Abstract
Background
Liver fibrosis stage is an important factor in determining prognosis and need for treatment in patients infected with hepatitis B virus (HBV). Liver biopsies are typically used to assess liver fibrosis; however, noninvasive alternatives such as the FIB-4 index have also been developed.
Aims
To quantify the accuracy of the FIB-4 index in the diagnosis of HBV related fibrosis and cirrhosis.
Methods
A meta-analysis of studies comparing the diagnostic accuracy of the FIB-4 index vs. liver biopsy in HBV-infected patients was performed using studies retrieved from the following databases: PubMed, Ovid, EMBASE, the Cochrane Library, the Chinese National Knowledge Infrastructure and the Chinese Biology Medicine disc. A hierarchical summary receiver operating curves model and bivariate model were used to produce summary receiver operating characteristic curves and pooled estimates of sensitivity and specificity. The heterogeneity was explored with meta-regression analysis. Publication bias was detected using Egger’s test and the trim and fill method.
Results
12 studies (N = 1,908) and 10 studies (N = 2,105) were included in the meta-analysis for significant fibrosis and cirrhosis, respectively. For significant fibrosis, the area under the hierarchical summary receiver operating curve (AUHSROC) was 0.78 (95% CI = 0.74–0.81). The recommended cutoff value was between 1.45 and 1.62, and the AUHSROC, summary sensitivity and specificity were 0.78 (95% CI = 0.74–0.81), 0.65 (95% CI = 0.56–0.73) and 0.77 (95% CI = 0.7–0.83), respectively. For cirrhosis, the AUHSROC was 0.89 (95% CI = 0.85–0.91). The recommended cutoff value was between 2.9 and 3.6, and the AUHSROC, summary sensitivity and specificity were 0.96 (95% CI = 0.92–1.00), 0.42 (95% CI = 0.36–0.48) and 0.96 (95% CI = 0.95–0.97), respectively. No publication bias was detected.
Conclusions
The FIB-4 index is valuable for detecting significant fibrosis and cirrhosis in HBV-infected patients, but has suboptimal accuracy in excluding fibrosis and cirrhosis.
Introduction
An accurate assessment of liver fibrosis in patients with hepatitis virus B (HBV) infection is essential not only in determining whether and when to initiate antiviral therapy, but also in predicting long-term clinical prognosis [1]–[3]. For example, with regard to antiviral therapy, it is known that maintenance of viral suppression can reduce liver-related complications in chronic hepatitis B (CHB) patients [1]–[3]. Furthermore, assessing prognosis in patients with cirrhosis is required to closely follow the potential development of hepatocellular carcinoma and other complications [2], [4].
To date, liver biopsy remains the gold standard for assessing liver fibrosis; however, it does have some limitations. The invasive nature of the biopsy is associated with patient discomfort, and can cause rare but important complications [5]. Furthermore, its accuracy is affected by sampling error and variability in pathological interpretation [6], [7], and the dynamic process of liver fibrosis related to disease progression and regression cannot be easily quantified. An ideal diagnostic index should be accurate, noninvasive, inexpensive, convenient and readily available. The limitations of the liver biopsy have lead many clinicians to develop noninvasive indexes, and most attention has been focused on whether noninvasive indexes can detect the presence or absence of significant fibrosis (i.e., ≥F2), severe fibrosis (i.e., ≥F3) and cirrhosis (i.e., ≥F4) according to the METAVIR histological score [8].
Currently, there are several categories of non-invasive indexes. Measures of hyaluronic acid, collagen, laminin and YKL-40 are direct laboratory indexes, but these are usually not routinely available. Indirect laboratory indexes are calculated from routine laboratory data, and include the aspartate aminotransferase (AST) to alanine aminotransferase (ALT) ratio (AAR), the AST to platelet (PLT) ratio index (APRI), the cirrhosis discriminant score (CDS), the age-PLT index (API), the FIB-4 index (see below), Lok’s model and the red cell distribution width (RDW) to platelet ratio [9]–[11]. While some of the calculations for these indexes are simple and accessible, some are more complex [11]. Assessment of these indexes has been reviewed and found to vary from bad to excellent [9], [11]; however, relevant systematic reviews in the context of HBV are rare. Thus, no current index has satisfied all the standards of the ideal diagnostic index [12].
The FIB-4 index is calculated using the formula: FIB-4 = Age (years)×AST (U/L)/[PLT(109/L)×ALT1/2 (U/L)]. The theoretical basis for this index has been previously described [13], and adheres to the following logic: (1) age is considered to be relevant to disease duration and is associated with more severe fibrosis; (2) elevations in AST more than ALT has been related to both delayed clearance of AST relative to ALT, and to the mitochondrial injury associated with more advanced fibrosis; (3) thrombocytopenia has been associated with the progression of fibrosis and worsening portal hypertension that not only destroys platelets by sequestration in the enlarged spleen, but also decreases the production of thrombopoietin by hepatocytes. Based on these foundations, the FIB-4 index was first applied to assess hepatic fibrosis in the context of human immunodeficiency virus (HIV) and hepatitis C virus (HCV) infection [14], [15].
The diagnostic value of the FIB-4 index is attractive because measures of AST, ALT and PLT are routine and inexpensive tests in the clinical laboratory, and the calculation is simple. Numerous studies have assessed the diagnostic performance of the FIB-4 index in HBV-related fibrosis and cirrhosis [10], [11], [13], [16]–[32], with several showing that the FIB-4 index was superior in comparison to other non-invasive indexes [9], [13], [16]. Despite the benefit shown by these studies, the utility of the FIB-4 index remains controversial. Thus, the aim of the current study was to perform a meta-analysis of diagnostic tests for predicting the accuracy of the FIB-4 index in predicting significant fibrosis (F2–F4 vs. F0–F1), severe fibrosis (F3–F4 vs. F0–F2) and cirrhosis (F4 vs. F0–F3) in patients with HBV infection.
Materials and Methods
Ethics statement
The data of this meta-analysis was extracted from published studies. So the data were analyzed anonymously.
Literature and search strategy
The following databases were searched without the use of time limitations: PubMed, Ovid, EMBASE, the Cochrane Library, the Chinese National Knowledge Infrastructure (CNKI) and the Chinese Biology Medicine disc (CBMdisc). The search strategy to identify all relevant articles involved the use of the following key words: FIB-4, aspartate aminotransferase, AST, alanine aminotransferase, ALT, platelet, PLT, hepatitis B, fibrosis and cirrhosis. For example, File S1 and S2 displayed the search strategy of Ovid and PubMed respectively. Additional studies were identified via a manual review of the reference lists of identified studies and review articles. This literature search was performed in November 2013.
Inclusion criteria
Studies were deemed eligible if they met the following inclusion criteria: 1) the study evaluated the performance of the FIB-4 index for the diagnosis of fibrosis in mono-HBV-infected patients before antiviral therapy. Studies including patients with other causes of liver disease were included if data of HBV-infected patients could be extracted. 2) Liver biopsy was used as the reference standard for assessing fibrosis. METAVIR [8] or comparable staging systems (i.e., Batts and Ludwig [33], Scheuer [34] or Ishak [35]) were applied to stage fibrosis. Significant fibrosis was defined as F≥2 for METAVIR, Batts and Ludwig, and Scheuer staging systems; or F≥3 for the Ishak system. Severe fibrosis was defined as F≥3 for METAVIR, Batts and Ludwig, and Scheuer staging systems. Cirrhosis was defined as F≥4 for METAVIR, Batts and Ludwig, and Scheuer staging systems; or F≥5 for the Ishak system. 3) Data could be extracted to allow the construction of at least one 2×2 table of test performance. 4) The study included more than 40 patients; otherwise it was excluded because of low statistical power and poor reliability.
Quality assessment and data extraction
Two reviewers (Drs. Li and Zhao) independently evaluated the eligibility of each study according to the inclusion criteria described above, and assessed methodological quality according to the Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool [36]. Discrepancies were resolved by consensus agreement. Note – some specific issues were defined before assessment, e.g. CHB was defined as hepatitis B surface antigen positive for more than 6 months. With regard to disease progression bias, the time interval between the determination of the FIB-4 index and liver biopsy was no longer than 7 days. As the FIB-4 index was calculated from four objective measures (ALT, AST, PLT and age), the item relating to blinding of the test interpreter to results of the reference standard was omitted. In addition to 2×2 tables of test performance, two kinds of data (patient related data and study related data) were also extracted. The patient related data included mean age, gender distribution, region and prevalence of the fibrosis stages. The study related data included sample size, interval time between determination of the FIB-4 index and liver biopsy, the size of liver biopsy, histological scoring system, blinded interpretation of the biopsy, and the cutoff value of the FIB-4. To avoid double counting of data, when multiple pairs of sensitivity or specificity were reported in one study, we consistently used the data with the highest Youden index (sensitivity + specificity-1) for meta-analysis [37], except for subgroup analysis based on different cutoff values.
Statistical analyses
For meta-analyses, a bivariate random effects model [38] was used to calculate summary estimates of sensitivity, specificity, positive likelihood ratio (PLR) and negative likelihood ratio (NLR), and to fit a hierarchical summary receiver-operating characteristic (HSROC) curve [39]. These models take into account potential threshold effects and the correlation between sensitivity and specificity. They also allow addition of covariates for investigation of potential sources of heterogeneity, thus are standard methods recommended for meta-analyses of diagnostic tests [40], [41]. Additionally, the following guidelines have been suggested for interpretation of the area under the hierarchical summary receiver-operating characteristic curve (AUHSROC): an area of 1.0 indicates perfect discrimination, and 0.90 to 1.0 has been classified as excellent, 0.80 to less than 0.90 as good, 0.70 to less than 0.80 as fair, and less than 0.70 as poor [42], [43].
Multiple sources of heterogeneity frequently exist in diagnostic studies. In addition to visual assessment with the use of the forest plots, we formally quantified the extent of heterogeneity by calculating the inconsistency index (I2 statistics) [44]. Statistically significant heterogeneity was considered present at I2>50%. To explore the source of heterogeneity, meta-regression and subgroup analysis were performed. The potential factors evaluated by meta-regression analysis were mean age of subjects, prevalence of fibrosis stages, disease spectrum, a consecutive or random sample enrollment, interval between FIB-4 index determination and liver biopsy, the liver blinded biopsy interpretation and a predefined cutoff value.
With respect to publication bias, the funnel plot is a basic and routine method for detecting biases, but it is subjective and qualitative. To counter these limitations, several quantitative methods such as Egger’s test [45] and the trim and fill method [46] have been developed. Egger’s test quantifies the degree of funnel plot asymmetry as measured by the intercept from regression of standard normal deviates against precision, but its capacity to detect bias is limited when meta-analyses are based on a limited number of small trials [45]. The trim and fill method is a nonparametric method for estimating the number of missing studies that might exist in a meta-analysis and the effect that these studies might have had on its outcome. This method also provides effective and relatively powerful tests for evaluating the existence of such publication bias [46]. To be cautious, the publication bias was assessed with two distinct methods. Statistical analyses were conducted using Review Manager 5.2 (The Cochrane Collaboration) and STATA 11.0 (Stata Corp., College Station, TX, USA), notably with the user-written ‘midas’ and ‘metandi’ programs for STATA.
Results
Search results
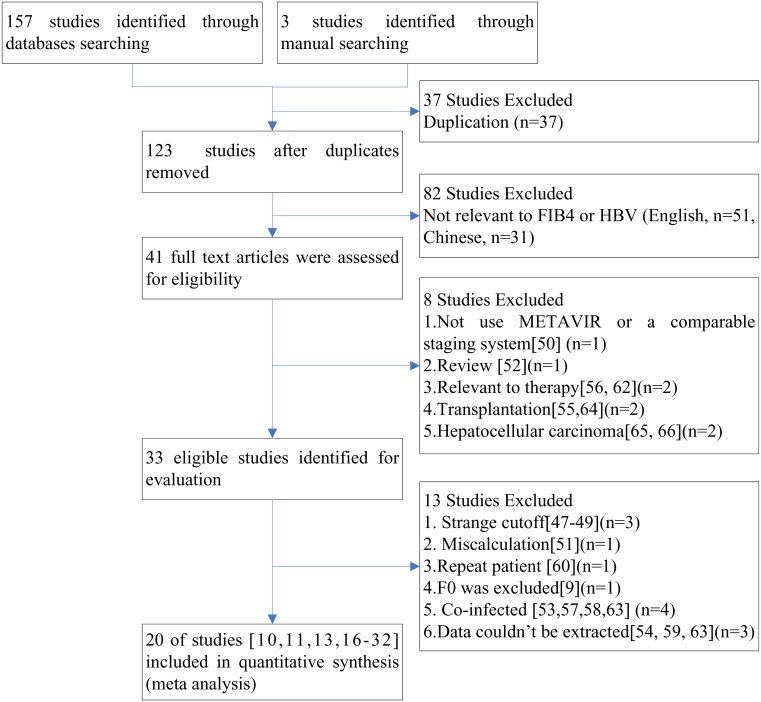
One hundred and sixty studies were retrieved based on the described search strategies. One hundred and forty studies [9], [47]–[66] were excluded in accord with our exclusion criteria (Figure 1). Xu et al. defined cutoff values for the FIB-4 index as 223.70 for predicting significant fibrosis and 808.77 for cirrhosis [47], and Gumusay et al. reported that the average FIB-4 index for healthy controls was 11.7±5.8 [48]. These cutoff values were much larger than that of other studies, which ranged from 0.8 to 4.9, and we could not calculate similar cutoff values from the data included in these articles, thus they were excluded [47], [48]. Wong et al. calculated cutoff values based on a >90% sensitivity to exclude and >90% specificity to confirm advanced liver fibrosis [49]. This method was different from other studies, so it was also excluded. Two studies [13], [60] included the same patient populations, thus the study with the smaller sample size and data that could not be extracted was excluded [60]. As the true negative and false positive patients of the study by Jing et al. were underestimated because they excluded non-fibrotic samples (i.e.,F0), we excluded it [9]. Ultimately, 20 studies [10], [11], [13], [16]–[32] were eligible for evaluation, and their characteristics are listed in Table 1. Although two studies [22], [32] were written by the same author, the patients were collected at different times and the study with the smaller sample size [32] was excluded for further sensitivity analysis.
Figure 1. Flow chart of article selection.
Table 1. Characteristics of studies eligible for meta-analysis.
| Author, Year, Region | Number(male%) | Age(years) | IntervalBetweenBiopsyand FIB-4 | Liver BiopsyScoringsystem | LiverBiopsyLength | Blinded |
| Chen[10], 2013, China | 148 (66%) | 40.36±11.2 | ≤7d | Metavir | >15 mm | Yes |
| Kim[13], 2010, Korea | 668 (66%) | 39.1±14.8 | ≤2d | Batts and Ludwig | >15 mm | Yes |
| Zhu[29], 2012, China | 159 (71%) | 42 (18∼62) | unclear | METAVIR | ≥15 mm | unclear |
| Ucar[18], 2013, Turkey | 73 (64%) | 42.81±12.86 | unclear | METAVIR | unclear | Yes |
| Gong[21], 2013, China | 41 (73%) | 50.8±10.3 | unclear | METAVIR | unclear | unclear |
| Wang[20], 2013, China | 231 (68%) | 34.1±9.8 | <1d | Scheuer | >15 mm | Yes |
| Ji[17], 2011, China | 313 (69%) | 35.6±11.2 | 1d | METAVIR | 20 mm | unclear |
| Başar[25], 2013, Turkey | 76 (55%) | unclear | <1d | METAVIR | >10 mm | Yes |
| Bonnard[19], 2010, France | 59 (68%) | 35±9 | 0.5–10 m | METAVIR | 21±6 mm | Yes |
| Erdogan[11], 2013, Turkey | 221 (63%) | 43.68±12.56 | ≤1d | Ishak | unclear | Yes |
| Wu[30], 2010, China | 78 (85%) | 32.6±12.3 | unclear | METAVIR | >15 mm | unclear |
| Mallet[16], 2009, France | 138 (71%) | 42±15 | <1d | METAVIR | 17.6±6.8 | unclear |
| Seto[24], 2011, China | 237 (68%) | 38.2 (18∼63) | same time | Ishak | ≥15 mm | Yes |
| Zhu[27], 2011, China | 175 (78%) | 36.5±9.4 | ≤7d | METAVIR | >15 mm | Yes |
| Liu[23], 2012, China | 114 (80%) | 38.32±11.36 | same time | METAVIR | 15∼20 mm | unclear |
| Wang[26], 2013, China | 149 (93%) | 37 (30∼42) | ≤2d | Scheuer | >10 mm | Yes |
| Xun[28], 2013, China | 197 (76%) | 31 (21–45) | same time | Scheuer | >15 mm | unclear |
| Zhang[32], 2009, China | 86 (60%) | 39 (16–64) | <1d | METAVIR | 15∼20 mm | unclear |
| Zhang[22], 2012, China | 361 (62%) | 36±11 | ≤7d | Scheuer | unclear | unclear |
| Zhang[31], 2010, China | 212 (88%) | 31±7 | 1day | Scheuer | 20 mm | Yes |
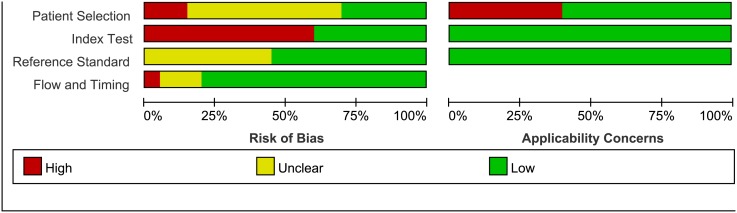
A cumulative bar plot of risk of bias and applicability concerns across all studies derived from QUADAS-2 was constructed (Figure 2). Unfortunately, a few studies stated that a consecutive or random sample of patients were enrolled, so there were not enough studies to do further subgroup analysis or sensitivity analysis. Despite this limitation, these factors were assessed in meta-regression for exploring sources of heterogeneity. The disease spectrum of 9 studies [11], [17], [19]–[21], [24], [26]–[28] were not in good accordance with our study and were excluded for further sensitivity analysis. Specifically, three of these studies [20], [24], [27] focused on patients with limited ALT (normal or less than 2× upper limit of normal), one focused on Hepatitis B virus e antigen (HBeAg)-positive patients [28], one focused on HBeAg-negative patients [26], one defined the urea nitrogen limitation when collecting samples [11], one included patients after therapy [19], one only included inpatients [17], and one did not describe the objective of the study clearly [21]. The bias of index test was mainly because many studies didn’t predefine the cutoff value. Five studies were found to have a disease progression bias [18], [19], [21], [29], [30], and nine studies did not describe whether interpretation of liver biopsy specimens was blinded to other test results [16], [17], [21]–[23], [28]–[30], [32].
Figure 2. Methodological quality graph.
Summary of methodological quality of studies according to Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool concerning risk of bias and applicability in review authors’ judgments about each domain for each included study and review authors’ judgments about each domain, presented as percentages across included studies.
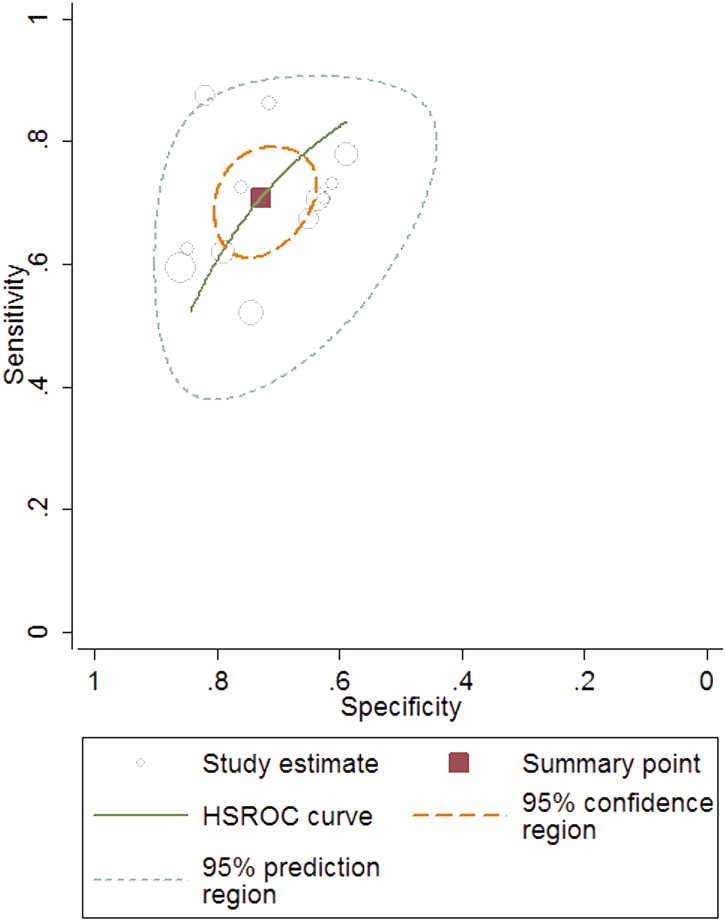
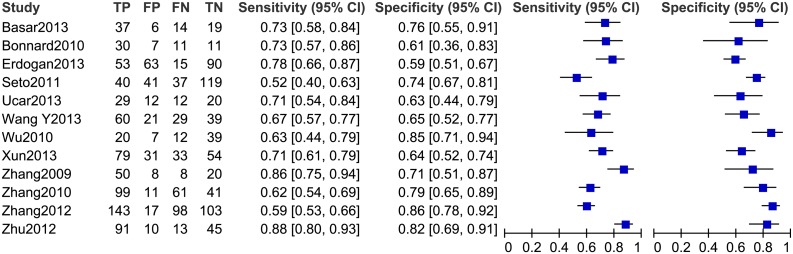
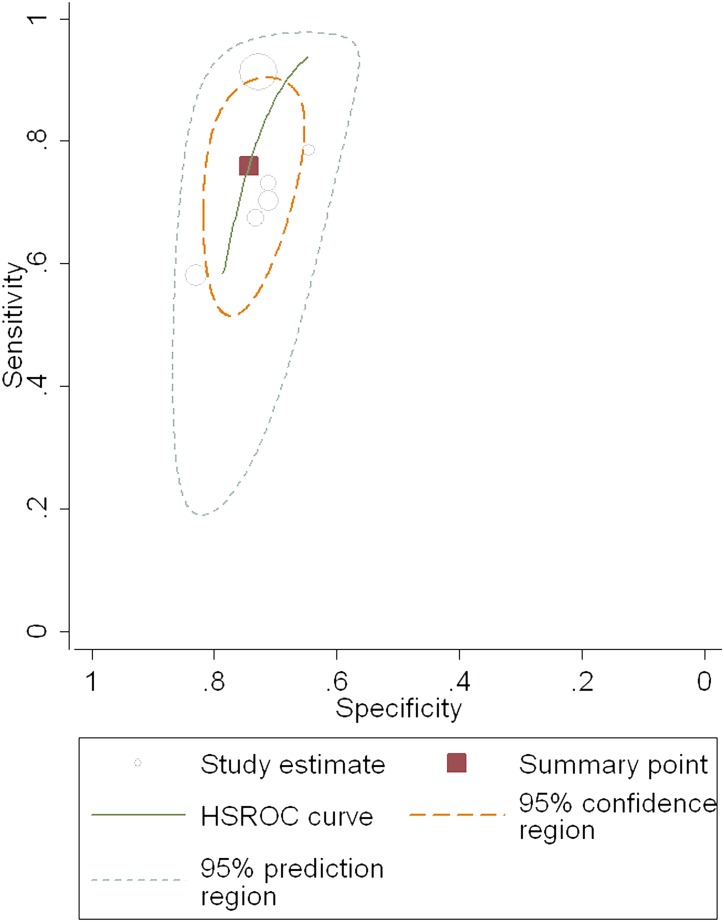
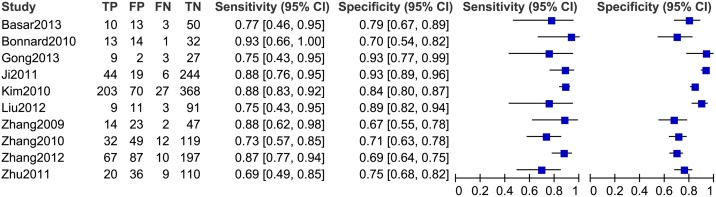
Diagnostic accuracy of the FIB-4 index for predicting significant fibrosis
Twelve studies, including 1,908 patients (male: 71%; average age: 37.1 years; average prevalence 57.4%) were used in our meta-analysis for testing the diagnostic accuracy of the FIB-4 index for predicting significant fibrosis (i.e. METAVIR F2–F4 vs. F0–F1; Table 2). The area under the HSROC was 0.78 (95% CI = 0.74–0.81; Figure 3). The summary sensitivity and specificity were 0.71 (95% CI = 0.64–0.77) and 0.73 (95% CI = 0.67–0.78), respectively (Figure 4). The heterogeneity was significant (I2 = 94%), and the meta-regression showed that disease spectrum (P = 0.00) and blindness (P = 0.05) lead to the heterogeneity. The diagnostic performance of the FIB-4 index was improved after excluding studies with improper disease spectrum (Table 2). Although the data derived from blinded tests was more reliable, it was understandable that the diagnostic performance of the non-blinded subgroup (AUHSROC = 0.83) was better than that of the blinded subgroup (AUHSROC = 0.73). We also performed a subgroup analysis based on different cutoff values (Table 3). Based on the highest AUHSROC, the most appropriate cutoff value for detecting significant fibrosis was between 1.45 and 1.62, with a PLR of 2.83, and a NLR of 0.45. This means that patients with significant fibrosis have about 3-fold higher chance of being FIB-4 positive (above 1.62) compared with patients without significant fibrosis. If the FIB-4 was below the cutoff value, the probability that the patient has significant fibrosis was 45%. Thus, the FIB-4 index with a cutoff value between 1.45 and 1.62 was not suitable as a test for excluding the presence of significant fibrosis. Additionally, when a cutoff value of 3.25 is used, the PLR (6.04, 95% CI = 2.61–13.96) of the FIB-4 index is high enough to be used as a test to identify significant fibrosis. As none of subgroups (Table 3) has a sufficiently low NLR to be used to exclude significant fibrosis, FIB-4 index has suboptimal accuracy in excluding significant fibrosis.
Table 2. The diagnostic performance of the FIB-4 index for detecting significant fibrosis, severe fibrosis and cirrhosis.
| Study characteristics | Number ofstudies | Summary estimates (95% CI) | Likelihood ratio (95% CI) | AUHSROC(95% CI) | ||||||||||
| Sensitivity | Specificity | DOR | PLR | NLR | ||||||||||
| Significant fibrosis | ||||||||||||||
| All | 12 | 0.71 (0.64–0.77) | 0.73 (0.67–0.78) | 6.52 (4.53–9.39) | 2.61 (2.12–3.21) | 0.4 (0.32 to 0.49) | 0.78 (0.74–0.81) | |||||||
| Exclude improper spectrumΔ | 7 | 0.73 (0.63–0.81) | 0.79 (0.73–0.84) | 10.31 (6.52–16.30) | 3.52 (2.75–4.51) | 0.341 (0.25–0.47) | 0.83 (0.80–0.86) | |||||||
| Blindness* | 7 | 0.68 (0.61–0.74) | 0.68 (0.61–0.73) | 4.39 (3.3–5.82) | 2.09 (1.78–2.45) | 0.48 (0.40–0.57) | 0.73 (0.69–0.77) | |||||||
| Non blindness | 5 | 0.75 (0.62–0.84) | 0.78 (0.69–0.85) | 10.74 (5.60–20.59) | 3.45 (2.39–4.98) | 0.32 (0.21–0.49) | 0.83 (0.80–0.86) | |||||||
Proper interval
|
8 | 0.69 (0.62–0.75) | 0.71 (0.64–0.78) | 5.39 (4.02–7.22) | 2.38 (1.95–2.90) | 0.44 (0.37–0.52) | 0.76 (0.72–0.79) | |||||||
| Improper interval | 4 | 0.76 (0.64–0.84) | 0.75 (0.63–0.84) | 9.45 (4.02–22.2) | 3.04 (1.92–4.83) | 0.32 (0.20–0.51) | 0.82 (0.78–0.85) | |||||||
| Exclude repeat patient# | 11 | 0.69 (0.63–0.75) | 0.73 (0.66–0.79) | 6.09 (4.23–8.76) | 2.56 (2.06–3.19) | 0.42 (0.35–0.51) | 0.77 (0.73–0.81) | |||||||
| Severe fibrosis | ||||||||||||||
| All | 6 | 0.76 (0.64–0.85) | 0.74 (0.70–0.79) | 9.14 (5.35–15.60) | 2.96 (2.48–3.53) | 0.32 (0.21–0.49) | 0.79 (0.75–82) | |||||||
| Exclude improper spectrumΔ | 5 | 0.79 (0.67–0.87) | 0.72 (0.68–0.75) | 9.17 (4.91–17.1) | 2.76 (2.28–3.33) | 0.3 (0.19–0.48) | 0.73 (0.69–0.77) | |||||||
| Blindness* | 5 | 0.76 (0.62–0.86) | 0.75 (0.70–0.79) | 9.54 (5.18–17.58) | 3.03 (2.50–3.68) | 0.32 (0.19–0.52) | 0.79 (0.76–0.83) | |||||||
| Cirrhosis | ||||||||||||||
| All | 10 | 0.83 (0.78–0.88) | 0.80 (0.73–0.86) | 20.64 (11.54–36.93) | 4.26 (3.04–5.96) | 0.21 (0.15–0.28) | 0.89 (0.85–0.91) | |||||||
| Exclude improper spectrumΔ | 6 | 0.85 (0.80–0.89) | 0.77 (0.7–0.83) | 19.10 (10.41–35.03) | 3.75 (2.72–5.16) | 0.2 (0.14–0.27) | 0.88 (0.85–0.91) | |||||||
| Blindness* | 5 | 0.80 (0.7–0.87) | 0.77 (0.72–0.82) | 13.25 (6.5–27.05) | 3.48 (2.59–4.69) | 0.26 (0.17–0.41) | 0.85 (0.81–0.88) | |||||||
| Non blindness | 5 | 0.85 (0.80–0.90) | 0.85 (0.72–0.92) | 32.53 (14.48–73.08) | 5.6 (3–10.57) | 0.17 (0.12–0.25) | 0.87 (0.84–0.90) | |||||||
Proper interval
|
8 | 0.83 (0.77–0.88) | 0.80 (0.72–0.86) | 20.04 (10.32–38.92) | 4.18 (2.9–6.04) | 0.21 (0.15–0.30) | 0.88 (0.85–0.91) | |||||||
| Exclude repeat patient# | 9 | 0.83 (0.77–0.88) | 0.82 (0.75–0.87) | 21.93 (11.75–40.95) | 4.52 (3.15–6.47) | 0.21 (0.15–0.29) | 0.89 (0.86–0.91) | |||||||
The disease spectrum of some studies [11], [17], [19]–[21], [24], [26]–[28] were not in good accordance with our study, thus they were excluded for sensitivity analysis.
*The studies in which the reference standard results were interpreted without knowledge of the results of the index tests, were grouped into “Blindness”.

The “proper interval” was defined as the time interval between the determination of the FIB-4 index and liver biopsy was no longer than 7 days.
As two studies [22], [32] were written by the same author, the study [32] with the smaller sample size was excluded for sensitivity analysis. 95% CI: 95% confidence interval. DOR: diagnostic odds ratio. PLR: positive likelihood ratio; NLR: negative likelihood ratio. AUHSROC: area under the hierarchical summary receiver operating characteristic curve.
Figure 3. The hierarchical summary receiver operating characteristic (HSROC) curve of FIB-4 index for predicting significant fibrosis.
The size of circles indicates the weight of the individual studies. The marked point on the curve represents the summary sensitivity and specificity. The area delimited by dashed line represents 95% confidence interval of the summary estimate. The area delimited by the dots represents the 95% prediction region, within which there is a 95%confidence that the true sensitivity and specificity of a future study should lie.
Figure 4. The forest plot of the FIB-4 index for predicting significant fibrosis.
Table 3. Subgroup analysis based on different FIB-4 index cutoff values.
| Thresholds | Number ofstudies | Summary estimates(95% CI) | Likelihood ratio (95%CI) | AUHSROC(95% CI) | |||
| Sensitivity | Specificity | DOR | PLR | NLR | |||
| Significant fibrosis | |||||||
| 0.8–1.085 | 5 | 0.73 (0.68–0.77) | 0.62 (0.56–0.67) | 4 (3–6) | 1.9 (1.6–2.2) | 0.44 (0.36–0.54) | 0.73 (0.69–0.77) |
| 1.45–1.62 | 6 | 0.65 (0.56–0.73) | 0.77 (0.7–0.83) | 6.24 (4.06–9.61) | 2.83 (2.16–3.71) | 0.45 (0.36–0.57) | 0.78 (0.74–0.81) |
| 3.25 | 3 | 0.18 (0.13–0.24) | 0.98 (0.95–0.99) | 7.53 (3.06–18.54) | 6.04 (2.61–13.96) | 0.85 (0.76–0.95) | 0.61 (0.57–0.65) |
| Severe fibrosis | |||||||
| 1.45–1.65 | 4 | 0.68 (0.6–0.75) | 0.75 (0.69–0.81) | 6.44 (4.44–9.35) | 2.75 (2.21–3.43) | 0.42 (0.34–0.53) | 0.77 (0.73–0.80) |
| Cirrhosis | |||||||
| 1.6–2.29 | 7 | 0.82 (0.75–0.88) | 0.77 (0.71–0.82) | 15.55 (8.69–27.80) | 3.59 (2.73–4.74) | 0.23 (0.16–0.33) | 0.87 (0.84–0.90) |
| 2.9–3.6 | 3 | 0.42 (0.36–0.48) | 0.96 (0.95–0.97) | 46.28 (18.3–117.04) | 13.38 (9.24–19.37) | 0.3 (0.06–0.45) | 0.96 (0.92–1.00) |
95% CI: 95% confidence interval. DOR: diagnostic odds ratio. PLR: positive likelihood ratio; NLR: negative likelihood ratio. AUHSROC: area under the hierarchical summary receiver operating characteristic curve.
Diagnostic accuracy of the FIB-4 index for predicting severe fibrosis
Six studies of 1,473 patients (male: 68.9%; average age: 37.3 years, average prevalence: 33.5%) were involved in the meta-analysis for testing the diagnostic accuracy of the FIB-4 index for predicting severe fibrosis (i.e., METAVIR F3–F4 vs. F0–F2). The cutoff values ranged from 1 to 3.25. The area under the HSROC was 0.79 (95% CI = 0.75-82; Figure 5). The summary sensitivity and specificity were 0.76 (95% CI = 0.64–0.85) and 0.74 (95% CI = 0.70–0.79), respectively (Figure 6). The heterogeneity was significant (I2 = 93%), and the meta-regression showed that disease spectrum (P = 0.01) and prevalence (P = 0.01) lead to the heterogeneity. There was only one study with improper disease spectrum [26]. At the same time, disease prevalence of this study (prevalence = 0.13) was also much lower than that of the others. After excluding this study, the area under HSROC dropped from 0.79 to 0.73. Subgroup analysis (Table 3) showed that in four studies with cutoff values ranging from 1.45 to 1.65, the area under the summary receiver-operating characteristic curve (AUROC) was 0.77 (95% CI = 0.73–0.80). The corresponding PLR (2.75, 95% CI = 2.21–3.43) and NLR (0.42, 95% CI = 0.34–0.53) indicated that using the FIB-4 index with a cutoff value between 1.45 and 1.65 has a suboptimal accuracy in identifying and excluding severe fibrosis.
Figure 5. The hierarchical summary receiver operating characteristic (HSROC) curve of FIB-4 index for predicting severe fibrosis.
The size of circles indicates the weight of the individual studies. The marked point on the curve represents the summary sensitivity and specificity. The area delimited by dashed line represents 95% confidence interval of the summary estimate. The area delimited by the dots represents the 95% prediction region, within which there is a 95% confidence that the true sensitivity and specificity of a future study should lie.
Figure 6. The forest plot of the FIB-4 index for predicting severe fibrosis.
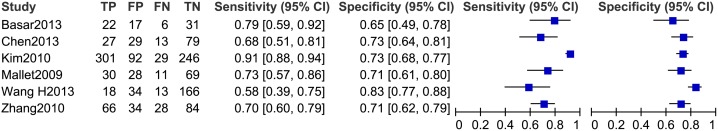
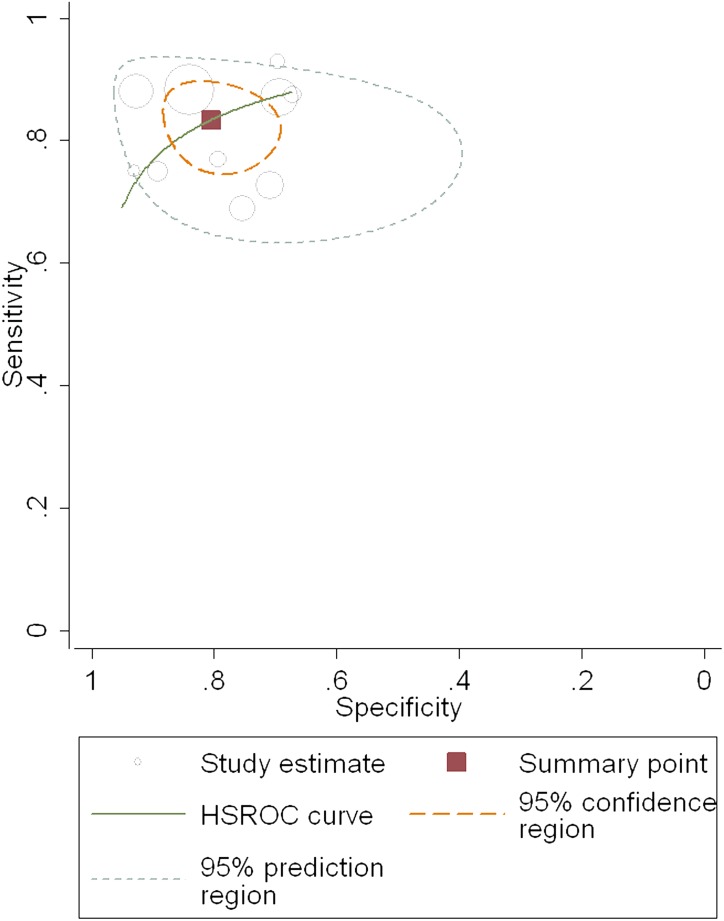
Diagnostic accuracy of the FIB-4 index for predicting cirrhosis
Ten studies of 2,105 patients (male: 69.9%, average age: 37.9 years, average prevalence of cirrhosis 20.8%) were involved in the meta-analysis for testing the diagnostic accuracy of the FIB-4 index for predicting cirrhosis (i.e., METAVIR F4 vs. F0–F3). The cutoff values ranged from 1.05 to 3.6, and the area under the HSROC was 0.89 (95% CI = 0.85–0.91; Figure 7), so the diagnostic performance was nearly excellent [42], [43]. The summary sensitivity and specificity were 0.83 (95% CI = 0.78–0.88) and 0.80 (95% CI = 0.73–0.86), respectively (Figure 8). The heterogeneity was significant (I2 = 67%), and the meta-regression showed that the potential factors described above didn’t lead to the heterogeneity (P>0.05). The most appropriate cutoff value for detecting significant fibrosis was between 2.9 and 3.6. At this range, the AUROC was 0.96 (95% CI = 0.92–1.00), so it was classified as excellent. The PLR (13.38, 95% CI = 9.24–19.37) for the FIB-4 index was high enough to be used to identify cirrhosis, although the NLR (0.3, 95% CI = 0.06–0.45) was not low enough to exclude cirrhosis.
Figure 7. The hierarchical summary receiver operating characteristic (HSROC) curve of FIB-4 index for predicting cirrhosis.
The size of circles indicates the weight of the individual studies. The marked point on the curve represents the summary sensitivity and specificity. The area delimited by dashed line represents 95% confidence interval of the summary estimate. The area delimited by the dots represents the 95% prediction region, within which there is a 95% confidence that the true sensitivity and specificity of a future study should lie.
Figure 8. The forest plot of the FIB-4 index for predicting cirrhosis.
Publication bias
A publication bias was not detected when tested using Egger’s test or the trim and fill method (Table 4). For Egger’s test, the publication bias 95% CI of every group included zero and the P-value was >0.05, so there was no statistical difference between publication bias and zero. This means that no publication bias was present. For the trim and fill method, the summary diagnostic odds ratio (SDOR) was always >1 both before and after trim and fill, meaning that trimming and filling studies didn’t influence the outcome of the meta-analysis (SDOR always >1). Taken together this means that publication bias was nonexistent in our meta-analysis.
Table 4. Analysis of publication bias for studies.
| Staging | P value of bias | 95%CI of bias | SDOR after trim and fill |
| Significant fibrosis | 0.18 | (−1.34∼6.26) | 6.394 (4.44∼9.21) |
| Severe fibrosis | 0.08 | (−12.56∼1.07) | 8.38 (4.27∼16.43) |
| Cirrhosis | 0.75 | (−3.93∼2.94) | 19.67 (10.53∼36.74) |
95% CI: 95% confidence interval. SDOR: summary diagnostic odds ratio.
Discussion
Accurate diagnosis of liver fibrosis is clinically advantageous. Liver biopsy is the gold standard for diagnosing fibrosis; however, its clinical application is hampered by various limitations. Despite these limitations, an ideal alternative to liver biopsies has not been found [67], [68]. In this meta-analysis we assessed the diagnostic accuracy of the FIB-4 index as a non-invasive alternative to liver biopsy.
The FIB-4 index is a simple and inexpensive noninvasive marker of liver fibrosis. Recently, the diagnostic value of the FIB-4 index in predicting the extent of fibrosis has been substantiated, and is even considered by some to be the best noninvasive index [11], [13]; however, others have highlighted its weaknesses [10], [26]. The current study comprehensively analyzed the predictive power of the FIB-4 index using a meta-analysis of previously published studies. The area under the HSROC for the FIB-4 index was 0.78, and 0.79 and 0.89 for predicting significant and severe fibrosis, and cirrhosis, respectively. Thus, the summary diagnostic performance of FIB-4 for significant and severe fibrosis was nearly good, and for cirrhosis was nearly excellent.
As the summary estimates of all cutoff values was deemed difficult to interpret and use in clinical practice, a subgroup analysis based on different cutoff values was performed. The recommended cutoff value for predicting significant fibrosis was between 1.45 and 1.62 based on the highest AUHSROC, but it still had suboptimal accuracy in excluding significant fibrosis. Fortunately, we found that the FIB-4 index with a cutoff value of 3.25 was suitable for identifying significant fibrosis. For severe fibrosis, the recommended cutoff value was between 1.45 and 1.65, and it has a suboptimal accuracy in identifying and excluding severe fibrosis. For cirrhosis, the recommended cutoff value was between 2.9 and 3.6, and the diagnostic performance was excellent (AUROC = 0.96). Thus, patient’s with a FIB-4 index above 3.6 can almost be diagnosed with cirrhosis, with a PLR = 13.38.
In terms of other noninvasive indexes, the APRI has the advantage of including only two inexpensive laboratory tests, which are performed routinely, and the FibroTest/Fibrosure is one of the most investigated and most frequently used tools for assessing liver fibrosis. The diagnostic performance of these two non-invasive indexes has been evaluated by meta-analysis [67], [69]. If we compare our meta-analysis of the FIB-4 index with these studies we can see that for significant fibrosis, AUROC of the APRI and FibroTest/Fibrosure was 0.79 (SE = 0.0243) and 0.84 (95% CI = 0.78–0.88), respectively. Thus, the diagnostic accuracy of the FIB-4 was similar to that of the APRI, and worse than the FibroTest/Fibrosure. For cirrhosis, the AUROC of the APRI and FibroTest/Fibrosure was 0.75 (SE = 0.0237) and 0.87 (95% CI = 0.85–0.90), respectively. Thus, based on our meta-analysis, the FIB-4 index was superior to that of the APRI, and similar to that of the FibroTest/Fibrosure for diagnosing cirrhosis. Additionally, another meta-analysis revealed that the AUROC of the FIB-4 index for significant fibrosis and cirrhosis with HCV infection was 0.74 and 0.87, respectively [70]. Thus, the diagnostic value of the FIB-4 index for predicting HBV-related fibrosis was also slightly better than that for HCV, although it was originally applied to HCV and HIV co-infection [14], [15]. Unfortunately, meta-analyses of other non-invasive tests for predicting HBV related fibrosis was not found, so comparison with the FIB-4 index was not possible.
There are two strengths to the current meta-analysis. First, although the diagnostic performance of the FIB-4 index for HBV-related fibrosis has previously been assessed by several studies [10], [11], [13], [16]–[32], our evaluation combined the data from previously published work in a meta-analysis, thereby strengthening its accuracy. Second, we searched the CNKI and CBMdisc databases that provided authoritative and comprehensive data from Chinese populations. This is important because the prevalence of HBV infection is much higher than that of HCV infection in Chinese populations [71]. Additionally, we found that of the 15 eligible studies written in English for this meta-analysis [10], [11], [13], [16], [18]–[20], [23]–[30], nine were written by Chinese groups [10], [20], [23], [24], [26]–[30]. Thus, authors not searching Chinese databases may have overlooked some valuable studies.
There are three limitations to the current meta-analysis. First, there were 20 eligible studies included in the meta-analysis, but this number was too small for further subgroup analysis. This limitation was compounded by the fact that there were few studies with a large sample size and multiple centers. The second limitation was the significant heterogeneity of included studies. A considerable variation between the results of diagnostic studies is a common occurrence, possibly to a greater extent than is seen for therapeutic interventions [72]. One of the potential sources of heterogeneity and a direct consequence of the fact that the importance of rigorous design has been less well appreciated for diagnostic studies than for therapeutic interventions, is poor adherence to methodological constraints [69], [73]. This is noticeable in many studies that we included, and can be considered as a general problem in many studies dealing with the diagnostic accuracy of liver fibrosis markers, as already noted by others [73]. In our study, although disease spectrum, blindness and prevalence were found to be the factors causing heterogeneity, and further sensitivity analysis and/or subgroup analysis were performed in our study, more detailed subgroup analysis, such as grouping by both proper disease spectrum and blindness, is needed. Unfortunately, the eligible studies were too few to perform this. Finally, we only included published manuscripts, so bias in the selection of search channels may have influenced our results.
Our meta-analysis has several implications for future research. For example, we believe that more studies on the diagnostic accuracy for liver fibrosis are needed in patient populations with CHB. In the future, authors of studies exploring the performance of the FIB-4 index in CHB patients should be encouraged to insist on a rigorous design and methodology. In this regard, QUADAS-2 [36] describes what is required for a rigorous study design and methodology, and is a good tool for guiding diagnostic study design. As common flaws in design and methodology found in our eligible studies, we emphasize two points: first, a study should ideally enroll all consecutive, or a random sample of, eligible patients with suspected disease – otherwise there is potential for bias. Second, selecting the test threshold to optimize sensitivity and/or specificity may lead to overoptimistic estimates of test performance, which is likely to be poorer in an independent sample of patients in whom the same threshold is used [74]. As a result, if a threshold was used, it should be pre-specified.
Implications for practice deriving from our results suggest that the FIB-4 index is of excellent utility for detecting cirrhosis in patients with CHB, and has moderate accuracy in detecting significant fibrosis. On the other hand, it has suboptimal performance in the exclusion of significant and severe fibrosis, and cirrhosis. Thus, it is necessary to further improve the test or combine it with other noninvasive modalities in order to improve its accuracy.
Supporting Information
Search strategy of Ovid database. This literature search was performed in November 2013.
(DOC)
Search strategy of Pubmed database. This literature search was performed in November 2013.
(CSV)
PRISMA 2009 checklist.
(DOC)
Acknowledgments
The authors thank Guocai Lv, PhD and Renyong Guo, PhD (Department of Laboratory Medicine, the First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou 310003, China) for critical comments on research design and statistics. We thank Elixigen Corporation (Huntington Beach, California, USA) for helping in proofreading and editing the English of final manuscript.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors have no support or funding to report.
References
- 1. Liaw YF, Sung JJ, Chow WC, Farrell G, Lee CZ, et al. (2004) Lamivudine for patients with chronic hepatitis B and advanced liver disease. N Engl J Med 351: 1521–1531. [DOI] [PubMed] [Google Scholar]
- 2. Lok AS, McMahon BJ (2007) Chronic hepatitis B. Hepatology. 45: 507–539. [DOI] [PubMed] [Google Scholar]
- 3. EASL clinical practice guidelines: Management of chronic hepatitis B virus infection. J Hepatol 57: 167–185. [DOI] [PubMed] [Google Scholar]
- 4. de Franchis R (2008) Non-invasive (and minimally invasive) diagnosis of oesophageal varices. J Hepatol 49: 520–527. [DOI] [PubMed] [Google Scholar]
- 5. Bravo AA, Sheth SG, Chopra S (2001) Liver biopsy. N Engl J Med 344: 495–500. [DOI] [PubMed] [Google Scholar]
- 6. Bedossa P, Dargere D, Paradis V (2003) Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology. 38: 1449–1457. [DOI] [PubMed] [Google Scholar]
- 7. Friedman LS (2004) Controversies in liver biopsy: who, where, when, how, why? Curr Gastroenterol Rep 6: 30–36. [DOI] [PubMed] [Google Scholar]
- 8. Bedossa P, Poynard T (1996) An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology 24: 289–293. [DOI] [PubMed] [Google Scholar]
- 9. Ma J, Jiang Y, Gong G (2013) Evaluation of seven noninvasive models in staging liver fibrosis in patients with chronic hepatitis B virus infection. Eur J Gastroenterol Hepatol 25: 428–434. [DOI] [PubMed] [Google Scholar]
- 10. Chen B, Ye B, Zhang J, Ying L, Chen Y (2013) RDW to Platelet Ratio: A Novel Noninvasive Index for Predicting Hepatic Fibrosis and Cirrhosis in Chronic Hepatitis B. PLOS ONE. 8: e68780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Erdogan S, Dogan HO, Sezer S, Uysal S, Ozhamam E, et al. (2013) The diagnostic value of non-invasive tests for the evaluation of liver fi brosis in chronic hepatitis B patients. Scandinavian Journal of Clinical & Laboratory Investigation 73: 300–308. [DOI] [PubMed] [Google Scholar]
- 12. Lin ZH, Xin YN, Dong QJ, Wang Q, Jiang XJ, et al. (2011) Performance of the aspartate aminotransferase-to-platelet ratio index for the staging of hepatitis C-related fibrosis: an updated meta-analysis. Hepatology 53: 726–736. [DOI] [PubMed] [Google Scholar]
- 13. Kim BK, Kim DY, Park JY, Ahn SH, Chon CY, et al. (2010) Validation of FIB-4 and comparison with other simple noninvasive indices for predicting liver fibrosis and cirrhosis in hepatitis B virus-infected patients. Liver International 30: 546–553. [DOI] [PubMed] [Google Scholar]
- 14. Sterling RK, Lissen E, Clumeck N, Sola R, Correa MC, et al. (2006) Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology 43: 1317–1325. [DOI] [PubMed] [Google Scholar]
- 15. Torriani FJ, Rodriguez-Torres M, Rockstroh JK, Lissen E, Gonzalez-Garcia J, et al. (2004) Peginterferon Alfa-2a plus ribavirin for chronic hepatitis C virus infection in HIV-infected patients. N Engl J Med 351: 438–450. [DOI] [PubMed] [Google Scholar]
- 16. Mallet V, Dhalluin-Venier V, Roussin C, Bourliere M, Pettinelli ME, et al. (2009) The accuracy of the FIB-4 index for the diagnosis of mild fibrosis in chronic hepatitis B. Alimentary Pharmacology & Therapeutics. 29: 409–415. [DOI] [PubMed] [Google Scholar]
- 17.Ji D, Shao Q, Han P, Zhang J, Niu X, et al.. (2011) Analysis of the efficiency of Fibroscan combined with serologic markers for diagnosing liver fibrosis. Med J Clin PLA 36.
- 18. Ucar F, Sezer S, Ginis Z, Ozturk G, Albayrak A, et al. (2013) APRI, the FIB-4 score, and Forn's index have noninvasive diagnostic value for liver fibrosis in patients with chronic hepatitis B. European Journal of Gastroenterology & Hepatology. 25: 1076–1081. [DOI] [PubMed] [Google Scholar]
- 19. Bonnard P, Sombie R, Lescure F-X, Bougouma A, Guiard-Schmid JB, et al. (2010) Comparison of Elastography, Serum Marker Scores, and Histology for the Assessment of Liver Fibrosis in Hepatitis B Virus (HBV)-Infected Patients in Burkina Faso. American Journal of Tropical Medicine & Hygiene 82: 454–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wang H, Xue L, Yan R, Zhou Y, Wang MS, et al. (2013) Comparison of FIB-4 and APRI in Chinese HBV-infected patients with persistently normal ALT and mildly elevated ALT. Journal of Viral Hepatitis 20: e3–e10. [DOI] [PubMed] [Google Scholar]
- 21. Gong H, Hu Y, Ye X, Lin H (2013) Diagnostic efficiency of real-time tissue elastography in evaluating liver fibrosis. ACTA UNIVERSITATIS MEDICINALIS NANJING (Natural Science) 33: 131–134. [Google Scholar]
- 22. Zhang Y, Zeng J, Fan Q, Zheng J, Li Q (2012) Four noninvasive score systems for diagnosis of liver fibrosis in patients with chronic hepatitis B. Chin J Clin Infect Dis. 5: 338–341. [Google Scholar]
- 23. Liu XD, Wu JL, Liang J, Zhang T, Sheng QS (2012) Globulin-platelet model predicts minimal fibrosis and cirrhosis in chronic hepatitis B virus infected patients. World J Gastroenterol 18: 2784–2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seto W-K, Lee C-F, Lai C-L, Ip PPC, Fong DY-T, et al.. (2011) A New Model Using Routinely Available Clinical Parameters to Predict Significant Liver Fibrosis in Chronic Hepatitis B. PLoS One 6: Article No. e23077. [DOI] [PMC free article] [PubMed]
- 25. Başar Ö, Yımaz B, Ekiz F, Giniş Z, Altınbaş A, et al. (2013) Non-invasive tests in prediction of liver fibrosis in chronic hepatitis B and comparison with post-antiviral treatment results. Clinics and Research in Hepatology and Gastroenterology 37: 152–158. [DOI] [PubMed] [Google Scholar]
- 26. Wang Y, Xu M-Y, Zheng R-D, Xian J-C, Xu H-T, et al. (2013) Prediction of significant fibrosis and cirrhosis in hepatitis B e-antigen negative patients with chronic hepatitis B using routine parameters. Hepatology Research 43: 441–451. [DOI] [PubMed] [Google Scholar]
- 27. Zhu X, Wang L-C, Chen E-Q, Chen X-B, Chen L-Y, et al. (2011) Prospective Evaluation of FibroScan for the Diagnosis of Hepatic Fibrosis Compared with Liver Biopsy/AST Platelet Ratio Index and FIB-4 in Patients with Chronic HBV Infection. Digestive Diseases & Sciences 56: 2742–2749. [DOI] [PubMed] [Google Scholar]
- 28. Xun Y-h, Zang G-q, Guo J-c, Yu X-l, Liu H, et al. (2013) Serum hepatitis B surface antigen quantification as a useful assessment for significant fibrosis in hepatitis B e antigen-positive hepatitis B virus carriers. Journal of Gastroenterology & Hepatology 28: 1746–1755. [DOI] [PubMed] [Google Scholar]
- 29. Zhu CL, Li WT, Li Y, Gao RT (2012) Serum levels of tissue inhibitor of metalloproteinase-1 are correlated with liver fibrosis in patients with chronic hepatitis B. Journal of Digestive Diseases. 13: 558–563. [DOI] [PubMed] [Google Scholar]
- 30. Wu SD, Wang JY, Li L (2010) Staging of liver fibrosis in chronic hepatitis B patients with a composite predictive model: a comparative study. World J Gastroenterol 16: 501–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zhang YF, Shi H, Chen LB, Xu QH (2010) Value of FIB-4 for the diagnosis of liver fibrosis in chronic hepatitis B. Zhonghua Shi Yan He Lin Chuang Bing Du Xue Za Zhi. 24: 215–217. [PubMed] [Google Scholar]
- 32. Zhang Y, Hong D, Bian W, Shen Y, Yan N (2009) Value of FIB-4 for the diagnosis of liver fibrosis in patients with chronic hepatitis B. Ch in J Gastroentero lH epato. l: 213–214. [Google Scholar]
- 33. Batts KP, Ludwig J (1995) Chronic hepatitis. An update on terminology and reporting. Am J Surg Pathol 19: 1409–1417. [DOI] [PubMed] [Google Scholar]
- 34. Scheuer PJ (1991) Classification of chronic viral hepatitis: a need for reassessment. J Hepatol 13: 372–374. [DOI] [PubMed] [Google Scholar]
- 35. Ishak K, Baptista A, Bianchi L, Callea F, De Groote J, et al. (1995) Histological grading and staging of chronic hepatitis. J Hepatol 22: 696–699. [DOI] [PubMed] [Google Scholar]
- 36. Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, et al. (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155: 529–536. [DOI] [PubMed] [Google Scholar]
- 37. Lu XL, Xiao ZH, Yang MY, Zhu YM (2013) Diagnostic value of serum procalcitonin in patients with chronic renal insufficiency: a systematic review and meta-analysis. Nephrol Dial Transplant 28: 122–129. [DOI] [PubMed] [Google Scholar]
- 38.Chu H, Cole SR (2006) Bivariate meta-analysis of sensitivity and specificity with sparse data: a generalized linear mixed model approach. J Clin Epidemiol 59: 1331–1332; author reply 1332–1333. [DOI] [PubMed]
- 39. Wang F, Gatsonis CA (2008) Hierarchical models for ROC curve summary measures: design and analysis of multi-reader, multi-modality studies of medical tests. Stat Med 27: 243–256. [DOI] [PubMed] [Google Scholar]
- 40. Leeflang MM (2014) Systematic reviews and meta-analyses of diagnostic test accuracy. Clin Microbiol Infect 20: 105–113. [DOI] [PubMed] [Google Scholar]
- 41. Leeflang MM, Deeks JJ, Gatsonis C, Bossuyt PM (2008) Systematic reviews of diagnostic test accuracy. Ann Intern Med 149: 889–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zweig MH, Campbell G (1993) Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clinical Chemistry 39: 561–577. [PubMed] [Google Scholar]
- 43. Altman DG, Bland JM (1994) Diagnostic tests 3: receiver operating characteristic plots. BMJ 309: 188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lijmer JG, Bossuyt PM, Heisterkamp SH (2002) Exploring sources of heterogeneity in systematic reviews of diagnostic tests. Stat Med 21: 1525–1537. [DOI] [PubMed] [Google Scholar]
- 45. Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Duval S, Tweedie R (2000) Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56: 455–463. [DOI] [PubMed] [Google Scholar]
- 47. Xu M-Y, Qu Y, Jia X-F, Wang M-L, Liu H, et al. (2013) Serum proteomic MRM identify peptide ions of transferrin as new fibrosis markers in chronic hepatitis B. Biomedicine & Pharmacotherapy. 67: 561–567. [DOI] [PubMed] [Google Scholar]
- 48. Gumusay O, Ozenirler S, Atak A, Sonmez C, Ozkan S, et al. (2013) Diagnostic potential of serum direct markers and non-invasive fibrosis models in patients with chronic hepatitis B. Hepatology Research. 43: 228–237. [DOI] [PubMed] [Google Scholar]
- 49. Wong GLH, Wong VWS, Choi PCL, Chan AWH, Chan HLY (2010) Development of a non-invasive algorithm with transient elastography (Fibroscan) and serum test formula for advanced liver fibrosis in chronic hepatitis B. Alimentary Pharmacology & Therapeutics. 31: 1095–1103. [DOI] [PubMed] [Google Scholar]
- 50.Ding D, Meng Z, Ke C, Li D, Chen Y (2013) The Correlation of FIB-4 Index with Child-Pugh Classification in Patients with HBV-related Cirrhosis. J HBUM: 245–247.
- 51.Zhou J (2013) Application of FibroScan combined with other serologic markers on the diagnosis of liver fibrosis. Int J Lab Med: 409–411.
- 52. Li X (2012) Developments in hepatic fibrosis diagnosis with the combination of serological indexes and Fibroscan. J Clin Hepatol 15: 472–474. [Google Scholar]
- 53. Stibbe KJ, Verveer C, Francke J, Hansen BE, Zondervan PE, et al. (2011) Comparison of non-invasive assessment to diagnose liver fibrosis in chronic hepatitis B and C patients. Scand J Gastroenterol 46: 962–972. [DOI] [PubMed] [Google Scholar]
- 54. Sebastiani G, Castera L, Halfon P, Pol S, Mangia A, et al. (2011) The impact of liver disease aetiology and the stages of hepatic fibrosis on the performance of non-invasive fibrosis biomarkers: an international study of 2411 cases. Aliment Pharmacol Ther 34: 1202–1216. [DOI] [PubMed] [Google Scholar]
- 55. Pissaia A Jr, Borderie D, Bernard D, Scatton O, Calmus Y, et al. (2009) APRI and FIB-4 Scores Are Useful After Liver Transplantation Independently of Etiology. Transplantation Proceedings 41: 679–681. [DOI] [PubMed] [Google Scholar]
- 56. Nalpas B, Mallet V, Vallet-Pichard A, Fontaine H, Pol S (2009) 374 THE FIB-4 INDEX IS ACCURATE TO ASSESS LIVER FIBROSIS BEFORE AND DURING TREATMENT IN CHRONIC HEPATITIS B. Journal of Hepatology. 50 Supplement 1 S142–S143. [Google Scholar]
- 57. Molto J, Llibre JM, Ribera E, Minguez C, del Rio JS, et al. (2009) Saquinavir exposure in HIV-infected patients with chronic viral hepatitis. Journal of Antimicrobial Chemotherapy 63: 992–997. [DOI] [PubMed] [Google Scholar]
- 58. Lee MH, Cheong JY, Um SH, Seo YS, Kim DJ, et al. (2010) Comparison of Surrogate Serum Markers and Transient Elastography (Fibroscan) for Assessing Cirrhosis in Patients with Chronic Viral Hepatitis. Digestive Diseases & Sciences 55: 3552–3560. [DOI] [PubMed] [Google Scholar]
- 59. Lee JH, Yoon JH, Lee CH, Myung SJ, Keam B, et al. (2009) Complete blood count reflects the degree of oesophageal varices and liver fibrosis in virus-related chronic liver disease patients. Journal of Viral Hepatitis 16: 444–452. [DOI] [PubMed] [Google Scholar]
- 60. Kim BK, Han KH, Park JY, Ahn SH, Chon CY, et al. (2010) External Validation of P2/MS and Comparison with Other Simple Non-invasive Indices for Predicting Liver Fibrosis in HBV-Infected Patients. Digestive Diseases & Sciences 55: 2636–2643. [DOI] [PubMed] [Google Scholar]
- 61. Jain MK, Seremba E, Bhore R, Dao D, Joshi R, et al. (2012) Change in fibrosis score as a predictor of mortality among HIV-infected patients with viral hepatitis. AIDS Patient Care STDS 26: 73–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. de Ledinghen V, Vergniol J, Barthe C, Foucher J, Chermak F, et al. (2013) Non-invasive tests for fibrosis and liver stiffness predict 5-year survival of patients chronically infected with hepatitis B virus. Alimentary Pharmacology & Therapeutics 37: 979–988. [DOI] [PubMed] [Google Scholar]
- 63. Cheong JY, Um SH, Seo YS, Kim DJ, Hwang SG, et al. (2011) Non-invasive index for predicting significant liver fibrosis: comparison of diagnostic performances in patients with chronic hepatitis B and C. Dig Dis Sci. 56: 555–563. [DOI] [PubMed] [Google Scholar]
- 64. Beckebaum S, Iacob S, Klein CG, Dechene A, Varghese J, et al. (2010) Assessment of Allograft Fibrosis by Transient Elastography and Noninvasive Biomarker Scoring Systems in Liver Transplant Patients. Transplantation 89: 983–993. [DOI] [PubMed] [Google Scholar]
- 65. Huang YC, Huang CF, Chang KC, Hung SF, Wang JH, et al. (2011) Community-based screening for hepatocellular carcinoma in elderly residents in a hepatitis B- and C-endemic area. J Gastroenterol Hepatol 26: 129–134. [DOI] [PubMed] [Google Scholar]
- 66. Chon YE, Jung ES, Park JY, Kim do Y, Ahn SH, et al. (2012) The accuracy of noninvasive methods in predicting the development of hepatocellular carcinoma and hepatic decompensation in patients with chronic hepatitis B. J Clin Gastroenterol. 46: 518–525. [DOI] [PubMed] [Google Scholar]
- 67. Jin W, Lin Z, Xin Y, Jiang X, Dong Q, et al. (2012) Diagnostic accuracy of the aspartate aminotransferase-to-platelet ratio index for the prediction of hepatitis B-related fibrosis: a leading meta-analysis. BMC Gastroenterol 12: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Castera L, Vergniol J, Foucher J, Le Bail B, Chanteloup E, et al. (2005) Prospective comparison of transient elastography, Fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology. 128: 343–350. [DOI] [PubMed] [Google Scholar]
- 69. Salkic NN, Jovanovic P, Hauser G, Brcic M (2014) FibroTest/Fibrosure for Significant Liver Fibrosis and Cirrhosis in Chronic Hepatitis B: A Meta-Analysis. Am J Gastroenterol 109: 796–809. [DOI] [PubMed] [Google Scholar]
- 70. Chou R, Wasson N (2013) Blood tests to diagnose fibrosis or cirrhosis in patients with chronic hepatitis C virus infection: a systematic review. Ann Intern Med 158: 807–820. [DOI] [PubMed] [Google Scholar]
- 71.Lan X (2012) Study on the area distribution of viral hepatitis in China. Chinese Journal of Health Laboratory Technology: 2467–2469.
- 72.Dinnes J, Deeks J, Kirby J, Roderick P (2005) A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy. Health Technol Assess 9: 1–113, iii. [DOI] [PubMed]
- 73. Regev A, Berho M, Jeffers LJ, Milikowski C, Molina EG, et al. (2002) Sampling error and intraobserver variation in liver biopsy in patients with chronic HCV infection. Am J Gastroenterol 97: 2614–2618. [DOI] [PubMed] [Google Scholar]
- 74. Leeflang MM, Moons KG, Reitsma JB, Zwinderman AH (2008) Bias in sensitivity and specificity caused by data-driven selection of optimal cutoff values: mechanisms, magnitude, and solutions. Clin Chem 54: 729–737. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategy of Ovid database. This literature search was performed in November 2013.
(DOC)
Search strategy of Pubmed database. This literature search was performed in November 2013.
(CSV)
PRISMA 2009 checklist.
(DOC)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.