Abstract
Dental implant restoration has been widely accepted as one of the treatment modalities to replace missing teeth and to restore human masticatory function. The use of root form endosseous implant has increased considerably and this restorative option has become more refined with the introduction of newer designs and concepts. Long term post placement studies have reported prosthetic complications, including screw loosening, screw fracture, framework and implant fracture. Abutment screw loosening is the second most common cause of failure of implant supported restoration, next to loss of osseointegration. This is more seen in single implant supported restoration. Management of screw loosening is challenging and this clinical report describes the management of an implant abutment screw loosening of upper anterior teeth with minimal damage to the existing restoration making it possible to be reused and a literature review on the various factors associated with abutment screw loosening.
Keywords: Abutment screw loosening, Settling effect, Preload, External and internal hex connection
Introduction
The replacement of missing teeth by implant supported prosthesis has become a popular option after the introduction of the concept of osseointegration with titanium fixtures [1, 2]. The use of root form endosseous implant has increased considerably and this restorative option has become more refined with the introduction of newer designs and concepts. Screw loosening, screw fracture, gold cylinder fracture, prosthetic component and implant fractures are the different prosthetic complications seen after loading the implant [3–5]. Among this screw loosening is the most common problem. This is seen more in single implant supported prosthesis with external connection and molars [6–9]. Reasons for screw loosening include inadequate preload, inappropriate implant position and occlusal scheme, variations in hex dimension and abutment counterparts, differences in fit and accuracy, tension on abutment, improper screw design and excessive occlusal forces [10–12]. Management of screw loosening is challenging and this clinical report describes the management of an implant abutment screw loosening of upper anterior teeth with minimal damage to the existing restoration making it possible to be reused.
Clinical Report
A 45 year old lady reported to the department clinic with chief complaint of mobility in relation to the recently cemented implant supported crown which restored her missing upper left central incisor (Fig. 1). The patient was rehabilitated using a zimmer implant (SWB) of internal hex connection of dimension 3.7 mm D and 12 mm L. The mobility was perceived by the patient from the next day after cementation of the prosthesis on the fixture. There was slight increase in the mobility which made her to report back after one week for examination. She did not complain of any pain or discomfort due to the mobility.
Fig. 1.

Initial photograph of the implant supported prosthesis
Medical history revealed nothing significant. She had an angle’s class 1 molar occlusion with normal overjet and overbite. On examination, there was mild inflammation of the gingiva around the cemented crown. This probably could be due to the irritation from the movement of the restoration. Intra oral periapical radiograph revealed spacing between the fixture and the abutment (Fig. 2). Hence it was diagnosed as an abutment screw loosening. Conservative management with immediate replacement was planned.
Fig. 2.
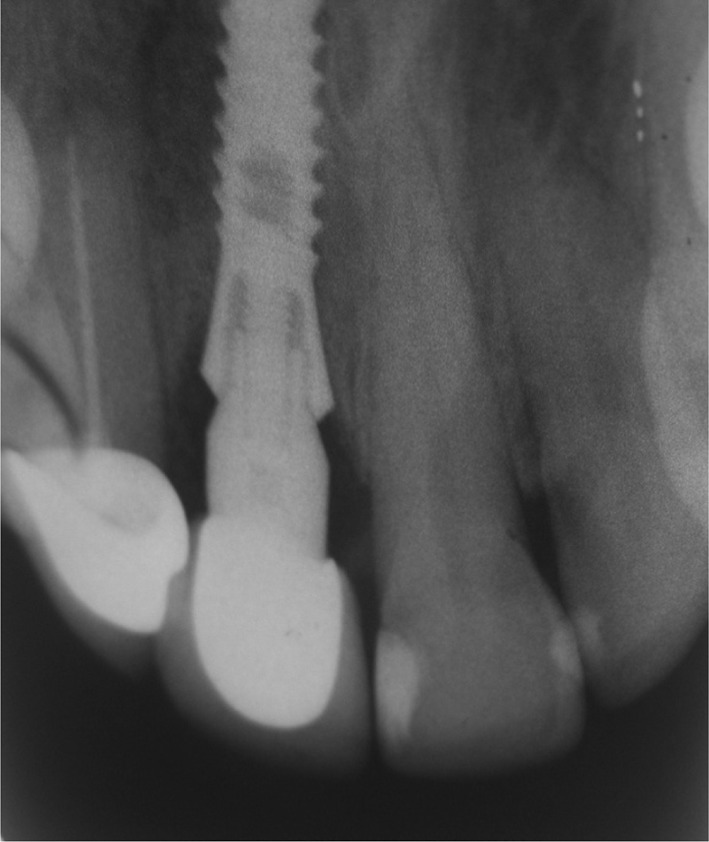
Periapical radiograph showing the inadequately tightened connecting screw
On manipulation the crown showed slight rotation along its long axis. The proximal contact of the crown with the adjacent tooth restricted its rotation and held it in position (Fig. 3). The veneering ceramic at the contact was removed from the crown using tapering fissure and round wheel diamond points in an airotor hand piece (Fig. 4a, b). This provided room for rotating the crown and thereby removing the cemented crown with the abutment and connecting screw from the fixture (Fig. 5, 6,and 7). The crown and the abutment with the connecting screw were then kept in the ceramic furnace at 250° C for 15 min. This resulted in disintegration of the luting cement (Fig. 8). This helped in separating the individual components (Fig. 9). The abutment with the connecting screw was tightened back into the fixture with a tightening torque of 35 N using a torque wrench. We waited for 10 min and retightened the connecting screw again to counter the settling effect or embedment relaxation. The seating of the crown was checked and it was found satisfactory. Impression of the abutment was then recorded using poly vinyl siloxane material. The veneering ceramic build up was done to reestablish the contact in the same crown using the model and it was glazed to achieve the needed esthetics. The restoration was recemented in the same day. (Fig. 10)
Fig. 3.

Implant supported crown rotated along the long axis due to abutment screw loosening for removal
Fig. 4.
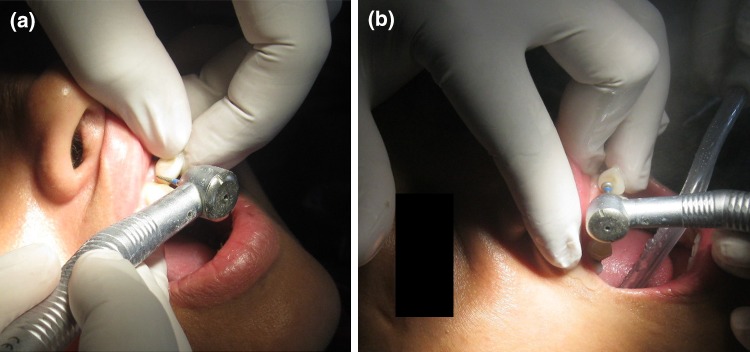
a, b Proximal contact removed using tapering fissure and round wheel diamond points for facilitating crown removal
Fig. 5.

Prosthesis with abutment and connecting screw removed from the patient’s mouth
Fig. 6.

Implant site after removal of the prosthesis and abutment
Fig. 7.

Removed prosthesis with abutment and connecting screw
Fig. 8.

Prosthesis with the abutment in the ceramic furnace for disintegrating the luting cement
Fig. 9.

Separated crown and abutment with connecting screw
Fig. 10.

Prosthesis cemented back after modifying the contact with ceramic build up
Clinical studies have shown that abutment screw loosening is the second most common complication of implant supported prosthesis. Various factors have been considered as possible cause for abutment screw loosening.
Review of Literature
Preload
The contact force clamping together the abutment and the implant is called the preload [13, 14]. Tightening of the implant screw with adequate torque should be done to achieve the optimum preload. Optimum preload of a screw is generated when the screw is elongated until it reaches but does not exceed its yield strength. Ideally the preload should be 75 % of the yield strength or 65 % of the screws fracture strength [13–15]. Preload is primarily dependent on the applied torque and secondarily on the component material, screw head and thread design and surface roughness [13, 14, 16].
Bending of the Screw Joint
Connection of two separated parts has inferior resistance to withstand tensile and shear forces and the bending moment. The stress is concentrated on the implant abutment connection. Hence the strength and stability of the implant abutment connection play an important role in protecting the screw preload. The anti bending ability of screw joint is important in resisting the screw loosening [16, 17]. The internal connection demonstrated increased resistance to the bending moment compared to a conventional external hexagon connection [16, 18].
Settling Effect
Settling occurs as the rough spots flatten under load, since they are the only contacting surface when the initial tightening torque is applied. When the settling effect is greater than the elastic elongation of the screw, screw loosening occurs due to the reduction in forces holding the surfaces together. 2–10 % of the initial preload is lost as a result of settling within the first few seconds or minutes after tightening [19]. So the screw needs to be tightened after initial screw insertion and periodically thereafter. So the screw should be retightened after 10 min to regain the lost preload due to settling [16].
Coefficient of Friction
The coefficient of friction is the ratio of the frictional force to the force acting perpendicular to the two surfaces in contact. Coefficient of friction is a major factor in influencing the preload achieved at a given torque force [20]. This is influenced by the hardness of the threads, surface finish, speed of torquing, surface treatments, presence and quality of lubricants, and fit and machining tolerances. Guda et al. [21] demonstrated that there is a lower limit on the coefficient of friction determined by the implant design geometry below which the abutment screw backs off and preload is lost. Achieving a value of coefficient of friction of about 0.12 for the interface resulted in greater preload at the interface which will reduce the screw loosening [13].
Screw Material
Titanium alloy retention screw followed by titanium alloy retention screw with diamond like carbon coating retained the maximum torque to maintain the preload [20]. Gold alloy retention screw with gold coating and titanium alloy retention screw with aluminum titanium nitride coating had low percentage of the torque retained in the screw for maintenance of preload.
Connection Geometry
Connection geometry influences the amount of screw loosening. They influence the amount of micro motion, stress distribution and micro gap formation. Internal hexagon and octagonal abutments have similar pattern of micro motion and stress distribution [22]. The internal conical abutment produced the highest magnitude of micro motion. The trilobe connection showed lowest magnitude of micro motion. Internal hexagonal connection required greater detorque values than the external hex and internal octagon connections. Morse taper connection provided reduced incidence of abutment screw loosening and also help in distributing the load more favorably in the bone [23–25].
Implant Number and Diameter
Wide diameter implant have wide platform which increases abutment stability by reducing the occlusal table to loading platform cantilever and the concomitant stress to the abutment screw. When wide diameter implant is subjected to masticatory like force (an off axis bending force), the force transmitted to the interface between abutment and implant is distributed over a wider area there by reducing the plastic deformation at the interface of the implant and the abutment. The number of implants also have an effective role in reducing the probability of screw loosening in two piece endosseous root form implants [19, 26]. Screw loosening will be less when two implants are used instead of one to replace a missing tooth. Two implant designs favorably withstood both mesiodistal and buccolingual bending.
Restoration Design and Occlusal Table
Reducing the width of the occlusal table reduced the tendency for screw loosening. Dykema advocated narrowing the buccolingual dimensions of the pontics up to 40 % as means of reducing the load on the abutments [19]. Narrowing the occlusal table and/or moving the occlusal contact area more in line with the implant location reduce the shearing stress on the retaining screws. Flattening the cuspal inclination of the crown also reduce the stress on the retaining screw. Reducing the buccolingual width may require selecting a different occlusal scheme such as a cross-bite relationship or lingualized occlusion to reduce the bending moments on implant and associated structures.
Discussion
In the aforementioned case, patient reported with loosened implant supported prosthesis one week after the cementation of crown. The intra oral periapical radiograph of the site established that it was because of abutment screw loosening. The reason for screw loosening was found to be inadequate application of tightening torque to generate the necessary preload. It is reported that abutment screw loosening is only surpassed by loss of osseointegration as the main cause of failure on implant-supported restorations [14, 27]. The loosening of implant-abutment connecting screw causes problem for both the clinician and patient. It is often necessary to sacrifice the overlying restoration to give access to the screw. The cement-retained implant restorations may be damaged or destroyed in the process, resulting in additional cost and further delay of treatment.
Screws have been studied extensively in the engineering literature and dental implant screws have improved as a result. Together with proper design of the occlusion and stable osseointegration, a reliable connection between implant and abutment is an important precondition for the appropriate functioning and stability of implant restoration [28]. Several clinical studies report widely varying incidences of abutment loosening in different types of abutment connections. In particular, external hex configurations seem to be prone to abutment screw loosening. Limited engagement of the external member and the presence of a short fulcrum point when tipping forces act, are the main reason for abutment screw loosening in external hex connections [29, 30]. In the external hex configuration, the axial preload of the abutment screw is a determining factor for stability of the connection. There is no lock form or positive locking by the external hex. The external hex determines the rotational position but does not absorb any lateral loading and the tensile force. So the stress is concentrated on the abutment screw. Different methods have been tried effectively to reduce the screw loosening. The two important methods used to counteract screw loosening include the incorporation of an antirotational element and attaining optimum screw joint preload [31].
Screw can be considered as a spring, stretched by the preload and the stretch is maintained by the frictional force in the threads [20]. The applied torque develops a force within the screw called preload [32]. As a screw is tightened, it elongates, producing tension [33]. Elastic recovery of the screw pulls the two parts together, creating a clamping force. The preload in the screw, from elongation and elastic recovery, is equal in magnitude to clamping force. Opposing the clamping force is a joint-separating force, which attempts to separate the screw joint. Screw loosening occurs when the joint-separating forces acting on the screw joint are greater than the clamping forces holding the screw unit together. During tightening the micro roughness of the entire metal contacting surface slightly flattens, reducing the distance between the contacting surfaces. There is 2–10 % decrease in the preload due to this and it is known as settling effect or embedment relaxation. [19, 33] The screw needs retightening after 10 min to counter the embedment relaxation. Size and surface area of the contacting threads, the pitch, the screw radius and the diameter of the head of the screw plays a major role in the relationship between applied torque and preload [20]. Additional preload reduction may occur due to creep of the metal contacting surface and possible plastic deformation of the screw. External forces cause slippage between the threads causing release of the stretch. This reduces the generated preload which maintain the resistance to loosening. So to avoid screw loosening the stretch generated on tightening which is the preload should be maintained or should be greater than the joint separating force.
Once the connecting screw has become loose, it keeps loosening further due to the various loads acting on the connection during teeth contact. This disengages the hex connection. If the screw has not loosened enough, then the crown may be pulled occlusally and repeatedly turned in anticlockwise direction. Sometimes this is not possible due to adjacent tooth contact. The contact with adjacent teeth may have to be relieved for complete rotation of the crown with the abutment and connecting screw. Even if the connective screw has loosened by one thread, the hex will get disengaged providing adequate room for the anticlockwise movement of connecting screw.
| Factors increasing the load to screw | Factors decreasing the load to screw |
| Micro movement between the implant and abutment | Friction lock design and absence of flat mating surface |
| Inadequate tightening torque | Adequate tightening torque |
| Mismatch between the implant and abutment | Reducing the coefficient of friction between the implant and abutment |
| Off axis load on the prosthesis | Axial load on the prosthesis |
| Reduced size and number of implants for replacing the teeth | Adequate number and width of implant |
| Increased cantilever | Reduced cantilever |
| Sharp cusp and large occlusal table | Flattened cusp and narrow occlusal table |
| External hex connection | Internal hex connection |
Binon and McHugh found that the reduction of rotational misfit would make the screw joint more resistant to screw loosening [6]. The implant hexagon extension height has been considered important in maintaining antirotational stability of the screw joint [31, 34]. English reported that the external hexagon requires a minimum height of 1.2 mm to attain optimal antirotational effect [35]. The amount of screw loosening is comparatively less in internal hex connections. Internal interface design offers a reduced vertical height for restorative components, distribution of lateral loading deep within the implant, a shielded abutment screw, long internal wall engagements that create a stiff unified body that resist joint opening, wall engagement with the implant that buffers vibration potential for a microbial seal, extensive flexibility and the ability to lower the restorative interface to the implant level esthetically.
The various reasons given in the literature for abutment screw loosening include inadequate preload, inappropriate implant position, inadequate occlusal scheme or crown anatomy, variations in hex dimension, coupled with equal variations in the abutment counterparts, slight differences in fit and accuracy, tension on abutment and cylinder from ill fitting restorations, improper screw design, and excessive occlusal forces [10–12].
The several guidelines recommended for improving screw joint stability are centering the occlusal contact, flattening cuspal inclination, proper tightening of the abutment screw, narrowing the buccolingual width of the restoration, and reducing cantilevers. [19] Incorporation of these features into the restoration will help to reduce the incidence of abutment screw loosening.
There are three methods for managing abutment screw loosening. The most conservative method is removal of the crown along with the abutment as described in the case report. The second method is to identify the access to the connecting screw head. The access may be labial, occlusal or lingual. This should be recorded during the cementation of the prosthesis. The abutment connecting screw is then removed or retightened through the perforation made at the access in the crown. Depending on the location of the access the crown can be reused or discarded. The third method vertical cuts are made on the crown to separate the crown from the abutment. This will render the crown non-reusable.
Conclusion
A conservative mode of managing abutment screw loosening without sacrificing the crown with review of literature on the various reasons for abutment screw loosening has been described. Inadequate preload is the most common reason for abutment screw loosening in two piece endosseous root form implants. Usage of recommended tightening torque with wrench having torque gauge will deliver the optimum preload. The screw has to be retightened after 10 min to counter the embedment relaxation between the mating threads. This provides enough clamping force to counteract the joint separating force. Centering the occlusal contact, flattening the cuspal inclination, narrowing the buccolingual width of the restoration and reducing the cantilevers add to the longevity of the implant supported prosthesis.
References
- 1.Adell R, Lekholm U, Branemark PI. A 15-year study of osseointegrated implants in the treatment of edentulous jaw. Int J Oral Surg. 1981;10:387–416. doi: 10.1016/S0300-9785(81)80077-4. [DOI] [PubMed] [Google Scholar]
- 2.Misch CE (2007) Contemporary Implant dentistry, 3rd edn. Mosby, p 3
- 3.Cox JF, Zarb GA. The longitudinal clinical efficacy of osseointegrated dental implants: A 3-year report. Int J Oral Maxillofac Implants. 1987;2:91–100. [PubMed] [Google Scholar]
- 4.Adell R, Eriksson B, Lekholm U, Branemark PI, Jemt T. A long-term follow-up of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants. 1990;5:347–359. [PubMed] [Google Scholar]
- 5.Zarb GA, Schmitt A. The longitudinal clinical effectiveness of osseointegrated implants: The Toronto study. PartIII. Problems and complications encountered. J Prosthet Dent. 1990;64:185–194. doi: 10.1016/0022-3913(90)90177-E. [DOI] [PubMed] [Google Scholar]
- 6.Binon PP. The effect of implant/abutment hexagonal misfit on screw joint stability. Int J Prosthodont. 1996;9:149–160. [PubMed] [Google Scholar]
- 7.Jemt T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Branemark implants in edentulous jaws: A study of treatment from the time of prosthesis placement to the first annual checkup. Int J Oral Maxillofac Implants. 1991;6:270–276. [PubMed] [Google Scholar]
- 8.Jemt T. Multicenter study of overdentures supported by Branemark. Int J Oral Maxillofac Implants. 1992;7:513–522. [PubMed] [Google Scholar]
- 9.Jemt T, Linden B, Lekholm U. Failures and complications in 127 consecutively inserted fixed prostheses supported by Branemark implants: From prostheses treatment to first annual checkup. Int J Oral Maxillofac Implants. 1992;7:40–43. [PubMed] [Google Scholar]
- 10.Artzi Z, Dreiangel A. A screw-lock for single tooth implant superstructures. J Am Dent Assoc. 1999;130:677–682. doi: 10.14219/jada.archive.1999.0277. [DOI] [PubMed] [Google Scholar]
- 11.Schwarz MS. Mechanical complications of dental implants. Clin Oral Implant Res. 2000;11(Suppl 1):156–158. doi: 10.1034/j.1600-0501.2000.011S1156.x. [DOI] [PubMed] [Google Scholar]
- 12.Cavazos E, Bell FA. Preventing loosening of implant abutment screws. J Prosthet Dent. 1996;75:566–569. doi: 10.1016/S0022-3913(96)90464-3. [DOI] [PubMed] [Google Scholar]
- 13.Lang LA, Kang B, Wang R-F, Lang BR. Finite element analysis to determine implant preload. J Prosthet Dent. 2003;90:539–546. doi: 10.1016/j.prosdent.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 14.Stuker RA, Teixeira ER, Beck JCP, da Costa NP. Preload and torque removal evaluation of three different abutment screw for single standing implant restorations. J Appl Oral Sci. 2008;16(1):55–58. doi: 10.1590/S1678-77572008000100011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rafee Al, Nagy WW, Fournelle RA, Dhuru VB, Tzenakis GK, Pechous CE. The effect of repeated torque on the ultimate tensile strength of slotted gold prosthetic screws. J Prosthet Dent. 2002;88(2):176–182. doi: 10.1067/mpr.2002.127652. [DOI] [PubMed] [Google Scholar]
- 16.K-T Yao, H-C Kao, C-K Cheng, H-W Fang, S-W Yip, M-L Hsu (2011). The effect of clockwise and counterclockwise twisting moments on abutment screw loosening. Clin Oral Implant Res 23:1–6 [DOI] [PubMed]
- 17.Akour SN, Fayyad MA, Nayfeh JF. Finite element analyses of two antirotational designs of implant fixtures. Implant Dent. 2005;14:77–81. doi: 10.1097/01.id.0000156388.73638.a7. [DOI] [PubMed] [Google Scholar]
- 18.Lee FK, Tan KB, Nicholls JI. Critical bending moment of four implant-abutment inter-face designs. Int J Oral Maxillofac Implants. 2010;25:744–751. [PubMed] [Google Scholar]
- 19.Bakaeen LG, Winkler S, Neff PA. The effect of implant diameter, restoration design, and occlusal table variations on screw loosening of posterior single-tooth implants restorations. J Oral Implantol. 2001;27:63–72. doi: 10.1563/1548-1336(2001)027<0063:TEOIDR>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.Assuncao WG, Delben JA, Tabata LF, Baraco VAR, Gomes EA, Garcia IR., Jr Preload evaluation of different screws in external hexagon joint. Implant Dent. 2012;21:46–50. doi: 10.1097/ID.0b013e31823fcbce. [DOI] [PubMed] [Google Scholar]
- 21.Guda T, Ross TA, Lang LA, et al. Probabilistic analysis of preload in the abutment screw of a dental implant complex. J Prosthet Dent. 2008;100:183–193. doi: 10.1016/S0022-3913(08)60177-8. [DOI] [PubMed] [Google Scholar]
- 22.Saidin S, Abdul Khadir MR, Sulaiman E, Abu Kasim NH. Effects of different implant-abutment connection on micromotion and stress distribution: Prediction of microgap formation. J dent. 2012;40:467–474. doi: 10.1016/j.jdent.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 23.Balshi TJ, Hernandez RE, Pryszalak MC, et al. A comparative study of one implant versus two replacing a single molar. Int J Oral Maxillofac Implants. 1996;11:372–378. [PubMed] [Google Scholar]
- 24.Hansson S. Implant- abutment interface: Biomechanical study of flat top versus conical. Clin Implant Dent Relat Res. 2000;2:33–41. doi: 10.1111/j.1708-8208.2000.tb00104.x. [DOI] [PubMed] [Google Scholar]
- 25.Hansson S. A conical implant-abutment interface at the level of the marginal bone improves the distribution of stresses in the supporting bone. an axisymmetric finite element analysis. Clin Oral Implants Res. 2003;14:286–293. doi: 10.1034/j.1600-0501.2003.140306.x. [DOI] [PubMed] [Google Scholar]
- 26.Mangano C, Mangano F, Shibli JA, Tettamanti L, Figliuzzi M, D’Avila S, et al. Prospective evaluation of 2,549 morse taper connection implants: 1 to 6-year data. J Periodontol. 2011;82:52–61. doi: 10.1902/jop.2010.100243. [DOI] [PubMed] [Google Scholar]
- 27.Hoyer SA, Stanford CM, Buranadham S, Fridrich T, Wagner J, Gratton D. Dynamic fatigue properties of the dental implant-abutment interface: Joint opening in wide-diameter versus standard-diameter hex-type implants. J Prosthet Dent. 2001;85:599–607. doi: 10.1067/mpr.2001.115250. [DOI] [PubMed] [Google Scholar]
- 28.Norton MR. An in vitro evaluation of the strength of an internal conical interface compared to a butt joint design. Clin Oral Implant Res. 1997;8:290–298. doi: 10.1034/j.1600-0501.1997.080407.x. [DOI] [PubMed] [Google Scholar]
- 29.Weinberg LA. The biomechanics of force distribution in implant-supported prostheses. Int J Oral Maxillofac Implants. 1993;8:19–31. [PubMed] [Google Scholar]
- 30.Weinberg LA, Kruger B. A comparison of implant-prosthesis loading with four clinical variables. Int J Prosthodont. 1995;8:421–433. [PubMed] [Google Scholar]
- 31.Ameen K, Akihiko H, Shuichi N, Osamu M. Effect of lateral cyclic loading on abutment screw loosening of an external hexagon implant system. J Prosthet Dent. 2004;91:326–334. doi: 10.1016/j.prosdent.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 32.Dixon Donna L, Breeding Larry C, Sadler Peter J, Mckay Mathew L. Comparison of screw loosening, rotation and deflection among three implant designs. J Prosthet Dent. 1995;74:270–278. doi: 10.1016/S0022-3913(05)80134-9. [DOI] [PubMed] [Google Scholar]
- 33.Tsuge T, Hagiwara Y. Influence of lateral oblique cyclic loading on abutment screw loosening of internal and external hexagon implants. Dent Mater J. 2009;28:373–381. doi: 10.4012/dmj.28.373. [DOI] [PubMed] [Google Scholar]
- 34.Beaty K. The role of screws in implant systems. Int J Oral Maxillofac Implant. 1994;9(suppl):52–54. [Google Scholar]
- 35.English CE. Externally hexed implants, abutments and transfer devices: a comprehensive overview. Implant Dent. 1992;1:273–282. doi: 10.1097/00008505-199200140-00009. [DOI] [PubMed] [Google Scholar]


