Abstract
There is limited evidence supporting the role of occlusal splints in Temporomandibular disorder (TMD) therapy. The aim of this randomized controlled clinical trial was to assess the efficacy of stabilization splint therapy on TMD related facial pain and mandibular mobility. The sample of study consisted of eighty consecutive patients diagnosed with TMD. Patients were randomly assigned into two groups: a splint group (n = 40) comprising of patients treated with stabilization splint, councelling and masticatory muscle exercises, and a control group (n = 40), comprising of patients treated with councelling and masticatory muscle exercises alone. Data from both the groups were collected at the beginning of the study and after a 6-month follow up. The outcome variables were visual analogue scale on facial pain intensity and clinical findings for TMD (anterior maximal opening, mandibular right laterotrusion, mandibular left laterotrusion, mandibular protrusion, and number of painful muscle sites). Changes within the splint and control groups (before treatment and 6 months after treatment) were analyzed using paired samples t test. Differences in change between the splint and control groups were analyzed using independent samples t-test. The level of significance was set at p < 0.05. Facial pain and number of painful muscle sites decreased, and the mandibular mobility increased significantly in both groups after treatment; however the differences in changes in VAS or clinical TMD findings between the two groups were not statistically significant. The findings of this study show that stabilization splint treatment in combination with counselling and masticatory muscle exercises has no additional benefit in relieving facial pain and increasing the mobility of the mandible than counselling and masticatory muscle exercises alone over a 6-months’ time interval.
Keywords: Temporomandibular disorders, Facial pain, Mandibular mobility, Stabilization splint, Randomized clinical trials
Introduction
Temporomandibular disorders (TMD), according to the American Academy of Orofacial Pain, are defined as ‘a collective term embracing a number of clinical problems that involve the masticatory muscles, the Temporomandibular joint (TMJ) and associated structures, or both’. TMD are a sub-classification of musculoskeletal disorders [1], having a recurrent or chronic course with noticeable fluctuation over time [2]. In adults, signs and symptoms of TMD occur frequently, more often in women than in men [3]. Patients suffering from TMD often present with pain in the jaws, earache, headache, and myofascial pain. The pain is often aggravated by mandibular movements, like chewing and yawning. It is also frequently associated with disturbed function and limited and/or asymmetric movements of the lower jaw [4].
Based on these presenting signs and symptoms, the research diagnostic criteria for temporomandibular disorders (RDC/TMD) applies a dual-axis system to diagnose and classify patients with TMD [5, 6]. The first axis is divided into three groups of commonly occurring TMDs:
Muscle disorders, including myofascial pain with and without limited mandibular opening.
Disc displacement with or without reduction or limited mandibular opening.
Arthralgia, arthritis, and arthrosis.
The second axis includes a 31-item questionnaire, used to evaluate relevant behavioral, psychological, and psychosocial factors (e.g., pain status variables, depression, nonspecific physical symptoms, and disability levels) [5, 6].
Management of TMD aims at relief of pain, reduction of load on masticatory muscles and TMJ, and restoration of normal function. Several different therapies, most of them conservative and reversible, others irreversible, have been advocated for patients with TMD. A number of successful treatment outcomes have been reported. Therapies may include occlusal appliances, pharmacological interventions, physical therapy, physical self-treatment, psychological intervention, acupuncture, and biofeedback [5]. More complex TMD conditions are recommended to be managed using combinations of single therapies [7, 8].
There are various types of occlusal splints described in the literature; they have different indications and functions. The stabilization splint, one such type of occlusal splint, is also known as the Tanner appliance, the Fox appliance, the Michigan splint, or the centric relation appliance. It is a removable appliance that allows the opposing natural teeth to glide unimpeded over its contact or biting surface [9, 10]. The stabilization splints are constructed to provide separation of the posterior teeth during protrusion and a canine rise during lateral excursions. Before use, these splints are adjusted to freedom in centric and to include multiple bilateral occlusal contacts in the centric relation position. Providing this kind of ideal occlusion by the use of splint therapy reduces abnormal muscle activity and produces “neuromuscular balance” [10]. It has been in use since the 1960s, was introduced by Ramfjord and Ash, and is considered the “gold standard” of all oral appliances [8]. It has been recommended by many clinicians around the world for the management of patients with TMDs, including masticatory muscle pain. In a recent German questionnaire survey, the stabilization appliance was by far the most frequently used appliance type among general dentists and dental specialists [11].
Normally, it is suggested that patients wear the splint only at night. The splint needs to be adjusted (rebalancing of the splint to the new position of the jaw by grinding some of its surface points, since the lower jaw will adopt a new position as a result of wearing the splint) over several visits as the masticatory muscles relax until a consistent jaw relationship is reached. The patients then should be reviewed at regular intervals. After a period of successful splint therapy (normally between two and three months), patients can be weaned off the splint [10].
Most of the patients who suffer from TMD problems of mainly muscular origin benefit from stabilization splints, but there is not enough evidence that they are better than placebo splints, soft splints or other conservative treatment methods [12]. Recently, randomized clinical trials (RCT) have found that stabilization splints are more effective than other treatments [13–15]. However, there are some studies that have yielded contradictory results [16, 17]. Because of these diverse opinions, there obviously is a strong need for further RCTs to identify if a stabilization appliance is really effective. The aim of this RCT was therefore to examine the efficacy (with a 6-month follow-up), of treatment with a stabilization appliance, on TMD-related facial pain and mandibular mobility.
Materials and Methods
Eighty patients were selected from those referred to Government Dental College and Hospital, Ahmedabad, for treatment of TMD over a period of one year, and comprised the study population.
The inclusion criteria for the study were as follows:
-
(i)
Subjects who experienced common symptoms of TMD (i.e.impaired range of movement, impaired TM-joint function, muscle pain, TM-joint pain, and/or pain on movement of the mandible) that had lasted for at least 6 months were targeted for participation in this trial. At the first visit, the clinician collected the patients’ anamnestic data and case histories, including questions about pain related to the TM and neck region, use of medication, and general musculoskeletal pain elsewhere. Finally, a functional examination of the masticatory system and diagnoses of the patients were made according to the Axis I RDC/TMD [6] by the same clinician.
-
(ii)
Subjects of at least 20 years of age.
-
(iii)
Subjects lacking general diseases (like rheumatoid arthritis) that may affect masticatory muscles or TMJs.
-
(iv)
Subjects wanting treatment for their condition.
The exclusion criteria were:
-
(i)
The presence of complete or removable partial prostheses with distal extensions.
-
(ii)
Patients already having received medical, pharmacological or any form of treatments for TMD.
-
(iii)
Individuals with recent facial or cervical trauma.
-
(iv)
Patients with major psychological disorders.
-
(v)
Symptoms related to disease in other components of the stomatognathic system e.g., toothache, neuralgia).
-
(vi)
Cases with congenital abnormality, concomitant inflammatory or neoplastic conditions.
-
(vii)
Patients with parafunctional oral habits such as clenching, bruxism etc.
The study was performed as a randomized controlled trial after it was independently reviewed and approved by an ethical board. After each participant’s eligibility was confirmed, and after an understanding and written consent for the study was obtained from each subject, a clinician drew a sealed envelope from a series of envelopes, each containing a card indicating either of two treatments for that individual, and two groups were made. The splint group (n = 40), was treated with stabilization splint therapy, counselling and masticatory muscle exercises, and the control group (n = 40) received counselling and instructions for masticatory muscle exercises. The assignment was made by a table of random sampling numbers. This allocation was done by a clinician who was independent of the trial and unaware of patient diagnosis, and was not involved at any stage in the clinical treatment phase.
Anamnestic data were collected from both groups at the beginning of the study. Anamnestic data included the nature, intensity and duration of the pain that were characterised using questionnaires. The intensity of the present facial pain was measured with a visual analogue scale (VAS) [18]. VAS is a measurement instrument that tries to measure a characteristic or attitude that is believed to range across a continuum of values and cannot easily be directly measured. Operationally a VAS is usually a horizontal line, 100 mm in length, anchored by word descriptors at each end. The patient marks on the line the point that they feel represents their perception of their current state. The VAS score is determined by measuring in millimetres from the left hand end of the line to the point that the patient marks.
A clinical stomatognathic examination, including registration of the ranges of movements of the mandible, deviations of movements, TMJ sounds, masticatory muscle pain, TMJ pain and pain during movements of the mandible according to the RDC/TMD criteria, was performed [18, 19]. All measurements were made with a vernier caliper. This was done as follows:
Measurement of Anterior Maximal Opening (AMO)
The subject was asked to place the mandible in a comfortable position. The subject was asked to open the mouth as far as possible (unassisted). The edge of the millimeter ruler was placed at the incisal edge of the maxillary central incisor that was the most vertically oriented and measured vertically to the labioincisal edge of the opposing mandibular incisor. This measurement was recorded as interincisal opening. If the subject did not open at least 30 mm, to insure understanding, the opening was repeated. If the second opening still did not produce more than a 30 mm opening, the measurement was recorded as interincisal opening. To measure the vertical incisal overlap, the patient was asked to close the teeth completely together. With a pen, the line where the incisal edge of the same maxillary central incisor used before for measurements, overlapped the mandibular incisor, was marked. The distance from the mandibular incisal edge to the marked line was marked and recorded as vertical incisal overlap. The anterior maximal opening is recorded as the sum of interincisal opening and the vertical incisal overlap [6].
Measurement of Right Lateral Excursion (RL)
The subject was asked to open slightly and move the mandible as far as possible to the right, even if it was uncomfortable. With the teeth slightly separated, a millimeter ruler was used to measure from the labioincisal embrasure between the maxillary centrals to the labioincisal embrasure of the mandibular incisors; and this measurement was recorded [6].
Measurement of Left Lateral Excursion (LL)
The subject was asked to open slightly and move the mandible as far as possible to the left, even if it was uncomfortable. This measurement was recorded in the same manner as right excursion [6].
Measurement of Protrusion (P)
With the teeth in occlusion, the distance from a point marked on the vestibular surface of the lower incisors to the incisal ridge of the upper incisors was measured. The subject was asked to open slightly and protrude the mandible. The subject was then asked to protrude his mandible by sliding it along the maxilla. If the subject had a deep overbite, he/she was asked to open wider so he/she could protrude without getting interference from the maxillary incisors. In this protruded mandibular position, the horizontal distance from the vestibular surface of the upper incisors to the incisal ridge of the lower incisors was measured. The sum resulted in the measure of mandibular protrusion [6].
Measurement of Number of Painful Muscle Sites (PMS)
Muscle tenderness was evaluated at 20 muscle sites and the number of painful muscle sites was recorded. These 20 sites (ten on each side) were: posterior, middle and anterior Temporalis; origin, body and insertion of Masseter; posterior mandibular region; Submandibular region; lateral Pterygoid; and tendon of Temporalis. The trigger points associated with myofascial pain were identified and any pattern of pain referral was determined. Functional manipulation techniques were used for evaluation of lateral Pterygoid as they are difficult to reliably palpate. Examining the remaining structures for tenderness required that the clinician press on a specific site using the fingertips of the index and third fingers or the spade-like pad of the distal phalanx of the index finger only with standardized pressure, as follows: palpations was done with 2 lb of pressure for extraoral muscles, 1 lb of pressure on the joints and intraoral muscles. Muscles were palpated while using the opposite hand to brace the head to provide stability. The subject’s mandible was kept in a resting position, without the teeth touching. Palpation was done with the muscles in a passive state. As was needed, the subject was asked to lightly clench and relax to identify and to ensure palpation of the correct muscle site. First the site of palpation was located using the landmarks specified for each muscle as in the RDC/TMD and then pressed. Because the site of maximum tenderness may vary from subject to subject and is localized, it was important to press in multiple areas in the region specified to determine if tenderness exists. The subject was asked to determine if the palpation hurts (painful) or if he/she just felt pressure. Any equivocal response or the report of pressure only was recorded as “No Pain”[6].
Stabilization splints were made using heat cure acrylic resin for the maxillary arch. The splints ensured occlusal contact of all mandibular teeth in centric relation, anterior guidance for disocclusion in protrusion, and canine guidance for disocclusion in lateral movements. The patients were instructed to wear the appliance while sleeping at night for a minimum of 12 h [20]. The appliance was adjusted at regular follow up intervals, and after 10 weeks, the patients were advised to gradually reduce wear of the appliance up to a minimum of 8 h a day. All patients were scheduled for recalls in 1-, 7-, 15-, 30-, 90-, 150-, and 180-day intervals for follow up.
Patients were instructed to perform a standardized program for masticatory muscle exercises as described by Carlsson and Magnusson [21]. At the beginning of the training program, active mouth openings, laterotrusive movements and protrusive movements were performed. The mandible was held in the maximal positions for a few seconds on each movement. Thereafter, these movements were made towards resistance provided by patient’s own fingers (Fig. 1). After jaw exercises, the patients were suggested to open the jaw wide, stretching it with fingers a few times for 10–20 s. These movements were repeated 7–10 times per training session, and the sessions were performed 2–3 times per day. The patients received written instructions, and the movements were also demonstrated by the dentist before the treatment and reprised if necessary. The instructions for masticatory muscle exercises were given by the same dentist who fabricated and delivered the splints.
Fig. 1.

Masticatory muscle exercises
Data was collected before treatment as baseline and at 6 months after treatment. The parameters taken into consideration for data analysis were pain intensity on visual analogue scale, anterior maximal opening, right laterotrusion, left laterotrusion, protrusion, and number of painful muscle sites. One specialist in stomatognathic physiology performed the screening, history-taking, clinical examination, reassurance, and information gathering before treatment at the patient’s first visit, as well as the evaluation after the treatment. Another specialist in stomatognathic physiology, who was not involved in the examination at baseline and at follow-up, delivered and adjusted the appliance at regular follow up intervals, and also gave the instructions for masticatory muscle exercise. All subjects had the same number of visits. The first specialist who recorded the data, thus, had no information as to which group the patients belonged.
Results were analyzed in the computer using the Statistical package for the social sciences (SPSS, Chicago, ill), version 12.0, the outcome variables were VAS on pain intensity and clinical TMD findings (masticatory muscle pain on palpation, TMJ pain on palpation, ranges of mandibular movements). Changes within the splint and control groups (before treatment and 6 months after treatment) were analyzed using paired samples t-test. Differences in change between the splint and control groups were analyzed using independent samples t-test. The level of significance was set at p < 0.05.
Results
Amongst the subjects selected for the study, 77.5 % were female and 22.5 % male. The mean age was 34.4 years (range, 20–56).
The distribution of diagnostic subgroups of TMD among the patients is shown in Table 1. The subjects in both the splint and control groups that were examined according to RDC/TMD criteria showed the maximum diagnosis of myofascial pain (85 and 80 % respectively) and none of the patients were diagnosed with Disc displacement without reduction, with limited opening.
Table 1.
Proportion (%) of TMD diagnoses before treatment, assessed with the RDC/TMD criteria
| Condition | Splint group (
n = 40), Number (% within group) |
Control group (n = 40), Number (% within group) |
|---|---|---|
| Myofascial pain | 34 (85) | 32 (80) |
| Myofascial pain with limited opening | 0 (0) | 02 (05) |
| Disc displacement with reduction | ||
| Right | 08 (20) | 07 (17.5) |
| Left | 10 (25) | 10 (25) |
| Disc displacement without reduction | ||
| Right | 02 (05) | 02 (05) |
| Left | 04 (10) | 03 (7.5) |
| Disc displacement without reduction, with limited opening | ||
| Right | 0 (0) | 0 (0) |
| Left | 0 (0) | 0 (0) |
| Arthralgia | ||
| Right extra-auricular | 15 (37.5) | 10 (25) |
| Left extra-auricular | 16 (40) | 09 (22.5) |
| Right intra- auricular | 01 (2.5) | 02 (05) |
| Left intra- auricular | 01(2.5) | 03 (7.5) |
| Osteoarthrosis | ||
| Right | 03 (7.5) | 01 (2.5) |
| Left | 01 (2.5) | 01 (2.5) |
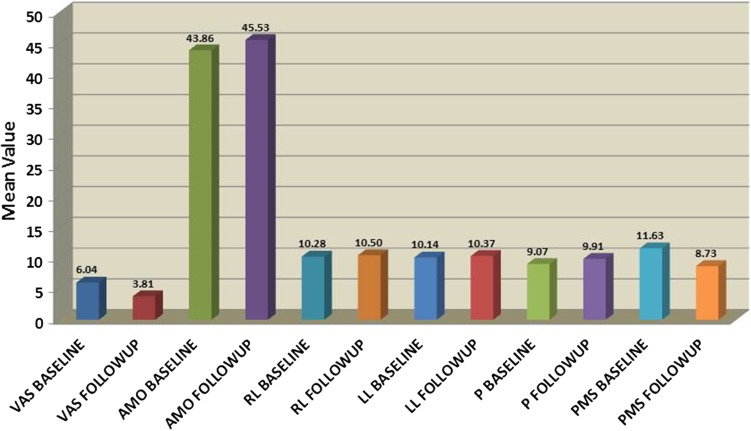
Table 2 demonstrates VAS on pain intensity and clinical TMD findings (anterior maximal opening, right laterotrusion, left laterotrusion, protrusion, and number of painful muscle sites) before the treatment and after a 6-month follow-up for the splint group. A comparison of follow-up data with that of baseline data shows that after 6 months of splint and exercise therapy, there was a decrease in pain intensity (from a mean of 6.043 to 3.808), an increase in anterior maximal opening (from a mean of 43.863 to 45.528 mm), an increase in degree of right mandibular laterotrusion (from a mean of 10.283 to 10.5 mm), an increase in degree of left mandibular laterotrusion (from a mean of 10.140 to 10.373 mm), an increase in degree of mandibular protrusion (from a mean of 9.073 to 9.905 mm). The number of painful muscle sites reduced from a mean of 11.625 to 8.725. The differences between the means in all of these parameters were statistically significant. (p = 0.05). Figure 2 is a graph that compares the VAS on pain intensity and clinical TMD findings before treatment and after a 6 month follow up for the splint group.
Table 2.
Pain intensity (estimated with visual analogue scale, VAS) and clinical TMD findings in the stabilisation splint group before treatment and after a 6-month follow-up
| Mean | N | Standard Deviation | Standard Error Mean | Mean Difference | t value | p value | |
|---|---|---|---|---|---|---|---|
| VAS_baseline | 6.043 | 40 | 0.754 | 0.119 | 2.2350 | 19.607 | <0.0001 |
| VAS_followup | 3.808 | 40 | 1.018 | 0.161 | |||
| AMO_baseline (mm) | 43.863 | 40 | 1.403 | 0.222 | −1.6650 | 6.645 | <0.0001 |
| AMO_followup (mm) | 45.528 | 40 | 1.395 | 0.221 | |||
| RL_baseline (mm) | 10.283 | 40 | 0.981 | 0.155 | −0.2175 | 8.054 | <0.0001 |
| RL_followup (mm) | 10.500 | 40 | 0.980 | 0.155 | |||
| LL_baseline (mm) | 10.140 | 40 | 0.906 | 0.143 | −0.2325 | 3.878 | <0.0001 |
| LL_followup (mm) | 10.373 | 40 | 0.838 | 0.132 | |||
| P_baseline (mm) | 9.073 | 40 | 1.079 | 0.171 | −0.8325 | 5.356 | <0.0001 |
| P_followup (mm) | 9.905 | 40 | 0.562 | 0.089 | |||
| PMS_baseline | 11.625 | 40 | 3.295 | 0.521 | 2.900 | 6.754 | <0.0001 |
| PMS_followup | 8.725 | 40 | 3.088 | 0.488 |
Fig. 2.
VAS on pain intensity and clinical TMD findings before the treatment and after 6-month follow-up for the splint group
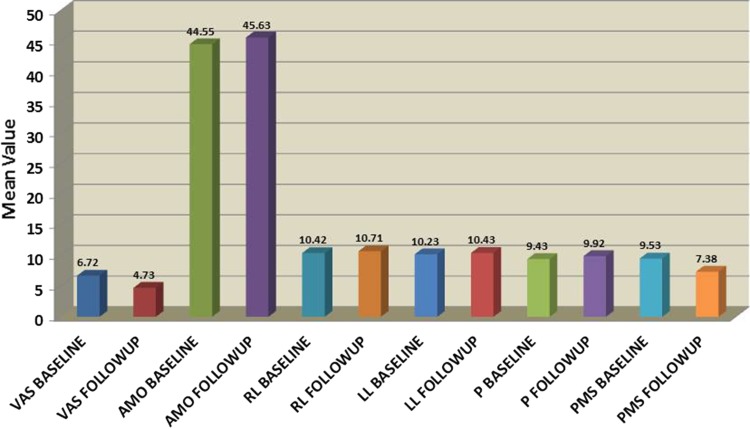
Table 3 demonstrates VAS on pain intensity and clinical TMD findings (anterior maximal opening, right laterotrusion, left laterotrusion, protrusion, and number of painful muscle sites) before the treatment and after a 6-month follow-up for the control group. A comparison of follow-up data with that of baseline data shows that after 6 months of exercise therapy, there was a decrease in pain (from a mean of 6.720 to 4.733), an increase in anterior maximal opening (from a mean of 44.545 to 45.633 mm), an increase in degree of right mandibular laterotrusion (from a mean of 10.415 to 10.713 mm), an increase in degree of left mandibular laterotrusion (from a mean of 10.225 to 10.433 mm), an increase in degree of mandibular protrusion (from a mean of 9.433 to 9.920 mm). The number of painful muscle sites reduced from a mean of 9.525 to 7.375. The differences between the means in all of these parameters were statistically significant. (p = 0.05). Figure 3 is a graph that shows the VAS on pain intensity and clinical TMD findings before treatment and after a 6 months follow up for the control group.
Table 3.
Pain intensity (estimated with visual analogue scale, VAS) and clinical TMD findings in the control group before treatment and after a 6-month follow-up
| Mean | N | standard deviation | Standard error mean | Mean difference | t value | p value | |
|---|---|---|---|---|---|---|---|
| VAS_baseline | 6.720 | 40 | 1.176 | 0.186 | 1.9875 | 13.812 | <0.0001 |
| VAS_followup | 4.733 | 40 | 1.200 | 0.190 | |||
| AMO_baseline (mm) | 44.545 | 40 | 1.846 | 0.292 | −1.0875 | −4.078 | <0.0001 |
| AMO_followup (mm) | 45.633 | 40 | 1.892 | 0.299 | |||
| RL_baseline (mm) | 10.415 | 40 | 0.939 | 0.148 | −0.2975 | −7.218 | <0.0001 |
| RL_followup (mm) | 10.713 | 40 | 0.920 | 0.146 | |||
| LL_baseline (mm) | 10.225 | 40 | 0.932 | 0.147 | −0.2075 | −6.346 | <0.0001 |
| LL_followup (mm) | 10.433 | 40 | 0.847 | 0.134 | |||
| P_baseline (mm) | 9.433 | 40 | 0.677 | 0.107 | −0.4875 | −5.052 | <0.0001 |
| P_followup (mm) | 9.920 | 40 | 0.672 | 0.106 | |||
| PMS_baseline | 9.525 | 40 | 2.987 | 0.472 | 2.150 | 6.569 | <0.0001 |
| PMS_followup | 7.375 | 40 | 3.200 | 0.506 |
Fig. 3.
VAS on pain intensity and clinical TMD findings before the treatment and after 6-month follow-up for the control group
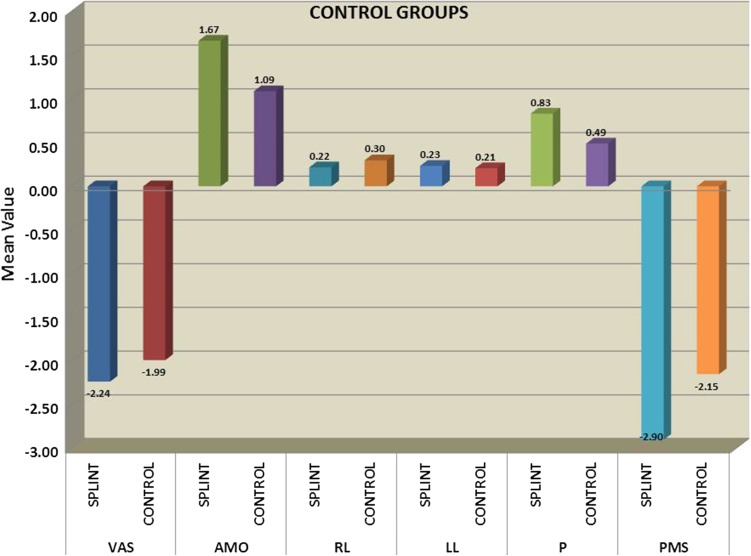
Table 4 compares the degree of improvement in VAS on pain intensity and in the clinical TMD findings between the splint and control group after the 6-months follow up period. The post treatment reduction in degree of VAS on pain intensity was greater in the splint group (difference between means in splint group: −2.235, and in control group: −1.988). The post treatment increase in degree of anterior maximal opening of mandible was greater in the splint group (difference between means in splint group: 1.665, and in control group: 1.088). The post treatment increase in degree of right laterotrusion of mandible was greater in the control group (difference between means in splint group: 0.218, and in control group: 0.298). The post treatment increase in degree of left laterotrusion of mandible was greater in the splint group (difference between means in splint group: 0.233, and in control group: 0.208). The post treatment increase in degree of protrusion of mandible was greater in the splint group (difference between means in splint group: 0.833, and in control group: 0.488). The post treatment decrease in degree of protrusion of mandible was greater in the splint group (difference between means in splint group: −2.900, and in control group: − 2.150). However, none of the difference in these changes between the groups were statistically significant in any of the outcome variables. (p = 0.05). Figure 4 shows the comparison of changes in VAS on pain intensity and clinical TMD findings after a 6-month follow-up, between splint and control groups.
Table 4.
The differences in changes in the visual analogue scale (VAS) and clinical findings of TMD between groups after a 6-month follow-up
| Group | N | Mean | Standard deviation | Standard error mean | Mean difference | t value | p value |
|---|---|---|---|---|---|---|---|
| VAS | |||||||
| Splint | 40 | −2.235 | 0.721 | 0.114 | −0.24750 | 1.348 | 0.182 |
| Control | 40 | −1.988 | 0.910 | 0.144 | |||
| AMO | |||||||
| Splint | 40 | 1.665 | 1.585 | 0.251 | 0.57750 | 1.578 | 0.119 |
| Control | 40 | 1.088 | 1.687 | 0.267 | |||
| RL | |||||||
| Splint | 40 | 0.218 | 0.171 | 0.027 | −0.08000 | 1.624 | 0.108 |
| Control | 40 | 0.298 | 0.261 | 0.041 | |||
| LL | |||||||
| Splint | 40 | 0.233 | 0.379 | 0.060 | 0.02500 | 0.366 | 0.715 |
| Control | 40 | 0.208 | 0.207 | 0.033 | |||
| P | |||||||
| Splint | 40 | 0.833 | 0.983 | 0.155 | 0.34500 | 1.886 | 0.063 |
| Control | 40 | 0.488 | 0.610 | 0.096 | |||
| PMS | |||||||
| Splint | 40 | −2.900 | 2.716 | 0.429 | −0.75000 | 1.389 | 0.169 |
| Control | 40 | −2.150 | 2.070 | 0.327 | |||
Fig. 4.
Comparison of changes in vas on pain intensity and clinical TMD findings after a 6-month follow-up, between splint and control groups
Discussion
The present study evaluates the efficacy of stabilization splint therapy in treatment of temporomandibular disorders. The methods of evaluation correspond to those in the current literature. Facial pain decreased and the mandibular mobility increased in both groups; however the differences in changes between groups revealed that there was no statistically significant difference in improvement in patients belonging to splint group when compared to control group.
In this study, the modest improvement in facial pain observed in both the splint and control group is most likely due to information and to actual positive effects of both treatment methods. There are several previous studies that have found the effect of stabilization splint to be doubtful. For example, the results of this study can be explained based on studies reporting that the symptoms associated with disc displacement with reduction (DDR) or disc displacement without reduction (DDWR) appear to improve over time without treatment [22, 23]. Similarly, the data from another study have showed that 41.9 % of the patients with DDWR who refused any treatment had a significant increase in mouth opening and decrease in pain after one year, although joint noises remained unchanged [23]. Taken together, these data show that not only is the ability of stabilizing splints to recapture the articular disc doubtful, but also, the clinical efficacy in the treatment of disorders like disc displacement remains to be proven. Findings in the above studies are also in accordance with previous reviews that have resulted in the conclusion that the evidence on the effectiveness of stabilisation splint treatment is poor [24, 25].
The significant improvement in facial pain and mandibular mobility in the control group in the present study, which was treated by exercise and councelling, is also in accordance with several studies. An earlier randomized study [26] showed that an exercise-based treatment had more improvement in terms of the daily activity limitation measure. There is also some evidence suggesting that, when combined with thermal application, specific exercise programs focusing on the painful area are effective in reducing pain, strengthening muscles, and improving jaw function [27, 28].
On the other hand, the results of this study are in contrast with those randomized controlled trial studies that have shown stabilisation splints to be more effective than other treatments [14, 15, 29]. In another study with random assignment in patients with disc displacement without reduction, stabilization splint therapy showed significant more pain reduction than therapy with transcutaneous electric nerve stimulation [30]. Other authors found that the use of occlusal stabilization appliances in managing arthralgia is sufficiently supported by evidence in the literature [31]. A prospective randomized study comparing stabilization and pivot splints in DDWR patients demonstrated that both the occlusal splint and a non-treatment control splint significantly improved maximum jaw opening and reduced subjective pain [32]. The two-year follow-up evaluation of splint therapy for ADDWOR (anterior disc displacement without reduction) proved that there was significant improvement in the maximum mouth opening and complaint of pain, and further that the flattening of the condyle had progressed under radiographic observation [33].
The results of the present study are in accordance with other controlled (but non-blinded) studies comparing the outcome of stabilizing splints with that of a control group; although the overall improvement in pain, joint sounds, and maximal opening was noticeable, no significant differences could be found between the groups [34]. Several other studies have found the effect of stabilisation splint to be about at the same level as ‘control’ treatments, that is, control splints [16, 17, 21] or therapeutic jaw exercises [35].
Because of these diverse opinions, there obviously is a strong need for further randomized controlled trials (RCTs) to identify if a stabilization appliance is really effective. Possible explanations for this disconcordance could be the treatment of control group or the length of the study. The majority of the studies have used a range of control splints to control the placebo effect. However, in some of the studies, the control group had received brief information and relaxation treatment or had not received any treatment. Sample sizes also vary across studies, which may explain why some of other studies have been able to show the superiority of the splint treatment compared with other treatments.
Differences in the treatment outcome are expected to be due to the heterogeneity of the patient material and psychological factors [36]. It has been found that patients suffering from widespread pain receive less benefit from stabilisation splint treatment when compared with patients with local masticatory muscle pain [33]. The possible heterogeneity of the patients could not be taken into account in this study. Anyhow, the homogeneity was increased by excluding patients with general diseases that might affect the treatment effect from the study. It should also be noted that the groups were not homogenous regarding the subclassification of TMD diagnosis, which is a limitation of the study. One problem regarding the study methods is the difficulty to control how accurately the patients perform the jaw exercises, which naturally depends on the patients’ own motivation.
In this study, we preferred using masticatory muscle exercises as a control treatment because of economical and practical reasons. This method has been recommended as the first treatment method for patients suffering from TMD of mainly muscular origin [35] and for those suffering from intensive TMD-related pain [37]. Also, it would be unethical to offer any other than commonly accepted treatments.
The treatment effect was measured based both on patients’ subjective estimates on pain intensity and clinical findings, which is the strength of the study. The VAS is a patient’s subjective, individual opinion of pain intensity that has generally been used in pain ratings [36]. All the patients were examined by the same dentist, which eliminates the intra-examiner error and ensures that the examination was made using the same protocol during the study.
Although the treatment time and length of follow-up was standardized in this study, it differs from similar previous studies in the sample size, the treatment time and the period of follow up. Also, because of the high proportion of myofascial pain diagnoses in both the groups and the overlap between different diagnoses, the diagnostic subgroup could not be taken into account in this study. Further studies with sufficient sample sizes are also needed to assess the efficacy of stabilization splint treatment on symptoms specifically related to distinct sub-groups of TMD.
Conclusion
The findings of this randomised controlled study show that stabilisation splint treatment in combination with counselling and masticatory muscle exercises has no additional benefit in relieving facial pain and increasing the mobility of the mandible than counselling and masticatory muscle exercises alone over a 6-months’ time interval. However, the efficacy of the stabilisation splint treatment on TMD in long-time follow-up remains to be confirmed. Further studies with sufficient sample sizes are also needed to assess the efficacy of stabilization splint treatment on symptoms specifically related to distinct sub-groups of TMD.
Contributor Information
Preeti Agarwal Katyayan, Email: preeti80_a@yahoo.com.
Manish Khan Katyayan, Email: drkatyayan@ymail.com.
References
- 1.Okeson JP. Management of temporomandibular disorders and occlusion. St Louis: Mosby; 2008. [Google Scholar]
- 2.Magnusson T, Egermark I, Carlsson GE. A longitudinal epidemiologic study of signs and symptoms of temporomandibular disorders from 15 to 35 years of age. J Orofac Pain. 2000;14:310–319. [PubMed] [Google Scholar]
- 3.LeResche L. Epidemiology of temporomandibular disorders: implications for the investigation of etiologic factors. Crit Rev Oral Biol Med. 1997;8:291–305. doi: 10.1177/10454411970080030401. [DOI] [PubMed] [Google Scholar]
- 4.Okeson JP (ed). Diagnostic classification of orofacial pain disorders. In: Orofacial pain. Guidelines for assessment, diagnosis, and management. Quintessence, Carol Stream, 1996; 45-52
- 5.Dworkin SF, Huggins K, Wilson L, et al. A randomized clinical trial using research diagnostic criteria for temporomandibular disorders:axis I to target clinic cases for a tailored self-care TMD program. J Orofac Pain. 2002;6:48–63. [PubMed] [Google Scholar]
- 6.Dworkin SF, LeResche L. Research diagnostic criteria for Temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301–355. [PubMed] [Google Scholar]
- 7.Vallon D, Nilner M, Soderfeldt B. Treatment outcome in patients with craniomandibular disorders of muscular origin: a 7-year follow-up. J Orofac Pain. 1998;12:210–218. [PubMed] [Google Scholar]
- 8.De Boever JA, Nilner M, Orthlieb J-D, Steenks MH. Recommendations by the EACD for examination, diagnosis, and management of patients with temporomandibular disorders and orofacial pain by the general dental practitioner. J Orofac Pain. 2008;3:268–278. [PubMed] [Google Scholar]
- 9.Gray RJM, Davies SJ, Quayle AA. A clinical guide to temporomandibular disorders. London: BDJ Books; 1997. pp. 1–43. [Google Scholar]
- 10.Gray RJM, Davies SJ. Occlusal splints and temporomandibular disorders: Why, when, how? Dent Update. 2001;28:194–199. doi: 10.12968/denu.2001.28.4.194. [DOI] [PubMed] [Google Scholar]
- 11.Ommerborn MA, Kollmann C, Handschel J, Depprich RA, Lang H, Raab WH-M. A survey on German dentists regarding the management of craniomandibular disorders. Clin Oral Invest. 2010;14:137–144. doi: 10.1007/s00784-009-0282-4. [DOI] [PubMed] [Google Scholar]
- 12.Tu¨ rp JC, Komine F, Hugger A. Efficacy of stabilization splints for the management of patients with masticatory muscle pain: a qualitative systematic review. Clin Oral Invest. 2004;8:179–195. doi: 10.1007/s00784-004-0265-4. [DOI] [PubMed] [Google Scholar]
- 13.Ekberg E, Nilner M. Treatment outcome of appliance therapy in temporomandibular disorder patients with myofascial pain after 6 and 12 months. Acta Odontol Scand. 2004;62:343–349. doi: 10.1080/00016350410010063. [DOI] [PubMed] [Google Scholar]
- 14.Magnusson T, Adiels AM, Nilsson HL, Helkimo M. Treatment effect on signs and symptoms of temporomandibular disorders—comparison between stabilization splint and a new type of splint (NTI). A pilot study. Swed Dent J. 2004;28:11–20. [PubMed] [Google Scholar]
- 15.Wahlund K, List T, Larsson B. Treatment of temporomandibular disorders among adolescents: a comparison between occlusal appliance, relaxation training, and brief information. Acta Odontol Scand. 2003;61:203–211. doi: 10.1080/00016350310003891. [DOI] [PubMed] [Google Scholar]
- 16.Nilner M, Ekberg E, Doepel M, Andersson J, Selovuo K, Le Bell Y. Short-term effectiveness of a prefabricated occlusal appliance in patients with myofascial pain. J Orofac Pain. 2008;22:209–218. [PubMed] [Google Scholar]
- 17.Wassel RW, Adams N, Kelly PJ. Treatment of temporomandibular disorders by stabilizing splints in general dental practice: results after initial treatment. Br Dent J. 2004;197:35–41. doi: 10.1038/sj.bdj.4811420. [DOI] [PubMed] [Google Scholar]
- 18.Fink M, Ku¨nsebeck HW, Schwanewede B, Stiesch-Scholz M, Tschernitschek H, Gehrke A. Introducing a short questionnaire on craniomandibulary dysfunction in daily life for patients with craniomandibulary disorders. J Pharmacol. 2001;10:154–159. [Google Scholar]
- 19.Huggins KH, Dworkin SF, Saunders K, Von Korff M, Barlow W. Five-year course for temporomandibular disorders using RDC/TMD. J Dent Res. 1996;75:352. [Google Scholar]
- 20.Okeson JP, Kemper JT, Moody PM. A study of the use of occlusal-splints in the treatment of acute chronic patients with craniomandibular-disorders. J Prosthet Dent. 1982;48:708–712. doi: 10.1016/S0022-3913(82)80034-6. [DOI] [PubMed] [Google Scholar]
- 21.Carlsson GE, Magnusson T. Treatment modalities. In: Bywaters LC, editor. Management of temporomandibular disorders in the general dental practice. Chicago: Quintessence; 1999. pp. 93–103. [Google Scholar]
- 22.Pedersen A, Hansen HJ. Long-term evaluation of 211 patients with internal derangement of the temporomandibular joint. Community Dent Oral Epidemiol. 1987;15:344–347. doi: 10.1111/j.1600-0528.1987.tb01750.x. [DOI] [PubMed] [Google Scholar]
- 23.Sato S, Kawamura H, Motegi K. Management of nonreducing temporomandibular joint disc displacement. Evaluation of three treatments. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:384–388. doi: 10.1016/S1079-2104(05)80328-2. [DOI] [PubMed] [Google Scholar]
- 24.Forssell H, Kalso E, Koskela P, Vehmanen R, Puukka P, Alanen P. Occlusal treatments in temporomandibular disorders: a qualitative systematic review of randomised controlled trials. Pain. 1999;83:549–560. doi: 10.1016/S0304-3959(99)00160-8. [DOI] [PubMed] [Google Scholar]
- 25.Forssell H, Kalso E. Application of principles of evidencebased medicine to occlusal treatment for temporomandibular disorders: are there lessons to be learned. J Orofac Pain. 2004;18:9–32. [PubMed] [Google Scholar]
- 26.Yuasa H, Kurita K, Treatment Group on Temporomandibular Disorders Randomized clinical trial of primary treatment for temporomandibular joint disc displacement without reduction and without osseous changes: a combination of NSAIDs and mouth-opening exercise versus no treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:671–675. doi: 10.1067/moe.2001.114005. [DOI] [PubMed] [Google Scholar]
- 27.Nelson SJ, Ash MM., Jr An evaluation of a moist heating pad for the treatment of TMJ/muscle pain dysfunction. Cranio. 1998;6:355–359. doi: 10.1080/08869634.1988.11678261. [DOI] [PubMed] [Google Scholar]
- 28.Clark GT, Adachi NY, Dornan MR. Physical medicine procedures affect temporomandibular disorders: a review. J Am Dent Assoc. 1991;121:151–162. doi: 10.14219/jada.archive.1990.0140. [DOI] [PubMed] [Google Scholar]
- 29.Raphael KG, Marbach JJ. Widespread pain and the effectiveness of oral splints in myofascial face pain. J Am Dent Assoc. 2001;132:305–316. doi: 10.14219/jada.archive.2001.0173. [DOI] [PubMed] [Google Scholar]
- 30.Linde C, Isacsson G, Jonsson BG. Outcome of 6-week treatment with transcutaneus electric nerve stimulation compared with splint on symptomatic temporomandibular joint disc displacement without reduction. Acta Odontol Scand. 1995;53:92–98. doi: 10.3109/00016359509005953. [DOI] [PubMed] [Google Scholar]
- 31.Kreiner M, Betancor E, Clark GT. Occlusal stabilization appliances. Evidence of their efficacy. J Am Dent Assoc. 2001;132:770–777. doi: 10.14219/jada.archive.2001.0274. [DOI] [PubMed] [Google Scholar]
- 32.Stiesch-Scholz M, Tschernitschek H, Roßbach A. Early begin of splint therapy improves treatment outcome in patients with temporomandibular joint disc displacement without reduction. Clin Oral Invest. 2002;6:119–123. doi: 10.1007/s00784-002-0162-7. [DOI] [PubMed] [Google Scholar]
- 33.Kai S, Kai H, Tabata O, Shiratsuchi Y, Ohishi M. Long-term outcomes of nonsurgical treatment in nonreducing anteriorly displaced disc of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:258–267. doi: 10.1016/S1079-2104(98)90005-1. [DOI] [PubMed] [Google Scholar]
- 34.Lundh H, Westesson PL, Jisander S, Eriksson L. Disc -repositioning onlays in the treatment of temporomandibular joint disc displacement: comparison with a flat occlusal splint and with no treatment. Oral Surg Oral Med Oral Pathol. 1988;66:155–162. doi: 10.1016/0030-4220(88)90084-9. [DOI] [PubMed] [Google Scholar]
- 35.Magnusson T, Syre′n M. Therapeutic jaw exercises and interocclusal appliance therapy. A comparison between two common treatments of temporomandibular disorders. Swed Dent J. 1999;23:27–37. [PubMed] [Google Scholar]
- 36.Conti PC, de Azevedo LR, de Souza NV, Ferreira FV. Pain measurement in TMD patients: evaluation of precision and sensitivity of different scales. J Oral Rehabil. 2001;28:534–539. doi: 10.1046/j.1365-2842.2001.00727.x. [DOI] [PubMed] [Google Scholar]
- 37.Fricton J. Current evidence providing clarity in management of temporomandibular disorders: summary of a systematic review of randomized clinical trials for intra-oral appliances and occlusal therapies. J Evid Based Dent Pract. 2006;6:48–52. doi: 10.1016/j.jebdp.2005.12.020. [DOI] [PubMed] [Google Scholar]