Abstract
Amelogenesis imperfecta (AI) is a hereditary disorder expressing a group of conditions which cause developmental alterations in the structure of enamel. This disorder has an adverse impact on oral health and also hampers the quality of life of the individual causing physiologic problems. The treatment of such patients would not only upgrade their quality-of-life, but also improve their self-esteem. The correction of such severely worn out dentition may require extensive restorative treatment to achieve appropriate results. It is important to identify the factors that contribute to the excessive wear and loss of vertical dimension. The correction of the defects has to be done without violating the biologic or mechanical principles. Full mouth rehabilitation in such patients improves esthetics, function and comfort. The following case report presents a systematic approach in rehabilitating a case of AI hypoplastic type using full mouth metal reinforced porcelain restorations.
Keywords: Amelogenesis imperfecta, full mouth rehabilitation, occlusal wear, vertical dimension
Introduction
Amelogenesis Imperfecta (AI) is a hereditary disorder that affects the development of enamel.1 The common problems associated with AI are sensitivity, loss of vertical height, dysfunction and esthetics. Restoration of these defects is important in meeting the esthetics, functional, and psychological concerns of the patient. Recent materials and improved clinical procedures have enabled esthetic and functional rehabilitation for patients with such severely worn out dentition.2 The following clinical report demonstrates a multidisciplinary approach in treating a patient who presented with AI.
Case Report
A 32-year-old male patient reported to the Department of Prosthodontics with a complaint of discolored teeth, generalized sensitivity, chipping off of teeth, and difficulty in chewing (Figure 1).
Figure 1.
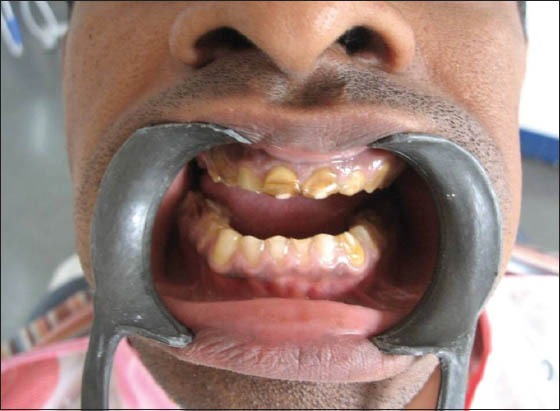
Pre-operative view shows discolored and chipped off teeth.
No abnormality was detected in temporomandibular joint movements. Intraoral examination revealed unaesthetic appearance, generalized attrition, decreased vertical dimension, dehiscence in relation to 13, sharp incisal edges and anterior edge to edge relation. Discrepancy between centric relation and maximum intercuspation was also found. Radiological examination revealed generalized loss of enamel (Figure 2). Based on the above features, the patient was diagnosed with AI hypoplastic type.
Figure 2.

Radiological examination revealed generalized loss of enamel.
Root canal treatment was advised in relation to 11, 13, 14, 21, 22, 23, 24, 25, 33, 36, 41 and 42. Pankey Mann Schyuler philosophy of full mouth rehabilitation was planned for this patient.3,4
Diagnostic casts were obtained. Following this a facebow transfer was completed. The centric relation position was recorded using aluwax and the casts were mounted on a semi adjustable articulator. The vertical dimension was increased by 3 mm. A heat cure clear acrylic occlusal splint of 3 mm was fabricated, which was to be used by the patient (Figure 3). The patient was examined on the first week and every 2 weeks for 4 months, the adaptation of the temporomandibular joints and muscles was carefully observed during this time.
Figure 3.

A heat cure clear acrylic occlusal splint.
Diagnostic wax up was completed with an increased vertical dimension (Figure 4). The wax up helped in assessing the outcome of the final prosthesis and it also helped in fabricating the temporary restorations. The maxillary and mandibular anterior teeth were prepared and restored with provisional restorations.5 The provisional restorations helped in assessing the esthetics and establishing the customized anterior guidance (Figure 5). Mandibular anteriors were restored followed by maxillary. The splint was modified by cutting the anterior portion, so that it could be used by the patient.
Figure 4.
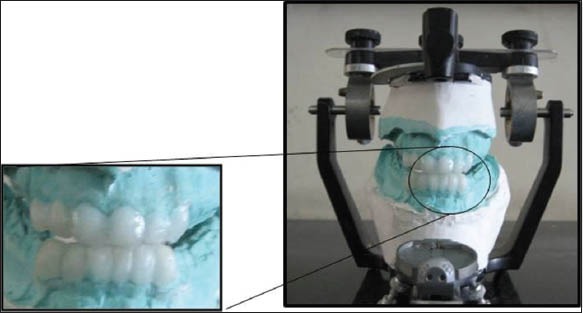
Diagnostic wax up with an increased vertical dimension.
Figure 5.
Customized anterior guidance.
The maxillary and mandibular anterior final restorations were fabricated and luted in the patient’s mouth (Figure 6). The next step was the restoration of the mandibular posterior teeth for which the occlusal plane was established using a Broadrick’s occlusal plane analyzer.3,6 Diagnostic wax pattern was fabricated for mandibular posteriors and verified using the Broderick’s occlusal plane analyzer (Figure 7). After the patterns were fabricated a silicon putty index was made, which acted as a guide in the ceramic build up. Once fabricated the restorations were luted (Figure 8)
Figure 6.

Anterior metal ceramic restorations.
Figure 7.

Broderick’s occlusal plane analyzer.
Figure 8.

Restoration of mandibular posteriors.
The luting of the mandibular posteriors was followed by the fabrication of the maxillary posteriors for which the functionally generated path (FGP) technique was used.3 After the preparation of the maxillary posterior teeth a master impression was made to obtain a maxillary master cast. A facebow transfer was done following which a clear acrylic base was fabricated which extended bilaterally on to the prepared teeth providing cross arch stabilization. The base was kept very thin on the occlusal surface, so that it would not contact the opposing teeth in either centric relation position or any lateral excursive movements. A softened functional wax (inlay wax) was added onto the acrylic base for recording the FGP, and the patient was asked to perform centric and eccentric movements (Figure 9). The FGP should be checked for all movements during excursions to make sure all pathways have been recorded in sufficient functional wax. After confirmation of the movements the wax is chilled with ice water to make it firm, and a smooth creamy mix of fast setting stone is jiggled into the depressions of the functional wax. The fast setting stone must cover at least one unprepared tooth (restored canine) in front that served as a definite vertical stop and a positive key to the master dies used in the laboratory (Figure 10). The mandibular cast was removed from the articulator, and the FGP base with the stone core was placed against the maxillary cast and mounted. The functional core is a 3 dimensional record of the border pathways and so the articulator serves merely as a devise to maintain the relationship of the dies to the recorded paths of movement of the lower teeth.3 The denture base with the functional wax was removed; the wax patterns were fabricated and casted. After the metal trial was verified the ceramic build up was completed with the help of the stone core. The stone core acted as a guide in removing the centric and eccentric interferences. The bisque trial was done in the patient’s mouth. After correcting the interferences the restorations were glazed and luted. A group function type of occlusal scheme was provided to the patient (Figure 11) and regular follow-up with good oral hygiene maintenance was advised (Figure 12).
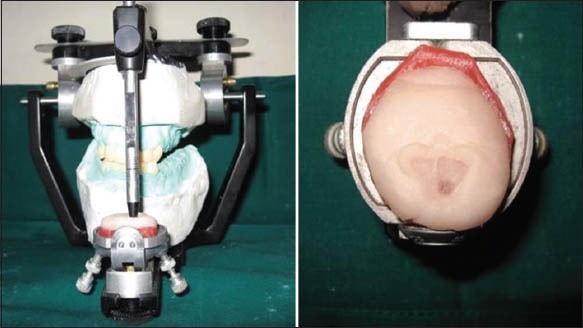
Figure 9.

Functionally generated path technique.
Figure 10.

Maxillary posterior restorations fabricated using stone core index.
Figure 11.

Group function type of occlusion on right and left sides.
Figure 12.

Pre- and post-operative views of the patient.
Discussion
The clinical presentation of AI varies with the type. The hypoplastic type shows well mineralized enamel, but its amount is reduced as seen in the radiograph.1 In this case, the patient presented with a decreased vertical dimension and a freeway space of 5 mm, hence it was decided to increase the vertical dimension by 3 mm.7,8 The severe wear of anterior teeth facilitates the loss of anterior guidance, which protects the posterior teeth from wear during excursive movements. Collapse of posterior dentition results in loss of normal occlusal plane and decreased vertical dimension.5
The choice of restoration in this case was porcelain fused to metal as this would double the mechanical durability, recover esthetics, and protect the residual dentin.9,10
Conclusion
Severe tooth wear is frequently multi-factorial and variable. The treatment of such cases involves a careful analysis of the relationship between natural teeth and the stomatognathic system.
Clinical significance
The above case reflects the importance of the use of prosthodontic principles and strategic planning in addition to a multidisciplinary approach in managing a patient of AI.
Footnotes
Source of Support: Nil
Conflict of Interest: None
References
- 1.Canger EM, Celenk P, Yenísey M, Odyakmaz SZ. Amelogenesis imperfecta, hypoplastic type associated with some dental abnormalities: A case report. Braz Dent J. 2010;21(2):170–4. doi: 10.1590/s0103-64402010000200014. [DOI] [PubMed] [Google Scholar]
- 2.Hedge C, Krishna DP, Jacob SJ, Shetty M. Full mouth rehabilitation of a severely worn out dentition to functional harmony. J Indian Prosthodont Soc. 2009;9(3):164–6. [Google Scholar]
- 3.Dawson PE. 2nd ed. St. Louis: C.V. Mosby Co; 1989. Evaluation, Diagnosis and Treatment of Occlusal Problems. [Google Scholar]
- 4.Agarwal HS, Agarwal NH, Shah RJ. Full mouth rehabilitation of a patient with enamel hypoplasia using hobo's twin tables technique for occlusal rehabilitation: A case report. J Adv Oral Res. 2012;3(2):23–9. [Google Scholar]
- 5.Song MY, Park JM, Park EJ. Full mouth rehabilitation of the patient with severely worn dentition: A case report. J Adv Prosthodont. 2010;2(3):106–10. doi: 10.4047/jap.2010.2.3.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nayar S, Aruna U, Hussain S, Bhuminathan S, Jayesh R. Full mouth rehabilitation of a patient with severly attrited dentition. Indian J Multidiscip Dent. 2011;1(3):157–60. [Google Scholar]
- 7.Banerjee S, Chakraborty N, Singh R, Gupta T, Banerjee A. Full mouth rehabilitation of a patient with severe attrition using hobo twin stage procedure. Int J Prosthodont Restor Dent. 2011;1(3):177–81. doi: 10.4103/0976-237X.94558. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 8.Moslehifard E, Nikzad S, Geraminpanah F, Mahboub F. Full-mouth rehabilitation of a patient with severely worn dentition and uneven occlusal plane: A clinical report. J Prosthodont. 2012;21(1):56–64. doi: 10.1111/j.1532-849X.2011.00765.x. [DOI] [PubMed] [Google Scholar]
- 9.Mizrahi B. Combining traditional and adhesive dentistry to reconstruct the excessively worn dentition. Eur J Esthet Dent. 2008;3(3):270–89. [PubMed] [Google Scholar]
- 10.Nam J, Raigrodski AJ, Heindl H. Utilization of multiple restorative materials in full-mouth rehabilitation: A clinical report. J Esthet Restor Dent. 2008;20(4):251–63. doi: 10.1111/j.1708-8240.2008.00188.x. [DOI] [PubMed] [Google Scholar]


