Abstract
Several studies demonstrate the benefits of low-power light therapy on wound healing. However, the use of LED as a therapeutic resource remains controversial. There are questions regarding the equality or not of biological effects promoted by LED and LASER. One objective of this review was to determine the biological effects that support the use of LED on wound healing. Another objective was to identify LED´s parameters for the treatment of wounds. The biological effects and parameters of LED will be compared to those of LASER. Literature was obtained from online databases such as Medline, PubMed, Science Direct and Scielo. The search was restricted to studies published in English and Portuguese from 1992 to 2012. Sixty-eight studies in vitro and in animals were analyzed. LED and LASER promote similar biological effects, such as decrease of inflammatory cells, increased fibroblast proliferation, stimulation of angiogenesis, granulation tissue formation and increased synthesis of collagen. The irradiation parameters are also similar between LED and LASER. The biological effects are dependent on irradiation parameters, mainly wavelength and dose. This review elucidates the importance of defining parameters for the use of light devices.
Keywords: Light, Phototherapy, Wound healing
INTRODUCTION
A wound is characterized by the interruption on the continuity of a body tissue. It can be caused by any type of physical, chemical and mechanical trauma or triggered by a medical condition.1 Cutaneous wounds are relatively common in adults and their incidence seems to increase in parallel with the advances in life expectancy in the population.2
The therapeutic approach to wound healing consists of preventive measures such as health professional continuing education, family counseling and guidelines to a proper patient nutrition. The use of medicinal plants, administration of essential fatty acids, calcium alginate, antiseptics and degerming products, activated carbon, semi-permeable films, biological collagen, cell growth factors, hydropolymer, hydrogel and hydrocolloid substances, proteolytic enzymes, sulfadiazine silver, gauze dressings, bandages for skin protection and compression are also advocated.3 Physical treatments such as therapeutic ultrasound and electrotherapy are cited likewise in the literature as important adjuncts in wound management.4,5 These therapies seem to be advantageous but they have limitations and do not always achieve satisfactory results.
Wounds that are difficult to heal represent a serious public health problem. The lesions severely affect the quality of life of individuals due to decreased mobility and substantial loss of productivity; they can also cause emotional damage and contribute to increase the burden of public expenditures in healthcare.6
The need to care for a population with poorly healing wounds is a growing challenge that requires innovative strategies. An approach that stands out in the treatment of these lesions is low-power light therapy, promoted by light devices such as LASER (Light Amplification by Stimulated Emission of Radiation) and LED (Light Emitting Diode).
The therapeutic benefits of LASER light in the treatment of wounds have been reported since the 1960s and those of LED light only since the 1990s.7,8 However, many of the results described show inconsistency, mainly due to methodology bias or lack of standardization in the studies. Furthermore, the use of LED as a therapeutic resource remains controversial. There are questions regarding the equality or not of biological and therapeutic effects promoted by LED and LASER resources, but also regarding the appropriate parameters to each of these light sources.
This study aimed to determine, through a literature review: 1 - the biological effects that support the use of light sources such as LED in the treatment of wounds and 2 - the light parameters (wavelength and dose) suitable for the treatment of wounds with LED light sources. The biological effects and light parameters of LED will be compared to those of LASER in order to verify the similarity (or not) regarding wound treatment.
MATERIALS AND METHODS
A literature search was performed in Medline, PubMed, SciELO and Science Direct databases. The literature search was restricted to studies published in English and Portuguese in the period of 1992-2012. The keywords used were "low level laser therapy", "laser", "light emitting diode", "LED", "phototherapy", "wound healing", "fibroblast", "collagen" and "angyogenesis" combined with each other.
RESULTS
Sixty-eight studies were analyzed, including 48 on LASER light, 14 related to LED light and 6 for both types of light (Tables 1 to 3). According to data presented on table 1, 16 of the 48 studies on the effects of LASER light were in vitro and 32 were performed in animals.9-56 The use of different wavelengths (532-1064 nm) was verified, with the most utilized spectral range being between 632.8 and 830 nm. Doses ranging from 0.09 to 90 J/cm2 were used, predominating the values from 1 to 5 J/cm2 . One study did not cite the dose value used.48 The biological effects promoted were reduction of inflammatory cells, increased proliferation of fibroblasts, stimulation of collagen synthesis, angiogenesis inducement and granulation tissue formation. It was noted in a study that the dose of 4 J/cm2 was more effective than 8 J/cm2 .14 Furthermore, doses of 10 and 16 J/cm2 promoted inhibitory effects.20,25,29,34
TABLE 1.
Biological effects of LASER light on cutaneous wounds
| Study | Model | Wavelength (nm) | Dose (J/cm2) | Biological effects |
|---|---|---|---|---|
| 632 | 9; 15; 30; 60; 90 | |||
| Lubart et al.9 | In vitro | + | ||
| 780 | 7; 18; 36; 72 | |||
| Yu et al.10 | Mouse | 630 | 5 | + |
| Almeida-Lopes et al.11 | In vitro | 670; 692; 780; 786 | 2 | + |
| Reddy et al.12 | Rat | 632,8 | 1 | + |
| Pereira et al.13 | In vitro | 904 | 3; 4; 5 | + |
| Medrado et al.14 | Rat | 670 | 4; 8 | + |
| Pugliese et al.15 | Rat | 670 | 4; 8 | + |
| Reddy16 | Rat | 904 | 1 | + |
| Byrnes et al.17 | Rat | 632.8 | 4; 5; 7.2 | + |
| Nascimento et al.18 | Rat | 670; 685 | 10 | + |
| Ribeiro et al.19 | Rat | 632.8 | 1 | + |
| Hawkins and Abrahamse20 | In vitro | 632.8 | 0.5; 2.5; 5; 10 | + |
| Maiya et al.21 | Rat | 632.8 | 4.8 | + |
| Moore et al.22 | In vitro | 625 - 675; 810 | 10 | + |
| Poon et al.23 | In vitro | 532 | 0.8 | + |
| Carvalho et al.24 | Rat | 632.8 | 4 | + |
| Hawkins and Abrahamse25 | In vitro | 632.8 | 2.5; 5; 16 | + |
| Rabelo et al.26 | Rat | 632.8 | 10 | + |
| Araújo et al.27 | Mouse | 632.8 | 1 | + |
| Hawkins and Abrahamse28 | In vitro | 632.8; 830 | 5 | + |
| Houreld and Abrahamse29 | In vitro | 632.8 | 5; 16 | + |
| Mirzaei et al.30 | In vitro | 632.8 | 0.09; 1; 4 | + |
| Rezende et al.31 | Rat | 830 | 1,3; 3 | + |
| Viegas et al.32 | Rat | 685; 830 | 4 | + |
| Yasukawa et al.33 | Rat | 632.8 | 2.09; 4.21 | + |
| Houreld and Abrahamse34 | In vitro | 632.8; 830 | 5; 16 | + |
| Medrado et al.35 | Rat | 670 | 4 | + |
| Meireles et al.36 | Rat | 660; 780 | 20 | + |
| Reis et al.37 | Rat | 670 | 4 | + |
| Gungormus and Akyol38 | Rat | 808 | 10 | + |
| Skopin and Molitor39 | In vitro | 980 | 3.1 - 14.4 | + |
| Carvalho et al.40 | Rat | 660 | 4 | + |
| Chung et al.41 | Mouse | 660 | 1.9 - 2.5 | + |
| 3.7 - 5.0 | ||||
| 7.4 - 10 | ||||
| Gonçalves et al.42 | Rat | 830 | 30; 60 | + |
| Gonçalves et al.43 | Rat | 830 | 30; 60 | + |
| 904 | 4 | |||
| Guirro et al.44 | Rat | 670 | 4; 7 | + |
| Houreld and Abrahamse45 | In vitro | 632.8; 830 | 5 | + |
| Lacjakova et al.46 | Rat | 670 | 5 | + |
| Medeiros et al.47 | Rat | 655 | 12 | + |
| Hussein et al.48 | Rabbit | 890 | ---------- | + |
| Silveira et al.49 | Rat | 660; 904 | 1; 3 | + |
| Weng et al.50 | In vitro | 532 | 35 | + |
| 1064 | 1.2 | |||
| Basso et al.51 | In vitro | 780 | 0.5; 1.5; 3; 5; 7 | + |
| Crisan et al.52 | In vitro | 830; 980 | 5.5 | + |
| Dawood and Salman53 | Mouse | 650 | 38.2; 57.3 | + |
| Fahimipour et al.54 | Mouse | 632.8; 830 | 4; 7.5 | + |
| Gonçalves et al.55 | Rat | 830 | 30; 90 | + |
| Nunez et al.56 | Rat | 660 | 1; 4 | + |
TABLE 3.
Biological effects of LED and LASER light on cutaneous wounds
| Study | Model | Type of light | Wavelength (nm) | Dose (J/cm2) | Biological effects |
|---|---|---|---|---|---|
| Vinck et al.70 | In vitro | LASER | 830 | 1 | + |
| LED | 570 | 0.1 | |||
| 660 | 0.53 | ||||
| 950 | 0.53 | ||||
| Corazza et al.71 | Rat | LASER | 660 | 5 | + |
| LED | 635 | 20 | |||
| Volpato et al.72 | In vitro | LASER | 660 | 4; 8 | + |
| 780 | 5; 10 | ||||
| LED | 637 | 4; 8 | |||
| Nishioka et al.73 | Rat | LASER | 660 | 5 | + |
| LED | 630 | ||||
| Sampaio et al.74 | Rat | LASER | 660 | 10 | + |
| LED | 700 | ||||
| Sousa et al.75 | Rat | LASER | 660; 790 | 10 | + |
| LED | 460; 530; 700 |
Eight of the 14 studies on the effects of LED light were in vitro studies and 6 performed in animals, as shown in table 2.57-70 Wavelengths ranging 456-880 nm were used, with spectral range from 627 to 670 nm predominating. Doses ranged from 0.1 to 10 J/cm2, and 4 J/cm2 was the predominant dose. However, not all studies reported the dose applied.64,66,67,68 Biological effects observed were reduction of inflammatory cells, increased fibroblast proliferation, collagen synthesis, stimulation of angiogenesis and granulation tissue formation, these being similar to the ones observed in studies with LASER.
TABLE 2.
Biological effects of LED light on cutaneous wounds
| Study | Model | Wavelength (nm) | Dose (J/cm2) | Biological effects |
|---|---|---|---|---|
| Whelan et al.57 | In vitro | 670; 728; 880 | 4; 8 | + |
| Vinck et al.58 | In vitro | 570 | 0.1 | + |
| Weiss et al.59 | In vitro | 590 | 0.1 | + |
| Huang et al.60 | In vitro | 630 | 1; 2 | + |
| Lanzafame et al.61 | Mouse | 670 | 5 | + |
| Agnol et al.62 | Rat | 640 | 6 | + |
| Tada et al.63 | In vitro | 627 | 1; 2; 4; 8; 10 | + |
| Komine et al.64 | In vitro | 627 | 4 | + |
| Meyer et al.65 | Rat | 515-525 | --------- | + |
| 620-630 | ||||
| Sousa et al.66 | Rat | 460; 530; 700 | 10 | + |
| Adamskaya et al.67 | Rat | 470; 629 | --------- | + |
| Lim et al.68 | In vitro | 635 | --------- | + |
| Cheon et al.69 | Rat | 470; 525; 633 | --------- | + |
| Fushimi et al.70 | In vitro | 456; 518; 638 | 0.2; 0.3; 0.6 | + |
Table 3 shows six studies comparing the biological effects of LASER and LED lights.71-76 Two of the studies were in vitro and 4 were performed in rats. It has been noticed that wavelengths varied from 460 to 950 nm, with the range of 630-790 nm being the most utilized both in LASER and LED studies. Doses ranging from 0.1 to 10 J/cm2 were used, with predominance of doses up to 5 J/cm2 . All studies reported similar effects between LASER and LED, such as increased fibroblast proliferation and stimulation of angiogenesis.
DISCUSSION
Since the introduction of photobiomodulation in healthcare, the effectiveness and applicability of light resources for the treatment of skin wounds have been extensively investigated both in vitro and in vivo. Nevertheless, the biological mechanisms that support the actions of low intensity light in tissues are still not clearly elucidated. While some studies report an increase in cellular proliferation of several cell types including fibroblasts, endothelial cells and keratinocytes, conflicting results about the clinical benefits of using light on skin wounds are found in the literature.
The way light interacts with the biological tissues will depend on the characteristics and parameters of light devices, mainly the wavelength and dose, and also the optical properties of the tissue.
Regarding the characteristics of light devices, LASER consists of a resonant optical cavity and different types of active media such as solid, liquid or gaseous materials, in which processes of light generation occur through the passage of an electric current.77 Potency in the range of 10-3 to 10-1 W, wavelength from 300 to 10,600 nm, pulse frequency from 0 (continuous emission) to 5,000 Hz, pulse duration and pulse interval from 1 to 500 milliseconds, total radiation from 10-3000 seconds, intensity between 10-2 and 100 Wcm-1 and dose from 10-2 to 102 Jcm-2 characterized LASER as a low potency device.78
On the other hand, LED is a diode formed by p-n junctions (p-positive, n-negative) that, when directly polarized, causes electrons to cross the potential barrier and recombine with holes within the device. After the spontaneous recombination of electron-hole pairs, the simultaneous emission of photons occurs. The physical mechanism by which LED emits light is spontaneous light emission. The light-emitting diodes convert the electrical current in a light spectrum, a process called electroluminescence.79 LEDs usually operate with outputs in the range of milliwatts and therefore are usually set up on small chips or connected to small light bulbs.80
The variable characteristics and parameters of light devices is one of the factors that complicate the interpretation of research results about the effects of low intensity light on skin wounds. As observed in this study, there is discordance between the types of light and parameters used in studies. This fact may limit the decision-making process regarding the role of light in treating wounds since photobiomodulator effects are parameter-dependent.
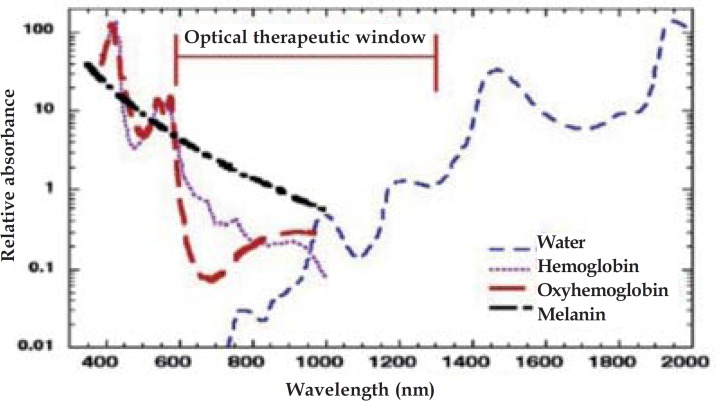
Energy absorption is the primary mechanism that allows light from LASER or LED to produce biological effects in the tissue. Light absorption is dependent on wavelength and the main tissue chromophores (hemoglobin and melanin) strongly absorb wavelengths shorter than 600 nm. For these reasons, there is a therapeutic window in the optical spectral range of red and near infrared, wherein the efficiency of light penetration in the tissue is maximum (Figure 1).81
FIGURE 1.
Optical therapeutic window
Fifty-nine of the 68 studies reviewed applied LASER or LED inside the optical therapeutic window and 9 applied them in the range of blue or green, and even so biological effects were observed. Although light in the blue and green wavelengths range can achieve significant effects in cells, the use of low power light in animals and humans involves almost exclusively light in red and near infrared wavelengths.81 Historical issues, mainly cost and availability may be related to this fact.
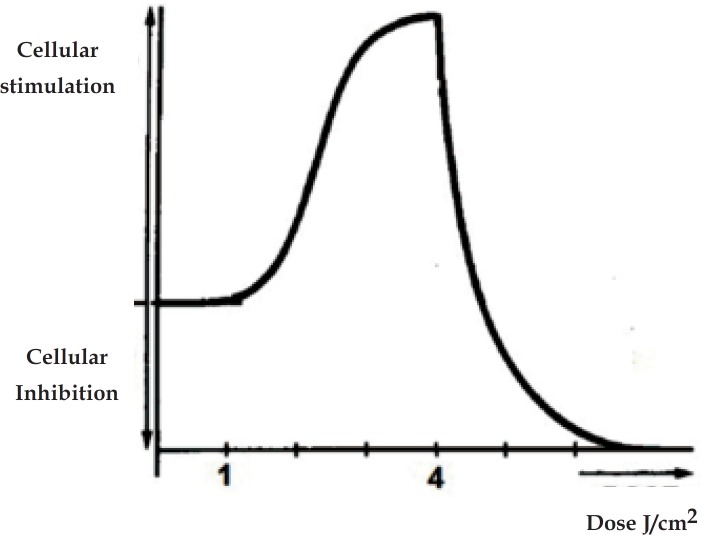
As noted in Tables 1, 2 and 3 studies applied LASER or LED with doses around 0.09 to 90 J/cm2. The most significant biological effects were seen with predominant dose values, i.e. up to 5 J/cm2, which are within the Arndt-Schultz curve (Figure 2). According to Sommer et al, very low doses do not promote biological effects, while higher doses result in inhibition of cellular functions.82 The energetic state of the cell, i.e. the physiological condition of the tissue in treatment is therefore critical to determine which dose to use.
FIGURE 2.
Arndt-Schultz Curve
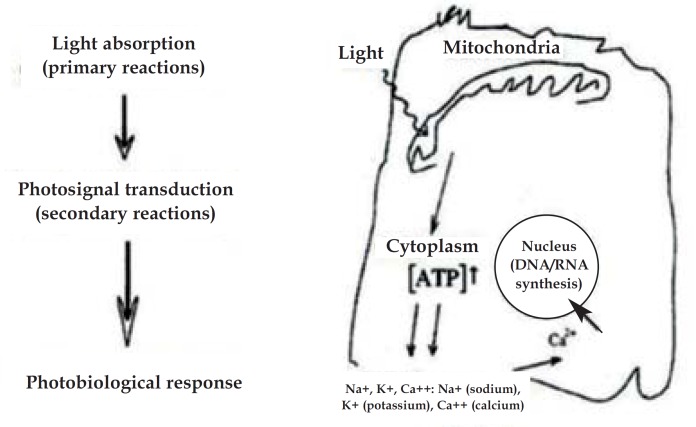
The mechanism of light action on the cellular level that supports its biological effects is based on photobiological reactions. A photobiological reaction involves the absorption of a specific wavelength of light by photoreceptor molecules.83
There is evidence that wavelengths in the spectral range from red to near infrared are absorbed by cytochrome c oxidase.83,84 In the study by Karu and Kolyakov action spectra of monochromatic light from 580 to 860 nm were analyzed.85 The authors noted four active spectral regions, two in the red range (peaks from 613.5 to 623.5 nm and 667.5 to 683.7 nm) and two infrared (peaks from 750.7 to 772, 3 nm and 812.5 to 846.0 nm). In addition, they also observed the absorption by cytochrome c oxidase in these four bands. The authors concluded that cytochrome c oxidase could absorb light in different spectral bands (red and near infrared), probably in the binuclear centers CuA and CuB (oxidized forms).
Photobiological reactions can be classified into primary and secondary. Primary reactions derive from the interaction between photons and the photoreceptor, and they are observed in a few seconds or minutes after the irradiation of light. On the other hand, secondary reactions are effects that occur in response to primary reactions, in hours or even days after the irradiation procedure.84,86
The primary reactions of light action on photoreceptors are not yet clearly established, but there are some hypotheses. After the absorption of light in the irradiated wavelength, cytochrome c oxidase displays an electronically excited status, from which it alters its redox status and causes the acceleration of electron transfer in the respiratory chain.87 Another hypothesis is that a part of the electronically excited status energy is converted into heat, causing a localized and transient heating in photoreceptors.88 A third assumption would be that when enabling the flow of electrons in the respiratory chain by light irradiation, an increase in the production of superoxide anion can be expected.89 A fourth reaction formula assumes that porphyrins and flavoproteins absorb photons and generate reactive species of singlet oxygen.90 It has also been proposed that light can reverse cytochrome c oxidase inhibition through nitric oxide and thereby increase the rate of respiration.91
The mechanism of secondary photobiological reactions is determined by transduction (energy transfer from one system to another) and photosignal amplification leading to photoresponse. This means that effects derived from primary reactions are amplified and transmitted to other parts of the cell, resulting in physiological effects such as alterations in cell membrane permeability with changes in intracellular calcium levels, increased cellular metabolism, DNA and RNA syntheses, fibroblast proliferation, activation of T lymphocytes, macrophages and mast cells, increased synthesis of endorphins and decreased bradykinin.83
Secondary reactions are responsible for the connection between response to light action by photoreceptors located inside the mitochondria and the effects located in the nucleus or different phenomena in other cell components. This process makes it possible to apply a very small amount of light to produce clinically significant effects on tissues.92
In short, light absorption depending on the wavelength, causes primary reactions on the mitochondria. These are followed by a cascade of secondary reactions (photosignal transduction and amplification) that occur in the cytoplasm, membrane and nucleus as shown by the Karu model (Figure 3).
FIGURE 3.
Karu Model
Nevertheless, there is a hypothesis about a modification in the Karu model. It is believed that the red light is absorbed by cytochrome-c oxidase inside the mitochondria, while the infrared wavelength is absorbed by specific cell membrane proteins directly affecting membrane permeability; both pathways lead to the same photobiological end response.93
Sources like LASER differ from LED ones because of a characteristic known as coherence. This feature is related to stimulated emission mechanisms, with LASER light being formed by same frequency, direction and phase waves.94 Some authors believe that coherence plays a role in the production of light therapy derived benefits, and LED (not coherent) would be less efficient than LASER (coherent) or even unable to promote therapeutic effects.95
The reviewed studies, however, have shown that LED light can be as effective as LASER, since both have similar biological effects, with no significant difference between them. The cellular response to photostimulation is not associated with specific properties of LASER light, such as coherence.96 According to Karu, the property of coherence is lost during the interaction of light with biological tissue, not being thus a prerequisite for the process of photostimulation or photoinhibition.86
More clinical studies, especially with LEDs, must be performed in order to assess the adequacy of parameters commonly used experimental in vitro and animal studies to the clinical practice, since, in the relevant literature, there is a diversity in methodology, as well as differences in wavelength, dose and types of study.
CONCLUSION
The reviewed studies show that phototherapy, either by LASER or LED, is an effective therapeutic modality to promote healing of skin wounds. The biological effects promoted by these therapeutic resources are similar and are related to the decrease in inflammatory cells, increased fibroblast proliferation, angiogenesis stimulation, formation of granulation tissue and increased collagen synthesis. In addition to these effects, the irradiation parameters are also similar between LED and LASER. Importantly, the biological effects are dependent on such parameters, especially wavelength and dose, highlighting the importance of determining an appropriate treatment protocol.
Footnotes
Conflict of interest: None
Financial Support: None
Work performed at the Bioengineering Laboratory at Universidade Federal de Minas Gerais (UFMG) - Belo Horizonte (MG), Brazil.
How to cite this article: Chaves MEA, Araújo AR, Piancastelli ACC, Pinotti M. Effects of low-power light therapy on wound healing: LASER x LED. An Bras Dermatol. 2014;89(4):616-23.
REFERENCES
- 1.Cesaretti IUR. Processo fisiológico de cicatrização da ferida. Pelle Sana. 1998;2:10–12. [Google Scholar]
- 2.Borges EL. Borges EL, Saar SRC, Lima VLAN, Gomes FSL, Magalhães MBB. Feridas: como tartar. Belo Horizonte: Coopmed; 2001. Fatores intervenientes no processo de cicatrização. [Google Scholar]
- 3.Mandelbaum SH, Di Santis EP, Mandelbaum MHS. Cicatrização: conceitos atuais e recursos auxiliaries - Parte II. An Bras Dermatol. 2003;78:525–542. [Google Scholar]
- 4.Poltawski L, Watson T. Transmission of therapeutic ultrasound by wound dressings. Wounds. 2007;19:1–12. [PubMed] [Google Scholar]
- 5.Cutting KF. Electric stimulation in the treatment of chronic wounds. Wounds. 2006;2:62–71. [Google Scholar]
- 6.Brem H, Kirsner RS, Falanga V. Protocol for the successful treatment of venous ulcers. Am J Surg. 2004;188:1–8. doi: 10.1016/S0002-9610(03)00284-8. [DOI] [PubMed] [Google Scholar]
- 7.Mester E, Juhász J, Varga P, Karika G. Lasers in clinical practice. Acta Chir Acad Sci Hung. 1968;9:349–357. [PubMed] [Google Scholar]
- 8.Yeh NG, Wu C, Cheng TC. Light-emitting diodes - their potential in biomedical applications. Renew Sust Energ Rev. 2010;14:2161–2166. [Google Scholar]
- 9.Lubart R, Wollman Y, Friedmann H, Rochkind S, Laulicht I. Effects of visible and near infrared lasers on cell cultures. J Photochem Photobiol B. 1992;12:305–310. doi: 10.1016/1011-1344(92)85032-p. [DOI] [PubMed] [Google Scholar]
- 10.Yu W, Naim JO, Lanzafame RJ. Effects of photostimulation on wound healing in diabetic mice. Lasers Surg Med. 1997;20:56–63. doi: 10.1002/(sici)1096-9101(1997)20:1<56::aid-lsm9>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 11.Almeida-Lopes L, Rigau J, Zângaro RA, Guidugli-Neto J, Jaeger MM. Comparison of the low-level laser therapy effects on cultured human gingival fibroblasts proliferation using different irradiance and same fluence. Lasers Surg Med. 2001;29:179–184. doi: 10.1002/lsm.1107. [DOI] [PubMed] [Google Scholar]
- 12.Reddy GK, Stehno-Bittel L, Enwemeka CS. Laser photostimulation accelerates wound healing in diabetic rats. Wound Repair Regen. 2001;9:248–255. doi: 10.1046/j.1524-475x.2001.00248.x. [DOI] [PubMed] [Google Scholar]
- 13.Pereira AN, Eduardo Cde P, Matson E, Marques MM. Effect of low-power laser irradiation on cell growth and procollagen synthesis of cultured fibroblasts. Lasers Surg Med. 2002;31:263–267. doi: 10.1002/lsm.10107. [DOI] [PubMed] [Google Scholar]
- 14.Medrado AR, Pugliese LS, Reis SR, Andrade ZA. Influence of low level laser therapy on wound healing and its biological action upon myofibroblasts. Lasers Surg Med. 2003;32:239–244. doi: 10.1002/lsm.10126. [DOI] [PubMed] [Google Scholar]
- 15.Pugliese LS, Medrado AP, Reis SR, Andrade Zde A. The influence of low level laser therapy on biomodulation of collagen and elastic fibers. Pesqui Odontol Bras. 2003;17:307–313. doi: 10.1590/s1517-74912003000400003. [DOI] [PubMed] [Google Scholar]
- 16.Reddy GK. Comparison of the photostimulatory effects of visible He-Ne and infrared Ga-As lasers on healing impaired diabetic rat wounds. Lasers Surg Med. 2003;33:344–351. doi: 10.1002/lsm.10227. [DOI] [PubMed] [Google Scholar]
- 17.Byrnes KR, Barna L, Chenault VM, Waynant RW, Ilev IK, Longo L, et al. Photobiomodulation improves cutaneous wound healing in an animal model of type II diabetes. Photomed Laser Surg. 2004;22:281–290. doi: 10.1089/pho.2004.22.281. [DOI] [PubMed] [Google Scholar]
- 18.do Nascimento PM, Pinheiro AL, Salgado MA, Ramalho LM. A preliminary report on the effect of laser therapy on the healing of cutaneous surgical wounds as a consequence of an inversely proportional relationship between wavelength and intensity: histological study in rats. Photomed Laser Surg. 2004;22:513–518. doi: 10.1089/pho.2004.22.513. [DOI] [PubMed] [Google Scholar]
- 19.Ribeiro MS, Da Silva Dde F, De Araújo CE, De Oliveira SF, Pelegrini CM, Zorn TM, et al. Effects of low intensity polarized visible laser radiation on skin burns: a light microscopy study. J Clin Laser Med Surg. 2004;22:59–66. doi: 10.1089/104454704773660994. [DOI] [PubMed] [Google Scholar]
- 20.Hawkins D, Abrahamse H. Biological effects of Helium-Neon laser irradiation on normal and wounded human skin fibroblasts. Photomed Laser Surg. 2005;23:251–259. doi: 10.1089/pho.2005.23.251. [DOI] [PubMed] [Google Scholar]
- 21.Maiya GA, Kumar P, Rao L. Effect of low intensity Helium-Neon (He-Ne) laser irradiation on diabetic wound healing dynamics. Photomed Laser Surg. 2005;23:187–190. doi: 10.1089/pho.2005.23.187. [DOI] [PubMed] [Google Scholar]
- 22.Moore P, Ridgway TD, Higbee RG, Howard EW, Lucroy MD. Effect of wavelength on low intensity laser irradiation stimulated cell proliferation in vitro. Lasers Surg Med. 2005;36:8–12. doi: 10.1002/lsm.20117. [DOI] [PubMed] [Google Scholar]
- 23.Poon VKM, Huang L, Burd A. Biostimulation of dermal fibroblast by sublethal Qswitched Nd:YAG 532 nm laser: collagen remodeling and pigmentation. J Photochem Photobiol B. 2005;81:1–8. doi: 10.1016/j.jphotobiol.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 24.Carvalho PT, Mazzer N, dos Reis FA, Belchior AC, Silva IS. Analysis of the influence of low power HeNe laser on the healing of skin wounds in diabetic and non-diabetic rats. Acta Cir Bras. 2006;21:177–183. doi: 10.1590/s0102-86502006000300010. [DOI] [PubMed] [Google Scholar]
- 25.Hawkins D, Abrahamse H. Effect of multiple exposures of low level laser therapy on the cellular responses of wounded human skin fibroblasts. Photomed Laser Surg. 2006;24:705–714. doi: 10.1089/pho.2006.24.705. [DOI] [PubMed] [Google Scholar]
- 26.Rabelo SB, Villaverde AB, Nicolau R, Salgado MC, Melo Mda S, Pacheco MT. Comparison between wound healing in induced diabetic and nondiabetic rats after low-level laser therapy. Photomed Laser Surg. 2006;24:474–479. doi: 10.1089/pho.2006.24.474. [DOI] [PubMed] [Google Scholar]
- 27.Araújo CEN, Ribeiro MS, Favaro R, Zezell DM, Zorn TMT. Ultrastructural and autoradiographical analyses show a faster skin repair in He-Ne laser-treated wounds. J Photochem Photobiol B. 2007;86:87–96. doi: 10.1016/j.jphotobiol.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 28.Hawkins D, Abrahamse H. Influence of broad-spectrum and infrared light in combination with laser irradiation on the proliferation of wounded skin fibroblasts. Photomed Laser Surg. 2007;25:159–169. doi: 10.1089/pho.2007.2010. [DOI] [PubMed] [Google Scholar]
- 29.Houreld N, Abrahamse H. In vitro exposure of wounded diabetic fibroblast cells to a Helium-Neon laser at 5 and 16 J/cm2. Photomed Laser Surg. 2007;25:78–84. doi: 10.1089/pho.2006.990. [DOI] [PubMed] [Google Scholar]
- 30.Mirzaei M, Bayat M, Mosafa N, Mohsenifar Z, Piryaei A, Farokhi B, et al. Effect of low level laser therapy on skin fibroblasts of streptozotocin-diabetic rats. Photomed Laser Surg. 2007;25:519–525. doi: 10.1089/pho.2007.2098. [DOI] [PubMed] [Google Scholar]
- 31.Rezende SB, Ribeiro MS, Nunez SC, Garcia VG, Maldonado EP. Effects of a single near infrared laser treatment on cutaneous wound healing: biometrical and histological study in rats. J Photochem Photobiol B. 2007;87:145–153. doi: 10.1016/j.jphotobiol.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 32.Viegas VN, Abreu ME, Viezzer C, Machado DC, Filho MS, Silva DN, et al. Effect of low level laser therapy on inflammatory reactions during wound healing: comparison with meloxicam. Photomed Laser Surg. 2007;25:467–473. doi: 10.1089/pho.2007.1098. [DOI] [PubMed] [Google Scholar]
- 33.Yasukawa A, Hrui H, Koyama Y, Nagai M, Takakuda K. The effect of low reactive level laser therapy (LLLT) with Helium-Neon laser on operative wound healing in a rat model. J Vet Med Sci. 2007;69:799–806. doi: 10.1292/jvms.69.799. [DOI] [PubMed] [Google Scholar]
- 34.Houreld NN, Abrahamse H. Laser light influences cellular viability and proliferation in diabetic wounded fibroblast cells in a dose and wavelength dependent manner. Lasers Med Sci. 2008;23:11–18. doi: 10.1007/s10103-007-0445-y. [DOI] [PubMed] [Google Scholar]
- 35.Medrado AP, Soares AP, Santos ET, Reis SR, Andrade ZA. Influence of laser photobiomodulation upon connective tissue remodeling during wound healing. J Photochem Photobiol B. 2008;92:144–152. doi: 10.1016/j.jphotobiol.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 36.Meireles GC, Santos JN, Chagas PO, Moura AP, Pinheiro AL. Effectiveness of laser photobiomodulation at 660 or 780 nanometers on the repair of third-degree burns in diabetic rats. Photomed Laser Surg. 2008;26:47–54. doi: 10.1089/pho.2007.2051. [DOI] [PubMed] [Google Scholar]
- 37.Reis SR, Medrado AP, Marchionni AM, Figueira C, Fracassi LD, Knop LA. Effect of 670 nm laser therapy and dexamethasone on tissue repair: a histological and ultrastructural study. Photomed Laser Surg. 2008;26:307–313. doi: 10.1089/pho.2007.2151. [DOI] [PubMed] [Google Scholar]
- 38.Gungormus M, Akyol UK. Effect of biostimulation on wound healing in diabetic rats. Photomed Laser Surg. 2009;27:607–610. doi: 10.1089/pho.2008.2349. [DOI] [PubMed] [Google Scholar]
- 39.Skopin MD, Molitor SC. Effects of near infrared laser exposure in a cellular model of wound healing. Photodermatol Photoimmunol Photomed. 2009;25:75–80. doi: 10.1111/j.1600-0781.2009.00406.x. [DOI] [PubMed] [Google Scholar]
- 40.Carvalho PTC, Silva IS, Reis FA, Perreira DM, Aydos RD. Influence of ingaalp laser (660 nm) on the healing of skin wounds in diabetic rats. Acta Cir Bras. 2010;25:71–79. doi: 10.1590/s0102-86502010000100016. [DOI] [PubMed] [Google Scholar]
- 41.Chung TY, Peplow PV, Baxter GD. Laser photobiostimulation of wound healing: defining a dose response for splinted wounds in diabetic mice. Lasers Surg Med. 2010;42:656–664. doi: 10.1002/lsm.20981. [DOI] [PubMed] [Google Scholar]
- 42.Gonçalves RV, Novaes RD, Matta SL, Benevides GP, Faria FR, Pinto MV. Comparative study of the effects of gallium-aluminum-arsenide laser photobiomodulation and healing oil on skin wounds in wistar rats: a histomorphometric study. Photomed Laser Surg. 2010;28:597–602. doi: 10.1089/pho.2009.2669. [DOI] [PubMed] [Google Scholar]
- 43.Gonçalves RV, Mezêncio JM, Benevides GP, Matta SL, Neves CA, Sarandy MM, et al. Effect of gallium-arsenide laser, gallium-aluminum-arsenide laser and healing ointment on cutaneous wound healing in Wistar rats. Braz J Med Biol Res. 2010;43:350–355. doi: 10.1590/S0100-879X2010007500022. [DOI] [PubMed] [Google Scholar]
- 44.de Oliveira Guirro EC, de Lima Montebelo MI, de Almeida Bortot B, da Costa Betito Torres MA, Polacow ML. Effect of laser (670 nm) on healing of wounds covered with occlusive dressing: a histologic and biomechanical analysis. Photomed Laser Surg. 2010;28:629–634. doi: 10.1089/pho.2008.2387. [DOI] [PubMed] [Google Scholar]
- 45.Houreld N, Abrahamse H. Low-intensity laser irradiation stimulates wound healing in diabetic wounded fibroblast cells (WS1) Diabetes Technol Ther. 2010;12:971–978. doi: 10.1089/dia.2010.0039. [DOI] [PubMed] [Google Scholar]
- 46.Lacjaková K, Bobrov N, Poláková M, Slezák M, Vidová M, Vasilenko T, et al. Effects of equal daily doses delivered by different power densities of low-level laser therapy at 670 nm on open skin wound healing in normal and corticosteroid-treated rats: a brief report. Lasers Med Sci. 2010;25:761–766. doi: 10.1007/s10103-010-0791-z. [DOI] [PubMed] [Google Scholar]
- 47.Medeiros JL, Nicolau RA, Nicola EM, dos Santos JN, Pinheiro AL. Healing of surgical wounds made with l970-nm diode laser associated or not with laser phototherapy (l655 nm) or polarized light (l400-2000 nm) Photomed Laser Surg. 2010;28:489–496. doi: 10.1089/pho.2009.2592. [DOI] [PubMed] [Google Scholar]
- 48.Hussein AJ, Alfars AA, Falih MA, Hassan AN. Effects of a low level laser on the acceleration of wound healing in rabbits. N Am J Med Sci. 2011;3:193–197. doi: 10.4297/najms.2011.3193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Silveira PC, Silva LA, Freitas TP, Latini A, Pinho RA. Effects of low-power laser irradiation (LPLI) at different wavelengths and doses on oxidative stress and fibrogenesis parameters in an animal model of wound healing. Lasers Med Sci. 2011;26:125–131. doi: 10.1007/s10103-010-0839-0. [DOI] [PubMed] [Google Scholar]
- 50.Weng Y, Dang Y, Ye X, Liu N, Zhang Z, Ren Q. Investigation of irradiation by different nonablative lasers on primary cultured skin fibroblasts. Clin Exp Dermatol. 2011;36:655–660. doi: 10.1111/j.1365-2230.2011.04043.x. [DOI] [PubMed] [Google Scholar]
- 51.Basso FG, Pansani TN, Turrioni AP, Bagnato VS, Hebling J, de Souza Costa CA. In vitro wound healing improvement by low-level laser therapy application in cultured gingival fibroblasts. Int J Dent. 2012;2012:719452. doi: 10.1155/2012/719452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Crisan B, Soritau O, Baciut M, Campian R, Crisan L, Baciut G. Influence of three laser wavelengths on human fibroblasts cell culture. Lasers Med Sci. 2013;28:457–463. doi: 10.1007/s10103-012-1084-5. [DOI] [PubMed] [Google Scholar]
- 53.Dawood MS, Salman SD. Low level diode laser accelerates wound healing. Lasers Med Sci. 2013;28:941–945. doi: 10.1007/s10103-012-1182-4. [DOI] [PubMed] [Google Scholar]
- 54.Fahimipour F, Mahdian M, Houshmand B, Asnaashari M, Sadrabadi AN, Farashah SE, et al. The effect of He-Ne and Ga-Al-As laser light on the healing of hard palate mucosa of mice. Lasers Med Sci. 2013;28:93–100. doi: 10.1007/s10103-012-1060-0. [DOI] [PubMed] [Google Scholar]
- 55.Gonçalves RV, Novaes RD, Cupertino Mdo C, Moraes B, Leite JP, Peluzio Mdo C, et al. Time-dependent effects of low-level laser therapy on the morphology and oxidative response in the skin wound healing in rats. Lasers Med Sci. 2013;28:383–390. doi: 10.1007/s10103-012-1066-7. [DOI] [PubMed] [Google Scholar]
- 56.Núñez SC, França CM, Silva DF, Nogueira GE, Prates RA, Ribeiro MS. The influence of red laser irradiation timeline on burn healing in rats. Lasers Med Sci. 2013;28:633–641. doi: 10.1007/s10103-012-1105-4. [DOI] [PubMed] [Google Scholar]
- 57.Whelan HT, Smits RL, Jr, Buchman EV, Whelan NT, Turner SG, Margolis DA, et al. Effect of NASA light-emitting diode irradiation on wound healing. J Clin Laser Med Surg. 2001;19:305–314. doi: 10.1089/104454701753342758. [DOI] [PubMed] [Google Scholar]
- 58.Vinck EM, Cagnie BJ, Cornelissen MJ, Declercq HA, Cambier DC. Green light emitting diode irradiation enhances fibroblast growth impaired by high glucose level. Photomed Laser Surg. 2005;23:167–171. doi: 10.1089/pho.2005.23.167. [DOI] [PubMed] [Google Scholar]
- 59.Weiss RA, McDaniel DH, Geronemus RG, Weiss MA. Clinical trial of a non-thermal LED array for reversal of photoaging: clinical, histologic and surface profilometric results. Lasers Surg Med. 2005;36:85–91. doi: 10.1002/lsm.20107. [DOI] [PubMed] [Google Scholar]
- 60.Huang PJ, Huang YC, Su MF, Yang TY, Huang JR, Jiang CP. In vitro observations on the influence of copper peptide aids for the LED photoirradiation of fibroblast collagen synthesis. Photomed Laser Surg. 2007;25:183–190. doi: 10.1089/pho.2007.2062. [DOI] [PubMed] [Google Scholar]
- 61.Lanzafame RJ, Stadler I, Kurtz AF, Connelly R, Peter TA, Sr, Brondon P, et al. Reciprocity of exposure time and irradiance on energy density during photoradiation on wound healing in a murine pressure ulcer model. Lasers Surg Med. 2007;39:534–542. doi: 10.1002/lsm.20519. [DOI] [PubMed] [Google Scholar]
- 62.Dall Agnol MA, Nicolau RA, de Lima CJ, Munin E. Comparative analysis of coherent light action (laser) versus non-coherent light (light-emitting diode) for tissue repair in diabetic rats. Lasers Med Sci. 2009;24:909–916. doi: 10.1007/s10103-009-0648-5. [DOI] [PubMed] [Google Scholar]
- 63.Tada K, Ikeda K, Tomita K. Effect of polarized light emitting diode irradiation on wound healing. J Trauma. 2009;67:1073–1079. doi: 10.1097/TA.0b013e318187ad02. [DOI] [PubMed] [Google Scholar]
- 64.Komine N, Ikeda K, Tada K, Hashimoto N, Sugimoto N, Tomita K. Activation of the extracellular signal-regulated kinase signal pathway by light emitting diode irradiation. Lasers Med Sci. 2010;25:531–537. doi: 10.1007/s10103-009-0743-7. [DOI] [PubMed] [Google Scholar]
- 65.Meyer PF, Araújo HG, Carvalho MGF, Tatum BIS, Fernandes ICAG, Ronzio OA, et al. Avaliação dos efeitos do LED na cicatrização de feridas cutâneas em ratos Wistar (Assessment of effects of LED on skin wound healing in Wistar rats) Fisioter Bras. 2010;11:428–432. [Google Scholar]
- 66.de Sousa AP, Santos JN, Dos Reis JA, Jr, Ramos TA, de Souza J, Cangussú MC, et al. Effect of LED phototherapy of three distinct wavelengths on fibroblasts on wound healing: a histological study in a rodent model. Photomed Laser Surg. 2010;28:547–552. doi: 10.1089/pho.2009.2605. [DOI] [PubMed] [Google Scholar]
- 67.Adamskaya N, Dungel P, Mittermayr R, Hartinger J, Feichtinger G, Wassermann K, et al. Light therapy by blue LED improves wound healing in an excision model in rats. Injury. 2011;42:917–921. doi: 10.1016/j.injury.2010.03.023. [DOI] [PubMed] [Google Scholar]
- 68.Lim WB, Kim JS, Ko YJ, Kwon H, Kim SW, Min HK, et al. Effects of 635nm lightemitting diode irradiation on angiogenesis in CoCl2-exposed HUVECs. Lasers Surg Med. 2011;43:344–352. doi: 10.1002/lsm.21038. [DOI] [PubMed] [Google Scholar]
- 69.Cheon MW, Kim TG, Lee YS, Kim SH. Low level light therapy by Red-Green-Blue LEDs improves healing in an excision model of Sprague-Dawley rats. Pers Ubiquit Comput. 2013;17:1421–1428. [Google Scholar]
- 70.Fushimi T, Inui S, Nakajima T, Ogasawara M, Hosokawa K, Itami S. Green light emitting diodes accelerates wound healing: characterization of the effect and its molecular basis in vitro and in vivo. Wound Repair Regen. 2012;20:226–235. doi: 10.1111/j.1524-475X.2012.00771.x. [DOI] [PubMed] [Google Scholar]
- 71.Vinck EM, Cagnie BJ, Cornelissen MJ, Declercq HA, Cambier DC. Increased fibroblast proliferation induced by light emitting diode and low power laser irradiation. Lasers Med Sci. 2003;18:95–99. doi: 10.1007/s10103-003-0262-x. [DOI] [PubMed] [Google Scholar]
- 72.Corazza AV, Jorge J, Kurachi C, Bagnato VS. Photobiomodulation on the angiogenesis of skin wounds in rats using different light sources. Photomed Laser Surg. 2007;25:102–106. doi: 10.1089/pho.2006.2011. [DOI] [PubMed] [Google Scholar]
- 73.Volpato LE, de Oliveira RC, Espinosa MM, Bagnato VS, Machado MA. Viability of fibroblasts cultured under nutritional stress irradiated with red laser, infrared laser, and red light-emitting diode. J Biomed Opt. 2011;16: doi: 10.1117/1.3602850. [DOI] [PubMed] [Google Scholar]
- 74.Nishioka MA, Pinfildi CE, Sheliga TR, Arias VE, Gomes HC, Ferreira LM. LED (660 nm) and laser (670 nm) use on skin flap viability: angiogenesis and mast cells on transition line. Lasers Med Sci. 2012;27:1045–1050. doi: 10.1007/s10103-011-1042-7. [DOI] [PubMed] [Google Scholar]
- 75.Oliveira Sampaio SC, de C Monteiro JS, Cangussú MC, Pires Santos GM, dos Santos MA, dos Santos JN, et al. Effect of laser and LED phototherapies on the healing of cutaneous wound on healthy and iron-deficient Wistar rats and their impact on fibroblastic activity during wound healing. Lasers Med Sci. 2013;28:799–806. doi: 10.1007/s10103-012-1161-9. [DOI] [PubMed] [Google Scholar]
- 76.de Sousa AP, Paraguassú GM, Silveira NT, de Souza J, Cangussú MC, dos Santos JN, et al. Laser and LED phototherapies on angiogenesis. Lasers Med Sci. 2013;28:981–987. doi: 10.1007/s10103-012-1187-z. [DOI] [PubMed] [Google Scholar]
- 77.Dias IFL, Siqueira CPCM, Toginho DO, Filho, Duarte JL, Laureto E, Lima FM, et al. Efeitos da luz em sistemas biológicos. Semina. 2009;30:33–40. [Google Scholar]
- 78.Schindl A, Schindl M, Pernerstorfer-Schon H, Schindl L. Low-intensity laser therapy. J Investig Med. 2000;48:312–326. [PubMed] [Google Scholar]
- 79.Schubert EF. Light emitting diodes. New York: Cambridge University Press; 2003. [Google Scholar]
- 80.Posten W, Wrone DA, Dover JS, Arndt KA, Silapunt S, Alam M. Low-level laser therapy for wound healing: mechanism and efficacy. Dermatol Surg. 2005;31:334–340. doi: 10.1111/j.1524-4725.2005.31086. [DOI] [PubMed] [Google Scholar]
- 81.Huang YY, Chen ACH, Hamblin M. Low-level laser therapy: an emerging clinical paradigm. SPIE Newsroom. 2009;9:1–3. [Google Scholar]
- 82.Sommer AP, Pinheiro AL, Mester AR, Franke RP, Whelan HT. Biostimulatory windows in low-intensity laser activation: lasers, scanners, and NASA's light-emitting diode array system. J Clin Laser Med Surg. 2001;19:29–33. doi: 10.1089/104454701750066910. [DOI] [PubMed] [Google Scholar]
- 83.Karu TI. Primary and secondary mechanisms of action of visible to near-IR radiation on cells. J Photochem Photobiol B. 1999;49:1–17. doi: 10.1016/S1011-1344(98)00219-X. [DOI] [PubMed] [Google Scholar]
- 84.Karu TI. Vo-Dinh T. Biomedical photonics handbook. Florida: CRC Press; 2003. Low-power laser therapy. [Google Scholar]
- 85.Karu TI, Kolyakov SF. Exact action spectra for cellular responses relevant to phototherapy. Photomed Laser Surg. 2005;23:355–361. doi: 10.1089/pho.2005.23.355. [DOI] [PubMed] [Google Scholar]
- 86.Karu TI. Photobiological fundamentals of low-power laser therapy. IEEE J Quantum Electron. 1987;23:1703–1717. [Google Scholar]
- 87.Karu TI. Molecular mechanism of the therapeutic effect of low intensity laser radiation. Lasers Life Sci. 1988;2:53–74. [Google Scholar]
- 88.Karu TI, Tiphlova OA, Matveyets Yu A, Yartsev AP, Letokhov VS. Comparison of the effects of visible femtosecond laser pulses and continuous wave laser radiation of low average intensity on the clonogenicity of Escherichia coli. J Photochem Photobiol B. 1991;10:339–344. doi: 10.1016/1011-1344(91)80019-e. [DOI] [PubMed] [Google Scholar]
- 89.Karu TI, Andreichuk T, And Ryabykh T. Changes in oxidative metabolism of murine spleen following diode laser (660-950nm) irradiation: effect of cellular composition and radiation parameters. Lasers Surg Med. 1993;13:453–462. doi: 10.1002/lsm.1900130410. [DOI] [PubMed] [Google Scholar]
- 90.Karu TI, Kalendo GS, Letokhov VS. Control of RNA synthesis rate in tumor cells HeLa by action of low-intensity visible light of copper laser. Lett Nuov Cim. 1981;32:55–59. [Google Scholar]
- 91.Karu TI, Pyatibrat LV, Afanasyeva NI. Cellular effects of low power laser therapy can be mediated by nitric oxide. Lasers Surg Med. 2005;36:307–314. doi: 10.1002/lsm.20148. [DOI] [PubMed] [Google Scholar]
- 92.Karu TI. The science of low-power laser therapy. Amsterdam: Gordon & Breach Science; 1998. [Google Scholar]
- 93.Ribeiro MS, Zezell DMP. Gutknecht N, Eduardo CP. A Odontologia e o laser - Atuação do laser na especialidade odontológica (Dentistry and laser: laser action in an odontological specialty) São Paulo: Quintessence Editora; 2004. Laser de baixa intensidade (Low intensity laser) [Google Scholar]
- 94.Nussbaum EL, Baxter GD, Lilge L. A review of laser technology and light-tissue interactions as a background to therapeutic applications of low intensity lasers and other light sources. Phys Ther Rev. 2003;8:31–44. [Google Scholar]
- 95.Viera Alemán C, Purón E, Hamilton ML, Santos Anzorandia C, Navarro A, Pineda Ortiz I. Evaluation of motor and sensory neuroconduction of the median nerve in patients with carpal tunnel syndrome treated with non-coherent light emitted by gallium arsenic diodes. Rev Neurol. 2001;32:717–720. [PubMed] [Google Scholar]
- 96.Enwemeka CS. The place of coherence in light induced tissue repair and pain modulation. Photomed Laser Surg. 2006;24:457. doi: 10.1089/pho.2006.24.457. [DOI] [PubMed] [Google Scholar]