To the Editor
Cardiac rehabilitation (CR) is a guideline-recommended therapy that reduces mortality after acute myocardial infarction (MI)(1). However, it is notoriously underutilized. Between 2000–2007, only 56% of eligible patients were referred to CR(1,2). In 2007, professional societies established CR referral from inpatient settings as a performance measure for acute MI(3,4). We examined whether CR referral has changed since 2007 using data from the National Cardiovascular Data Registry (NCDR®) Acute Coronary Treatment and Intervention Outcomes Network- ACTION Registry®-GWTG™ (ACTION Registry – GWTG) (www.ncdr.com/webncdr/ACTION/Default.aspx).
We evaluated patients admitted with primary diagnosis of ST- or non-ST segment MI from January 1, 2007-June 30, 2012 who were discharged home and had CR referral data (Supplemental Figure 1). CR referral was defined as “an official communication between the health care provider and the patient to recommend and carry out a referral order to an early outpatient CR program. This includes the provision of all necessary information to the patient that will allow the patient to enroll in an early outpatient CR program. This also includes a communication between the health care provider or health care system and the CR program that includes the patient’s referral information for the program. A hospital discharge summary or office note may potentially be formatted to include the necessary patient information.” Ineligibility was defined as documented patient-based barriers, patient-based criteria, or health care system barriers.
Covariates included age, sex, race/ethnicity, insurance type, body mass index (BMI), current/recent smoking, hypertension, dyslipidemia, diabetes, current dialysis, prior MI, prior percutaneous coronary intervention (PCI), prior coronary artery bypass graft surgery (CABG), prior stroke, peripheral arterial disease, length of stay, ST-elevation MI on admission electrocardiogram, in-hospital PCI, in-hospital CABG, in-hospital catheterization, left ventricular ejection fraction, in-hospital cardiogenic shock, in-hospital heart failure, in-hospital major bleeding, hospital region (West, Northeast, Midwest, or South), teaching hospital status, and hospital bed size.
Multivariate predictors of CR referral were estimated using a generalized estimating equations logistic regression model with backward selection (p<0.05). The model was implemented with empirical (sandwich) standard error estimates and was adjusted for clustering of observations from the same hospital. We also conducted multivariate analyses to estimate the odds of CR referral in each year (as compared with 2007). Missing data (less than 1.5% for all covariates) were imputed using standard techniques. All analyses were performed using SAS software (version 9.2, SAS Institute, Cary, North Carolina).
Between January 1, 2007 and June 30, 2012, 329,698 registry patients with acute MI were discharged from participating hospitals with CR referral data. Of these, 301,247 patients (91.4%) from 624 hospitals were reported eligible for CR (Supplemental Table 1); 28,451 (8.6%) were reported ineligible. From 2007–2012, CR referral increased by approximately 8% (from 72.9% to 80.7%; p<0.0001 for trend) (Figure 1).
Figure 1.
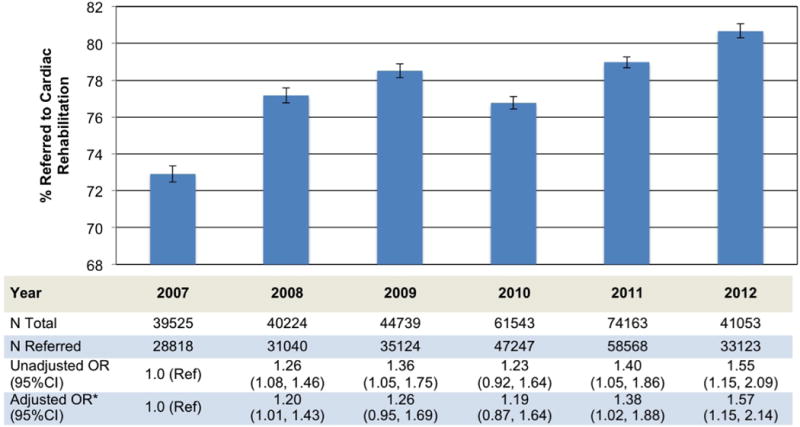
Cardiac rehabilitation referral after acute myocardial infarction, 2007 – 2012. Error bars represent 95% confidence intervals. P-value for trend <0.0001
*Adjusted for age, gender, race/ethnicity, body mass index, dyslipidemia, diabetes, dialysis status, prior percutaneous coronary intervention, ST elevation myocardial infarction at admission, in-hospital catheterization, in-hospital percutaneous coronary, in-hospital coronary artery bypass surgery, ejection fraction, length of stay, hospital region, hospital size, and teaching hospital status.
After multivariate adjustment, independent patient-level predictors of CR referral included age, male gender, white race, BMI, dyslipidemia, not having diabetes mellitus, not currently on dialysis, no prior PCI, ST-elevation MI at admission, in-hospital catheterization, in-hospital PCI, in-hospital CABG, mild left ventricular systolic dysfunction, and length of stay (Supplemental Table 2). Independent hospital-level predictors of CR referral included hospital in Midwest region, hospital bed-size, and non-academic hospital. After adjustment for multivariate predictors of CR referral, referral was significantly greater in 2011 (OR 1.38, 95%CI 1.02–1.88) and 2012 (OR 1.57, 95%CI 1.15–2.14), compared with 2007 (Figure 1).
CR referral improved across gender and racial/ethnic groups, but remained highest in males and whites (Supplemental Table 3). For hospitals in the lowest quartile of adherence to ACC/AHA 2008 performance measures (other than CR referral)(4) referral increased from 54% in 2007 to 64% in 2011, still significantly behind the 87% referral rate for highest quality quartiles hospitals in 2007 and 2011.
We note several limitations. First, ACTION Registry – GWTG is a voluntary registry and may not be representative of hospitals lacking the resources or desire to contribute. Our results may overestimate referral to CR and may not be fully generalizable. Data is drawn solely from inpatient medical records abstracted for the registry. Misclassification of CR eligibility may have occurred. The registry’s liberal definition of referral may overestimate meaningful referral(3). Finally, inter-hospital variation in what constitutes CR referral and eligibility may be present. In summary, referral to CR has significantly increased since its introduction as a quality measure in 2007, with 81% of eligible patients now being referred. Nonetheless, referral remains below achievable benchmarks. Compared to other acute MI discharge performance measures, CR referral has the lowest adherence, with measures like aspirin prescription, beta-blocker prescription, and smoking cessation counseling achieving adherence in ≥ 95% of patients (5). Improvement strategies may include identifying key personnel to direct the process of introducing CR in the inpatient setting and developing systems for automatic referral(1).
Supplementary Material
Acknowledgments
Funding Sources: Alexis Beatty was supported by the NIH National Center for Advancing Translational Sciences (KL2TR000143). The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. This research was supported by the American College of Cardiology Foundation’s NCDR®. The views expressed in this manuscript represent those of the authors and do not necessarily represent the official views of the NCDR® or its associated professional societies identified at www.ncdr.com.
ACTION Registry®–GWTG™ is an initiative of the American College of Cardiology Foundation and the American Heart Association, with partnering support from the Society of Chest Pain Centers, the American College of Emergency Physicians, and the Society of Hospital Medicine.
Selected Abbreviations and Acronyms
- ACTION
Acute Coronary Treatment and Intervention Outcomes Network
- BMI
Body Mass Index
- CABG
Coronary Artery Bypass Graft
- CR
Cardiac Rehabilitation
- GWTG
Get With The Guidelines
- MI
Myocardial Infarction
- NCDR®
National Cardiovascular Data Registry
- PCI
Percutaneous Coronary Intervention
Footnotes
Relationships with Industry: Dr. Whooley receives research support from Janssen Research and Development, LLC.
References
- 1.Balady GJ, Ades PA, Bittner VA, et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation. 2011;124:2951–60. doi: 10.1161/CIR.0b013e31823b21e2. [DOI] [PubMed] [Google Scholar]
- 2.Brown TM, Hernandez AF, Bittner V, et al. Predictors of cardiac rehabilitation referral in coronary artery disease patients: findings from the American Heart Association’s Get With The Guidelines Program. J Am Coll Cardiol. 2009;54:515–21. doi: 10.1016/j.jacc.2009.02.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomas RJ, King M, Lui K, et al. AACVPR/ACC/AHA 2007 performance measures on cardiac rehabilitation for referral to and delivery of cardiac rehabilitation/secondary prevention services. Circulation. 2007;116:1611–42. doi: 10.1161/CIRCULATIONAHA.107.185734. [DOI] [PubMed] [Google Scholar]
- 4.Krumholz HM, Anderson JL, Bachelder BL, et al. ACC/AHA 2008 performance measures for adults with ST-elevation and non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to develop performance measures for ST-elevation and non-ST-elevation myocardial infarction): developed in collaboration with the American Academy of Family Physicians and the American College of Emergency Physicians: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation, Society for Cardiovascular Angiography and Interventions, and Society of Hospital Medicine. Circulation. 2008;118:2596–648. doi: 10.1161/CIRCULATIONAHA.108.191099. [DOI] [PubMed] [Google Scholar]
- 5.Peterson ED, Roe MT, Rumsfeld JS, et al. A call to ACTION (acute coronary treatment and intervention outcomes network): a national effort to promote timely clinical feedback and support continuous quality improvement for acute myocardial infarction. Circulation Cardiovascular quality and outcomes. 2009;2:491–9. doi: 10.1161/CIRCOUTCOMES.108.847145. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


