bioassay. The data shown is representative of results obtained from two independent experiments.
B. pDCs and CD11b+ cells from wild-type or TLR3/MyD88 deficient mice (KO) were infected with NDVs. Supernatants were harvested 23 hpi and analyzed for murine IFN-α by ELISA.
C. 293xl/TLR7 cells were transfected with either a NFκB (left panel) or IFN-β luciferase (right panel) reporter plasmid and assayed for TLR activation (following Imiquimod treatment) or RLR activation (RIG-I CARD transfection) in the presence of varying amounts of co-transfected VP35. Imiquimod treatment, triangles; RIG-I CARD co-transfection, squares; mock activation, circles.
To determine if the presence of the TLR signaling pathway in pDCs is responsible for the ability of these cells to circumvent the inhibitory action of VP35, we infected pDCs from MyD88 and TLR3 double-knockout mice (DKO), or wild-type mice, and measured their interferon response. As we observed with human monocytes and macrophages, NDV/VP35 is able to inhibit the IFN production from infected murine CD11b positive cells, which include monocytes and macrophages. These cells of the monocytic lineage presumably lack TLR7, and use the RLR pathway to produce IFN in response to viral infection.41 Infection of wild-type pDCs with either NDV/Luc or NDV/VP35 resulted in greater than 2000 pg/ml of IFN-α, demonstrating the inability of VP35 to suppress IFN production in murine pDCs (Figure 3B). However, when TLR-deficient pDCs were infected with NDV/VP35, significantly less IFN-α was produced when compared to NDV/Luc infected cells, suggesting the TLR pathway allows pDCs to bypass the inhibition caused by VP35.
The results thus far are consistent with previous findings identifying VP35 as an inhibitor of the components of the RLR pathway. To test if VP35 was able to inhibit the TLR pathway, we used an immortalized HEK cell line stably expressing human TLR7, which responds to imiquimod (IMQ) by activating the NFκB pathway. We hypothesized that VP35 would be able to inhibit the activation of the RLR pathway, but not the TLR pathway in this cell line. Transient transfection of these cells with a constitutively active RIG-I construct (RIG-I/CARD) led to activation of an IFN-β promoter driven luciferase reporter, and this activation is inhibited in a dose-dependent manner by co-transfection with VP35 (Figure 3C, Right Panel). In contrast, the same amount of transfected VP35 only slightly reduces NFkB-luciferase reporter activity after IMQ treatment (Figure 3C, Left Panel). Thus, under this experimental system, the RLR pathway appears to be substantially more sensitive to VP35 than the TLR pathway.
NDV/VP35 infection of cDCs results in the expression of interferon induced genes (ISGs)
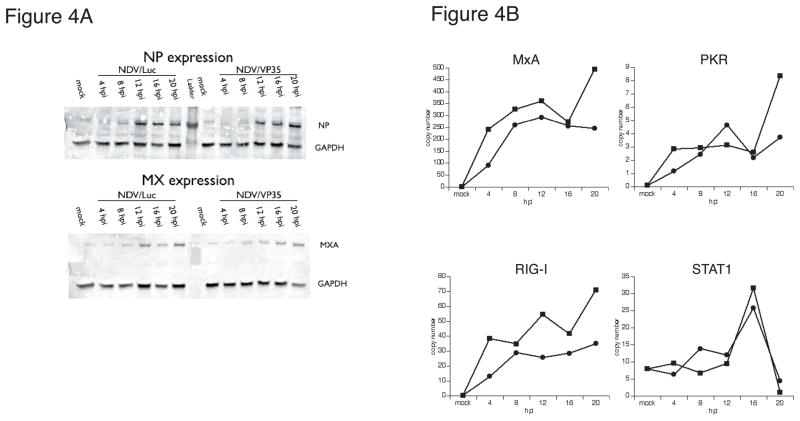
Although NDV/VP35 infection elicited smaller amounts of IFN in cDCs compared to cells infected with NDV/Luc, there were still modest levels present. Therefore, we examined the infected cells for the induction of ISGs. Lysates of infected cells were analyzed by Western blot for the presence of the MxA protein, which is known to be induced by IFN. In cDCs infected with either NDV/Luc or NDV/VP35, the MxA protein was detectable at 12 hpi, suggesting the small amounts of IFN produced during the first 8hpi was sufficient to induce MxA expression (Figure 4A). This interpretation is further supported by QPCR analysis, which revealed that in addition to MxA, NDV/LUC and NDV/VP35 infection led to the induction of ISGs such as PKR, RIG-I, and STAT1 (Figure 4B). We conclude that in the context of our experimental infections, the Ebola VP35 protein inhibits the bulk of IFN production, as well as TNF-α secretion, but does not prevent ISG induction.
Figure 4. Conventional dendritic cells (cDC) infected with NDV/VP35 express IFN-stimulated genes.
A. Cell pellets from infected cDC were lysed and analyzed for NDV NP and MxA protein expression by Western blot.
B. Total RNA from aliquots of the cell pellets from 4 was analyzed by qPCR for MxA, PKR, RIG-I and STAT1 expression. Relative copy numbers are shown in the ordinate axes, and were computed as described in Material and Methods. NDV/Luc infection: squares; NDV/VP35 infection: circles.
VP35 inhibits the activation, but not the expression of IRF7 in NDV infected cells
Since VP35 did not inhibit the induction of IFN stimulated genes such as MxA, we asked if the expression of the transcription factor IRF7 was impaired in NDV infected cDCs. Since robust IFN production requires the expression and activation of IRF7, one simple explanation for the loss of most, but not all IFN from cDC infected with NDV/VP35 is that the ~200 units/ml of IFN produced during the first ~5 hours of infection was insufficient to elicit IRF7 expression. We therefore examined the expression of IRF7 before and after NDV/VP35 infection of cDCs.
Prior to infection, IRF7 is not detectably expressed in cDC, but is present in pDCs (Figure 5A). After infection for 20h with either NDV/Luc or NDV/VP35, we observed similar levels of IRF7 expression between NDV/Luc and NDV/VP35 infected cells (Figure 5B). Western blot analysis showed that cDCs infected with either virus expressed IRF7 with kinetics similar to MxA (Figure 5C). Both IRF7 and MxA appear prominently by 10hpi, consistent with their induction after IFN production. From these data, we conclude that, in this system, the suppression of robust IFN production from cDCs by VP35 is not due to a suppression of IRF7 expression relative to the NDV/Luc control.
Figure 5. IRF7 is absent in cDC, but is expressed after NDV infection.
A. cDCs (top row) and pDCs (bottom row) were fixed with paraformaldehyde ad analyzed for IRF7 expression by immunostaining. Images were acquired with a 63x oil objective on a Leica SP5 confocal microscope.
B. NDV/Luc (top) or NDV/VP35 (bottom) infected cDC were fixed onto coverslips at 8 hpi and analyzed for the expression of NP and IRF7 by immunostaining. Images were acquired with a 63x oil immersion objective on Leica SP5 laser scanning confocal microscope.
C. cDCs infected with NDVs were harvested at the indicated time points and analyzed for MxA, IRF7 (left), GAPDH and NDV NP (right) expression by Western blot. (*) indicates non-specific bands from the rabbit polyclonal antibody raised against NP.
At this point our results are consistent with the 2-step model of IFN production42–44 in which NDV triggers activation of the RLR pathway within 4 hours of infection, leading to a low level of IFN production and subsequent expression of ISGs, including IRF7. Sometime after 8hpi, IRF7 is activated, leading to a second, more robust IFN production. Based on the kinetics of IFN production from NDV infected cDCs (Figure 2A), we hypothesized that NDV/VP35 suppressed the IRF7-dependent production of IFN.
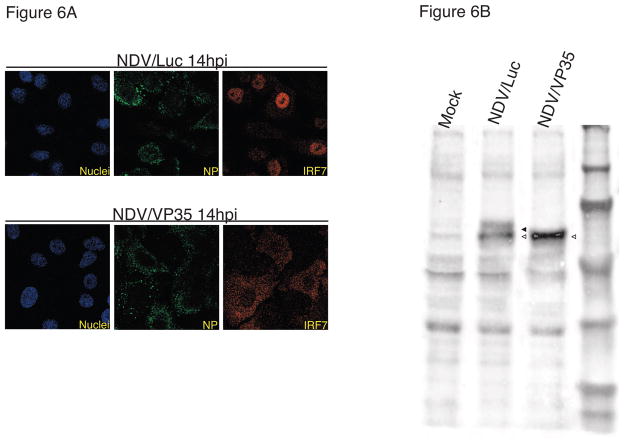
Since we did not observe a loss of IRF7 expression in cDC infected with NDV/VP35, we hypothesized that VP35 might prevent the activation of IRF7. We tested this hypothesis using A549 cells, which we have shown to behave similarly to cDC with respect to IFN production in response to NDV infection. Confocal microscopy of A549 cells revealed a clear nuclear localization of IRF7 14 hpi with NDV/Luc, but this is not observed in NDV/VP35 infected cells (Figure 6A). To further analyze the activation state of IRF7, we performed Western blot analysis of cells infected for 15 hours. In cells infected with NDV/Luc, we observed the induction of IRF7, as well as a higher molecular weight band that is consistent with a phosphorylated IRF7.45, 46 This higher molecular weight band is absent in cells infected with NDV/VP35 (Figure 6B). Taken together these data suggest that VP35 inhibits IRF7 activation, suppressing IFN production.
Figure 6. IRF7 activation is inhibited by VP35.
A. A549 cells were NDV/Luc infected (top panels) or NDV/VP35 infected (bottom panels), fixed and stained for the expression of NDV NP (green) and IRF7 (red).
B. A549 cells infected with NDVs were lysed 15 hpi and analyzed for IRF7 by Western blot. The position of IRF7 (empty arrowhead) and p-IRF7 (filled arrowhead) are shown.
Discussion
Production of IFN by dendritic cells and the subsequent induction of ISGs are critical early responses to viral infection. Recognition of the single stranded RNA genomes of negative-stranded viruses, such as ebolavirus, can be mediated by TLRs in the plasma membrane or endosomes, or by RLRs in the cytosol, which also detect the viral mRNA produced after virus entry and replication.47–51 These independent pathways both result in the phosphorylation of IRF3 and/or IRF7, which, in combination with ATF2/c-jun and NFκB, create a transcription complex that binds to IFN promoters, leading to IFN production. In the case of negative strand RNA viruses and cDCs, IFN production is currently thought to result from the recognition of cytosolic viral RNA by RIG-I, ultimately leading to the activation of TBK1/IKKε.52 These kinases in turn phosphorylate the transcription factor IRF3 and/or IRF7. In pDCs, viral nucleic acids are recognized by endosomal TLR7, which signal through MyD88 to activate either IKKa or IRAK1, which phosphorylate IRF747, 51 (Figure 7). It is also possible for pDCs to use the RIG-I pathway to recognize and respond to viral mRNA.
Figure 7. The TLR pathway allows pDCs to overcome the VP35 interferon evasion function.
Endosomal TLR7 in pDCs can bind single-stranded RNA (including, but not limited to viral genomes), and trigger a MyD88 dependent kinase cascade that leads to the activation of IRF7. The kinases IRAK1 and IKKα are the kinases that directly phosphorylate IRF7, which then translocates to the nucleus to bind the IFN promotors. pDC can produce IFN rapidly and in large quantities due in part to 1) the ability of the sensor (TLR7) to detect pathogen associated molecules even in the absence of viral replication, and 2) the constitutive expression of IRF7.
Cytosolic RIG-I binds to ssRNA or dsRNA with 5′-triphosphates, most likely the product of viral transcription, leading to the activation of the IRF3/7 kinases TBK1 and IKKε. RIG-I can also trigger IFN production in response to double-stranded RNA, a structure that may exist as part of viral replication. Prior to infection, cDC do not express IRF7 until IFN (produced either by the cDC itself in response to viral infection, or by neighboring cells) triggers its production. Phosphorylation and nuclear translocation of IRF7 thus occurs several hours after viral infection.
When a virus encoding VP35 infects cDCs, the time required by the virus to synthesize the protein allows the immune cell to produce IFN and begin the synthesis of ISGs, including IRF7. Once expressed, VP35 inhibits the kinase activity of IKKε or TBK1, preventing the activation of IRF7. It is also possible that VP35 interferes with the interaction between viral RNA and RIG-I, preventing the detection of viral infection. The failure of VP35 to suppress IFN production from pDCs could be due to its inability to inhibit IKKα or IRAK1.
We demonstrate that virally expressed ebolavirus protein VP35 inhibits a significant portion of the IFN produced by cDCs, but not pDCs. The inhibition in cDCs reflects the suppression of the RLR pathway, either at the level of RIG-I, or the downstream kinases. The absence of inhibition in pDCs could be due to the constitutive expression of IRF7 in pDCs, or the inability of VP35 to inhibit the IRF7 kinases in pDCs. In either case, our results suggest that TLR sensing pathways present in some cells, such as pDCs, can overcome the IFN antagonism of VP35. Since pDCs are not as potent as cDCs in inducing proliferation of naive T cells, this could also explain the paradoxical observation of IFN production without antibody production in some cases of fatal ebolavirus infection.19, 20
The mechanism(s) by which VP35 inhibits IFN production remains an active area of investigation. A recent study concludes that VP35 can enhance the SUMOylation of IRF7,38 leading to suppression of its ability to activate IFN gene transcription. Our data do not exclude a role for IRF7 SUMOylation in inhibition of IRF7-dependent transcription, but they clearly indicate that VP35 inhibits IRF7 activation. If the SUMOylation pathway were active in both cDCs and pDCs, VP35 would be expected to suppress IFN production from both dendritic cell types. However, as we have shown, NDV/VP35 infection of pDCs results in robust IFN production, which could be explained if VP35 blocks the action of TBK1/IKKε, but not IRAK1/IKKα, which serve as the kinases for IRF7 in pDCs (Figure 7). Consistent with our model of IFN suppression by VP35, transgenic mice deficient for components of the RLR pathway also have impaired IFN production from cDCs infected with NDV, yet pDCs from these animals respond with robust IFN production when infected under the same conditions.16 Additional studies will be necessary to unequivocally determine the mechanisms by which VP35 suppresses IFN production.
The ability of VP35 to suppress the IFN production in cDCs was previously demonstrated using recombinant Venezuelan equine encephalitis virus replicon particles (VRP). Infection of cDCs with VRP encoding VP35 completely inhibited secretion of IFN-α compared to VRP encoding GFP.53 Our results show that VP35 inhibits most, but not all IFN secretion from cDCs, and does not prevent the induction of ISGs. This difference could be explained by the timing of the expression of VP35 relative to the initial induction of IFN in response to viral infection in cDCs. In the case of our negative strand RNA virus, uncapped viral RNA is produced within 3 hours after infection, presumably resulting in the activation of the RIG-I pathway. However, due to the transcriptional gradient inherent within paramyxoviruses, much less VP35 mRNA, and consequently VP35 protein, will be expressed at this point. In contrast, we suspect that VRPs are able to produce sufficient VP35 early during viral transcription. It is also possible the VRP transcript is not recognized by RIG-I,54 further delaying the induction of IFN, allowing VP35 to accumulate to sufficient inhibitory levels. Thus, in the case of VRP infection of cDCs, the rapid expression of VP35 would inhibit the early, small production of IFN, as well as the ensuing ISG induction. In the case of NDV infection, the encoded VP35 is expressed after the initiation of the RIG-I pathway, which may be similar to the events that occur during ebolavirus infection. It is noteworthy that, despite the incomplete inhibition of IFN responses early in infection, effective inhibition of IRF7 activation later in infection is sufficient to substantially impair the antiviral effects of the IFN system.
In addition to inhibiting the production of IFN, VP35 also inhibits the production of TNF-α and other inflammatory cytokines such as RANTES and MIP-1β from NDV infected cells. Interestingly, TNF-α production from human primary immune cells in response to myxoma virus infection has been shown to be dependent upon signaling through the RLR pathway46 and more importantly, to act synergistically with IFN to restrict virus replication. A role for TNF-α in counteracting ebolavirus infection is consistent with the observation of transient inflammatory cytokine and chemokine production from asymptomatically infected individuals.55, 56 In the 1996 outbreak in Gabon, non-fatally infected individuals had high concentrations of TNF-α, IL6, and IL1-β, as well as chemokines MIP1α/β and MCP, 7 days after exposure to ebolavirus. Of note, this inflammatory response, which lasted for 2–3 days, was absent in the fatal cases of infection, suggesting that an early inflammatory response is protective against ebolavirus infection. This may be due in part to the ability of TNF-α to impair the entry of Ebolavirus into cDCs.57
Our findings identify monocytes, macrophages and dendritic cells as the cell types that are susceptible to the inhibitory effect of VP35, and also point to pDCs as a source of IFN production in some cases of ebolavirus infection. The consequences of selective inhibition of these cells of the innate immune response is unclear, but may contribute to the inappropriate activation of other cell types such as neutrophils and T cells, leading to a pathogenic cytokine response. Future studies using reverse-engineered viruses, such as our NDV system, will clarify the mechanisms of deregulated immune response to infection, which is a feature common to viral hemorrhagic fevers caused by pathogens such as Lassa, Marburg, and Ebola viruses.
Experimental Procedures
Reagents and Antibodies
General lab reagents were purchased from Sigma (St. Louis, MO), unless otherwise specified. A mouse antibody (IgG2a, clone 6C5) recognizing Zaire ebolavirus VP35 was generated in collaboration with the Mount Sinai Hybridoma Center. Antiserum from rabbits immunized with formalin-treated NDV was provided by the laboratory of Peter Palese (Mount Sinai School of Medicine, MSSM). Rabbit antibodies raised against a synthetic NDV NP peptide (RSQGQPEAGDGETQC) were purchased from Genscript (Piscataway, NJ). Mouse IgG2a recognizing the MxA protein was provided by Georg Kochs (University of Freiburg, Freiburg, Germany). Mouse IgG2a raised against human IRF7 was purchased from Santa Cruz Biotechnology (catalog # 74472, Santa Cruz, CA). Mouse and rabbit antibodies recognizing GAPDH were purchased from Abcam (Cambridge, MA). Fluorochrome conjugated antibodies were purchased from Invitrogen (Carlsbad, CA).
Cell Lines
The immortalized cells lines A549 (human lung adenocarcinoma) and Vero (African Green monkey kidney) were obtained from ATCC (Manassas, VA) and propagated according to the supplier’s recommendations. HuH7 cells (human hepatocarcinoma) were provided by the DiFeo Lab (MSSM) and cultured with 10% FBS in DMEM. 293xl/TLR7 cells were obtained from Invivogen (San Diego, CA) and cultured according to the supplier’s recommendations.
Preparation of primary immune cells
Human immune cells
CD14+ monocytes were obtained using the CD14+ selection kit from Miltenyi Biotec (Auburn, CA) starting with buffy coats (the leukocyte fraction of whole blood) provided by the New York Blood Center (Long Island City, NY). To generate cDCs, monocytes were cultured in RPMI (Invitrogen, Carlsbad, CA) supplemented with 4% human AB serum (Cambrex, Rockland, ME), 10 mM sodium pyruvate, 10 mM L-glutamine, 500 U/ml of IL-4 (Peprotech, Rocky Hill, NJ) and 500 U/ml of GM-CSF (Peprotech, Rocky Hill, NJ) at a density of 0.75 × 106 cells/ml. Typically, we obtained 6–8 × 106 cDCs from a 30 ml culture after 5 days. To generate macrophages, CD14+ monocytes were cultured in RPMI supplemented with 10% fetal bovine serum (Invitrogen, Carlsbad, CA) and 500 U/ml of M-CSF (Peprotech, Rocky Hill, NJ) for 10–14 days. To isolate pDC, a BDCA4 isolation kit from Miltenyi Biotec (Auburn, CA) was used, starting with buffy coats as the source material. pDCs were used immediately after isolation.
Murine immune cells
Murine pDCs and CD11b positive cells were isolated from mouse splenocytes using the mPDCA4 or CD11b positive selection kits, respectively (Miltenyi Biotec, Aurburn, CA). Cells were used within 4 hours after isolation. Experiments with mice were conducted under institutional guidelines from the Mount Sinai School of Medicine Institutional Animal Care and Use Committee.
Recombinant NDV
The NDV B1 (Hitchner strain) with a mutation to prevent the expression of the V protein30 was used to generate the VP35 recombinant virus (NDV/VP35) employed in this study. For the construction of the rescue plasmid encoding NDV/VP35, PCR primers were used to generate a cDNA encoding VP35 along with NDV virus gene end and gene start sequences flanked by NheI restriction sites (sense primer: 5′-GCG CGC TAG CTT AGA AAA AAT ACG GGT AGA AGT GAA ACT AGT CCG CCA CCA TGA CAA CTA GAA CAA AGG GCA GG-3′; antisense primer: 5′-CGC GGC TAG CCG TCA TCA AAT TTT GAG TCC AAG TGT TTT-3′). A pcDNA3 plasmid expressing Zaire ebolavirus (strain Mayinga) VP35 was used as the PCR template. The corresponding PCR product was ligated into the pGEM-T vector (Promega, Madison, WI) and transformed into competent cells. Individual clones were identified and used to produce the plasmid, which was then digested with NheI. The gel purified insert was then ligated to the NDV B1 plasmid, which had been digested with XbaI and CIP. The resulting rescue plasmid was used to generate recombinant NDV using a previously published procedure. The NDV virus expressing firefly luciferase (NDV/Luc) was provided by Adam Vigil of the Garcia-Sastre lab (Mount Sinai School of Medicine). Production of the NDV virus expressing GFP (NDV/GFP) has been previously described.30 All NDVs were propagated in 10-day old embryonated chicken eggs. NDV titers were determined by infecting Vero cells with serial dilutions of the virus. Fluorescent focus forming units were counted after fixation and staining for the NDV NP protein using a rabbit antibody against NP and Alexa 488 conjugated goat anti-rabbit antibodies.
Viral infection
Monocytes, cDCs and pDC were harvested by centrifugation at 200xg, and then rinsed once with DMEM containing 0.2% BSA (BSA/DMEM). The supernatant was removed and replaced with the NDV diluted in BSA/DMEM. We used a final volume of 100 ul per 106 for infection of cells in suspension. For mock infections, allantoic fluid was used. Cells were incubated for 45 mins at 37°C and then diluted to a final density of 1×106 cells per ml using RPMI containing 4% human sera (for cDCs and pDC), or RPMI containing 10% FBS (for monocytes).
For adherent tissue culture cells and macrophages, cell monolayers were rinsed with BSA/DMEM, and incubated with NDV diluted in BSA/DMEM. After 1 h at 37°C, the inoculum was removed and replaced with tissue culture medium (tissue culture cells), or RPMI containing 10% FBS (macrophages).
Interferon Bioassay, ELISA
Tissue culture supernatants were UV irradiated for 10 mins on ice to inactivate virus. Two-fold serial dilutions were prepared, and then transferred onto Vero 76 cells cultured in 96 well plates (Costar catalog # 3904, Corning, NY). Some cells were incubated with 2-fold dilutions of IFN-β (PBL, Piscataway, NJ), and were used to generate a standard dose-response curve. After incubating in a 5% CO2 incubator at 37°C for 14–16 hours, the supernatants were removed and the cells were infected with NDV/GFP at MOI 4. After 20–24 h, the cells were fixed with 4% PFA in PBS, and then rinsed with PBS. GFP fluorescence was measured using a Beckman DTX880 microplate reader (Beckman Coulter, Fullerton, CA). Linear regression using the curve fitting function of ImageJ (NIH, Bethesda MD) was used to convert GFP intensity into IFN units. Although we used IFN-β as our standard, the tissue culture supernatants presumably contain a mixture of interferon-α/β, and thus we report “IFN units”, and not IFN-β units in our results.
Human TNF-α was measured using the Ready-Set-Go kit from Ebioscience (San Diego, CA) following the manufacturer’s recommended protocol. Murine IFN-α was measured using the Verikine Mouse IFN ELISA kit from PBL (Piscataway, NJ).
Immunofluorescent microscopy
Dendritic cells (pDC and cDC), which are typically non-adherent, were suspended in cold PBS at a concentration of 2 ×106 cells/ml and placed onto poly-L-lysine coated 12 mm diameter glass coverslips. After incubating at 37°C for 10–20 mins, the cells became adherent, and were fixed with 4% PFA in PBS. For adherent cells (A549, Vero and macrophages), cells were cultured directly on 12 mm glass coverslips and fixed with 4% PFA in PBS. After rinsing cells with PBS, coverslips were permeabilized by incubating in 0.2% Triton X-100 in PBS for 10 mins at ambient temperature, and then incubated with blocking buffer (PBS containing 4% human IgG, 2% goat IgG (both IgG were purchased from Jackson Immunoresearch, West Grove, PA), 0.5% BSA and 20 mM glycine) for 30–60 mins. The longer incubation times were required to block non-specific binding of antibodies by the Fc receptor of primary immune cells. Primary antibodies were diluted in blocking buffer and used as follows: 1) rabbit polyclonal raised against NDV NP at a 1:400 dilution for 1 h at RT, 2) mouse IgG2a raised against Ebola VP35, 0.2 ug/ml for 1 h at RT, 3) mouse IgG2a raised against human IRF7, 2 ug/ml 16 h at 4°C. For pDCs, NDV infection was detected using rabbit antisera raised against formalin inactivated virus diluted 1:400 in blocking buffer.
After incubating with primary antibodies, coverslips were rinsed three times with PBS and incubated for 30 mins at RT with i) Alexa 488 dye conjugated to goat IgG raised against rabbit or ii) Alexa 568 dye conjugated to goat IgG raised against mouse IgG in PBS containing 0.5% BSA and 20 mM glycine (PBG buffer). Hoechst 33342 dye (0.1 ug/ml) or Alexa 633 phallodin (0.5 ug/ml) were added to stain nuclei and actin cytoskeleton, respectively.
After rinsing three times with PBS, coverslips were mounted using ProLong antifade reagent (Invitrogen, Carlsbad, CA). Widefield fluorescent images were acquired using 40x (NA 0.85) or 63x (NA 0.90) air objectives on a Zeiss DM6000B epifluorescent microscope controlled by the InVivo image acquisition software (MediaCybernetics Bethesda, MD). Images were saved as 16-bit TIFF files, pseudocolored and merged using ImageJ (NIH, Bethesda, MD). Image manipulation was limited to the background subtraction and contrast enhancement functions, and was applied to all samples within the same set.
Confocal microscopy images were acquired using a 63x (NA 1.4) oil immersion objective on a Leica TCS SP5 DM microscope controlled by the Leica LCS software. Images were exported as 8-bit TIFF files.
qPCR
Total RNA from infected cells was extracted using the Qiagen RNeasy kit (Qiagen, Valencia, CA), following the manufacturer’s recommendation. cDNA was prepared, and analyzed by qPCR using an ABI Prism 7900HT instrument at the Mount Sinai Quantitative PCR Shared Resource Facility as previously described.23 Data shown are representative of results from dendritic cells obtained from 3 different human donors.
Western Blot
Adherent cells were harvested by scraping into ice-cold PBS and centrifuging at 200xg for 5 mins at 4°C, while suspension cells were centrifuged directly. Cell pellets were lysed with RIPA buffer (50 mM Tris-HCl, pH 7.4, 140 mM sodium chloride,1% NP40, 0.025% sodium deoxycholate) containing 1 mM sodium orthovanadate, 1 mM PMSF, and 1 ug/ul each of pepstatin, leupeptin and aprotinin. Cell were vortexed for 10 seconds, incubated on ice for 20 mins, and then centrifuged at 14,000xg for 10 mins at 4°C. For A549 cells, we found it necessary to pass the cell suspension through a syringe fitted with a 25 gauge needle ten times to fully lyse the cells. The supernatant was removed and boiled with 6X SDS sample loading buffer (40 mM Tris-HCl, pH 6.8, 10% SDS, 30% glycerol, 0.12% DTT) for 5 mins. Samples were electrophoresed on SDS-PAGE gels, and transferred to Immobilon P membranes (Millipore, Billerica, MA) using a Mini-Genie blotter (Idea Scientific, Minneapolis MN).
Membranes were blocked in 3% BSA in TBS containing 0.2% Tween for 1 hour, and then incubated with antibodies against NDV NP (1:2000), MxA (1 ug/ml), VP35 (0.5 ug/ml), or GAPDH (0.1 ug/ml) for 1h at RT. Antibody to IRF7 was used at 2 ug/ml and incubated 14–16 h at 4°C. After washing three times with TBS containing 0.2% Tween, membranes were incubated with Allophycocyanin (APC) conjugated goat anti-mouse or anti-rabbit antibodies. For some blots, Alexa 546 conjugated goat anti-mouse or anti-rabbit antibodies were used. After rinsing, membranes were dried and imaged on a Typhoon 9400 Multimode imager (GE Healthsciences, Piscataway, NJ). A 633 nm excitation source and Cy5 emission filter was used to detect the APC-labeled antibodies, while a 532 nm excitation and Cy3 emission filter was used to detect Alexa 546-labeled antibodies. The scanned images were converted to 8-bit TIFF files using ImageJ (NIH, Bethesda MD).
NFκB and IFN-β reporter assay
293xl/TLR7 cells were plated into 96-well plates at an approximate density of 2×104 cells per well, and each well was transfected with 100 ng of total plasmid DNA and 0.5 ul of Lipofectamine 2000 (Invitrogen). Each transfection mixture consisted of either 10 ng of NFκB Luciferase reporter plasmid (Promega) and 1 ng of pCAGGS/Renilla, or 10 ng of pIFN-β reporter and 1 ng of pCAGGS/Renilla. For RIG-I activation, cells were transfected with 3 ng of pCAGGS/RIG-I CARD. Some cells received varying amounts of pCAGGS/FLAG-VP35, or pCAGGS alone. Sixteen hours after transfection, the medium from all wells was removed and replaced with DMEM + 0.2% BSA with or without 10 μg/ml of Imiquimod (Invivogen) and cultured for an additional 6 hours. The cells were harvested and assayed for reporter activity using the Dual Luciferase reporter system (Promega) following the manufacturers recommended protocol. Data are shown as the average of 3 samples.
Supplementary Material
Acknowledgments
This work was supported by grants to CFB from the NIH, including AI059536, the Northeast Biodefense Center (AI057158-Lipkin) and AI62623 (Center for Investigating Viral Immunity and Antagonism (CIVIA). MSP acknowledges current support from the Medical Research Center program of MOST/KOSEF (R13-2005-022-02002; Man-Seong Park, PI) and the Hallym University Research Fund, 2007(HRF-2007-043). Confocal laser scanning microscopy was performed at the MSSM-Microscopy Shared Resource Facility, supported with funding from NIH-NCI shared resources grant (R24 CA095823-04), NSF Major Research Instrumentation grant (DBI-9724504) and NIH shared instrumentation grant (S10 RRO 9145-01). The authors thank Kathleen C. Prins and Hannah Phipps-Yonas for sharing unpublished data, Mauricio “Freddy” Sanchez for technical assistance with buffy coats, Luis Muñoz for assistance with mice, the lab of Anna Fernandez-Sesma for sharing reagents, and finally, the MSSM Microbiology Monday Lab Meeting attendees for stimulating discussions.
Footnotes
Authorship and Conflict of Interest Statements
LWL designed and conducted experiments, analyzed data, and wrote the paper. MSP contributed vital new reagents. OM conducted experiments and analyzed data. CV conducted experiments. CBL contributed vital reagents. CFB designed experiments, analyzed data, and wrote the paper. The authors have no competing financial interests.
References
- 1.Bray M, Geisbert TW. Ebola virus: the role of macrophages and dendritic cells in the pathogenesis of Ebola hemorrhagic fever. Int J Biochem Cell Biol. 2005;37:1560–6. doi: 10.1016/j.biocel.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 2.Geisbert TW, Hensley LE. Ebola virus: new insights into disease aetiopathology and possible therapeutic interventions. Expert Rev Mol Med. 2004;6:1–24. doi: 10.1017/S1462399404008300. [DOI] [PubMed] [Google Scholar]
- 3.Sanchez A, Geisbert TW, Feldmann H. Marburg and Ebola Viruses. In: Knipe DM, PMH, editors. Fields Virology. 5 . Vol. 1. Lippincott Williams and Wilkins; Philadelphia: 2007. pp. 1409–48. [Google Scholar]
- 4.Geisbert TW, Hensley LE, Larsen T, Young HA, Reed DS, Geisbert JB, et al. Pathogenesis of Ebola hemorrhagic fever in cynomolgus macaques: evidence that dendritic cells are early and sustained targets of infection. Am J Pathol. 2003;163:2347–70. doi: 10.1016/S0002-9440(10)63591-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bosio CM, Aman MJ, Grogan C, Hogan R, Ruthel G, Negley D, et al. Ebola and Marburg viruses replicate in monocyte-derived dendritic cells without inducing the production of cytokines and full maturation. J Infect Dis. 2003;188:1630–8. doi: 10.1086/379199. [DOI] [PubMed] [Google Scholar]
- 6.Hartman AL, Dover JE, Towner JS, Nichol ST. Reverse genetic generation of recombinant Zaire Ebola viruses containing disrupted IRF-3 inhibitory domains results in attenuated virus growth in vitro and higher levels of IRF-3 activation without inhibiting viral transcription or replication. J Virol. 2006;80:6430–40. doi: 10.1128/JVI.00044-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hartman AL, Ling L, Nichol ST, Hibberd ML. Whole-genome expression profiling reveals that inhibition of host innate immune response pathways by Ebola virus can be reversed by a single amino acid change in the VP35 protein. J Virol. 2008;82:5348–58. doi: 10.1128/JVI.00215-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prins KC, Delpeut S, Leung DW, Reynard O, Volchkova VA, Reid SP, et al. Mutations abrogating VP35 interaction with double-stranded RNA render Ebola virus avirulent in guinea pigs. J Virol. 84:3004–15. doi: 10.1128/JVI.02459-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Basler CF, Amarasinghe GK. Evasion of interferon responses by Ebola and Marburg viruses. J Interferon Cytokine Res. 2009;29:511–20. doi: 10.1089/jir.2009.0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Basler CF, Mikulasova A, Martinez-Sobrido L, Paragas J, Muhlberger E, Bray M, et al. The Ebola virus VP35 protein inhibits activation of interferon regulatory factor 3. J Virol. 2003;77:7945–56. doi: 10.1128/JVI.77.14.7945-7956.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Basler CF, Wang X, Muhlberger E, Volchkov V, Paragas J, Klenk HD, et al. The Ebola virus VP35 protein functions as a type I IFN antagonist. Proc Natl Acad Sci U S A. 2000;97:12289–94. doi: 10.1073/pnas.220398297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cardenas WB, Loo YM, Gale M, Jr, Hartman AL, Kimberlin CR, Martinez-Sobrido L, et al. Ebola virus VP35 protein binds double-stranded RNA and inhibits alpha/beta interferon production induced by RIG-I signaling. J Virol. 2006;80:5168–78. doi: 10.1128/JVI.02199-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prins KC, Cardenas WB, Basler CF. Ebola virus protein VP35 impairs the function of interferon regulatory factor-activating kinases IKKepsilon and TBK-1. J Virol. 2009;83:3069–77. doi: 10.1128/JVI.01875-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kimberlin CR, Bornholdt ZA, Li S, Woods VL, Jr, MacRae IJ, Saphire EO. Ebolavirus VP35 uses a bimodal strategy to bind dsRNA for innate immune suppression. Proc Natl Acad Sci U S A. 107:314–9. doi: 10.1073/pnas.0910547107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leung DW, Prins KC, Borek DM, Farahbakhsh M, Tufariello JM, Ramanan P, et al. Structural basis for dsRNA recognition and interferon antagonism by Ebola VP35. Nat Struct Mol Biol. 17:165–72. doi: 10.1038/nsmb.1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kato H, Sato S, Yoneyama M, Yamamoto M, Uematsu S, Matsui K, et al. Cell type-specific involvement of RIG-I in antiviral response. Immunity. 2005;23:19–28. doi: 10.1016/j.immuni.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 17.Yoneyama M, Fujita T. Function of RIG-I-like receptors in antiviral innate immunity. J Biol Chem. 2007;282:15315–8. doi: 10.1074/jbc.R700007200. [DOI] [PubMed] [Google Scholar]
- 18.Spiropoulou CF, Ranjan P, Pearce MB, Sealy TK, Albarino CG, Gangappa S, et al. RIG-I activation inhibits ebolavirus replication. Virology. 2009;392:11–5. doi: 10.1016/j.virol.2009.06.032. [DOI] [PubMed] [Google Scholar]
- 19.Sanchez A, Lukwiya M, Bausch D, Mahanty S, Sanchez AJ, Wagoner KD, et al. Analysis of human peripheral blood samples from fatal and nonfatal cases of Ebola (Sudan) hemorrhagic fever: cellular responses, virus load, and nitric oxide levels. J Virol. 2004;78:10370–7. doi: 10.1128/JVI.78.19.10370-10377.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Villinger F, Rollin PE, Brar SS, Chikkala NF, Winter J, Sundstrom JB, et al. Markedly elevated levels of interferon (IFN)-gamma, IFN-alpha, interleukin (IL)-2, IL-10, and tumor necrosis factor-alpha associated with fatal Ebola virus infection. J Infect Dis. 1999;179 (Suppl 1):S188–91. doi: 10.1086/514283. [DOI] [PubMed] [Google Scholar]
- 21.Rubins KH, Hensley LE, Wahl-Jensen V, Daddario DiCaprio KM, Young HA, Reed DS, et al. The temporal program of peripheral blood gene expression in the response of nonhuman primates to Ebola hemorrhagic fever. Genome Biol. 2007;8:R174. doi: 10.1186/gb-2007-8-8-r174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gupta M, Mahanty S, Ahmed R, Rollin PE. Monocyte-derived human macrophages and peripheral blood mononuclear cells infected with ebola virus secrete MIP-1alpha and TNF-alpha and inhibit poly-IC-induced IFN-alpha in vitro. Virology. 2001;284:20–5. doi: 10.1006/viro.2001.0836. [DOI] [PubMed] [Google Scholar]
- 23.Borderia AV, Hartmann BM, Fernandez-Sesma A, Moran TM, Sealfon SC. Antiviral-activated dendritic cells: a paracrine-induced response state. J Immunol. 2008;181:6872–81. doi: 10.4049/jimmunol.181.10.6872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Escribese MM, Kraus T, Rhee E, Fernandez-Sesma A, Lopez CB, Moran TM. Estrogen inhibits dendritic cell maturation to RNA viruses. Blood. 2008;112:4574–84. doi: 10.1182/blood-2008-04-148692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fernandez-Sesma A, Marukian S, Ebersole BJ, Kaminski D, Park MS, Yuen T, et al. Influenza virus evades innate and adaptive immunity via the NS1 protein. J Virol. 2006;80:6295–304. doi: 10.1128/JVI.02381-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gabriele L, Fragale A, Borghi P, Sestili P, Stellacci E, Venditti M, et al. IRF-1 deficiency skews the differentiation of dendritic cells toward plasmacytoid and tolerogenic features. J Leukoc Biol. 2006;80:1500–11. doi: 10.1189/jlb.0406246. [DOI] [PubMed] [Google Scholar]
- 27.Kumagai Y, Kumar H, Koyama S, Kawai T, Takeuchi O, Akira S. Cutting Edge: TLR-Dependent viral recognition along with type I IFN positive feedback signaling masks the requirement of viral replication for IFN-{alpha} production in plasmacytoid dendritic cells. J Immunol. 2009;182:3960–4. doi: 10.4049/jimmunol.0804315. [DOI] [PubMed] [Google Scholar]
- 28.Matsui K, Kumagai Y, Kato H, Sato S, Kawagoe T, Uematsu S, et al. Cutting edge: Role of TANK-binding kinase 1 and inducible IkappaB kinase in IFN responses against viruses in innate immune cells. J Immunol. 2006;177:5785–9. doi: 10.4049/jimmunol.177.9.5785. [DOI] [PubMed] [Google Scholar]
- 29.Habjan M, Andersson I, Klingstrom J, Schumann M, Martin A, Zimmermann P, et al. Processing of genome 5′ termini as a strategy of negative-strand RNA viruses to avoid RIG-I-dependent interferon induction. PLoS One. 2008;3:e2032. doi: 10.1371/journal.pone.0002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Park MS, Garcia-Sastre A, Cros JF, Basler CF, Palese P. Newcastle disease virus V protein is a determinant of host range restriction. J Virol. 2003;77:9522–32. doi: 10.1128/JVI.77.17.9522-9532.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vigil A, Martinez O, Chua MA, Garcia-Sastre A. Recombinant Newcastle disease virus as a vaccine vector for cancer therapy. Mol Ther. 2008;16:1883–90. doi: 10.1038/mt.2008.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vigil A, Park MS, Martinez O, Chua MA, Xiao S, Cros JF, et al. Use of reverse genetics to enhance the oncolytic properties of Newcastle disease virus. Cancer Res. 2007;67:8285–92. doi: 10.1158/0008-5472.CAN-07-1025. [DOI] [PubMed] [Google Scholar]
- 33.Bjorndal AS, Szekely L, Elgh F. Ebola virus infection inversely correlates with the overall expression levels of promyelocytic leukaemia (PML) protein in cultured cells. BMC Microbiol. 2003;3:6. doi: 10.1186/1471-2180-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reid SP, Leung LW, Hartman AL, Martinez O, Shaw ML, Carbonnelle C, et al. Ebola virus VP24 binds karyopherin alpha1 and blocks STAT1 nuclear accumulation. J Virol. 2006;80:5156–67. doi: 10.1128/JVI.02349-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Emeny JM, Morgan MJ. Regulation of the interferon system: evidence that Vero cells have a genetic defect in interferon production. J Gen Virol. 1979;43:247–52. doi: 10.1099/0022-1317-43-1-247. [DOI] [PubMed] [Google Scholar]
- 36.Sumpter R, Jr, Loo YM, Foy E, Li K, Yoneyama M, Fujita T, et al. Regulating intracellular antiviral defense and permissiveness to hepatitis C virus RNA replication through a cellular RNA helicase, RIG-I. J Virol. 2005;79:2689–99. doi: 10.1128/JVI.79.5.2689-2699.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Park MS, Shaw ML, Munoz-Jordan J, Cros JF, Nakaya T, Bouvier N, et al. Newcastle disease virus (NDV)-based assay demonstrates interferon-antagonist activity for the NDV V protein and the Nipah virus V, W, and C proteins. J Virol. 2003;77:1501–11. doi: 10.1128/JVI.77.2.1501-1511.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chang TH, Kubota T, Matsuoka M, Jones S, Bradfute SB, Bray M, et al. Ebola Zaire virus blocks type I interferon production by exploiting the host SUMO modification machinery. PLoS Pathog. 2009;5:e1000493. doi: 10.1371/journal.ppat.1000493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jin H, Yan Z, Prabhakar BS, Feng Z, Ma Y, Verpooten D, et al. The VP35 Protein of Ebola Virus Impairs Dendritic Cell Maturation Induced by Virus and Lipopolysaccharide. J Gen Virol. 2009 doi: 10.1099/vir.0.017343-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hensley LE, Young HA, Jahrling PB, Geisbert TW. Proinflammatory response during Ebola virus infection of primate models: possible involvement of the tumor necrosis factor receptor superfamily. Immunol Lett. 2002;80:169–79. doi: 10.1016/s0165-2478(01)00327-3. [DOI] [PubMed] [Google Scholar]
- 41.Honda K, Yanai H, Negishi H, Asagiri M, Sato M, Mizutani T, et al. IRF-7 is the master regulator of type-I interferon-dependent immune responses. Nature. 2005;434:772–7. doi: 10.1038/nature03464. [DOI] [PubMed] [Google Scholar]
- 42.Levy DE, Marie I, Smith E, Prakash A. Enhancement and diversification of IFN induction by IRF-7-mediated positive feedback. J Interferon Cytokine Res. 2002;22:87–93. doi: 10.1089/107999002753452692. [DOI] [PubMed] [Google Scholar]
- 43.Marie I, Durbin JE, Levy DE. Differential viral induction of distinct interferon-alpha genes by positive feedback through interferon regulatory factor-7. EMBO J. 1998;17:6660–9. doi: 10.1093/emboj/17.22.6660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tailor P, Tamura T, Kong HJ, Kubota T, Kubota M, Borghi P, et al. The feedback phase of type I interferon induction in dendritic cells requires interferon regulatory factor 8. Immunity. 2007;27:228–39. doi: 10.1016/j.immuni.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Joo CH, Shin YC, Gack M, Wu L, Levy D, Jung JU. Inhibition of interferon regulatory factor 7 (IRF7)-mediated interferon signal transduction by the Kaposi’s sarcoma-associated herpesvirus viral IRF homolog vIRF3. J Virol. 2007;81:8282–92. doi: 10.1128/JVI.00235-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang F, Gao X, Barrett JW, Shao Q, Bartee E, Mohamed MR, et al. RIG-I mediates the co-induction of tumor necrosis factor and type I interferon elicited by myxoma virus in primary human macrophages. PLoS Pathog. 2008;4:e1000099. doi: 10.1371/journal.ppat.1000099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mogensen TH. Pathogen recognition and inflammatory signaling in innate immune defenses. Clin Microbiol Rev. 2009;22:240–73. doi: 10.1128/CMR.00046-08. Table of Contents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nakhaei P, Genin P, Civas A, Hiscott J. RIG-I-like receptors: sensing and responding to RNA virus infection. Semin Immunol. 2009;21:215–22. doi: 10.1016/j.smim.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 49.Pichlmair A, Reis e Sousa C. Innate recognition of viruses. Immunity. 2007;27:370–83. doi: 10.1016/j.immuni.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 50.Pichlmair A, Schulz O, Tan CP, Naslund TI, Liljestrom P, Weber F, et al. RIG-I-mediated antiviral responses to single-stranded RNA bearing 5′-phosphates. Science. 2006;314:997–1001. doi: 10.1126/science.1132998. [DOI] [PubMed] [Google Scholar]
- 51.Takeuchi O, Akira S. Innate immunity to virus infection. Immunol Rev. 2009;227:75–86. doi: 10.1111/j.1600-065X.2008.00737.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yoneyama M, Kikuchi M, Natsukawa T, Shinobu N, Imaizumi T, Miyagishi M, et al. The RNA helicase RIG-I has an essential function in double-stranded RNA-induced innate antiviral responses. Nat Immunol. 2004;5:730–7. doi: 10.1038/ni1087. [DOI] [PubMed] [Google Scholar]
- 53.Bosio CM, Moore BD, Warfield KL, Ruthel G, Mohamadzadeh M, Aman MJ, et al. Ebola and Marburg virus-like particles activate human myeloid dendritic cells. Virology. 2004;326:280–7. doi: 10.1016/j.virol.2004.05.025. [DOI] [PubMed] [Google Scholar]
- 54.Burke CW, Gardner CL, Steffan JJ, Ryman KD, Klimstra WB. Characteristics of alpha/beta interferon induction after infection of murine fibroblasts with wild-type and mutant alphaviruses. Virology. 2009;395:121–32. doi: 10.1016/j.virol.2009.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Baize S, Leroy EM, Georges AJ, Georges-Courbot MC, Capron M, Bedjabaga I, et al. Inflammatory responses in Ebola virus-infected patients. Clin Exp Immunol. 2002;128:163–8. doi: 10.1046/j.1365-2249.2002.01800.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Leroy EM, Baize S, Volchkov VE, Fisher-Hoch SP, Georges-Courbot MC, Lansoud-Soukate J, et al. Human asymptomatic Ebola infection and strong inflammatory response. Lancet. 2000;355:2210–5. doi: 10.1016/s0140-6736(00)02405-3. [DOI] [PubMed] [Google Scholar]
- 57.Martinez O, Johnson J, Manicassamy B, Rong L, Olinger GG, Hensley LE, et al. Zaire Ebola virus entry into human dendritic cells is insensitive to cathepsin L inhibition. Cell Microbiol. 2009 doi: 10.1111/j.1462-5822.2009.01385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.